Abstract
Background/Aim
MR is an important complication after PMV. Transthoracic echocardiography is widely used to screen for native MR, but can be limited with PMV. Cine-CMR holds potential to non-invasively assess regurgitant severity based on MR-induced inter-voxel dephasing. This study evaluated routine cine-CMR for visual assessment of prosthetic mitral valve (PMV) associated mitral regurgitation (MR).
Methods
Routine cine-CMR was performed at 9 sites. A uniform protocol was used to grade MR based on jet size in relation to the left atrium (mild <1/3, moderate 1/3–2/3, severe >2/3): MR was graded in each long axis orientation, with overall severity based on cumulative grade. Cine-CMR was also scored for MR density and pulmonary vein systolic flow reversal (PSFR). Visual interpretation was compared to quantitative analysis in a single center (derivation) cohort, and to transesophageal echocardiography (TEE) in a multicenter (validation) cohort.
Results
The population comprised 85 PMV patients (59% mechanical, 41% bioprosthetic). Among the derivation cohort (n=25), quantitative indices paralleled visual scores, with stepwise increases in jet size and density in relation to visually graded MR severity (both p=0.001): Patients with severe MR had nearly a 3-fold increase in quantitative jet area (p=0.002), and 2-fold increase in density (p=0.04) than did others. Among the multicenter cohort, cine-CMR and TEE (Δ=2±3 days) demonstrated moderate agreement (κ=0.44); 64% of discordances differed by ≤ 1 grade (Δ=1.2±0.5). Using a TEE reference, cine-CMR yielded excellent diagnostic performance for severe MR (sensitivity, negative predictive value=100%). Patients with visually graded severe MR also had more frequent PVSFR (p<0.001), denser jets (p<0.001), and larger left atria (p=0.01) on cine-CMR.
Conclusions
Cine-CMR is useful for assessment of PMV-associated MR, which manifests concordant quantitative and qualitative changes in size and density of inter-voxel dephasing. Visual MR assessment based on jet size provides an accurate non-invasive means of screening for TEE-evidenced severe MR.
Keywords: CMR, mitral regurgitation, echocardiography
Introduction
Mitral regurgitation (MR) is an important complication that can occur after prosthetic mitral valve (PMV) replacement, conferring increased risk for heart failure and arrhythmias. Despite advanced surgical techniques, MR can recur following both mechanical and bioprosthetic valve replacement.1, 2 Accurate diagnosis impacts clinical care of PMV patients, as severe MR constitutes a potentially treatable cause of clinical symptoms. However, whereas transthoracic echocardiography (TTE) is widely used as a screening test for MR in patients with native mitral valves, it can be limited in the evaluation of PMV due to prosthesis-associated image artifacts.3–5 Transesophageal echocardiography (TEE) provides incremental utility over transthoracic imaging,6 but is invasive and thus not well suited for screening purposes. Approximately 100,000 mitral valve prostheses are implanted annually in the United States,7 a number which may further increase due to both growing prevalence of native mitral regurgitation and advances in surgical techniques.8, 9 Thus, improved non-invasive imaging methods for assessment of PMV-associated MR is of substantial clinical importance.
Cardiac magnetic resonance (CMR) offers several different approaches for MR assessment. Phase velocity encoded imaging enables flow quantification, and can be used to measure MR.10, 11 However, this approach requires dedicated imaging with additional breath-holds that can be challenging for patients with heart failure and/or advanced MR. Additionally, translational valve motion and regurgitant jet eccentricity can contribute to inaccurate quantification by conventional phase velocity encoded imaging.12 Cine-CMR provides an alternative approach, whereby MR can be graded based on extent of regurgitation-associated inter-voxel de-phasing.13–17 As cine-CMR is a standard component of nearly all exams, this approach holds particular appeal as a simple means of visually screening for MR so as to identify patients with substantial regurgitation who warrant further dedicated imaging for MR quantification. To date, performance of routine cine-CMR for prosthesis-associated MR has not been evaluated.
The aims of this study were two-fold: First, to compare cine-CMR evidenced qualitative and quantitative indices of MR severity among patients with PMV. Second, to test diagnostic performance of a simple visual scoring system for PMV-associated MR in relation to a reference standard of TEE.
Methods
Population
The study population was comprised of patients with PMV undergoing routine clinical cine-CMR. A standardized protocol for assessment of MR severity was developed in a single center (derivation) cohort, consisting of consecutive patients with PMV undergoing CMR at a designated data coordination center (Weill Cornell Medical College). In this cohort, qualitative visual cine-CMR interpretation was compared to quantitative indices.
