Abstract
From 5000 to 10 000 kidney patients die prematurely in the United States each year, and about 100 000 more suffer the debilitating effects of dialysis, because of a shortage of transplant kidneys. To reduce this shortage, many advocate having the government compensate kidney donors. This paper presents a comprehensive cost‐benefit analysis of such a change. It considers not only the substantial savings to society because kidney recipients would no longer need expensive dialysis treatments—$1.45 million per kidney recipient—but also estimates the monetary value of the longer and healthier lives that kidney recipients enjoy—about $1.3 million per recipient. These numbers dwarf the proposed $45 000‐per‐kidney compensation that might be needed to end the kidney shortage and eliminate the kidney transplant waiting list. From the viewpoint of society, the net benefit from saving thousands of lives each year and reducing the suffering of 100 000 more receiving dialysis would be about $46 billion per year, with the benefits exceeding the costs by a factor of 3. In addition, it would save taxpayers about $12 billion each year.
Keywords: clinical research/practice, health services and outcomes research, kidney transplantation/nephrology, law/legislation, organ transplantation in general, dialysis, donors and donation: living, quality of life (QOL), kidney transplantation: living donor, organ allocation
Short abstract
This analysis of a government program to compensate kidney donors indicates the monetary value of saving thousands of lives each year and reducing the suffering of a hundred thousand more on dialysis would be about $46 billion per year, and would save taxpayers about $12 billion a year.
Abbreviations
- ESRD
end‐stage renal disease
- NOTA
National Organ Transplant Act
- QALY
quality‐adjusted life‐year
- SRTR
Scientific Registry of Transplant Recipients
- USRDS
US Renal Data System
Introduction
In June 2014, the American Society of Transplantation and the American Society of Transplant Surgeons held the joint Workshop on Increasing Organ Donation in the United States. They recently released a meeting report 1 on the workshop that concluded, “…we should be working together along the arc of change to remove remaining disincentives, explore opportunities to either change or modify NOTA (National Organ Transplant Act 2), and lay the groundwork for the next steps with our professional colleagues, experts in economics, law and ethics, our partners in Congress and agencies responsible for US health policy and the American public.”
This paper is a response to that invitation. It provides a comprehensive cost‐benefit analysis of a proposed change to NOTA, that is, moving from our current kidney procurement system in which compensation of donors is legally prohibited to one in which the government (not private individuals) compensates living kidney donors $45 000, and deceased donors $10 000. Such compensation would be considered an expression of appreciation by society for someone who has given the gift of life to another. It could include an insurance policy against any health problems that might develop in the future as a result of the donation, including disability and death. Compensation for living donors could be paid in a delayed form, such as tax credits or health insurance, so people who are desperate for cash would not be tempted to sell a kidney. Compensation for deceased donors would be paid to their estate. All other aspects of the kidney procurement and allocation process would continue exactly as they are under the current system. In particular, living donors would continue to be carefully screened and informed of possible hazards associated with kidney donation. Kidneys would be allocated as the organs from deceased donors are now—by the federally funded and managed Organ Procurement and Transplant Network (currently administered under contract by United Network for Organ Sharing). (Satel 3 and Beard et al. 4 have made similar proposals for government compensation of donors.)
A program of government compensation of kidney donors would provide the following benefits:
Transplant kidneys would be readily available to all patients who had a medical need for them, which would prevent 5000 to 10 000 premature deaths each year and significantly reduce the suffering of 100 000 more receiving dialysis.
This would be particularly beneficial to patients who are poor and African American because they are considerably overrepresented on the transplant waiting list. Indeed, it would be a boon to poor kidney recipients because it would enable them to reap the great benefits of transplantation at very little expense to themselves.
Because transplant candidates would no longer have to spend almost 5 years receiving dialysis while waiting for a transplant kidney, they would be younger and healthier when they receive their transplant, increasing the chances of a successful transplantation.
With a large number of transplant kidneys available, it would be much easier to ensure the medical compatibility of donors and recipients, which would increase the success rate of transplantation.
When a first kidney graft fails, the patient would be readily able to obtain a second transplant kidney. (Other considerations might delay a second transplant but not a shortage of transplant kidneys.)
Taxpayers would save about $12 billion each year. Dialysis is not only an inferior therapy for end‐stage renal disease (ESRD), it is also almost 4 times as expensive per quality‐adjusted life‐year (QALY) gained as a transplant.
The incentive for Americans to participate in transplant tourism or the black market for kidneys would virtually cease.
