Abstract
Background
Patients with acute respiratory failure are at risk of deterioration during prehospital transport. Ventilatory support with continuous positive airway pressure (CPAP) can be initiated in the prehospital setting. The objective of the study is to evaluate adherence to treatment and effectiveness of CPAP as an addition to standard care.
Methods
In North Denmark Region, patients with acute respiratory failure, whom paramedics assessed as suffering from acute cardiopulmonary oedema, acute exacerbation of chronic obstructive pulmonary disease or asthma were treated with CPAP using 100 % O2 from 1 March 2014 to 3 May 2015. Adherence to treatment was evaluated by number of adverse events and discontinuation of treatment. Intensive care admissions and mortality were reported in this cohort. Effectiveness was evaluated by changes in peripheral oxygen saturation (SpO2) and respiratory rate during transport and compared to a historical control (non-CPAP) group treated with standard care only. Values were compared by hypothesis testing and linear modelling of SpO2 on arrival at scene and ΔSpO2 stratified according to treatment group.
Results
In fourteen months, 171 patients were treated with CPAP (mean treatment time 35 ± 18 min). Adverse events were reported in 15 patients (9 %), hereof six discontinued CPAP due to hypotension, nausea or worsening dyspnoea. One serious adverse event was reported, a suspected pneumothorax treated adequately by an anaesthesiologist called from a mobile emergency care unit. Among CPAP patients, 45 (27 %) were admitted to an intensive care unit and 24 (14 %) died before hospital discharge. The non-CPAP group consisted of 739 patients. From arrival at scene to arrival at hospital, CPAP patients had a larger increase in SpO2 than non-CPAP patients (87 to 96 % versus 92 to 96 %, p < 0.01) and a larger decrease in respiratory rate (32 to 25 versus 28 to 24 breaths/min, p < 0.01). In a linear model, CPAP was superior to non-CPAP in patients with initial SpO2 ≤90 % (p < 0.05). One CPAP patient (0.6 %) and eight non-CPAP patients (1.1 %) were intubated in the prehospital setting.
Discussion
The study design reflects the daily prehospital working environment including long transport timesand paramedics educated in treating symptoms of acute respiratory failure, rather than treating one specific diagnosis. The study population was included consecutively and few patients were lost to follow-up. However, the study was too small to allow assessment of any effect of prehospital CPAP on mortality, nor could the effectiveness in specific disease conditions be examined.
Conclusions
In an emergency medical service including physician backup, adherence to CPAP treatment administered by paramedics was high and treatment was effective in patients with acute respiratory failure.
Keywords: Noninvasive ventilation, Continuous positive airway pressure, CPAP, Dyspnea, Respiratory insufficiency, Prehospital, Emergency medical services, Paramedic
Background
Acute respiratory failure is one of the major causes of emergency department admission as reflected by the fact that 7.3 % of calls to the Danish emergency medical communication centres (EMCCs) have “difficulty in breathing” as the main symptom [1, 2]. Common causes of non-traumatic breathing difficulties include acute cardiopulmonary oedema, lower respiratory tract infections and acute exacerbation of chronic obstructive pulmonary disease (COPD) or asthma, which in severe cases may require non-invasive positive pressure ventilation or endotracheal intubation and mechanical ventilation. Non-invasive positive pressure ventilation administered in hospital reduces mortality in patients suffering from acute cardiopulmonary oedema or acute exacerbations of chronic obstructive pulmonary disease, while its effect in patients with acute exacerbations of asthma is uncertain [3–7]. Patients with acute respiratory failure have a risk of further deterioration during transport to hospital by emergency medical services (EMS). To prevent situations of such deterioration, prehospital initiation of continuous positive airway pressure (CPAP) has become available. CPAP is administered to patients with spontaneous breathing through a non-invasive facemask with a positive airway pressure applied during the entire respiratory cycle and it has been shown that prehospital CPAP reduces dyspnoea and respiratory rate when compared to standard medical therapy alone [8, 9]. In previous studies of patients treated with CPAP in the prehospital setting, reporting of adverse events have included either none at all, mask intolerance or minor complications such as hypotension, nausea or vomiting [9–17]. In three of four randomised controlled trials in prehospital settings, standard care plus CPAP reduced intubation rate compared to standard care alone [9, 13, 14, 18]. There have been conflicting results in recent systematic reviews including both randomised and observational studies regarding the effectiveness of prehospital CPAP on mortality in patients with acute respiratory failure [19–21]. Original research studies of CPAP in Nordic EMS systems are sparse; in a Finnish observational study from 2003, use of prehospital CPAP administered by physicians to patients with presumed acute severe pulmonary oedema improved oxygen saturation, respiratory rate, heart rate and systolic blood pressure [15]. In 2014, the EMS organisation in North Denmark Region decided to let paramedics administer CPAP to patients with non-traumatic acute respiratory failure. Introduction of prehospital CPAP was preceded by educational training including preparation of a clinical guideline. The aim of this study is to evaluate 1) adherence to prehospital CPAP treatment in patients with acute respiratory failure and 2) effectiveness of additional CPAP in comparison with standard care only.
Methods
Study design
The present study was performed in two steps; firstly, a prospective study of adherence to prehospital CPAP treatment in patients with acute respiratory failure, administered in addition to standard care (subsequently denoted “CPAP group”). Secondly, in an uncontrolled before and after study, measures of effectiveness were compared to a historical “non-CPAP” group of patients with symptoms of acute respiratory failure in the same geographical area, identified from a database of prehospital medical records. The primary objective was to evaluate adherence to prehospital CPAP treatment assessed by incidence of adverse events and discontinuation of CPAP treatment. The secondary objective was to evaluate effectiveness of prehospital CPAP in a post-hoc analysis, assessed by changes in peripheral capillary oxygen saturation (SpO2) and in respiratory rate upon treatment.
