Abstract
The effects of vitamin D on osteoblast mineralization are well documented. Reports of the effects of vitamin D on osteoclasts, however, are conflicting, showing both inhibition and stimulation. Finding that resorbing osteoclasts in human bone express vitamin D receptor (VDR), we examined their response to different concentrations of 25-hydroxy vitamin D3 [25(OH)D3] (100 or 500 nmol·L−1) and 1,25-dihydroxy vitamin D3 [1,25(OH)2D3] (0.1 or 0.5 nmol·L−1) metabolites in cell cultures. Specifically, CD14+ monocytes were cultured in charcoal-stripped serum in the presence of receptor activator of nuclear factor kappa-B ligand (RANKL) and macrophage colony-stimulating factor (M-CSF). Tartrate-resistant acid phosphatase (TRAP) histochemical staining assays and dentine resorption analysis were used to identify the size and number of osteoclast cells, number of nuclei per cell and resorption activity. The expression of VDR was detected in human bone tissue (ex vivo) by immunohistochemistry and in vitro cell cultures by western blotting. Quantitative reverse transcription-PCR (qRT-PCR) was used to determine the level of expression of vitamin D-related genes in response to vitamin D metabolites. VDR-related genes during osteoclastogenesis, shown by qRT-PCR, was stimulated in response to 500 nmol·L−1 of 25(OH)D3 and 0.1–0.5 nmol·L−1 of 1,25(OH)2D3, upregulating cytochrome P450 family 27 subfamily B member 1 (CYP27B1) and cytochrome P450 family 24 subfamily A member 1 (CYP24A1). Osteoclast fusion transcripts transmembrane 7 subfamily member 4 (tm7sf4) and nuclear factor of activated T-cell cytoplasmic 1 (nfatc1) where downregulated in response to vitamin D metabolites. Osteoclast number and resorption activity were also increased. Both 25(OH)D3 and 1,25(OH)2D3 reduced osteoclast size and number when co-treated with RANKL and M-CSF. The evidence for VDR expression in resorbing osteoclasts in vivo and low-dose effects of 1,25(OH)2D3 on osteoclasts in vitro may therefore provide insight into the effects of clinical vitamin D treatments, further providing a counterpoint to the high-dose effects reported from in vitro experiments.
Introduction
Vitamin D was discovered based on its role as an anti-rachitic agent and it is now well understood that vitamin D deficiency results in rickets in adolescents and osteomalacia in adults.1 Regulation of calcium and phosphate by vitamin D is widely studied and it is known to have a major role in maintaining a healthy skeleton. Conversely, vitamin D deficiency on bone in vivo can be compensated by the administration of calcium and phosphate. There is also growing evidence that vitamin D has a direct effect on bone cells; osteoblasts, osteocytes, and osteoclasts.2–4
In vitro studies have revealed that osteoblasts and osteocytes can locally synthesize the active metabolite 1,25(OH)2D3 as they express CYP27B1, as well as having the ability to locally catabolize vitamin D by expressing the CYP24A1 enzyme.5 Peripheral blood mononuclear cell (PBMC)-derived osteoclasts have been shown to express CYP27B1 and are capable of metabolizing 25(OH)D3 into 1,25(OH)2D3, suggesting that metabolism of vitamin D has a role in osteoclast differentiation.6,7 The level of CYP27B1 transcript expression has been shown to increase during RANKL-induced osteoclast differentiation in PBMCs as well as in RAW 264.7 murine cell line.7,8
Our current understanding of the effect of 1,25(OH)2D3 on osteoclast behavior is that 1,25(OH)2D3 promotes formation, but inhibits the resorptive activity of mature osteoclasts derived from human PBMCs and murine cell line RAW 264.7.9 The action of vitamin D on the reduction of osteoclastogenesis is not well defined, but it has been suggested that the metabolism of 25(OH)D3 into 1,25(OH)2D3 reduces osteoclast resorptive capacity by the modification of cellular adhesion and a reduction in the migration of resorptive osteoclasts.10 It has further been proposed that the action of 1,25(OH)2D3 on bone resorption might be by an increase in the proliferation of the precursors of osteoclasts.11
It has been reported that VDR is not expressed by mature osteoclasts in vivo human tissues, but rather in osteoclast precursors.12,13 Stimulation of osteoclast formation by 1,25(OH)2D3 has been shown to be by the upregulation of RANKL in osteoblasts and osteocytes and a direct cell-to-cell contact between osteoclast precursors and osteoblasts.14 Osteoclast function can be blocked by osteoprotegerin, a decoy receptor for RANKL, and osteoprotegerin has been shown to be downregulated in osteoblasts by 1,25(OH)2D3.15–17
Vitamin D metabolites have been used as therapeutic drugs for the treatment of osteoporosis, as bone mass density has been shown to increase in these patients.18 Paradoxically, suppression of bone resorption should lead to an increase in bone mass density. Several studies have been conducted to elucidate the effect of vitamin D on osteoclasts in vivo; however, the effects have been reported as both inhibitory and stimulatory, and the exact mechanisms remain unknown.19 In in vitro studies (doses of more than 1 nmol·L−1), 1,25(OH)2D3 has been shown to have both stimulatory as well as inhibitory effects on osteoclast activity.19–22
In co-culture studies of osteoblasts and hematopoietic cells, active metabolites of vitamin D has been shown to stimulate osteoclastogenesis.23–25 This stimulation has been shown to be an increase in RANKL production and consequently osteoclast stimulation. Hence, 1,25(OH)2D3 has been believed to directly stimulate osteoclast resorption. As the active metabolites of vitamin D has been used therapeutically, the increase in bone mass density in osteoporotic patients has been assumed to be suppression of bone resorption. Thus, the effects of 1,25(OH)2D3 on osteoclast bone resorption in in vitro studies seem to be opposite to in vivo studies. The direct effects of 1,25(OH)2D3 on osteoclast precursor and stimulation of resorption has been suggested, but the mechanism of direct action of vitamin D on bone cells and the dose of vitamin D yet to be determined.19
Seeking to improve the understanding of the effects of vitamin D on osteoclasts, we have examined the expression of VDR receptor in multinucleated resorbing osteoclasts in human bone tissue, as well as in osteoclast cell lysates from in vitro studies. We have also studied the effects of 25(OH)D3 and 1,25(OH)2D3 metabolites on osteoclast activity, with a particular emphasis on lower doses of 1,25(OH)2D3.