The overall proficiency of kidney transplantation would increase as the number of transplants increases. Currently, the typical kidney transplant center performs only two transplantations a month.
Given the controversial nature of the subject matter of this paper, we have written 12 supplements to explain, justify, and document our key estimates and calculations (which are summarized in Table 1).
Table 1.
Key estimates and calculations
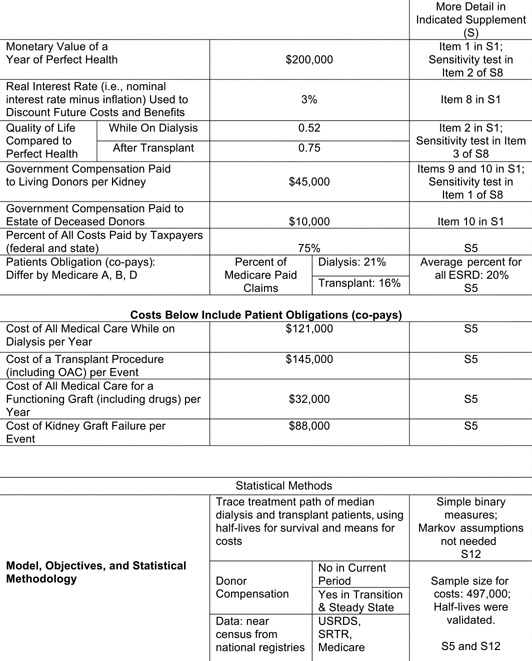
|
This paper updates and expands the path‐breaking work of Matas and Schnitzler 6. The major differences are that this study (a) uses cost‐benefit rather than cost‐effectiveness analysis, (b) uses a consensus monetary value of the extra years of life gained from a transplant, (c) includes patient obligations (copays) in the costs, (d) uses consensus values of the quality of life before and after transplantation, (e) analyzes compensation of deceased donors as well as living donors, (f) uses more recent data on outcomes from dialysis and transplantation, and (g) is more transparent in methodology (Supplement 4 provides a detailed comparison of the two papers.)
Methods
Cost‐benefit analysis is a tool for analyzing public policy issues. It helps clarify who wins and who loses from a given policy, by how much they win or lose, and whether the policy makes society as a whole better or worse off. The costs and benefits are conceived of in the broadest possible sense and include the value of the longer and higher‐quality lives that kidney transplant recipients enjoy. These costs and benefits are calculated in greater detail in Supplement 2. As is standard in cost‐benefit analysis, costs and benefits in the future are discounted back to the present. A consensus real (i.e. zero inflation) interest rate of 3% per annum is used.
This analysis focuses on average (median) ESRD patients. It traces their years of life after starting dialysis or receiving a kidney transplant (see Supplement 12). The median lifetime (half‐life) for a patient group is the time it takes for 50% of them to die, and for kidney grafts, the time it takes for 50% to fail. The median is a good representative statistic for right‐skewed distributions such as survival. Our half‐life estimates are based on 10‐year survival statistics. Our cost estimates are based on the costs of the median dialysis patient and the median transplant patient.
Data
Whenever the literature provided a range of estimates of a variable, the midpoint was used (which we will refer to as the consensus estimate). Our own estimates deliberately err on the side of conservatism; i.e. they tend to reduce the net benefits from having the government compensate kidney donors. (If we had made more realistic estimates, the net benefits from the government compensating kidney donors would have been even greater.)
All statistics on survival and costs originated with Medicare, which provides this information through both the US Renal Data System (USRDS) 7 and the Scientific Registry of Transplant Recipients (SRTR) 8. Our half‐life estimates were validated by comparison with published information and actual survival statistics. (See Supplements 5 and 12 for details on our cost estimates.)
We use a consensus estimate of the value of a year of life of $200 000. (See Item 1 of Supplement 1 3, 11, 13. See also Item 2 of Supplement 8, which provides a sensitivity analysis using $100 000 and $300 000 per year of life.) We follow Whiting 12 in concluding the quality of life—on a scale of 0.0 for death to 1.0 for perfect health—of a dialysis patient is about 0.52 before a transplant and about 0.75 afterward (see Item 2 in Supplement 1).
Table 1 summarizes key estimates and calculations and points toward the supplements where more detail can be found. Table 1 also discusses our statistical methods.