Setting
The regional EMS served 583,471 inhabitants in mixed rural and urban areas (7,933 km2) [22]. The EMS was structured as a three-tier system with 36 primary ambulances, five paramedic vehicles stationed in the rural areas and 24-h operative mobile emergency care units (MECUs) staffed by anaesthesiologists in two cities 54 km apart. On a daily basis, 130–150 patients were transported by the EMS to one of the three emergency departments in the region. Nurses operated the regional emergency medical communication centre by use of a Criteria Based Dispatch system, The Danish Index of Emergency Care [23]. Either the EMCC nurse or the EMS personnel on scene could request assistance from a MECU. Prior to the introduction of CPAP, paramedic supervisors completed a four-hour educational course on CPAP treatment conducted by an anaesthesiologist and a fellow doctor. The supervisors subsequently trained all paramedic squads for four hours. Additionally, comprehensive educational booklets on respiratory pathophysiology, indications, contraindications and practical handling were distributed to all paramedics including an overview action card. Whenever an EMCC nurse categorized a patient’s complaint as “difficulty in breathing”, one of the five paramedic vehicles equipped with disposable CPAP equipment was dispatched along with a primary ambulance. All EMS transport events were entered into a regional database, amPHITM, which included registrations of the patient’s respiratory status observed upon EMS arrival, of treatments administered, and of clinical observations and vital signs obtained during transport.
Participants
CPAP patients were included during the first 14 months after introduction of prehospital CPAP: 1 March 2014 to 3 May 2015. Selection criteria were all of the following three: 1) Patient age ≥18 years, 2) categorized by the EMCC nurse as having “difficulty in breathing” by use of The Danish Index of Emergency Care and 3) patient assessed by paramedics as suffering from acute exacerbation of COPD, asthma or acute cardiopulmonary oedema and treated with prehospital CPAP. Contraindications for initiation of CPAP treatment and reasons for discontinuing CPAP were as follows: Nausea or vomiting, reduced level of consciousness, respiratory fatigue, suspected pneumothorax on auscultation, hypotension (systolic blood pressure <90 mmHg), cranial or facial trauma, suspected stroke, foreign object in the airways, penetrating chest trauma, massive bleeding and epiglottitis.
In order to have a similar comparison group of adult patients with acute respiratory failure in the uncontrolled before and after study of effectiveness, we included non-CPAP patients from the regional EMS database, amPHITM from the previous 14 months prior to introduction of CPAP: 1 January 2013 to 28 February 2014. Non-CPAP selection criteria were all of the following three: 1) Patient age ≥18 years, 2) patient assessed by the arriving EMS personnel as having severe difficulty in breathing and 3) treated by the EMS with standard prehospital care which included high flow oxygen through a non-rebreathing facemask plus beta agonist and/or diuretics. In both study groups, pharmacological treatment was in some cases administered before arrival of the EMS, e.g. by the general practitioner who had called the EMCC. In both the CPAP and non-CPAP study groups, patients were included consecutively, including patients with repeated EMS transports during the intervention and control study periods.
Standard prehospital care and intervention
Standard prehospital care for acute respiratory failure consisted of proper positioning of the patient, high flow oxygen administered by Bag-Valve-Mask ventilation (with 100 % oxygen at a flow of 6–12 L/min) and, depending on the presumed aetiology, salbutamol inhalation, intravenous furosemide, sublingual nitroglycerine spray and/or intravenous fentanyl. The MECU physician could be consulted by telephone and be called to the scene in case non-invasive ventilation was insufficient or in case of acute deterioration to secure optimal treatment including endotracheal intubation. In the CPAP study period, paramedics were instructed to administer CPAP immediately as an additional treatment to the standard care. The Flow-Safe II EZ® CPAP System (©Mercury Medical®, Clearwater, Florida, USA (CE 0086)) provided high flow oxygen on a fixed level of 100 % and adjustable CPAP/PEEP in the range 0–13 cm H2O [24]. An integral nebulizer allowed administration of medications without disrupting the positive pressure applied. CPAP treatment was continued until arrival at hospital if no adverse events occurred or contraindications arose.
Variables and data collection
Prospective data collection included systematic recording of: Indication of CPAP treatment, the level of pressure applied, duration of CPAP treatment and any preterm discontinuation of CPAP, any adverse events, and any technical issues on a dedicated registration form. SpO2, systolic and diastolic blood pressures were monitored continuously by a LIFEPAK® 12-defibrillator/monitor (©Physio-Control, Inc., Redmond, Washington, USA). The prehospital database amPHITM provided information on demographics, paramedic assessment of the patient’s presumed cause of acute respiratory failure, pharmacological treatment, respiratory rate, endotracheal intubation, and transport times. For CPAP patients, number of days in hospital, intensive care unit (ICU) admission, in-hospital treatment with CPAP, non-invasive ventilation (NIV) or mechanical ventilation and mortality were collected from medical records via the regional Patient Administrative System. In the prospective study, the primary outcome measures were incidence of adverse events and discontinuation of CPAP treatment and secondary outcome measures included number of days in hospital, admissions to an ICU and in-hospital and 30 day mortality in CPAP patients. In the uncontrolled before and after study, changes in SpO2 and in respiratory rate measured upon arrival at scene and upon hospital arrival were primary outcome measures of effectiveness.