Materials and methods
Reagents and chemicals
All chemicals were purchased from Sigma-Aldrich (Gillingham, Dorset, UK), or as otherwise stated. 25(OH)D3 and 1,25(OH)2D3 (Isoscience, CertiMass, Pennsylvania, USA) were dissolved in absolute ethanol at 10−3 mol·L−1 concentration as a stock solution, and stored in light-protected glass vials at −80 °C. Working dilutions of 25(OH)D3 were evaluated by liquid chromatography–mass spectrometry. All sera used for tissue culture were routinely assessed for endogenous levels of 25(OH)D3. Recombinant human M-CSF was purchased from R&D systems Europe (Abingdon, UK) and recombinant human RANKL was purchased from PeproTech (London, UK).
Immunohistochemistry
Human bone samples were collected from patients undergoing total hip/knee replacement under ethical approval and in compliance with the University of Oxford Musculoskeletal Biobank and Human Tissue Act ethical procedures. Cylindrical bone cores were taken longitudinally, fixed in 4% paraformaldehyde at 4 °C overnight, decalcified in 0.5 mol·L−1 ethylenediaminetetraacetic acid (Lonza, UK) solution over 6 weeks, and embedded in paraffin. Paraffin-embedded human bone samples (non-pathological) were kindly provided by Dr Kashima Takeshi, Pathology Department, Nuffield Orthopaedic Centre, University of Oxford. Bone samples were cut in serial sections at 5 μm and mounted on adhesive glass slides (Lecia Biosystems, Milton Keynes, UK). Slides were deparaffinised in xylene and rehydrated through a graded series of alcohols to water. Slides were washed with tris-buffered saline and Tween 20 (TBST), and endogenous peroxidase activity was quenched by 3% hydrogen peroxide for 30 min. Antigen retrieval was performed on an 85 °C hot plate using citrate buffer for 10 min. Non-specific reactivity was blocked in TBST–5% bovine serum albumin for 30 min at room temperature. Representative slides were incubated overnight at 4 °C with mouse anti-human VDR monoclonal antibody (Santa Cruz Biotechnology, Heidelberg, Germany) or for 1 h with mouse anti-human cathepsin K monoclonal antibody (Merck Millipore, Hertfordshire, UK) at a dilution of 1:200 and 1:400, respectively.
After primary antibody incubation reaction, secondary biotinylated rabbit anti-mouse antibody (Vector Laboratories, Peterborough, UK) was applied for 30 min at room temperature. Sections then were rinsed with TBST, and visualized using the avidin–biotin peroxidise diluted at 1:200 for 30 min. Sections were rinsed with TBST and treated with 3,3-diaminobenzidine (Vector Laboratories). Sections were counterstained with hematoxylin for 10 s, washed under running water for 30 s, dehydrated in ethanol, cleared in xylene, and cover slipped with Dibutylphthalate Polystyrene Xylene mounting medium. Sections were examined using an Olympus BX40 light microscope (Philadelphia, PA, USA) and photographs were captured at ×4–20 magnifications. For general morphological analysis, decalcified sections were stained with Mayer’s hematoxylin and eosin, and negative control sections were incubated with the non-immunized mouse IgG2a and IgG1 (R&D Systems, UK).
Cell sorting
Buffy coats enriched of CD14+ monocytes were obtained from Oxford Radcliffe Biobank (Oxford, UK), and cell sorting was performed using the Magnetic-activated cell sorting (MACS) column separation kit according to the manufacturer’s instructions (Miltenyi Biotec, Surrey, UK). Buffy coats were diluted in a 1:1 ratio in α-minimal essential medium (Invitrogen, Paisley, UK), layered over Histopaque and centrifuged (750 g) for 25 min. The interface layer was resuspended in α-minimal essential medium and then centrifuged (600 g) for a further 10 min. The resultant cells were incubated with MACS CD14+ microbeads (Miltenyi Biotec) for 20 min at 4 °C, passed through MACS magnetic column separator, and resuspended in medium supplemented with 10% heat-inactivated charcoal-stripped serum (CSS; Sigma-Aldrich) and the cells were counted by hemocytometer.
Osteoclast formation assay
To assess the extent of osteoclast formation, isolated human CD14+ cells were cultured in 24-well plates (1×106) and maintained in 1 ml α-minimal essential medium-CSS with 25 ng·mL−1 recombinant human M-CSF (R&D Systems) and ±50 ng·mL−1 recombinant human sRANKL (osteoclast culture media; PeproTech). Cells were maintained in osteoclast culture media and treated every other day in the presence or absence of 25(OH)D3 (100 or 500 nmol·L−1) or 1, 25(OH)2D3 (0.1 or 0.5 nmol·L−1) in ethanol as vehicle (total added volume was <1% of the culture medium volume). Osteoclast culture media containing the vitamin D metabolites were changed every other day up to 6 days before RNA and 14 days for protein extraction.