Results
Costs and benefits at the current time when compensating donors is prohibited
(Note: The analysis of costs and benefits presented in this section is abbreviated; greater detail is provided in Supplement 2.) The left column of Table 2 shows statistics for the current situation when donors are not compensated. The top row indicates a typical patient receiving dialysis can expect to live 12.3 years, while the second row shows he or she can expect to live 19.3 years if the patient receives a kidney transplant. (The latter half‐life is the weighted average of the half‐lives of patients who have received kidneys from deceased and living donors, as explained in detail in Supplement 12, particularly Figure S12‐5.) The third row shows the difference (i.e. the transplant recipient can expect to live an additional 7.0 years).
Table 2.
Increase in life years from receiving a transplant compared with remaining on dialysis on waiting list
| No donor compensation (current situation) (2015) | If donors are compensated (steady state after first 5 years) (2020) | ||
|---|---|---|---|
| Expected remaining lifetime (half‐life in years) | If remain on dialysis on waiting list | 12.3 | 15.0 |
| If receive a transplant | 19.3 | 24.9 | |
| Increase in life years from receiving a transplant (vs remaining on dialysis on waiting list) | Increase in life years (unadjusted) | 7.0 | 9.9* |
| Increase in discounted QALYs | 4.7 | 6.7 | |
| Half‐life of transplant kidney graft | 12.6* | 15.7 | |
In the current situation, when the graft fails in 12.6 years, 86% of the patients go back on dialysis. In the steady state case, when the first graft fails, most patients will be readily able to obtain a second transplant kidney.
Based on only 14% receiving a second transplant. In the steady state case, the percentage may approach 100%; hence the number (9.9) may approach 12 years.
Since (as discussed above) the quality of life of a dialysis patient is 0.52 before a transplant and 0.75 afterward, the gain in QALYs for a typical kidney transplant recipient is 0.75 times the life expectancy after receiving a transplant minus 0.52 times the life expectancy if the recipient had remained on dialysis.
After discounting, this yields a gain of 4.7 discounted QALYs as a result of the transplant (row 4 of the left column of Table 2). And valuing each of these years at the consensus estimate of $200 000 produces a lifetime welfare gain of $937 000 per kidney recipient (top row of the left column of Table 3). It is well known that kidney recipients benefit greatly from receiving a transplant, and this puts a credible monetary value on it.
Table 3.
Present value of benefits and costs over a kidney recipient's lifetime (per kidney recipient)
| No donor compensation (current situation) | If donors are compensated (steady state after first 5 years) | |
|---|---|---|
| Benefits | ||
| Welfare gain for kidney recipient (over a lifetime) | $937 000 | $1 335 000 |
| Savings from stopping dialysis (over a lifetime) | $735 000 | $1 454 000 |
| Costs | ||
| Cost of transplant (everything at time of transplant except compensation to donors) | $145 000 | $236 000 |
| Compensation to donors | $0 | $73 000 |
| Medical costs after transplant (including cost of kidney graft failure) | $395 000 | $607 000 |
| Net welfare gain for society per kidney recipient | $1 132 000 | $1 873 000 |
| Addendum | ||
| Taxpayer savings per kidney recipient | $146 000 | $403 000 |
A second benefit of kidney transplants is the savings from kidney recipients no longer requiring dialysis and other medical treatments, which cost about $121 000 per patient‐year and would have continued for the 12.3‐year expected life of a dialysis patient on the waiting list. But the half‐life of a kidney transplant is only 12.6 years (bottom row of left column of Table 2), after which a typical kidney transplant recipient has to return to dialysis for their remaining 6.7 years of life. Consequently, the lifetime net savings from temporarily stopping dialysis would be $735 000 (row 2 of the left column of Table 3).
Turning to the other side of the ledger, the cost of the transplant itself (i.e. payments at the time of the transplant to all parties except the kidney donor) is about $145 000 (row 3 of the left column of Table 3). And compensation to kidney donors is zero because it is currently legally prohibited (row 4).
Medical costs following a transplant are about $32 000 per year for the 12.6‐year expected life of the kidney graft, plus an additional $88 000 when the graft of the typical patient fails in 12.6 years. Thus, the lifetime total costs are $395 000, as shown in the fifth row of the left column of Table 3.
The net welfare gain for society over the lifetime of a kidney recipient (row 6 of the left column of Table 3) is just the net of the rows above it, or $1 132 000.
The bottom row of the left column of Table 3 shows taxpayer savings over the lifetime of the kidney recipient. Because taxpayers currently bear about 75% of the cost of both dialysis and kidney transplants (see Supplement 5), taxpayers would reap 75% of the benefits from patients stopping dialysis after receiving a transplant. Specifically, taxpayer savings are equal to 75% of the savings from stopping dialysis, minus: (a) the cost of the transplant, (b) compensation to donors (when allowed), and (c) medical costs after the transplant. This comes to $146 000 per kidney recipient.