Statistical methods
As the primary objective was adherence to an additional treatment, no power calculations were done prior to the study. Data was entered in EpiData Version 3.1. Statistics were calculated using “R” version 3.2.0. Descriptive data are presented as mean (± standard deviation (SD)) or median (interquartile range (IQR)). Vital signs were compared by either two-sample t test or Mann-Whitney test according to the distribution of data and results presented with 95 % confidence intervals [95 % CI]. Proportions were compared by chi-square test or Fisher’s exact test as appropriate. The association between SpO2 on arrival at scene and ΔSpO2 was modelled by linear regression (Generalized Linear Models (package glm)) with adjustment for sex and age and stratified according to CPAP or non-CPAP group. Patients were categorized according to initial SpO2 and recorded values ≤70 % were excluded from the linear model, as LIFEPAK12 did not provide precise measures of SpO2 below this limit, according to the manufacturer [25]. Linearity of the association between initial SpO2 value and ΔSpO2 were visually assessed and accepted, as was the normal distribution of residuals. The ggplot2 package (smoothing method LOESS) was used for graphical presentation. Two-tailed p-values below 0.05 were considered significant.
Ethical approval
The Danish Data Protection Agency approved the study (record no. 2008-58-0028). According to The North Denmark Region Committee on Health Research Ethics, the study did not require ethical approval or collection of informed consent from the patients. The Danish Health Authority waived the requirement for patients to consent to have their medical records accessed by the researchers (3-3013-999/1/SABN).
Results
Adherence and adverse events related to prehospital CPAP treatment
Prehospital CPAP administration was adequately registered in 171 patients in the CPAP study period. Mean transport time from departure from scene to arrival at hospital was 27 (±12) min (N = 149, missing data in 22 patients). Paramedics administered CPAP treatment for ≤20 min in 42 cases, for 21–40 min in 78 cases and for more than 40 min in 48 cases and mean treatment time was 35 ± 18 min (N = 168, missing data in three patients). Adherence to treatment was 88 % (151/171) measured by the proportion of patients who continued CPAP treatment all the way to arrival at hospital. Reasons for discontinuation of CPAP treatment included intolerance to the facemask in eight patients, occurrence of an adverse event in six patients, prehospital intubation in one patient and unknown reasons in five patients. Overall, paramedics reported adverse events in 9 % (15/171) of the CPAP patients (Table 1).
Table 1.
Adverse events of prehospital CPAP treatment
| CPAP (N = 171) | |
|---|---|
| None | 156 |
| Hypotensionab | 4 |
| Hereof discontinued CPAP: 1 | |
| Nausea | 3 |
| Hereof discontinued CPAP: 3 | |
| Decrease in level of consciousnessc | 2 |
| Hereof discontinued CPAP: 0 | |
| Worsening dyspnoea | 2 |
| Hereof discontinued CPAP: 1 | |
| Suspected pneumothorax | 1 |
| Hereof discontinued CPAP: 1 | |
| Tachycardia | 1 |
| Coughing mucus | 1 |
| Dry nose and/or mouth | 1 |
No missing data
CPAP continuous positive airway pressure
aSystolic blood pressure ≤90 mmHg
bNone of the 4 cases were below 80 mmHg
cGlasgow Coma Scale from 15 to 14
In addition to the fifteen listed adverse events, five patients experienced a critical decrease in SpO2 during prehospital transport: from 92 to 86 %, from 97 to 91 %, from 87 to 80 %, from 93 to 85 % and from 94 to 71 %, respectively (N = 158, missing data in 13 patients). The latter of the cases was a patient with pulmonary sarcoidosis, in which SpO2 decreased markedly even before initiation of CPAP and a MECU was called to the scene. The attending anaesthesiologist suspected a pneumothorax and performed an ultrasound examination of the lungs. CPAP was discontinued and the anaesthesiologist performed a needle decompression, which resulted in audible escape of air from pleura, ease of breathing and immediate improvement in SpO2 from 71 % to 95 %. As previously described, discontinuation of CPAP before arrival at hospital due to an adverse event occurred in this and five more patients; three due to nausea, one due to hypotension and one due to worsening dyspnoea. The latter patient developed shallow breathing during transport, CPAP treatment was discontinued and replaced by Bag-Valve-Mask ventilation and the breathing pattern was normalised.
In-hospital outcomes in CPAP treated patients
During hospital stay, 64 % (107/168) of patients in the CPAP group received no in-hospital ventilation support in the form of CPAP, NIV and/or mechanical ventilation. Twenty-seven percent of the patients (45/168) in the CPAP group were transferred to an ICU. Overall, in-hospital mortality was 14 % (24/168). Among ICU admitted patients, in-hospital mortality was 24 % (11/45) (Table 2).
Table 2.
In-hospital outcomes in CPAP treated patients
| CPAP (N = 168) | |
|---|---|
| Days in hospital, median (IQR) | 5.5 (3.0–9.0) |
| Admitted to ICU, N (%) | 45 (27 %) |
| Mortality | |
| In-hospital, all patients, N (%) | 24 (14 %) |
| In-hospital, ICU patients, N (%) | 11 (24 %) |
| 30 daysa, N (%) | 36 (24 %) |
No missing data
CPAP continuous positive airway pressure, ICU intensive care unit, IQR interquartile range
aBased on first time events only (N = 153)
The most frequent diagnoses among patients who died in hospital were acute exacerbation of COPD, lower airway tract infections and sepsis.
Patient characteristics in CPAP versus non-CPAP groups in the prehospital setting
The CPAP group consisted of 171 patients and 739 patients met the criteria for inclusion in the non-CPAP group (Fig. 1). The proportion of males was higher in the CPAP group, while the distribution of age was similar (Table 3).
Fig. 1.