After 6 days in culture, the expression of TRAP in the cultures was examined histochemically. The culture plates were rinsed in phosphate-buffered saline, fixed with 4% formaldehyde for 10 min, and rinsed in distilled water. TRAP was histochemically revealed by a simultaneous coupling reaction using Naphtol AS-BI-phosphate (Sigma-Aldrich, Dorset, UK) as a substrate and Fast violet B (Sigma-Aldrich, Dorset, UK) as the diazonium salt. The wells were then incubated for 60 min at 37 °C in the dark, rinsed three times in distilled water, and the residual activity was inhibited by 4 % NaF for 30 min. TRAP-positive cells, with more than three nuclei, were identified as osteoclasts. The number of generated osteoclasts were assessed using light microscopy. The size of the osteoclasts was determined by image analysis using the ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Osteoclast resorption assay
To assess the extent of resorption, human CD14+ cells were cultured in 96-well plates on 3 mm dentin slices. Cells were maintained in osteoclast culture media and treated every other day in the presence or absence of 25(OH)D3 (100 or 500 nmol·L−1) or 1, 25(OH)2D3 (0.1 or 0.5 nmol·L−1) in ethanol as vehicle. After 14 days, the dentine slices were removed from the 96-well plates, placed in 1 mol·L−1 NH4OH for 30 min, and sonicated to remove adherent cells. Dentins were rinsed in distilled water, air dried, images were captured by light microscopy, and resorption pit surface areas (μm2) were analyzed with image analysis software (ImageJ; http://rsbweb.nih.gov/ij/). In some experiments, cells were removed with 1 mol·L−1 NH4OH, and resorptive pits were stained with toluidine blue and analyzed by light microscopy.
Western blotting
After 3 days of culture of osteoclast precursor and 14 days of culture of osteoclasts, cells were washed with phosphate-buffered saline and homogenized in radioimmunoprecipitation lysis buffer containing protease inhibitor. Samples were sonicated for 30 s and spun at 12 000 r·min−1 for 20 min at 4 °C, the supernatant was collected. and protein concentration was determined using a bicinchoninic acid protein assay kit (Pierce Biotechnology, Rockford, IL, USA). Samples (20 μg per lane) were separated using 10% acrylamide gels and blotted onto polyvinylidene difluoride membranes. Membranes were washed in TBST and blocked with TBST–5% bovine serum albumin. Samples were incubated overnight with mouse anti-human VDR monoclonal antibody (Santa Cruz Biotechnology). Subsequently, the membranes were washed in TBST and incubated with the appropriate secondary antibodies coupled with horseradish peroxidase. Immunoreactive bands were visualized and detected using an enhanced chemiluminescence kit (GE Healthcare Life Sciences, Amersham, UK). For comparison and conformation of VDR expression in human CD14+ cells, cell lysates of human (SaOS-2 and MG-63) and murine (2T3 and MC3T3) osteoblast-like cells as well as HL-60 cell lysates were loaded and examined.
RNA extraction, complementary DNA synthesis, and RT-PCR
Human CD14+ cells were cultured in 24-well plates (1×106) in osteoclast culture medium and presence or absence of 25(OH)D3 (100 or 500 nmol·L−1) or 1,25(OH)2D3 (0.1 or 0.5 nmol·L−1) over 6 days. Total RNA from each treatment was extracted using the RNeasy Mini kit (Qiagen, Manchester, UK) according to the manufacturer’s instructions. Nucleic acid concentrations were measured by NanoDrop ND-1000 spectrophotometer (Thermo Scientific, Loughborough, UK) at 260 nm. The absorbance ratios at 260/280 and 260/230 were used to detect any protein or organic carryover. Samples with both 260/280 and 260/230 ratios of ≥2 were used for further analysis. The integrity of total RNA purified with Qiagen RNeasy kit was also assessed using 1.5% agarose gel electrophoresis and ethidium bromide staining.
A total of 2 μg from each extract was treated with RNase-free DNase I (Thermo Scientific) for 30 min at 37 °C. Removal of genomic DNA was terminated by further heat inactivation with 100 mmol·L−1 ethylenediaminetetraacetic acid at 65 °C for 10 min. First strand complementary DNA synthesis of template RNA extracts was performed using a Veriti 96-well Thermal Cycler (Applied Biosystems, Warrington, UK) using Bio-Rad iScript Reverse Transcription Supermix (Bio-Rad, Hertfordshire, UK) in a final reaction volume of 40 μl according to the manufacturer’s instruction.
RT-PCR was performed using a ViiA7 system (Applied Biosytems) with commercially available lyophilized QuantiTect Qiagen primers: vdr, cyp27b1, cyp24a1, nfatc1, and tm7sf4. A volume of 1 μL of one-twentieth dilutions of templates were used in a total volume of 10 μl reaction in 384-well plates (Applied Biosystems) by two-step cycling (polymerase activation at 95 °C for 2 min, 40 cycles of template denaturation at 95 °C for 5 s, and primer annealing and extension at 65 °C for 30 s) using SYBR green Master Mix (SensiFAST SYBR Lo-Rox kit, Bioline, London, UK). The Ct values for treated samples were normalized to housekeeping genes gapdh and the relative expressions were calculated using ΔΔCt with amplification and accuracy of 98%–100%.
Statistical analysis
All experiments were carried out at least in triplicates and the mean±s.e.m. was calculated. Statistical analyses were carried out using SPSS version 11.0 for windows (SPSS, Chicago, IL, USA). Effects of vitamin D treatments in respect to untreated cells were compared by Student’s t-test and a P value of <0.05 was regarded to indicate a significant difference.