The visual cine-CMR interpretation protocol was further tested in a multicenter (validation) cohort, consisting of patients undergoing CMR and echocardiography between 3/2005 and 1/2013 at nine centers (Weill Cornell, Duke Cardiovascular Magnetic Resonance Center, New York University Langone Medical Center, New York Methodist Hospital, Methodist DeBakey Heart and Vascular Center, Allegheny General Hospital, Virginia Commonwealth University, Washington Hospital Center, University of Illinois/Chicago). Patients were identified retrospectively via query of pre-existing databases at each respective institution. In all multicenter patients, CMR and echocardiography (echo) were performed within a 10 day interval.
For both the derivation and validation cohorts, the sole exclusion criterion was absence of non-contrast cine-CMR images: No patients were excluded based on clinical characteristics or image quality. The study was conducted in accordance with the Institutional Review Board at each participatory site.
Cine-CMR
Image Acquisition
CMR was performed using commercial 1.5 Tesla scanners. Cine-CMR was acquired using a standard 2-dimensional steady state free precession (SSFP) pulse sequence (typical parameters: repetition time 3 msec, echo time 1 msec, bandwidth 977 Hz/pixel, temporal resolution 30–50 msec, in-plane spatial resolution 1.6 mm × 1.3 mm). Cine-CMR was acquired in conventional 2-, 3-, and 4-chamber long axis imaging planes.
Image Analysis
Derivation Cohort
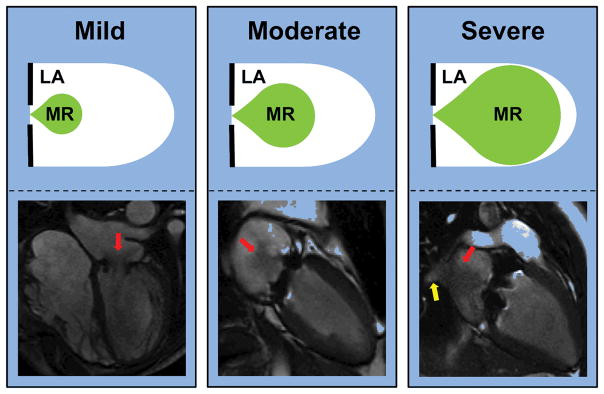
Cine-CMR exams were visually scored for MR severity. A simple MR grading system was applied, for which cumulative MR severity was visually graded based solely on jet size in relation to the left atrium (Figure 1): MR was graded as mild if jet area (for central jets) or length (for eccentric jets) was <1/3, moderate if 1/3–2/3, or severe if >2/3 of the left atrium. MR was graded in each long axis (2-, 3-, 4-chamber) orientation, with overall severity based on maximal grade assigned in at least two long axis planes. Intermediate grades (mild-moderate, moderate-severe) were assigned for cases in which maximal MR severity was visualized in < two long axis planes. A random sample representing > 10% of the study population (n=11 patients) was used to assess intra- and inter-observer reproducibility of the MR grading system.
Figure 1. Graded Severity of Cine-CMR Evidenced Mitral Regurgitation.
Representative cartoons (top) and corresponding patient examples (bottom) demonstrating visually assigned MR grades: Central MR was graded mild if jet area occupied < 1/3, moderate if 1/3–2/3, and severe if >2/3 of the left atrium (red arrows denote MR). Eccentric jets were graded using equivalent cutoffs as applied to jet length. Note pulmonary vein systolic flow reversal (yellow arrow) in association with severe mitral regurgitation.
Ancillary indices relating to MR were also scored, including jet direction (central or eccentric), density (graded using a 4 point scoring system), and pulmonary vein systolic flow reversal ([PSVR]; defined as an MR contiguous systolic flow jet extending into any pulmonary vein ostium).
Cine-CMR exams were further analyzed quantitatively, so as to compare visually scored parameters to corresponding quantitative indices. MR area (jet/left atrial area) was measured in the long axis orientation in which the MR jet appeared most prominent, and compared to corresponding qualitative scores. MR jet density was quantified based on Δ signal intensity (1 - systole/diastole) within a fixed (1.0cm2) region of interest within the regurgitant jet. Quantitative and qualitative analyses were performed by readers blinded to results of the other analytic approach.