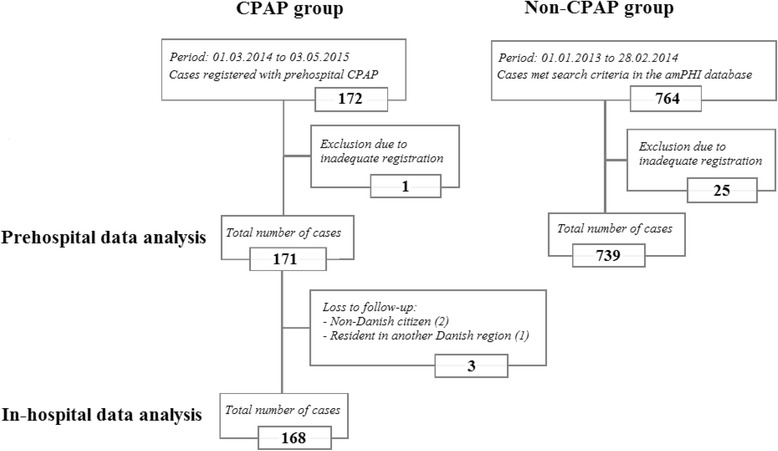
Study population flowchart
Table 3.
Patient demographics and presumed cause of ARF assessed by the EMS
| CPAP (N = 171) | Non-CPAP (N = 739) | ρ-value | |
|---|---|---|---|
| Patient demographics | |||
| Male, % | 60 % | 50%a | 0.02 |
| Age, years, median (IQR) | 73 (64–80) | 74 (64–81)b | 0.99 |
| Presumed cause of ARF | |||
| Acute cardiopulmonary oedema | 18.1 % | 13.3 % | 0.10c |
| Asthma, acute exacerbation | 5.3 % | 7.3 % | 0.34c |
| COPD, acute exacerbation | 57.3 % | 45.5 % | 0.01c |
| Combined COPD and acute cardiopulmonary oedema | 2.3 % | 3.4 % | 0.63d |
| Combined COPD and asthma | 1.2 % | 4.2 % | 0.07d |
| Other | 12.9 % | 14.2 % | 0.65c |
| Unknown or not reported | 2.9 % | 12.2 % | <0.01d |
No missing data unless otherwise stated
ARF acute respiratory failure, COPD chronic obstructive pulmonary disease, CPAP continuous positive airway pressure, EMS emergency medical services, IQR interquartile range
a N = 716
b N = 704
cCalculated by chi-square test
dCalculated by Fisher’s exact test
Presumed causes of acute respiratory failure assessed by the EMS varied between the two study groups; acute exacerbation of COPD and acute cardiopulmonary oedema were more frequently reported in the CPAP group whereas unknown causes were more frequent in the non-CPAP group (Table 3). Amongst “other” causes were e.g. unspecified dyspnoea, angina pectoris, allergic reactions and unconsciousness. On arrival at scene, patients in the CPAP group had a lower SpO2 (87 % versus 92 %) and a higher respiratory rate (32 breaths/min versus 28 breaths/min) than non-CPAP patients, while blood pressures were similar (Table 4).
Table 4.
Vital signs recorded upon arrival at scene and arrival at hospital
| CPAP | Non-CPAP | ρ-value | |
|---|---|---|---|
| Status on arrival at scene | |||
| SpO2, % | 87 (77–94) | 92 (85–97) | <0.01 |
| (N = 159) | (N = 723) | ||
| Respiratory rate, breaths/min | 32 (28–38) | 28 (24–32) | <0.01 |
| (N = 163) | (N = 692) | ||
| Systolic blood pressurea, mmHg | 157 (± 34) | 155 (± 33) | 0.51 |
| (N = 159) | (N = 704) | ||
| Diastolic blood pressurea, mmHg | 92 (± 24) | 93 (± 24) | 0.93 |
| (N = 145) | (N = 704) | ||
| Status on arrival at hospital | |||
| SpO2, % | 96 (94–99) | 96 (91–98) | 0.02 |
| (N = 168) | (N = 715) | ||
| Respiratory rate, breaths/min | 25 (21–30) | 24 (21–30) | 0.67 |
| (N = 163) | (N = 550) | ||
| Systolic blood pressurea, mmHg | 140 (± 25) | 142 (± 30) | 0.25 |
| (N = 156) | (N = 679) | ||
| Diastolic blood pressurea, mmHg | 85 (± 19) | 86 (± 24) | 0.59 |
| (N = 145) | (N = 676) | ||
Data presented as median (IQR) unless otherwise stated
CPAP continuous positive airway pressure, IQR interquartile range, SD standard deviation, SpO 2 peripheral capillary oxygen saturation
amean (± SD)
Effectiveness of prehospital CPAP versus non-CPAP treatment
During transport, CPAP patients had a larger median increase in SpO2 compared to non-CPAP patients (8 percentage points versus 2 percentage points, p < 0.01, 95 % CI [4, 7]) (CPAP group: N = 158, non-CPAP group: N = 712). Increases in SpO2 were higher the lower the initial SpO2 value as demonstrated in Fig. 2, and this pattern was unaffected by adjustment for sex and age (Table 5).
Fig. 2.
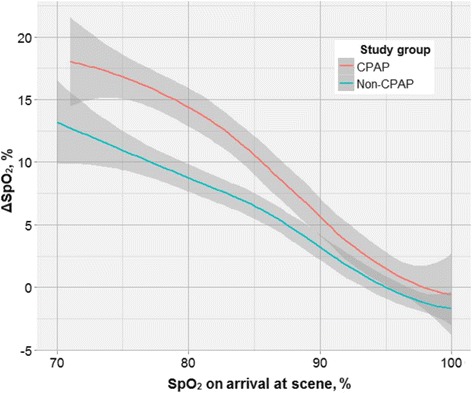
Changes in SpO2 from arrival at scene to arrival at hospital as a function of initial SpO2 value and according to study group. Grey areas represent 95 % confidence limits. Number of points: 30. CPAP group: N = 136. Non-CPAP group: N = 663
Table 5.