Results
Immunohistochemistry
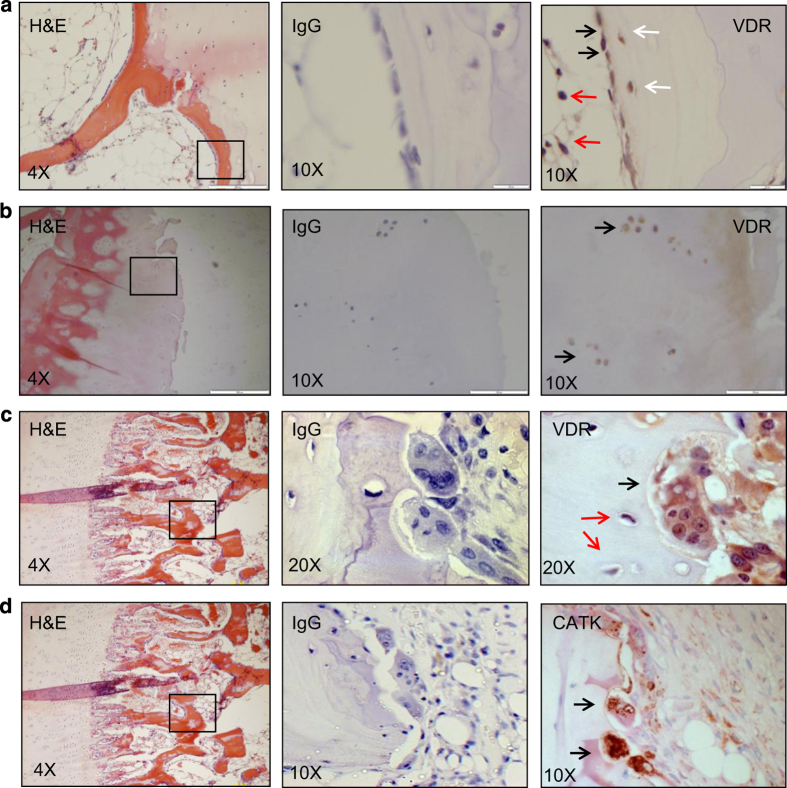
VDR immunoreactivity in human bone tissue was observed in bone lining osteoblasts (Figure 1a, black arrows) and newly embedded osteocytes (Figure 1a, white arrows), but not in mature osteocytes (Figure 1c, red arrows), adipocytes (Figure 1a, red arrows), and chondrocytes (Figure 1b, black arrows). Multinucleated osteoclasts on the bone surfaces with clear lacunar pit (Figure 1c, black arrow) also showed VDR immunoreactivity. Immunohistochemical staining of serial sections revealed that osteoclasts also were immune-reactive for cathepsin K (Figure 1d, black arrows). There was no staining of VDR or cathepsin K in serial sections exposed to non-immunized mouse IgG negative (Figure 1a–d, middle images).
Figure 1.
VDR is expressed by BMSCs, osteoblasts, osteocytes, chondrocytes, and osteoclasts in bone tissue. Serial sections of human bone samples, right column; hematoxylin and eosin staining, middle column; negative staining (IgG), left column; IHC of VDR (a–c), and (d) Cathepsin K (CATK). Positive cross-reactivity of VDR was observed in bone lining osteoblasts (black arrows in a), newly embedded osteocytes (white arrows in a), adipocytes (red arrows in a), chondrocytes (black arrows in b), bone resorbing multinucleated osteoclast (black arrow in c). Negative cross-reactivity was observed in mature osteocytes (red arrows in c).
Western blotting
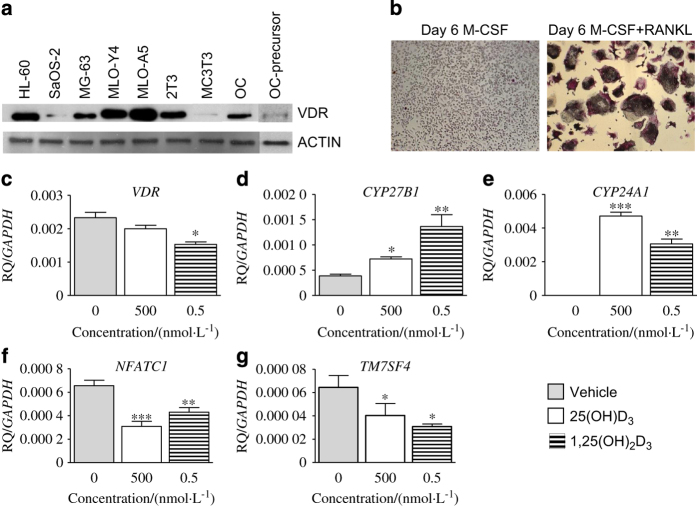
To assess the expression of VDR in vitro cell cultures, cell lysates of human osteoclasts as well as other in-house bone cell lysates were assessed by western blotting. VDR protein was expressed in all cell lysates; human osteoclast precursor, differentiated osteoclasts, human and mouse osteoblast, and mouse osteocyte-like cell lysates as well as HL-60 control sample (Figure 2a), with highest expression in MLO-Y4 and MLO-A5 osteocyte-like cell lines and lowest expression in SaOS-2, MC3T3 osteoblasts, and human osteoclast precursor.
Figure 2.
Bone cells express VDR in in vitro cell culture. Western blots of 20 μg extracts of human osteoblast-like cells SaOS-2, MG-63, osteocyte-like cells MLO-Y4 and MLO-A5, mouse osteoblast-like cells 2T3 and MC3T3 as well as osteoclasts (OC) cell lysates (a). Human CD14+ cells were cultured in 24-well plates (1×106) in osteoclast culture medium (RANKL–M-CSF) and presence or absence of 25(OH)D3 (500 nmol·L−1) or 1,25(OH)2D3 (0.5 nmol·L−1) over 6 days. (b) Representative image of TRAP staining of CD14+ cells in response to M-CSF or RANKL–M-CSF on day 6. Effects of vitamin D metabolites on the relative quantity (RQ) of vitamin D-related signature gene expression; VDR (c), CYP27B1 (d), CYP24A1 (E), NFATC1 (f), and TM7SF4 (g). The magnitude of increase in expression of each gene is normalized to the housekeeping gene GAPDH. Error bars: mean±s.e.m. of triplicates (Student’s t-test), *P<0.05, **P<0.01, and ***P<0.001 for comparisons between vitamin D metabolite treatments against control (gray). Note that Western blot of osteoclast (OC) precursor in a was run separately.