Aggregating the per‐recipient costs and benefits of the left column of Table 3 over all of the kidney recipients in a given year yields the left column of Table 4 (the top seven rows of which have the same arrangement as Table 3). For example, if the $146 000 taxpayer savings per kidney recipient (from the bottom row of the left column of Table 3) is multiplied by a conservatively high estimate of 17 500 kidney recipients each year, the result is the total taxpayer saving from all kidney recipients each year, which is $2.6 billion per year (row 7 of the left column of Table 4).
Table 4.
Present value of benefits and costs for all kidney recipients in a given year (per year)
| No donor compensation (current situation) | If donors are compensated (steady state after first 5 years) | |
|---|---|---|
| 17 500 kidney recipients per year | 35 000 kidney recipients per year | |
| Benefits | ||
| Welfare gain for all kidney recipients in a given year | $16.4 billion/y | $46.7 billion/y |
| Savings from stopping dialysis for all kidney recipients in a given year | $12.9 billion/y | $50.9 billion/y |
| Costs | ||
| Costs of transplants for all kidney recipients in a given year (everything at time of transplant except compensation to donors) | $2.5 billion/y | $8.3 billion/y |
| Compensation to donors for all kidney recipients in a given year | 0 | $2.6 billion/y |
| Medical costs after transplant for all kidney recipients in a given year (including cost of kidney graft failure) | $6.9 billion/y | $21.2 billion/y |
| Net welfare gain for society from all transplant recipients in a given year | $19.8 billion/y | $65.6 billion/y |
| Addendum | ||
| Taxpayer savings from all transplant recipients in a given year | $2.6 billion/y | $14.1 billion/y |
| Benefit‐cost ratio for society | 3.0 | |
| Benefit‐cost ratio for taxpayers | 1.7 | |
Life expectancies when donors are compensated
Now consider two subperiods after the government begins compensating kidney donors: (a) the first 5 years, during which we estimate the 94 000‐patient waiting list for kidneys will be gradually eliminated, and (b) the subsequent “steady state” situation that will obtain after the waiting list has been ended. We will first estimate life expectancies and then use them to estimate the costs and benefits of the government compensating kidney donors.
We assume compensation of $45 000 per kidney will be sufficient to elicit an adequate supply of kidneys from living donors, which, together with some additional kidneys from deceased donors, will end the kidney shortage and eliminate the waiting list in 5 years (see Item 9 of Supplement 1). Thus, during the 5‐year transition period, the number of kidney recipients will increase to about 43 000 per year. This is the sum of the 31 000 patients currently being added to the waiting list each year, plus an additional 12 000 transplants per year needed to reduce the waiting list to zero in 5 years (see Supplement 11 for a discussion of the current capacity of the transplant community).
To simplify comparisons of the current situation with the postcompensation period, we will focus on the steady‐state case after the waiting list has been eliminated. Because the supply of transplant kidneys will now be sufficient to meet the demand, transplant candidates will no longer have to wait about 5 years for a kidney. This has two important implications. First, the average age of kidney recipients will fall from 50 to 45 years. Second, kidney recipients will now be far healthier because they will no longer have to suffer the debilitating effects of several years of dialysis. We estimate these considerations will increase the life expectancy of the typical kidney recipient to about 24.9 years in the steady‐state case from 19.3 years in the current situation (shown in the second row of Table 2 and discussed in Supplement 12). In contrast, if the kidney patient had remained on dialysis, their life expectancy would have been only 15.0 years (top row of the right column of Table 2). This can also be seen in Figure 1, which shows the two treatment paths ESRD patients can take in steady state: dialysis or transplant. Note that the typical kidney recipient in steady state will receive a second transplant after the first graft fails in 15.7 years.
Figure 1.
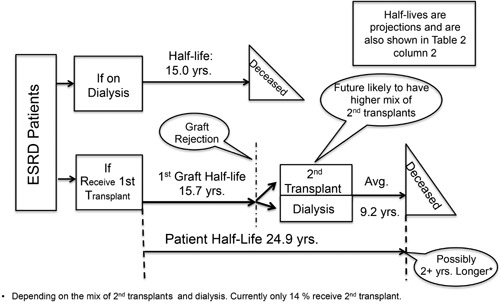
Two treatment paths for ESRD: dialysis or transplant (with donor compensation, steady state, 2020). ESRD, end‐stage renal disease.