Changes in SpO2 during transport to hospital
| SpO2 on arrival at scene | ||||||
|---|---|---|---|---|---|---|
| 71–80 % | 81–90 % | >90 % | ||||
| CPAP | Non-CPAP | CPAP | Non-CPAP | CPAP | Non-CPAP | |
| Unadjusted | +16.2* | +9.4* | +9.8* | +5.9* | +1.5 | 0 |
| Adjusted for sex and age | +16.5* | +9.2* | +9.9* | +6.0* | +1.6 | −0.1 |
Changes in SpO2 from arrival at scene to arrival at hospital according to initial SpO2 value and study group
CPAP group: N = 136. Non-CPAP group: N = 663
CPAP continuous positive airway pressure, SpO 2 peripheral capillary oxygen saturation
*p < 0.05
In this linear model, initial SpO2 ≤70 % were excluded due to imprecision of the measuring device; 23 in the CPAP group and 60 in the non-CPAP group. The decrease in respiratory rate was larger among CPAP patients than among non-CPAP patients; a median decrease of 8 breaths/min versus 2 breaths/min, respectively (p < 0.01, 95 % CI [−5, −3]) (CPAP group: N = 162, non-CPAP group: N = 539). On arrival at hospital, SpO2 (CPAP 96 % versus non-CPAP 96 %) and respiratory rate (CPAP 25 breaths/min versus non-CPAP 24 breaths/min) did not differ between the study groups (Table 4). Lowest respiratory rate after CPAP treatment was 11 breaths per minute.
Concurrent prehospital management in CPAP versus non-CPAP groups
Use of concurrent pharmacological treatments varied between the two study groups (Table 6); a larger proportion of patients in the CPAP group received furosemide, fentanyl and nitroglycerine than in the non-CPAP group, while a smaller proportion received salbutamol. One patient (0.6 %) in the CPAP group and eight patients (1.1 %) in the non-CPAP group were intubated before arrival at hospital (missing data in 0 patients).
Table 6.
Prehospital pharmacological treatment
| CPAP (N = 171) | Non-CPAP (N = 739) | ρ-value | |
|---|---|---|---|
| Intravenous | |||
| Furosemide, N (%) | 50 (29 %) | 152 (21 %) | 0.01 |
| Fentanyl, N (%) | 29 (17 %) | 88 (12 %) | 0.08 |
| Sublingual spray | |||
| Nitroglycerine, N (%) | 46 (27 %) | 140 (19 %) | 0.02 |
| Inhalation | |||
| Salbutamol, N (%) | 108 (63 %) | 589 (80 %) | <0.01 |
No missing data
CPAP continuous positive airway pressure
Discussion
In this prospective study of prehospital CPAP to patients with acute respiratory failure, adherence to treatment was high as 88 % of all patients were treated with CPAP during the entire transport from scene to hospital. Adverse events were minor, except for one serious event, a pneumothorax. CPAP as a supplement to standard care was associated with larger improvements in SpO2 and respiratory rate compared to a historical cohort of patients treated with standard care alone.
Adherence to treatment
CPAP is used in-hospital to treat patients with acute cardiopulmonary oedema, but is not recommended for acute exacerbations of COPD or asthma. Previous studies of prehospital CPAP treatment with cohorts of 60–149 patients with acute cardiogenic pulmonary oedema have not reported any serious adverse events [9–15]. Williams et al. reported that only 41 % of patients, who were coded as acute pulmonary oedema by a paramedic had this particular emergency department discharge diagnosis [26]. Accordingly, a CPAP protocol restricted to patients with presumed acute cardiopulmonary oedema is likely to be started even if the patient is suffering from acute respiratory failure from a different aetiology. In our study, we investigated if CPAP was safe to use in prehospital patients with acute respiratory failure from either acute cardiopulmonary oedema, acute exacerbation of COPD or asthma. Prehospital data collection including potential adverse events was planned prospectively, which made paramedics consistently assess and report any adverse events, minor as well as serious. Potential serious adverse events of prehospital CPAP treatment include apnoea, therapy failure in cardiogenic shock for example due to acute myocardial infarction and risk of either resulting in a pneumothorax or worsening an existing one [27, 28]. In the present study, no patients developed a systolic blood pressure <80 mmHg as an indication of impaired cardiac function. Likewise, no patients developed apnoea, yet two patients experienced worsening dyspnoea upon treatment with CPAP. We consider it likely, that the one serious adverse event of a pneumothorax in our cohort was due to or worsened by CPAP. A similar adverse event has been reported in a case series study, where one patient had failed prehospital CPAP and a pneumothorax was discovered following intubation and mechanical ventilation in the emergency department [29]. In five cases in our study, SpO2 actually decreased upon CPAP treatment, indicating a worsening of the condition. All adverse events of CPAP treatment in the present study was managed and treated adequately in the prehospital setting with shift to standard care or assistance from a physician staffed MECU. These cases illustrate how CPAP may be administered inadvertently to a patient, whose final diagnosis is different than presumed by paramedics. Our results demonstrate, that CPAP treatment is feasible in a prehospital setting, where time is limited and differentiation between cardiogenic, pulmonary and other aetiologies of acute respiratory failure is difficult. The results also emphasize the need for caution and frequent reassessment of the patient’s SpO2 and clinical condition during CPAP treatment and call for physician assistance to manage any complications.