Effect of vitamin D metabolites on vitamin D-related genes
The effects of vitamin D metabolites during osteoclastogenesis on vitamin D metabolic pathway genes was examined by qRT-PCR. Initially, we tested the effects of M-CSF or RANKL–M-CSF for the generation of osteoclasts, where 6 days of RANKL–M-CSF generated maximal number of multinucleated osteoclasts (Figure 2b). The data revealed that osteoclasts express VDR, CYP27B1, and CYP24A1 at messenger RNA level. VDR messenger RNA expression was not altered in response to 500 nmol·L−1 25(OH)D3 (Figure 2c), whereas treatments of osteoclast with 0.5 nmol·L−1 1,25(OH)2D3 suppressed VDR expression (Figure 2c; P<0.05). Treatment of human CD14+ cells with either 500 nmol·L−1 25(OH)D3 or 0.5 nmol·L−1 1,25(OH)2D3 significantly upregulated CYP27B1 (Figure 2d; P<0.05 and P<0.01, respectively) and CYP24A1 (Figure 2e; P<0.001 and P<0.01, respectively). Both 500 nmol·L−1 25(OH)D3 or 0.5 nmol·L−1 1,25(OH)2D3 significantly suppressed NFATC1 (Figure 2f; P<0.001 and P<0.01, respectively) and TM7SF4 (Figure 2g; P<0.05) expression in osteoclasts.
Osteoclast function in response to vitamin D metabolites
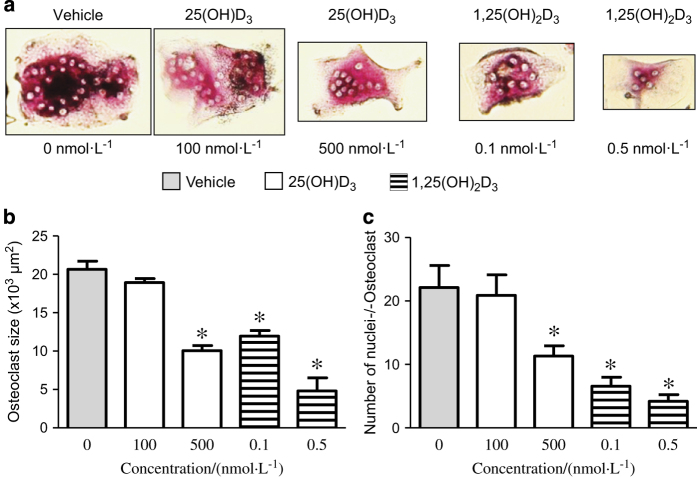
Osteoclast size was not affected in response to concentration of 100 nmol·L−1 of 25(OH)D3 (Figures 3a and b), whereas high concentration of 25(OH)D3 (500 nmol·L−1) significantly reduced osteoclast size (Figures 3a and b: P<0.001). Both doses of 0.1 and 0.5 nmol·L−1 of 1,25(OH)2D3 significantly reduced osteoclast size (Figure 3a and b: 0.1 and 0.5 nmol·L−1; P<0.001).
Figure 3.
Osteoclast size and number of nuclei per osteoclast are reduced by vitamin D metabolites. Human CD14+ cells were cultured in 96-well plates (0.25×106) in osteoclast culture medium (RANKL–M-CSF) and presence or absence of 25(OH)D3 (100 and 500 nmol·L−1) or 1,25(OH)2D3 (0.1 and 0.5 nmol·L−1) over 6 days. After 6 days in culture, the expression of TRAP in the cultures was examined histochemically (a). The size of each osteoclast (b) (μm2) and number nuclei per cell (c) were assessed and determined by image analysis using the ImageJ software (National Institutes of Health). Error bars: mean±s.e.m. of triplicates (Student’s t-test), *P<0.001 for comparisons between vitamin D metabolite treatments against control (gray).
The number of nuclei per osteoclast that is an indication of how many osteoclasts precursors may have fused together was examined in response to vitamin D metabolites. The number of nuclei per osteoclast was not changed in response to 100 nmol·L−1 25(OH)D3, but significantly decreased in response to 500 nmol·L−1 of 25(OH)D3 (Figure 3c). Concentrations of 0.1 and 0.5 nmol·L−1 1,25(OH)2D3 dose-dependently decreased the number of nuclei per osteoclast (Figure 3c).
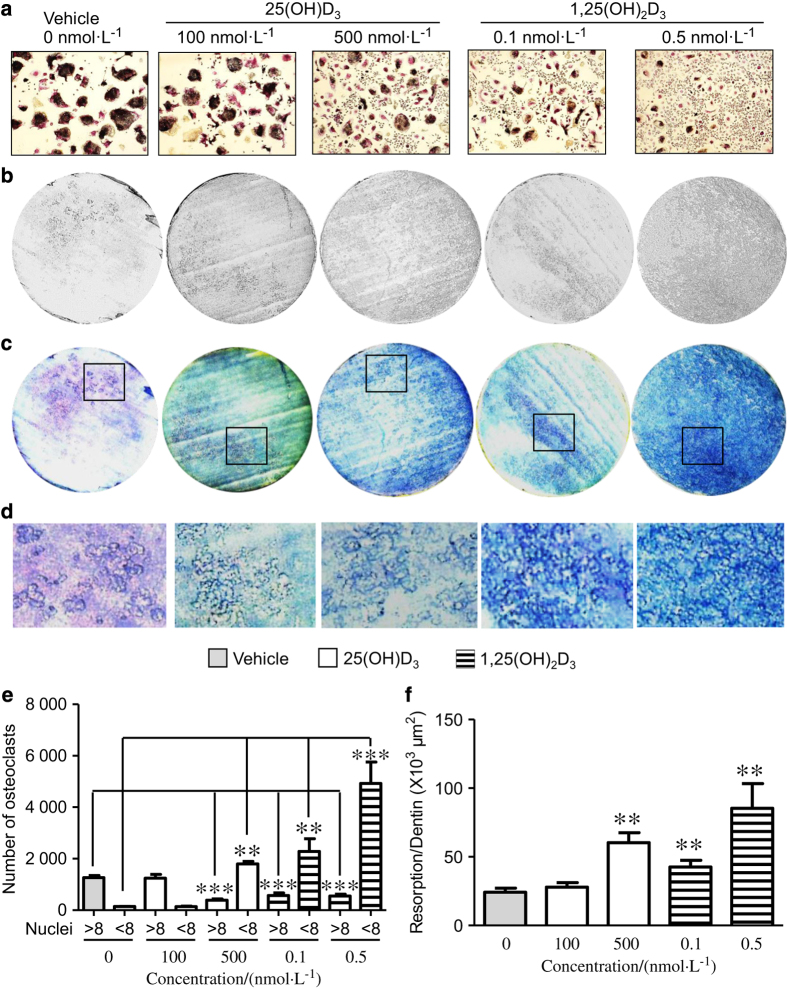
TRAP staining of vitamin D-treated osteoclasts (Figure 4a) revealed that only 500 nmol·L−1 of 25(OH)D3 increased osteoclast cell number (Figure 4e; P<0.05), whereas active metabolites of 1,25(OH)2D3 significantly increased osteoclast cell number (with ≤8 nuclei) dose-dependently (Figure 4e; 0.1 nmol·L−1: P<0.05, 0.5 nmol·L−1: P<0.001, respectively). A concentration of 500 nmol·L−1 of 25(OH)D3 or 0.1 nmol·L−1 of 1,25(OH)2D3 significantly reduces osteoclasts with ≥8 nuclei (Figure 4e; P<0.001). To determine the functional activity of osteoclasts in response to vitamin D metabolites, their resorptive activities on dentine discs were examined (Figures 4b-d). Resorption was not altered when cells were treated with 100 nmol·L−1 25(OH)D3; however, resorption was significantly increased in response to 500 nmol·L−1 25(OH)D3 (Figure 4f). When cells were treated with 1,25(OH)2D3 both concentrations of 0.1 and 0.5 nmol·L−1 significantly increased resorption (Figure 4f). Supra-physiological concentrations of 25(OH)D3 (≥1 000 nmol·L−1) or 1, 25(OH)2D3 (≥1 nmol·L−1) metabolites abolished osteoclast activities (data not shown).
Figure 4.