Costs and benefits in the steady‐state case
With these life expectancies, we can calculate the increase in discounted QALYs—and the benefits and costs of receiving a kidney transplant—in the steady‐state case, using the same methodology we used in the current situation case.
A kidney recipient in this steady‐state case gains an additional 9.9 years of life from receiving a kidney transplant (row 3 of the right column of Table 2), which translates into 6.7 discounted QALYs (row 4). When this is multiplied by the consensus estimate of the value of a year of life, the result is a lifetime welfare gain of $1 335 000 per recipient (top row of right column of Table 3).
The savings from stopping dialysis is again found by multiplying the expected life of a dialysis patient by the yearly medical cost of dialysis, which yields a lifetime gain of $1 454 000 (row 2 of Table 3). Note that this savings is almost twice that in the current situation case because the typical kidney recipient, instead of going back on dialysis after the first graft fails, will, because of the greater availability of transplant kidneys, soon receive a second transplant.
The cost of the first transplant is, again, $145 000. The cost of the second transplant is the same, and after discounting for a delay of 15.7 years, this raises the total to $236 000 (row 3).
The fourth row of the right column of Table 3 includes the two $45 000 government payments to kidney donors. The first will occur at the time of the initial transplant, and the second occurs 15.7 years later for a typical patient, for a total cost of $73 000. Note that this number is much smaller than the other costs and benefits in Table 3, especially the huge welfare gain for kidney recipients and the savings from stopping dialysis. One of the most surprising and important results of this paper is how small the cost of compensating donors would be compared with the very large welfare gains for society that would result. Note also that it is conservatively assumed that all donors will be paid $45 000 per kidney, including those who previously were willing to donate their kidneys for free. If some of the latter are still willing to donate for free, that will just reduce the costs and increase the net benefits from compensating kidney donors. But if some now decline to donate at all, the cost of replacing their donations with kidneys from compensated donors is already included in the above calculation. This conservative $45 000 estimate also covers the small possibility that—after the government starts compensating kidney donors—all kidneys might come from living donors and none from deceased donors.
The fifth row of the right column of Table 3 shows the lifetime medical costs after a transplant. The 24.9‐year life expectancy of a transplant recipient (from row 2 of the right column of Table 2) is multiplied by the yearly medical expenses. To this is added the $88 000 expense when the kidney graft fails in 15.7 years, bringing the total to $607 000. This is higher than in the current situation because the typical transplant recipient will receive a second transplant with its associated costs.
The net welfare gain for society over a kidney recipient's lifetime will be $1 873 000 (row 6 of the right column of Table 3). This is much larger than in the current situation case because of the longer life expectancy of the kidney recipient and the greater savings from stopping dialysis (because the typical patient will not return to dialysis very long after the first graft fails). The value of these benefits would greatly exceed the additional costs of the second transplant.
The bottom row of the right column of Table 3 shows how much taxpayers would save over the kidney recipient's lifetime, which is $403 000. This is more than twice as much as in the current situation because the additional savings from ending dialysis is much greater than the additional costs of the second transplant.
Aggregating these costs and benefits per kidney recipient in the right column of Table 3 over an estimated 35 000 transplant recipients per year during the steady state period, results in the right column of Table 4. Note in particular that – with a successful donor compensation program – the net welfare gain for society (row 6 of Table 4) would more than triple to $65.6 billion per year from $19.8 billion per year currently. Note also that the savings for taxpayers would increase to $14.1 billion per year from $2.6 billion per year (row 7 of Table 4). Finally, note in the bottom two rows of Table 4 that—moving from the current situation in which compensation of kidney donors is prohibited to one in which the government compensates donors—the benefit‐cost ratio would be a large 3.0 for society as a whole and 1.7 for taxpayers considered alone.
Discussion
Would government compensation of kidney donors exploit the poor?
One of the major arguments of those who oppose compensating kidney donors is that poor people would be more likely to become living donors than would rich people, and, therefore, rich people would wind up buying kidneys from poor people, thereby “exploiting” them. So, it is argued, poor people would be worse off if kidney donors were compensated than they are under the present system.
Our cost‐benefit framework reveals that this line of reasoning is exactly backward. As explained in detail in Supplement 3, the present system, in which compensation of kidney donors is legally prohibited, has resulted in a huge shortage of transplant kidneys that seriously harms all transplant candidates—especially the poor, and especially poor African Americans, because they are considerably overrepresented on the kidney waiting list due to the generally worse state of their health. In contrast, if the government compensated kidney donors, it would greatly increase the availability of transplant kidneys, making all transplant candidates, especially the poor, much better off. Indeed, the poor would enjoy the greatest net benefit because they would gain the $1.3 million value of a longer and healthier life, but almost all of the costs of transplantation for the poor person would be borne by the taxpayer through Medicare and Medicaid.