Effectiveness
The present study was too small to allow assessment of any effect of prehospital CPAP on mortality, nor could the effectiveness of CPAP treatment in specific disease conditions be examined. The study design, however, reflects the daily prehospital working environment, in which EMS personnel generally do not give specific diagnoses before considering how to treat the patient, and on average respiratory parameters improved in our study population. As expected from the oxygen-haemoglobin dissociation curve, the effectiveness of treatment on SpO2 reported in this study diminished with increasing initial SpO2 values (>90 %), which should be taken into consideration when planning future studies. Measures of gas exchange would have been valuable to the study. Originally, registration of end-tidal CO2 was mandatory; however, the variable was dropped as the patients’ CO2 were diluted from the high gas flow in the CPAP system. Development of respiratory acidosis as an outcome measure was not applicable in this study as the patients’ arterial gas samples were not routinely entered in to the patients’ electronic medical records. In future studies, arterial gas sampling will be a useful outcome measure. Addition of prehospital CPAP to medical therapy improved SpO2 and respiratory rate in patients with acute respiratory failure in several observational studies [16, 27, 28]. Comparison of standard medical therapy plus CPAP to standard medical therapy alone has shown, that CPAP is superior when using SpO2 or respiratory rate as outcome measures of effectiveness in patients with acute cardiopulmonary oedema or acute respiratory failure [10, 12, 17]. Two recent studies of prehospital patients with respiratory distress, conducted in North American urban settings, did not find any benefit of CPAP when comparing groups before and after implementation [30, 31]. The study protocols aimed at patients with presumed heart failure, COPD or asthma and the study patients’ initial oxygen saturation and respiratory rate were comparable to initial values in this study population. Transport time from departure from scene to arrival at emergency department was considerably shorter than in the present study, only 9.6 min [30]. Distance and transport time to hospital is an important factor when deciding how to treat patients with acute respiratory failure during ambulance transport; it is always a balance between time used to initiate a prehospital treatment and a faster arrival to definitive treatment at hospital. Our study showed that CPAP was effective in an EMS system with a mean treatment time of 35 min, reflecting the relatively long transport times in the region. In the prehospital setting, oxygen therapy should be given cautiously; high flow oxygen has been associated with increased mortality compared to titrated oxygen treatment in patients with presumed acute exacerbation of COPD [32]. In both our study groups, the high concentration of oxygen may have removed nitrogen from the alveoli and subsequently induced absorption atelectasis and it may also have led to hypercapnia in oxygen sensitive COPD patients. We presume that no patients experienced severe hyperoxaemia and/or severe hypercapnia in our study, since the two examples of decrease in level of consciousness were minor and respiratory rate did not decrease below 11 breaths per minute following CPAP treatment. Moreover, in acute myocardial infarction, prehospital oxygen therapy has been associated with larger myocardial infarct size compared to no oxygen therapy in patients with acute ST-elevation myocardial infarction and no hypoxia [33]. Lower fractional oxygen with CPAP improved oxygen saturation and respiratory rate in patients with acute respiratory failure in previous observational studies [17, 27]. Nonetheless, both our study groups were treated with 100 % oxygen as titrated oxygen treatment was not yet possible in the region’s ambulances.
Strengths and limitations
Strengths of the present study include a population based and consecutive sample of 171 patients treated with CPAP in daily prehospital practice, and few patients were lost to follow-up. External validity of this observational study is regarded as high in countries with similar disease patterns and EMS structures. The study design contains limitations; retrospective data collection from the historical non-CPAP group, risk of regression to the mean value and obvious confounding in the form of concurrent pharmacological treatment. No changes, apart from addition of CPAP trough a tight facemask, were made to EMS treatment for acute respiratory failure across the two study periods. Nevertheless, concurrent pharmacological treatments varied between study groups, probably due to differences in the case mix between the two groups, and though differences were small, the impact on our results is unknown. During the CPAP study period, inclusion was limited to cases, in which a paramedic vehicle was available and dispatched, causing a selection bias. In the study design, the individual paramedic both served as treatment provider and data collector by which observer bias was induced. We cannot estimate the impact of case mix differences that were not included in the linear model, e.g. presumed pathology, initial respiratory rate or any bias resulting from the varying selection criteria of patients in the two study groups. Due to above mentioned limitations, the presented results ought to be interpreted as exploratory results. As patients with initial SpO2 values ≤70 % were excluded from both treatment groups due to imprecise measurement, we are not able to conclude on effectiveness of CPAP in patients with SpO2 values below this limit.
Conclusions
In a three-tier EMS system including on-call physician backup, adherence to prehospital CPAP treatment administered by paramedics was high in patients with acute respiratory failure. Few adverse events were reported, including one potentially serious adverse event averted by a rendezvous physician. Patients treated with standard care plus CPAP experienced larger increases in SpO2 and reduced respiratory rate during prehospital transport compared to a historical cohort of patients treated with standard care only. The study is useful in future trial planning and for EMS systems intending to implement prehospital CPAP. Randomised studies are required to demonstrate short-term and long-term effects of prehospital CPAP including effects of low versus high flow oxygen.
Acknowledgements
The authors thank Poul Anders Hansen and Flemming Bøgh Jensen from Prehospital Emergency Medical Services, North Denmark Region, Aalborg, Denmark and paramedics from Falck Denmark for their cooperation and participation in the study.
Funding
The professorship of EFC is supported by an unrestricted grant to Aalborg University, Denmark from the non-profit organisation TrygFonden. VN received a research grant from Aalborg University, Denmark. KL was employed at the Prehospital Care Organisation, North Denmark Region. The remaining authors had departmental funding only.