Validation Cohort
At each participatory site, cine-CMR exams were visually interpreted for MR severity using the same qualitative scoring system tested in the derivation cohort. Cine-CMR analysis was performed by experienced, ACC/AHA level III certified, readers blinded to clinical patient information and results of other imaging modalities.
TTE and TEE, as performed at each participatory site, were used as references for MR severity. Echocardiography results were categorized based on clinically reported data, with MR severity assignment based on a 5-grade scale (mild, mild-moderate, moderate, moderate-severe, severe) in accordance with established American Society of Echocardiography (ASE) guidelines.3, 18 MR grade was categorized as indeterminate (i.e. due to image artifact) when documented as such in clinical echo reports.
Statistical Methods
Continuous variables (expressed as mean±standard deviation) were compared using Student’s t-test for two group comparisons, and analysis of variance (ANOVA) for multiple group comparisons. Categorical variables were compared using Chi-square and McNemar’s test for paired proportions. Inter- and intra-reader agreement was assessed using the kappa (κ) coefficient. Two-sided p <0.05 was considered indicative of statistical significance. Statistical calculations were performed using SPSS 12.0 (SPSS Inc, Chicago, IL).
Results
The study population consisted of a total of 85 patients with PMV. Over half (59%) of patients had mechanical mitral prostheses, with bioprosthetic valves in the remainder (Table 1). Nearly all patients (95%) had cine-CMR acquired in at least 2 orthogonal long axis orientations; 3 long axis images were acquired for PMV evaluation in 91% of the study population.
Table 1.
Population Characteristics
| Age (year) | 60 ± 15 |
| Male gender | 42% (36) |
| Mitral Valve Type | |
| Mechanical | 59% (50) |
| Bioprosthetic | 41% (35) |
| Image Acquisition Parameters | |
| Vendor (Siemens/GE/Phillips) | 58/39/4% |
| TR | 2.8 ± 0.4 |
| TE | 1.2 ± 0.3 |
| Flip Angle | 66 ± 12 |
| Bandwidth | 843 ± 304 |
| Long Axis Views Acquired | |
| Mean # | 2.9 ± 0.5 |
| % with 3 views | 91% (77) |
| Geometric and Functional Indices | |
| Left Atrium | |
| Diameter (cm) | 4.8 ± 1.1 |
| Area (cm2) | 29 ± 13 |
| Area index (cm2/m2) | 16 ± 8 |
| Left Ventricle | |
| Ejection fraction (%) | 47 ± 16 |
| End-diastolic volume (ml) | 176 ± 98 |
| End-diastolic volume index (ml/m2) | 94 ± 54 |
| End-systolic volume (ml) | 102 ± 93 |
| End-systolic volume index (ml/m2) | 54 ± 51 |
| Stroke volume (ml) | 74 ± 29 |
Derivation Cohort
Qualitative and quantitative analyses of MR severity were independently performed in 25 patients with PMV undergoing cine-CMR at the data coordination center (Weill Cornell).
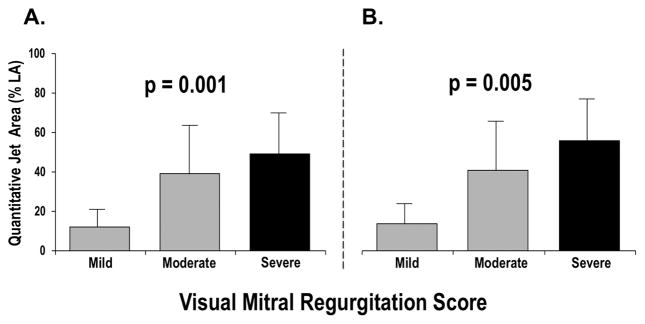
Figure 2 stratifies quantified MR area (jet/left atrial area) in relation to visual scored MR severity. As shown, quantified MR size (% left atrium) increased stepwise in relation to visual MR score for both the overall population (2A; p=0.001 for trend), as well as among the sub-group of patients with central regurgitant jets (2B; p=0.005). Quantified MR area was nearly 3-fold larger among patients with visually scored severe MR (49±21%) compared to those with ≤ moderate MR (18±17%; p=0.002).
Figure 2. Quantitative in Relation to Qualitative Assessment of MR Severity.
Quantified MR jet area (mean±SD) stratified by visually assigned MR grade. Results presented for overall derivation cohort (2A) as well as the sub-group of patients with central MR (2B). Note correspondence between quantitative and qualitative MR analysis, as evidenced by stepwise increases in jet area in relation to visually graded MR severity.