Vitamin D metabolites increase osteoclast number and resorption. Human CD14+ cells were cultured in 24-well plates (1×106) in osteoclast culture medium (RANKL–M-CSF) or 96-well plates (0.25×106) on 3 mm dentin slices in the presence or absence of 25(OH)D3 (100 and 500 nmol·L−1) or 1,25(OH)2D3 (0.1 and 0.5 nmol·L−1) over 6 days for TRAP staining or 14 days for resorption. After 6 days, the expression of TRAP in the cultures was examined histochemically, images were taken by Zeiss AX10 microscope (Carl Zeiss, Jena, Germany) and number of positive cells (a) with greater or less than eight nuclei were counted manually (e). After 14 days, the dentine slices were removed from the 96-well plates, placed in 1 mol·L−1 NH4OH for 30 min and sonicated to remove adherent cells. Dentins were rinsed in distilled water, air dried, and images were captured by light microscopy (b). Dentins were stained with toluidine blue, photographed (c), and resorption areas per dentin slice (f) (μm2) were analyzed with ImageJ software (National Institutes of Health). (d) High magnifications (×10) of dentins in c. Error bars: mean±s.e.m. of triplicates experiments (Student’s t-test), **P<0.01, and ***P<0.001 for comparisons between vitamin D metabolite treatments against control (gray).
Discussion
This study found that osteoclasts in bone tissue as well as in vitro cell cultures express VDR, and aimed to establish their responsiveness to various concentrations of vitamin D. As shown by qRT-PCR, osteoclastogenesis was stimulated in response to 500 nmol·L−1 of 25(OH)D3 and 0.1–0.5 nmol·L−1 of 1,25(OH)2D3, upregulating CYP27B1 and CYP24A1, but osteoclast fusion markers NFATC1 and TM7SF4 were suppressed by vitamin D metabolites osteoclast number and resorption activity were also increased in response to 25(OH)D3 and 1,25(OH)2D3. Both 25(OH)D3 and 1,25(OH)2D3 reduced osteoclast size and number when co-treated with RANKL and M-CSF. Lower concentrations (100 nmol·L−1) of 25(OH)D3 had no effect on osteoclast activity.
There is growing evidence that bone is an autocrine organ for vitamin D metabolism.21,26 The direct effect of circulatory 25(OH)D3 on bone mineralization has been shown both in human27 and rodent28 studies as well as the effect of 25(OH)D3 and 1,25(OH)2D3 on human and rodent osteoblast cells in in vitro studies.2 Detection of VDR in multinucleated resorbing osteoclasts with distinct resorption lacunae in the current study suggests that in addition to regulating osteoblast mineralization, other cells such as osteoclasts are also direct target of vitamin D metabolites.
Current evidence suggests that osteoblasts, through their VDR expression, mediate the action of 1,25(OH)2D3 on osteoclast activities via RANKL and osteoprotegerin.29 In the current study, we observed that the level of CYP27B1 transcript expression was increased during osteoclast differentiation when treated with 25(OH)D3, M-CSF, and RANKL. This observation suggests that osteoclast cells as being an extra-renal target for 1,25(OH)2D3 synthesis and action and this is consistent with reduced osteoclast TRAP positivity and osteoclast number in CYP27B1 null mouse.30 CYP24A1 is an enzyme that catalyzes the initial steps in inactivation of 1,25(OH)2D3. An increase in the level of this enzyme during osteoclastogenesis initially confirms the action of vitamin D metabolites in osteoclasts and furthermore determine both the level and duration of osteoclast response to 1,25(OH)2D3. These observations are consistent with low level of VDR protein expression in osteoclast precursor compared with higher VDR protein expression in mature osteoclasts as shown by western blotting.
Osteoclast fusion has been shown previously to be regulated by NFATC1 (ref. 31) and TM7SF4,32 and a decrease in the expression of these markers in response to vitamin D metabolites in our study suggests that osteoclast fusion is inhibited. These data are consistent with a decrease in osteoclast size and number of nuclei per each osteoclast. Our data indicate that an increase in osteoclast resorption is due to less fusion resulting in more small osteoclasts in treated conditions rather than fewer larger multinucleated osteoclasts in control samples.