Availability of data and material
The datasets will not be shared as they contain a direct identifier (date of birth) and several indirect identifiers (place of treatment, sex, anthropometry measures, age).
Authors’ contributions
JM, KL and AA organised training sessions for paramedic supervisors and emergency department personnel. All authors participated in the design and writing of the study protocol. VN collected data and performed statistical analysis in collaboration with APTP. VN drafted the manuscript, and all authors read and approved the final edition.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
According to The North Denmark Region Committee on Health Research Ethics, the study did not require ethical approval or collection of informed consent from the patients. The Danish Health Authority waived the requirement for patients to consent to have their medical records accessed by the researchers (3-3013-999/1/SABN).
Abbreviations
- amPHITM
Ambulance pre-hospital intervention (trademark)
- COPD
Chronic obstructive pulmonary disease
- CPAP
Continuous positive airway pressure
- EMCC
Emergency medical communication centre
- EMS
Emergency medical services
- ICU
Intensive care unit
- MECU
Mobile emergency care unit
- NIV
Non-invasive ventilation
- PEEP
Positive end-expiratory pressure
- SpO2
Peripheral capillary oxygen saturation
Contributor Information
Vibe Maria Laden Nielsen, Email: vibe.n@rn.dk.
Jacob Madsen, Email: jama@rn.dk.
Anette Aasen, Email: a_aasen@hotmail.com.
Anne Pernille Toft-Petersen, Email: aptp@rn.dk.
Kenneth Lübcke, Email: k.lubcke@rn.dk.
Bodil Steen Rasmussen, Email: bodil.steen.rasmussen@rn.dk.
Erika Frischknecht Christensen, Email: efc@rn.dk.
References
- 1.Ray P, Birolleau S, Lefort Y, Becquemin M-H, Beigelman C, Isnard R, Teixeira A, Arthaud M, Riou B, Boddaert J. Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Crit Care. 2006;10:R82. doi: 10.1186/cc4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersen MS, Johnsen SP, Sørensen JN, Jepsen SB, Hansen JB, Christensen EF. Implementing a nationwide criteria-based emergency medical dispatch system: A register-based follow-up study. Scand J Trauma Resusc Emerg Med. 2013;21:53. doi: 10.1186/1757-7241-21-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vital FMR, Ladeira MT, Atallah AN. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2013;5:CD005351. doi: 10.1002/14651858.CD005351.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Masip J, Roque M, Sánchez B, Fernández R, Subirana M, Expósito JA. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA. 2005;294:3124–30. doi: 10.1001/jama.294.24.3124. [DOI] [PubMed] [Google Scholar]
- 5.Winck JC, Azevedo LF, Costa-Pereira A, Antonelli M, Wyatt JC. Efficacy and safety of non-invasive ventilation in the treatment of acute cardiogenic pulmonary edema - a systematic review and meta-analysis. Crit Care. 2006;10:R69. doi: 10.1186/cc4905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ram FSF, Wellington S, Rowe B, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst Rev. 2005;3:CD004360. doi: 10.1002/14651858.CD004360.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Ram FSF, Picot J, Lightowler J, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2004;3:CD004104. doi: 10.1002/14651858.CD004104.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Mattera C. Positive Pressure: The physiology of respirations with CPAP. J Emerg Med Serv. 2011;Suppl 1:6–10. [Google Scholar]
- 9.Plaisance P, Pirracchio R, Berton C, Vicaut E, Payen D. A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: Physiological and clinical effects. Eur Heart J. 2007;28:2895–2901. doi: 10.1093/eurheartj/ehm502. [DOI] [PubMed] [Google Scholar]
- 10.Dib JE, Matin SA, Luckert A. Prehospital use of continuous positive airway pressure for acute severe congestive heart failure. J Emerg Med. 2012;42:553–8. doi: 10.1016/j.jemermed.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Foti G, Sangalli F, Berra L, Sironi S, Cazzaniga M, Rossi GP, Bellani G, Pesenti A. Is helmet CPAP first line pre-hospital treatment of presumed severe acute pulmonary edema? Intensive Care Med. 2009;35:656–62. doi: 10.1007/s00134-008-1354-7. [DOI] [PubMed] [Google Scholar]
- 12.Hubble MW, Richards ME, Jarvis R, Millikan T, Young D. Effectiveness of Prehospital Continuous Positive Airway Pressure in the Management of Acute Pulmonary Edema. Prehospital Emerg Care. 2006;10:430–9. doi: 10.1080/10903120600884848. [DOI] [PubMed] [Google Scholar]
- 13.Ducros L, Logeart D, Vicaut E, Henry P, Plaisance P, Collet JP, Broche C, Gueye P, Vergne M, Goetgheber D, Pennec PY, Belpomme V, Tartière JM, Lagarde S, Placente M, Fievet ML, Montalescot G, Payen D. CPAP for acute cardiogenic pulmonary oedema from out-of-hospital to cardiac intensive care unit: A randomised multicentre study. Intensive Care Med. 2011;37:1501–9. doi: 10.1007/s00134-011-2311-4. [DOI] [PubMed] [Google Scholar]