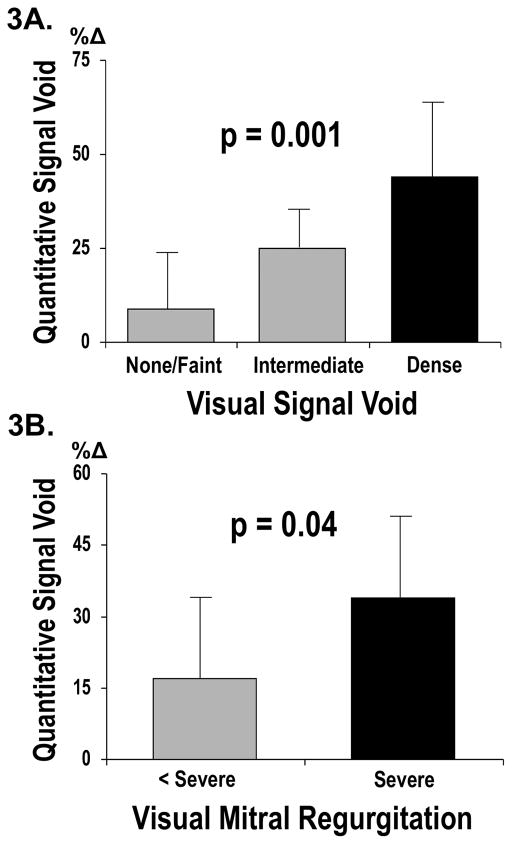
Figure 3 reports quantitative data concerning MR-induced changes in signal intensity within the regurgitant jet. Quantitative results again paralleled visual scores, with stepwise decrements in signal intensity (an index of inter-voxel de-phasing) between groups stratified based on visually assigned jet density (p=0.001 for trend). As shown in 3B, patients with visually scored severe MR had greater changes in signal intensity (Δ=34±17) than did those with lesser or absent MR (Δ=17±17; p=0.04), consistent with greater MR-associated voxel dephasing.
Figure 3. Mitral Regurgitation Density.
3A. Quantitative MR induced signal intensity change (1- systole/diastole) stratified by visually scored MR jet density. Note correspondence between quantitative signal intensity change and visually graded MR jet density.
3B. Quantitative signal intensity change compared between patients with and without severe MR.
Validation Cohort
Cine-CMR performance was further tested in a multicenter cohort of 75 patients, for whom echo was performed within 10 days of CMR. 44% of patients (n=33) underwent transesophageal echo (Δ=2±3 days), and 79% (n=59) underwent transthoracic echo (Δ=3±3 days).
MR was read as present on cine-CMR in 72% of patients (mild 39%, mild-moderate 7%, moderate 4%, moderate-severe 8%, severe 15%). Good intra- and inter-reader reproducibility was found for overall MR grade, as respectively tested at the data coordination center (κ=0.76) and at all participatory sites (κ=0.56). When categorized as a binary variable based on presence/absence of substantial (≥ moderate) MR, visually assigned grade demonstrated similarly high intra (κ=1.00) and inter-reader (κ=0.93) reproducibility.
Diagnostic Performance in Relation to Echo
Cine-CMR yielded moderate overall agreement in comparison to TEE (κ=0.44), with MR graded concordantly by the two modalities in 56% (18/32) of patients. Among cases of discordance (n=14), the majority (64%; 9/14) differed by ≤1 MR grade (mean Δ 1.2±0.5).
Table 2A reports diagnostic performance of cine-CMR using a threshold of TEE-evidenced severe MR. As shown, all patients with severe MR by the reference of TEE were concordantly diagnosed by cine-CMR (sensitivity=100%, negative predictive value 100%). Conversely, cine-CMR identified one patient with severe MR, for whom TEE diagnosed moderate-severe MR (specificity=96%, positive predictive value 86%). As shown in Table 2B, cine-CMR yielded lesser diagnostic performance when a broader TEE threshold of ≥ moderate MR was applied; Negative predictive value (90%) was reasonable, whereas positive predictive value (75%) was lower in relation to TEE.
Table 2.