So the current prohibition on compensating kidney donors, which is supposedly intended to keep the poor from being exploited, is in fact seriously harming them. And having the government compensate kidney donors would be an enormous boon for the poor.
Key Innovations
One of the key innovations of this paper is using a consensus estimate of the monetary value of a QALY, which enables us to employ cost‐benefit analysis to determine the net benefit to society from having the government compensate kidney donors. Our value of $200 000 per QALY is based on a careful review of the literature (see Item 1 in Supplement 1). Moreover, sensitivity tests of $100 000 and $300 000 per QALY were performed (see Item 2 in Supplement 8) and revealed that even for QALY values as low as $100 000, the net welfare gain for society per recipient in steady state would still be a large $1.2 million (vs $1.9 million using the consensus QALY of $200 000).
On the other hand, our proposed donor compensation of $45 000 per kidney is very conservative. It is three times the estimate made by Becker and Elías 5, which is the only serious attempt to estimate this parameter. Sensitivity tests of $25 000 and $65 000 per kidney were performed and had very little effect on our results because donor compensation is very small compared with the other magnitudes in this analysis (see Item 1 of Supplement 8). Indeed, donor compensation could be increased to $375 000 per kidney before taxpayers would no longer save money by paying for kidney transplantation instead of dialysis. And compensation could be increased all the way to $1 200 000 per kidney before society would no longer enjoy a net welfare gain from transplantation.
Cost‐effectiveness
Although the central focus of this paper is a cost‐benefit analysis of the government compensation of kidney donors, it also provides as a side benefit a comparison of the cost‐effectiveness of dialysis and transplantation (see Supplement 10). In steady state, the cost of a QALY obtained through dialysis is $186 000, while the cost of a QALY obtained through transplantation is only $49 000, less than a third as much. Transplantation is clearly the more cost‐effective treatment for ESRD, as has been shown by other studies (e.g. Matas and Schnitzler 6).
Conclusions
The main conclusions of this analysis are that if the government successfully implements a kidney donor compensation program, the following would occur.
The lifetime value of a kidney transplant to a recipient would be very large—about $1.3 million per recipient. And the savings from stopping dialysis would be even larger—about $1.45 million per recipient.
In contrast, even a conservatively high $45 000‐per‐kidney cost of compensating kidney donors would be very small compared with the other costs and benefits. Indeed, the total cost of compensating all donors in a given year would be only about $2.6 billion per year. Yet this small cost is the key to unlocking the great welfare gains for transplant recipients and society, as well as the savings for the taxpayer.
The net welfare gain for society each year from kidney transplants would more than triple from $20 billion per year currently to $66 billion per year. This means the transplant community would be able to do three times as much good for society as it is currently doing. The ratio of benefits to costs for society would be a very large 3.0.
Having the government compensate kidney donors would even be a good deal for taxpayers considered alone. Because they currently bear most of the cost of both dialysis and kidney transplants, they would reap most of the benefits from more patients stopping expensive dialysis treatments after receiving a transplant. Taxpayers would save $403 000 for every dialysis patient who receives a kidney transplant. The aggregate savings for taxpayers would increase from $2.6 billion per year currently to $14.1 billion per year, and the benefit‐cost ratio for taxpayers would be a healthy 1.7.
It would also be an especially good deal for poor people considered alone because poor kidney recipients would gain the $1.3 million value of a longer and healthier life, but almost all of the costs of transplantation would be borne by the taxpayer through Medicare and Medicaid.
The bottom line of this analysis is that if the government compensated kidney donors, it would not only prevent 5000 to 10 000 premature deaths each year in the United States and substantially increase the quality of life for almost 100 000 patients on dialysis, but the benefits would greatly exceed the costs for both society in general and taxpayers and the poor in particular. One of the most surprising and important results of this paper is how large the welfare gain for society would be compared with the very small cost of compensating kidney donors.
We believe the estimates used in this paper are solidly based in the literature. But these are matters about which reasonable people can differ, so we invite others to offer their own numbers. Because the benefits of the government compensating kidney donors are so large and the cost of compensating donors is so small, we are confident that any reasonable estimates of these numbers will arrive at the same conclusion we did—that the benefits greatly exceed the costs.