- 14.Frontin P, Bounes V, Houzé-Cerfon CH, Charpentier S, Houzé-Cerfon V, Ducassé JL. Continuous positive airway pressure for cardiogenic pulmonary edema: a randomized study. Am J Emerg Med. 2011;29:775–81. doi: 10.1016/j.ajem.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Kallio T, Kuisma M, Alaspää A, Rosenberg PH. The use of prehospital continuous positive airway pressure treatment in presumed acute severe pulmonary edema. Prehosp Emerg Care. 2003;7:209–13. doi: 10.1080/10903120390936798. [DOI] [PubMed] [Google Scholar]
- 16.Cheskes S, Turner L, Thomson S, Aljerian N. The Impact of Prehospital Continuous Positive Airway Pressure on the Rate of Intubation and Mortality from Acute Out-of-hospital Respiratory Emergencies. Prehospital Emerg Care. 2013;17:435–41. doi: 10.3109/10903127.2013.804138. [DOI] [PubMed] [Google Scholar]
- 17.Garuti G, Bandiera G, Cattaruzza MS, Gelati L, Osborn JF, Toscani S, Confalonieri M, Lusuardi M. Out-of-hospital helmet CPAP in acute respiratory failure reduces mortality: a study led by nurses. Monaldi Arch Chest Dis. 2010;73:145–51. doi: 10.4081/monaldi.2010.283. [DOI] [PubMed] [Google Scholar]
- 18.Thompson J, Petrie DA, Ackroyd-Stolarz S, Bardua DJ. Out-of-Hospital Continuous Positive Airway Pressure Ventilation Versus Usual Care in Acute Respiratory Failure: A Randomized Controlled Trial. Ann Emerg Med. 2008;52:232–41. doi: 10.1016/j.annemergmed.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 19.Williams TA, Finn J, Perkins GD, Jacobs IG. Prehospital continuous positive airway pressure for acute respiratory failure: a systematic review and meta-analysis. Prehosp Emerg Care. 2013;17:261–73. doi: 10.3109/10903127.2012.749967. [DOI] [PubMed] [Google Scholar]
- 20.Bakke SA, Botker MT, Riddervold IS, Kirkegaard H, Christensen EF. Continuous positive airway pressure and noninvasive ventilation in prehospital treatment of patients with acute respiratory failure: a systematic review of controlled studies. Scand J Trauma Resusc Emerg Med. 2014;22:69. doi: 10.1186/s13049-014-0069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandor A, Thokala P, Goodacre S, Poku E, Stevens JW, Ren S, Cantrell A, Perkins GD, Ward M, Penn-Ashman J. Pre-hospital non-invasive ventilation for acute respiratory failure: a systematic review and cost-effectiveness evaluation. Health Technol Assess. 2015;19(42):1–102. [DOI] [PMC free article] [PubMed]
- 22.Population in Denmark 2015Q3 by Statistics Denmark. https://www.dst.dk/en/Statistik/emner/befolkning-og-befolkningsfremskrivning/folketal. Accessed 29 Jan 2016.
- 23.Danske Regioner . Dansk Indeks for Akuthjælp - Version 1.4. 2013. [Google Scholar]
- 24. ©Mercury Medical®. Only One Flow-Safe II Disposable CPAP Systems Flow-Safe Tubing Kit. 2014.
- 25.© 2008-2011 Physio-Control, Inc. Instruction manual for LIFEPAK 12-defibrillator/monitor. 2011.
- 26.Williams TA, Finn J, Celenza A, Teng T-H, Jacobs IG. Paramedic identification of acute pulmonary edema in a metropolitan ambulance service. Prehosp Emerg Care. 2013;17:339–47. doi: 10.3109/10903127.2013.773114. [DOI] [PubMed] [Google Scholar]
- 27.Bledsoe BE, Anderson E, Hodnick R, Johnson L, Johnson S, Dievendorf E. Low-fractional oxygen concentration continuous positive airway pressure is effective in the prehospital setting. Prehosp Emerg Care. 2011;16:217–21. doi: 10.3109/10903127.2011.640765. [DOI] [PubMed] [Google Scholar]
- 28.Luiz T, Kumpch M, Grüttner J, Madler C, Viergutz T. Prehospital CPAP Therapy by Emergency Physicians in Patients with Acute Respiratory Failure due to Acute Cardiogenic Pulmonary Edema or Acutely Exacerbated COPD. In Vivo. 2016;30(2):133–9. [PubMed] [Google Scholar]
- 29.Kosowsky JM, Stephanides SL, Branson RD, Sayre MR. Prehospital use of continuous positive airway pressure (CPAP) for presumed pulmonary edema: a preliminary case series. Prehosp Emerg Care. 2001;5(2):190–6. doi: 10.1080/10903120190940119. [DOI] [PubMed] [Google Scholar]
- 30.Willmore A, Dionne R, Maloney J, Ouston E, Stiell I. Effectiveness and safety of a prehospital program of continuous positive airway pressure (CPAP) in an urban setting. CJEM. 2015;17:609–16. doi: 10.1017/cem.2014.60. [DOI] [PubMed] [Google Scholar]
- 31.Aguilar SA, Lee J, Castillo E, Lam B, Choy J, Patel E, Pringle J, Serra J. Assessment of the Addition of Prehospital Continuous Positive Airway Pressure (CPAP) to an Urban Emergency Medical Services (EMS) System in Persons with Severe Respiratory Distress. J Emerg Med. 2013;45:210–9. doi: 10.1016/j.jemermed.2013.01.044. [DOI] [PubMed] [Google Scholar]
- 32.Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ. 2010;341:c5462. doi: 10.1136/bmj.c5462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray JE, Cameron P, Barger B, Ellims AH, Taylor AJ, Meredith IT, Kaye DM, AVOID Investigators Air Versus Oxygen in ST-Segment-Elevation Myocardial Infarction. Circulation. 2015;131:2143–50. doi: 10.1161/CIRCULATIONAHA.114.014494. [DOI] [PubMed] [Google Scholar]