Diagnostic Performance of Cine-CMR in Relation to Transesophageal Echocardiography
| Sensitivity | Specificity | Accuracy | Positive Predictive Value | Negative Predictive Value | |
|---|---|---|---|---|---|
| 2A. | |||||
| Severe MR | 100% (6/6) | 96% (25/26) | 97% (31/32) | 86% (6/7) | 100% (25/25) |
| 2B. | |||||
| ≥ Moderate MR | 82% (9/11) | 86% (18/21) | 84% (27/32) | 75% (9/12) | 90% (18/20) |
MR severity as graded by cine-CMR yielded poor overall agreement with TTE (κ=0.15), as evidenced by discordance in over half (59%) of patients. In cases of discordance (n=32), over one third (38%; 12/32) of cases differed by > 1 MR grade (mean Δ 1.3±0.6). Among patients with > moderate (i.e. moderate-severe or severe) MR on cine-CMR, 75% (6/8) had lesser (≤ moderate) MR on TTE. Among the limited cohort of patients (n=17) with all three tests (cine-CMR, TEE, TTE), all patients with > moderate MR on cine-CMR (n=4) were concordantly diagnosed with > moderate MR on TEE, among whom 3 of 4 were diagnosed with lesser or indeterminant MR on TTE.
Additional Cine-CMR Findings
Table 3 reports ancillary MR features as scored visually on cine-CMR. MR directionality was most often central, with eccentric MR present in 20% of affected patients. Consistent with quantitative data in the derivation cohort, patients with severe MR in the validation cohort had visual scores indicating denser regurgitant jets (p<0.001). Additionally, severe MR was associated with higher prevalence of PVSFR on cine-CMR (p<0.001).
Table 3.
Regurgitant Jet Properties
| Overall | Severe Mitral Regurgitation | |||
|---|---|---|---|---|
| Absent | Present | P | ||
| Direction | ||||
| Central | 80% (43) | 84% (36) | 64% (7) | 0.21 |
| Eccentric | 20% (11) | 16% (7) | 36% (4) | 0.21 |
| Pulmonary Vein Reversal | 13% (7) | 2% (1) | 55% (6) | <0.001 |
| Dense Signal Intensity (qualitative) | 22% (12) | 9% (4) | 73% (8) | <0.001 |
Table 4 stratifies indices of cardiac geometry and function in relation to MR severity. As shown, left atrial diameter was larger among patients with severe MR (p=0.01), with a similar albeit non-significant relationship for left atrial area (p=0.12). Neither LV geometric nor functional parameters differed between groups stratified based on presence or absence of cine-CMR evidenced severe MR (all p=NS).
Table 4.
Geometric and Functional Indices in Relation to Cine-CMR Evidenced Mitral Regurgitation
| Severe Mitral Regurgitation | |||
|---|---|---|---|
| Absent | Present | P | |
| Mitral Valve Type | |||
| Mechanical | 61% (39) | 55% (6) | 0.69 |
| Bioprosthetic | 39% (25) | 46% (5) | 0.69 |
| Left Atrium | |||
| Diameter (cm) | 4.6 ± 1.0 | 5.5 ± 0.9 | 0.01 |
| Area (cm2) | 29 ± 14 | 36 ± 10 | 0.12 |
| Area index (cm2/m2) | 16 ± 9 | 19 ± 4 | 0.26 |
| Left Ventricle | |||
| Ejection fraction (%) | 46 ± 16 | 53 ± 14 | 0.16 |
| End-diastolic volume (ml) | 180 ± 105 | 159 ± 86 | 0.55 |
| End-diastolic volume index (ml/m2) | 96 ± 58 | 85 ± 47 | 0.58 |
| End-systolic volume (ml) | 107 ± 102 | 83 ± 60 | 0.47 |
| End-systolic volume index (ml/m2) | 57 ± 56 | 45 ± 37 | 0.52 |
| Stroke volume (ml) | 72 ± 26 | 76 ± 45 | 0.75 |
Discussion
This is the first study to evaluate cine-CMR for prosthetic heart valve assessment. There are several key findings: First, among a single center cohort of consecutive patients, visually scored cine-CMR parameters agreed with quantified MR jet area and signal intensity. Second, among a multicenter cohort, visually graded MR on cine-CMR yielded good diagnostic performance as compared to TEE, including 100% negative predictive value for exclusion of TEE-evidenced severe MR. Among patients (n=17) with all three tests (cine-CMR, TEE, TTE), all cases with > moderate MR on cine-CMR (n=4) were concordantly diagnosed with > moderate MR on TEE, among whom 3 of 4 were diagnosed with lesser or indeterminant MR on TTE. Third, cine-CMR demonstrated adjunctive functional and structural changes associated with valvular regurgitation, as evidenced by larger left atrial chamber diameter (p=0.01) and higher prevalence of cine-CMR evidenced pulmonary vein systolic flow reversal (p<0.001) among patients with visually scored severe MR.