The present study provides immunohistochemical evidence in human bone tissue that osteoclasts express VDR, possibly for metabolism of 25(OH)D3 as well as being responsive to 1,25(OH)2D3 active metabolite. Consistent with our finding, other studies have shown increased expression of VDR messenger RNA in osteoclast resorption lacunae from samples of hyperparathyroidism, osteoclastoma, or pagetic bone.33 It was of interest that beside osteoclasts, other bone cells, such as osteoblasts, newly embedded osteocytes, and adipocytes, as well as chondrocytes, also express VDR, confirming that bone cells could be a target for direct effect of vitamin D metabolites. The tissue expression of VDR by osteoclasts was consistent with its expression in pre-osteoclasts and osteoclasts derived from CD14+ cell lysates from in vitro cell cultures.
Osteoclast cells have been shown to express CYP27B1, metabolizing significant levels of 1,25(OH)2D3 (0.5 nmol·L−1), stimulating osteoclastogenesis, when treated with high concentrations (500 nmol·L−1) of 25(OH)D3.7 An increase in osteoclast cell number and resorption activity in response to 500 nmol·L−1 doses of 25(OH)D3 in our data is probably due to an increase in 1,25(OH)2D3 metabolism that is shown elsewhere.7 The dose-dependent increase in bone resorption observed with 0.1 and 0.5 nmol·L−1 concentrations of 1,25(OH)2D3 active metabolite, however, is in stark contrast to previous findings of a decline in bone resorption by 1,25(OH)2D3.19–21 Our findings also conflict with previous reports on 25(OH)D3. Osteoclast resorption has been reported in response to 25(OH)D3 or its active metabolites, whereas we have shown an increase in osteoclast in response to both metabolites.7,19
This opposite effect could be due to a number of points of difference in the materials used for this study. Of particular, importance is the substantially lower doses of 1,25(OH)2D3 with respect to the literature, which reports doses in the range of 1–100 nmol·L−1.
Related to dosage was the use of CSS and vitamin D metabolites that were pre-screened by liquid chromatography–mass spectrometry for metabolite concentration and the effects of sera+M-CSF alone. After observing surprising TRAP staining results in the control samples in a number of CSS with M-CSF treatment alone, we examined all in-house sera for 25(OH)D3 content by liquid chromatography–mass spectrometry, finding levels of 25(OH)D3 up to 150 nmol·L−1 (fetal calf serum). The CSS used in this study was the only tested sera with no detectable metabolite levels and no TRAP staining was observed in the presence of M-CSF alone. Extending the mass spectroscopy measurements to metabolite supplies, we further observed two batches of purchased 25(OH)D3 and 1,25(OH)2D3 in which vitamin D metabolites could not be detected.
Another source of difference to the majority of previous studies may be the use of CD14+ cells rather than PBMCs, and combined rather than separate treatments of RANKL and M-CSF. This selective isolation of osteoclast precursor cells that are committed to differentiate in response to RANKL–M-CSF factors, may produce a different ‘bulk’ response to PBMCs (containing ~10% precursor).
In conclusion, resorbing osteoclast cells in human bone tissue express VDR, suggesting that vitamin D metabolites could directly affect osteoclast function. Treatments of osteoclasts derived from CD14+ cells with vitamin D metabolites increased osteoclast cell number and resorption. Concentrations of 1,25(OH)2D3 in the 0.1–0.5 nmol·L−1 range dose-dependently increase osteoclast cell number and resorption.
Acknowledgments
We gratefully acknowledge financial support from Orthopaedic Research UK (P 470), Arthritis Research UK (grant 20299 and Oxford EOTC), Marie Curie IRSES skelGEN, the John Fell Fund, and the Oxford NIHR BRU in musculoskeletal disease. We thank Afsie Sabokbar for supplying dentin samples.
The authors declare no conflict of interest.
References
- Holick MF. Vitamin D deficiency. N Engl J Med 357: 266–2812007. [DOI] [PubMed] [Google Scholar]
- Pols H, van Leeuwen J. Osteoblast differentiation and control by vitamin D and vitamin D metabolites. Curr Pharm Des 2004; 10: 2535–2555. [DOI] [PubMed] [Google Scholar]
- Turner AG, Hanrath MA, Morris HA et al. The local production of 1, 25 (OH) 2 D 3 promotes osteoblast and osteocyte maturation. J Steroid Biochem Mol Biol 2014; 144: 114–118. [DOI] [PubMed] [Google Scholar]
- Nociti F, Foster BL, Tran AB et al. Vitamin D represses dentin matrix protein 1 in cementoblasts and osteocytes. J Dent Res 2014; 93: 148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St-Arnaud R. The direct role of vitamin D on bone homeostasis. Arch Biochem Biophys 2008; 473: 225–230. [DOI] [PubMed] [Google Scholar]
- Adams JS, Beeker TG, Hongo T et al. Rapid publication: constitutive expression of a vitamin D 1‐hydroxylase in a myelomonocytic cell line: a model for studying 1, 25‐dihydroxyvitamin D production in vitro. J Bone Miner Res 1990; 5: 1265–1269. [DOI] [PubMed] [Google Scholar]
- Kogawa M, Findlay DM, Anderson PH et al. Osteoclastic metabolism of 25 (OH)-vitamin D3: a potential mechanism for optimization of bone resorption. Endocrinology 2010; 151: 4613–4625. [DOI] [PubMed] [Google Scholar]
- van Driel M, Koedam M, Buurman CJ et al. Evidence for auto/paracrine actions of vitamin D in bone: 1α-hydroxylase expression and activity in human bone cells. FASEB J 2006; 20: 2417–2419. [DOI] [PubMed] [Google Scholar]
- Kogawa M, Anderson P, Findlay D et al. The metabolism of 25-(OH) vitamin D 3 by osteoclasts and their precursors regulates the differentiation of osteoclasts. J Steroid Biochem Mol Biol 2010; 121: 277–280. [DOI] [PubMed] [Google Scholar]
- Kogawa M, Findlay D, Anderson P et al. Modulation of osteoclastic migration by metabolism of 25 (OH)-vitamin D 3. J Steroid Biochem Mol Biol 2013; 136: 59–61. [DOI] [PubMed] [Google Scholar]
- Sahota O, Hosking D. Update on calcium and vitamin D metabolism. Curr Orthop 1999; 13: 53–63. [Google Scholar]
- Bikle D, Adams J, Christakos S. Vitamin D: production, metabolism, mechanism of action, and clinical requirements. In: Rosen C (ed.). Primer on the metabolic bone diseases and disorders of mineral metabolism, 7th ed, Washington, DC, USA: American Society for Bone and Mineral Research; 2009, pp 141–149.