Finally, we encourage those who oppose compensating kidney donors to place a monetary value on their concerns and to show how they outweigh the very large net benefits demonstrated by this analysis. If they do, they may discover—as we did in Supplement 6—that many of the arguments usually made against compensation of kidney donors turn out instead to be arguments in favor.
Disclosure
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Index of Supplements for: A Cost‐Benefit Analysis of Government Compensation of Kidney Donors
| No. | Name | Pg. No. |
|---|---|---|
| 1 | Important Footnotes for Main Text | 2–11 |
| 2 | Detailed Calculations of Costs and Benefits | 12–18 |
| 3 | Compensating Kidney Donors Would Be a Boon for the Poor | 19–21 |
| 4 | Comparison of Matas and Schnitzler with Held and McCormick et al. (this paper) | 22–23 |
| 5 | Estimates of Transplant and Dialysis Costs | 24–32 |
| 6 | Some Arguments Against Compensating Kidney Donors | 33–35 |
| 7 | Conservative Assumptions | 36–38 |
| 8 | Sensitivity Analyses | 39–44 |
| 1. Compensation | ||
| 2. Value of a QALY | ||
| 3. Quality of Life | ||
| 9 | Living vs. Deceased Donors Under a Donor Compensation Program | 45–46 |
| 10 | Cost of a Quality Adjusted Life Year: Dialysis vs. Transplantation | 47–48 |
| 11 | Capacity of U.S. Kidney Transplant Centers | 49 |
| 12 | Estimating Half‐Lives of Dialysis Patients, Transplant Patients, and Kidney Grafts | 50–66 |
Supporting information
Supporting Information
Acknowledgments
The authors want to thank Robert Heller, PhD, and Heywood Fleisig, PhD, who provided a careful reading of the paper at an early stage. Two editors and two reviewers of the American Journal of Transplantation supplied useful and thorough comments that greatly strengthened this work. Any remaining errors are the responsibility of the authors. The data and statistics reported here have been supplied by the USRDS and the SRTR. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government.
Held PJ, McCormick F, Ojo A & Roberts JP. A Cost‐Benefit Analysis of Government Compensation of Kidney Donors. Am J Transplant 2016; 16: 877–885.
References
- 1. Salomon DR, Langnas AN, Reed AI, et al; for the AST/ASTS Incentives Workshop Group (IWG). Meeting report, AST/ASTS Workshop on Increasing Organ Donation in the United States: creating an “arc of change” from removing disincentives to testing incentives. Am J Ttransplant 2015; 5: 1600–6143. [DOI] [PubMed] [Google Scholar]
- 2.Public Law 1984. Oct 19. Public Law 98‐507 NOTA. [PubMed]
- 3. Huang ES, Thakur N, Meltzer DO. The cost‐effectiveness of renal transplantation In Satel S, editor. When altruism isn't enough: the case for compensating kidney donors. Washington, DC: American Enterprise Institute for Public Policy Research; 2008. [Google Scholar]
- 4. Beard TR, Kaserman DL, Osterkamp R. The global organ shortage. Stanford University Press; 2013. [Google Scholar]
- 5. Becker GS, Elías JJ. Introducing incentives in the market for live and cadaveric organ donations. Journal of Economic Perspectives 2007; 21: 3–24. [DOI] [PubMed] [Google Scholar]
- 6. Matas AJ, Schnitzler M. Payment for living donor (vendor) kidneys: a cost‐effectiveness analysis. Am J Transplant 2003; 4: 216–221. [DOI] [PubMed] [Google Scholar]
- 7.US Renal Data System. USRDS 2013 annual data report: atlas of chronic kidney disease and end‐stage renal disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2013.
- 8.Scientific Registry of Transplant Recipients (SRTR). Annual data report, I. Kidney. Washington, DC: US Department of Health and Human Services, HRSA; 2012.