A major goal of our study was to evaluate a simple protocol for assessment of PMV-associated MR severity. To this end, our algorithm required no dedicated pulse sequences or tailored imaging planes. Instead, we evaluated routine cine-CMR and limited our interpretation to standard long axis images acquired in nearly all clinical CMR exams. While quantitative indices were used as comparators for visually scored parameters, actual diagnostic performance of cine-CMR was tested using visual cutoffs (<1/3, 1/3–2/3, > 2/3) for MR jet size and length. We speculate that this straightforward approach may explain the performance of our visual analysis, which yielded high reproducibility between participatory sites for presence or absence of substantial (≥ moderate) MR (κ=0.93).
Applied clinically, our results support cine-CMR as a non-invasive means of screening for substantial MR. Dedicated quantitative imaging, using CMR or TEE based methods, could then be reserved for patients with substantial MR on cine-CMR. This approach would address an important unmet clinical need for patients with PMV. While TTE is well validated as a non-invasive screening test for native MR, it is known to be limited for assessment of prosthetic valve function due to prosthesis-associated reverberation artifact that interferes with ultrasound wave transmission, impeding visualization of left atrial regurgurgitant jets.3–5 Similarly, phase contrast CMR imaging is well validated for assessment of native valvular regurgitation,10, 11 but can be compromised by localized field disturbances as can be produced by prosthetic materials.19, 20 Of course, prosthetic materials within both bio- and mechanical mitral valves can produce susceptibility artifacts due to localized changes in magnetic field homogeneity,21, 22 prohibiting direct cine-CMR evaluation of valve morphology and obscuring small amounts of regurgitant flow. However, our results demonstrate that such localized disturbances do not typically interfere with assessment of substantial (i.e. moderate or severe) MR jets, which would be expected to extend well beyond valve prostheses and thus appear on cine-CMR as dynamic regions of systolic signal heterogeneity.
While we are unaware of prior studies that have tested any CMR method (cine or otherwise) for evaluation of prosthetic valves, cine-CMR has been shown to be useful for native valve regurgitation. This concept was initially demonstrated using gradient echo based cine-CMR. Wagner et al, studying a cohort that included 34 patients with mitral regurgitation, demonstrated that MR jet size (on gradient echo cine-CMR) increased stepwise in relation to severity of echo and/or x-ray angiography evidenced MR.13 Consistent with our findings regarding regurgitant jet signal intensity on SSFP, Pflugfelder et al demonstrated that left atrial signal intensity on gradient echo cine-CMR was lower in patients with severe MR as compared to normative controls.14 More recently, SSFP cine-CMR has been used to assess presence and severity of MR.16, 17, 23 Among a cohort of 68 patients, Heitner et al reported that cine-CMR yielded moderate agreement (κ=0.47) with echocardiography, paralleling our current results (κ=0.45).16 However, this study graded MR based on an amalgam of 4–6 different cine-CMR criteria, thereby prohibiting direct examination of whether MR jet size alone could be used as a simple index of MR severity.
Beyond direct assessment of MR jet size, our findings also demonstrate that cine-CMR can be useful to evaluate MR-associated alterations in both left atrial remodeling and pulmonary vein flow patterns. Our finding of an association between severe MR and PVSFR is consistent with established echocardiography data concerning MR physiology.24, 25 Regarding left atrial remodeling, we speculate that our observed association between severe MR and increased chamber size may reflect one or more phenomena. On the one hand, it is possible that left atrial chamber dilation occurs as a consequence of recurrent MR following PMV. Alternatively, it is conceivable that pre-operative left atrial geometry impacts prosthetic valve function, thereby contributing to post-operative MR. Future studies, for which serial cine-CMR is performed before and after PMV, may be useful to test whether pre-operative left atrial geometry predicts long term valve integrity following PMV.
Several limitations should be noted. First, whereas all cine-CMR exams were interpreted using a uniform protocol, echocardiography results were based on documented clinical reports rather than primary image analysis. While all echoes were performed and interpreted in experienced, high volume tertiary care centers, it is important to recognize that established ASE guidelines state that MR severity should be graded based on integrated findings from different echo methods,3 and that this study did not entail direct comparison between individual echo methods and cine-CMR. Second, while the mean interval between CMR and echo was short (Δ 3 days), MR itself can vary somewhat on a near instantaneous basis and be influenced by afterload changes, as can occur in the setting of TEE. Finally, whereas our study encompassed a broad cohort of patients with PMV, results may not necessary be applicable to other valvular prostheses.