- Menaa C, Barsony J, Reddy SV et al. 1,25-Dihydroxyvitamin D3 hypersensitivity of osteoclast precursors from patients with Paget's disease. J Bone Miner Res 2000; 15: 228–236. [DOI] [PubMed] [Google Scholar]
- Yasuda H, Shima N, Nakagawa N et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci USA 1998; 95: 3597–3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldock PA, Thomas GP, Hodge JM et al. Vitamin D action and regulation of bone remodeling: suppression of osteoclastogenesis by the mature osteoblast. J Bone Miner Res 2006; 21: 1618–1626. [DOI] [PubMed] [Google Scholar]
- Udagawa N, Takahashi N, Jimi E et al. Osteoblasts/stromal cells stimulate osteoclast activation through expression of osteoclast differentiation factor/RANKL but not macrophage colony-stimulating factor. Bone 1999; 25: 517–523. [DOI] [PubMed] [Google Scholar]
- Kondo T, Kitazawa R, Maeda S et al. 1α, 25 dihydroxyvitamin D3 rapidly regulates the mouse osteoprotegerin gene through dual pathways. J Bone Miner Res 2004; 19: 1411–1419. [DOI] [PubMed] [Google Scholar]
- Matsumoto T, Ito M, Hayashi Y et al. A new active vitamin D 3 analog, eldecalcitol, prevents the risk of osteoporotic fractures—a randomized, active comparator, double-blind study. Bone 2011; 49: 605–612. [DOI] [PubMed] [Google Scholar]
- Takahashi N, Udagawa N, Suda T. Vitamin D endocrine system and osteoclasts. BoneKEy Rep 2014; 3: 495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai S, Takaishi H, Matsuzaki K et al. 1-Alpha, 25-dihydroxy vitamin D3 inhibits osteoclastogenesis through IFN-beta-dependent NFATc1 suppression. J Bone Miner Metab 2009; 27: 643–652. [DOI] [PubMed] [Google Scholar]
- Bikle DD. Vitamin D and bone. Curr Osteoporos Rep 2012; 10: 151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suda T, Takahashi N, Abe E. Role of vitamin D in bone resorption. J Cell Biochem 1992; 49: 53–58. [DOI] [PubMed] [Google Scholar]
- Chambers T. The cellular basis of bone resorption. Clin Orthop Relat Res 1980; 151: 283–293. [PubMed] [Google Scholar]
- Takahashi N, Akatsu T, Udagawa N et al. Osteoblastic cells are involved in osteoclast formation. Endocrinology 1988; 123: 2600–2602. [DOI] [PubMed] [Google Scholar]
- Atkins GJ, Kostakis P, Welldon KJ et al. Human trabecular bone‐derived osteoblasts support human osteoclast formation in vitro in a defined, serum‐free medium. J Cell Physiol 2005; 203: 573–582. [DOI] [PubMed] [Google Scholar]
- Anderson PH, Atkins GJ. The skeleton as an intracrine organ for vitamin D metabolism. Mol Aspects Med 2008; 29: 397–406. [DOI] [PubMed] [Google Scholar]
- Need AG, Horowitz M, Morris HA et al. Seasonal change in osteoid thickness and mineralization lag time in ambulant patients. J Bone Miner Res 2007; 22: 757–761. [DOI] [PubMed] [Google Scholar]
- Atkins GJ, Anderson PH, Findlay DM et al. Metabolism of vitamin D 3 in human osteoblasts: evidence for autocrine and paracrine activities of 1α, 25-dihydroxyvitamin D 3. Bone 2007; 40: 1517–1528. [DOI] [PubMed] [Google Scholar]
- Takeda S, Yoshizawa T, Nagai Y et al. Stimulation of osteoclast formation by 1, 25-dihydroxyvitamin D requires its binding to vitamin D receptor (VDR) in osteoblastic cells: studies using VDR knockout mice. Endocrinology 1999; 140: 1005–1008. [DOI] [PubMed] [Google Scholar]
- Panda DK, Miao D, Bolivar I et al. Inactivation of the 25-hydroxyvitamin D 1α-hydroxylase and vitamin D receptor demonstrates independent and interdependent effects of calcium and vitamin D on skeletal and mineral homeostasis. J Biol Chem 2004; 279: 16754–16766. [DOI] [PubMed] [Google Scholar]
- Kim K, Lee S-H, Ha Kim J et al. NFATc1 induces osteoclast fusion via up-regulation of Atp6v0d2 and the dendritic cell-specific transmembrane protein (DC-STAMP). Mol Endocrinol 2008; 22: 176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita K, Iwasaki M, Ochi H et al. Vitamin E decreases bone mass by stimulating osteoclast fusion. Nat Med 2012; 18: 589–594. [DOI] [PubMed] [Google Scholar]
- Mee A, Hoyland JA, Braidman IP et al. Demonstration of vitamin D receptor transcripts in actively resorbing osteoclasts in bone sections. Bone 1996; 18: 295–299. [DOI] [PubMed] [Google Scholar]