- 9. Viscusi WK, Aldy JE. The value of a statistical life: a critical review of market estimates throughout the world. J Risk Uncertainty 2003; 27: 1, 5–76. [Google Scholar]
- 10. Schold JD, Srinivas TR, Kayler LK, Meier‐Kriesche HU. The overlapping risk profile between dialysis patients listed and not listed for renal transplantation. Am J Transplant 2008; 8: 58–68. [DOI] [PubMed] [Google Scholar]
- 11. Hirth RA, Chernew ME, Miller E, Fendrick AM, Weissert WG. Willingness to pay for a quality‐adjusted life‐year: in search of a standard. Med Decis Making 2000; 20: 332–342. [DOI] [PubMed] [Google Scholar]
- 12. Whiting JF; for the Transplant Outcomes Research Group. Standards for economic and quality of life studies in transplantation. Transplantation 2000; 70: 1115–1121. [DOI] [PubMed] [Google Scholar]
- 13. Tolley G, Kenkel D, Fabian R, editors. Valuing health for policy: an economic approach. Chicago: University of Chicago Press; 1994. [Google Scholar]
- 14. Laupacis A, Keown P, Pus N, et al. A study of the quality of life and cost‐utility of renal transplantation. Kidney Int 1996; 50: 235–242. [DOI] [PubMed] [Google Scholar]
- 15. Russell JD, Beecroft ML, Ludwin D, Churchill DN. The quality of life in renal transplantation: a prospective study. Transplantation 1992; 54: 656–660. [DOI] [PubMed] [Google Scholar]
- 16. Hornberger JC, Best JH, Garrison LP Jr. Cost‐effectiveness of repeat medical procedures: kidney transplantation as an example. Med Decis Making 1997; 17: 363–372. [DOI] [PubMed] [Google Scholar]
- 17. Tanriover B, Stone PW, Mohan S, Cohen DJ, Gaston RS. Future of Medicare immunosuppressive drug coverage of kidney transplant recipients in the United States. Clin J Am Soc Nephrol 2013. April 4. doi:10.2215/CJN.09440912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Englesbe MJ, Ads Y, Cohn JA, et al. The effects of donor and recipient practices on transplant center finances. Am J Transplant 2008; 8: 586–592. [DOI] [PubMed] [Google Scholar]
- 19. Wolfe RA, McCullough KP, Schaubel DE, et al. Calculating life years from transplant (LYFT): methods for kidney and kidney‐pancreas candidates. Am J Transplant 2008; 8(Pt 2): 997–1011. [DOI] [PubMed] [Google Scholar]
- 20. Cook PJ, Krawiec K. A primer on kidney transplantation: anatomy of the shortage. Law Contemp Probl 2014; 77: 16–19. [Google Scholar]
- 21. Muzaale AD, Massie AB, Wang MC, et al. Risk of end‐stage renal disease following live kidney donation. JAMA 2014; 311: 579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hall MJ, Levant S, DeFrances CJ. Trends in inpatient hospital deaths: National Hospital Discharge Survey, 2000–2010. NCHS Data Brief No. 118, March 2013. [PubMed]
- 23. Lee CP, Chertow GM, Zenios SA. An empiric estimate of the value of life: Updating the Renal Dialysis Cost‐Effectiveness Standard. Value in Health 2008; 12: 80–87. [DOI] [PubMed] [Google Scholar]
- 24.DaVita Health Care Partners Inc. Form 10K filed with the U.S. Security and Exchange Commission for fiscal year ended 12 31 2012. Washington, DC: DaVita Health Care Partners Inc; 2012.
- 25.Fresenius Medical Care AG & Co. Form 20‐F Securities and Exchange Commission, Washington, D.C. 20549 and 2012 continuity corporate report. Bad Homburg, Germany: Fresenius Medical Care AG & Co; 2012.
- 26. Ghods AJ, Savaj S. Iranian model of paid and regulated living‐unrelated kidney donation. Clin J Am Soc Nephrol 2006; 1: 1136–1145. [DOI] [PubMed] [Google Scholar]
- 27. Mahdavi‐Mazdeh M. The Iranian model of living renal transplantation. Kidney Int 2012; 82: 627–634. [DOI] [PubMed] [Google Scholar]
- 28. Rana A, Gruessner A, Agopian VG, et al. Survival benefit of solid‐organ transplant in the United States. JAMA Surg 2015; 150: 3. [DOI] [PubMed] [Google Scholar]
- 29. Limou S, Nelson GW, Kopp JB, Winkler CA. APOL1 kidney risk alleles: population genetics and disease associations. Adv Chronic Kidney Dis 2014; 21: 426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meier‐Kriesche HU, Port FK, et al. Effect of waiting time on renal transplant outcome. Kidney Int 2000; 58: 1311–1317. [DOI] [PubMed] [Google Scholar]
- 31. Wetmore JB, Rigler SK, Mahnken JD, Mukhopadhyay P, Shireman TI. Considering health insurance: how do dialysis initiates with Medicaid coverage differ from persons without Medicaid coverage? Nephrol Dialysis Transplant 2010; 25: 198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Leighton T, Gustafson S, Snyder J, Israni A, Kasiske B. Changes in Medicare coverage after kidney transplant. Am J Transplant 2014; 14(Suppl 3): 848–849. Abstract D2750. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