In conclusion, this study demonstrates utility of routine cine-CMR for assessment of PMV-associated MR, which manifests concordant quantitative and qualitative changes in size and density of inter-voxel dephasing. Visual MR assessment based on regurgitant jet size provides an accurate non-invasive means of screening for TEE-evidenced severe MR.
Acknowledgments
The authors thank Pascal Spincemaille PhD for valuable input regarding technical aspects of this manuscript.
Sources of Funding: K23 HL102249-01
Footnotes
Conflicts of Interests: None.
References
- 1.Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, Rahimtoola SH. Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial. J Am Coll Cardiol. 2000;36:1152–1158. doi: 10.1016/s0735-1097(00)00834-2. [DOI] [PubMed] [Google Scholar]
- 2.Kulik A, Bedard P, Lam BK, Rubens FD, Hendry PJ, Masters RG, Mesana TG, Ruel M. Mechanical versus bioprosthetic valve replacement in middle-aged patients. Eur J Cardiothorac Surg. 2006;30:485–491. doi: 10.1016/j.ejcts.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 3.Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener JS, Grayburn PA, Khandheria BK, Levine RA, Marx GR, Miller FA, Jr, Nakatani S, Quinones MA, Rakowski H, Rodriguez LL, Swaminathan M, Waggoner AD, Weissman NJ, Zabalgoitia M. Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound. J Am Soc Echocardiogr. 2009;22:975–1014. doi: 10.1016/j.echo.2009.07.013. quiz 1082–1014. [DOI] [PubMed] [Google Scholar]
- 4.Daniel LB, Grigg LE, Weisel RD, Rakowski H. Comparison of transthoracic and transesophageal assessment of prosthetic valve dysfunction. Echocardiography. 1990;7:83–95. doi: 10.1111/j.1540-8175.1990.tb00352.x. [DOI] [PubMed] [Google Scholar]
- 5.Sprecher DL, Adamick R, Adams D, Kisslo J. In vitro color flow, pulsed and continuous wave Doppler ultrasound masking of flow by prosthetic valves. J Am Coll Cardiol. 1987;9:1306–1310. doi: 10.1016/s0735-1097(87)80470-9. [DOI] [PubMed] [Google Scholar]
- 6.van den Brink RB, Visser CA, Basart DC, Duren DR, de Jong AP, Dunning AJ. Comparison of transthoracic and transesophageal color Doppler flow imaging in patients with mechanical prostheses in the mitral valve position. Am J Cardiol. 1989;63:1471–1474. doi: 10.1016/0002-9149(89)90010-6. [DOI] [PubMed] [Google Scholar]
- 7. [accessed 1/7/13];Healthcare Cost and Utilization Project: The Nationwide Inpatient Sample. at http://hcupnet.ahrg.gov.
- 8.Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 9.Enriquez-Sarano M, Akins CW, Vahanian A. Mitral regurgitation. Lancet. 2009;373:1382–1394. doi: 10.1016/S0140-6736(09)60692-9. [DOI] [PubMed] [Google Scholar]
- 10.Fujita N, Chazouilleres AF, Hartiala JJ, O’Sullivan M, Heidenreich P, Kaplan JD, Sakuma H, Foster E, Caputo GR, Higgins CB. Quantification of mitral regurgitation by velocity-encoded cine nuclear magnetic resonance imaging. J Am Coll Cardiol. 1994;23:951–958. doi: 10.1016/0735-1097(94)90642-4. [DOI] [PubMed] [Google Scholar]
- 11.Hundley WG, Li HF, Willard JE, Landau C, Lange RA, Meshack BM, Hillis LD, Peshock RM. Magnetic resonance imaging assessment of the severity of mitral regurgitation. Comparison with invasive techniques. Circulation. 1995;92:1151–58. doi: 10.1161/01.cir.92.5.1151. [DOI] [PubMed] [Google Scholar]
- 12.Westenberg JJ, Roes SD, Ajmone Marsan N, Binnendijk NM, Doornbos J, Bax JJ, Reiber JH, de Roos A, van der Geest RJ. Mitral valve and tricuspid valve blood flow: accurate quantification with 3D velocity-encoded MR imaging with retrospective valve tracking. Radiology. 2008;249:792–800. doi: 10.1148/radiol.2492080146. [DOI] [PubMed] [Google Scholar]
- 13.Wagner S, Auffermann W, Buser P, Lim TH, Kircher B, Pflugfelder P, Higgins CB. Diagnostic accuracy and estimation of the severity of valvular regurgitation from the signal void on cine magnetic resonance images. Am Heart J. 1989;118:760–767. doi: 10.1016/0002-8703(89)90590-5. [DOI] [PubMed] [Google Scholar]
- 14.Pflugfelder PW, Sechtem UP, White RD, Cassidy MM, Schiller NB, Higgins CB. Noninvasive evaluation of mitral regurgitation by analysis of left atrial signal loss in cine magnetic resonance. Am Heart J. 1989;117:1113–1119. doi: 10.1016/0002-8703(89)90870-3. [DOI] [PubMed] [Google Scholar]
- 15.Aurigemma G, Reichek N, Schiebler M, Axel L. Evaluation of mitral regurgitation by cine magnetic resonance imaging. Am J Cardiol. 1990;66:621–625. doi: 10.1016/0002-9149(90)90491-i. [DOI] [PubMed] [Google Scholar]
- 16.Heitner J, Bhumireddy GP, Crowley AL, Weinsaft J, Haq SA, Klem I, Kim RJ, Jollis JG. Clinical application of cine-MRI in the visual assessment of mitral regurgitation compared to echo and cardiac catheterization. PLoS One. 2012;7:e40491. doi: 10.1371/journal.pone.0040491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reddy DT, Shah M, Doyle M, Thompson DV, Williams RB, Yamrozik J, Biederman RW. Evaluation of Cardiac Valvular Regurgitant Lesions by Cardiac MRI Sequences: Comparison of a Four Valve Semi-quantitative vs. Quantitative Approach. J Heart Valve Disease. 2013 (in press) [PubMed] [Google Scholar]
- 18.Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16:777–802. doi: 10.1016/S0894-7317(03)00335-3. [DOI] [PubMed] [Google Scholar]
- 19.Lethimonnier F, Bouligand B, Thouveny F, Furber A, Jallet P, Caron-Poitreau C, Le Jeune JJ. Error assessment due to coronary stents in flow-encoded phase contrast MR angiography: a phantom study. J Magn Reson Imaging. 1999;10:899–902. doi: 10.1002/(sici)1522-2586(199911)10:5<899::aid-jmri40>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 20.Bartels LW, Smits HF, Bakker CJ, Viergever MA. MR imaging of vascular stents: effects of susceptibility, flow, and radiofrequency eddy currents. J Vasc Interv Radiol. 2001;12:365–371. doi: 10.1016/s1051-0443(07)61918-6. [DOI] [PubMed] [Google Scholar]
- 21.Di Cesare E, Enrici RM, Paparoni S, Castaldo F, Alagia MG, Splendiani A, Bottone A, Lupattelli L. Low-field magnetic resonance imaging in the evaluation of mechanical and biological heart valve function. Eur J Radiol. 1995;20:224–228. doi: 10.1016/0720-048x(95)00656-b. [DOI] [PubMed] [Google Scholar]
- 22.Immel E, Gilbert FJ, Melzer A. Experimental MRI visible resonant prosthetic heart valves. Minim Invasive Ther Allied Technol. 2009;18:149–155. doi: 10.1080/13645700902921310. [DOI] [PubMed] [Google Scholar]
- 23.Krombach GA, Kuhl H, Bucker A, Mahnken AH, Spuntrup E, Lipke C, Schroder J, Gunther RW. Cine MR imaging of heart valve dysfunction with segmented true fast imaging with steady state free precession. J Magn Reson Imaging. 2004;19:59–67. doi: 10.1002/jmri.10428. [DOI] [PubMed] [Google Scholar]
- 24.Enriquez-Sarano M, Dujardin KS, Tribouilloy CM, Seward JB, Yoganathan AP, Bailey KR, Tajik AJ. Determinants of pulmonary venous flow reversal in mitral regurgitation and its usefulness in determining the severity of regurgitation. Am J Cardiol. 1999;83:535–541. doi: 10.1016/s0002-9149(98)00909-6. [DOI] [PubMed] [Google Scholar]
- 25.Pu M, Griffin BP, Vandervoort PM, Stewart WJ, Fan X, Cosgrove DM, Thomas JD. The value of assessing pulmonary venous flow velocity for predicting severity of mitral regurgitation: A quantitative assessment integrating left ventricular function. J Am Soc Echocardiogr. 1999;12:736–743. doi: 10.1016/s0894-7317(99)70024-6. [DOI] [PubMed] [Google Scholar]