Abstract
Aim
Intra and inter tumour heterogeneity is a known feature in cancer because tumour cells undergo changes at genetic and epigenetic level as they spread from their primary tumour site. Adjuvant treatment protocols in breast cancer are currently based on the biological characteristics of the primary tumour, which in most cases has been removed surgically. Considering tumour heterogeneity in metastases we examined the present status of knowledge regarding measurable differences in tumour profiling between the primary breast tumour and its synchronous axillary lymph node metastases (ALNM) and if so whether adjuvant therapy directed towards the tumour characteristics of the ALNM instead of those of the primary tumour is more effective.
Methods
We performed a literature search in Pubmed with the following MeSH headings: HUMAN and BREAST NEOPLASMS and RECEPTORS and ErbB-2.
Results
A significant change in tumour features was seen in metachronous metastases. In contrast, a high concordance of biomarker expression was reported between a primary breast tumour and its synchronous ALNM.
Conclusion
Tumour heterogeneity is a challenge for targeted therapy. A poor response can be explained by the diversity of tumour cells. The biological profile of synchronous ALNM measured by oestrogen (ER), progesterone (PR) and her-2-neu receptor status does not differ from the primary breast tumour and is not predictive of the tumour profile in metachronous metastasis. New techniques, such as profiling of circulating tumour cells or tumour behaviour in xenografts, are promising in directing more effective adjuvant therapy.
Keywords: Biomarker, breast cancer, breast neoplasms, metastases, oestrogen receptors, progesterone receptors
Introduction
Breast cancer remains the most common cancer in women worldwide and rated second in cancer related mortality (World Cancer Report, 2014). Breast cancer treatment strategies and prognosis are guided by classification into molecular subtypes as there are: Luminal A, Luminal B, her-2-neu positive and triple negative/basal-like tumours. Surgery remains the primary treatment in most cases and entails the complete removal of the primary tumour in the breast and a surgical staging of the axilla. Adjuvant treatment is dictated by stage of disease, type of surgery and the molecular subtype of the primary tumour (Goldhirsch et al., 2013).
Our understanding of carcinogenesis was driven by the observation that a tumour consists of cell groups (clones) with molecular and phenotypic differences. This phenomenon is known as tumour heterogeneity and is caused by differences in susceptibility for genetic mutations, epigenetic alterations and differences in tumour microenvironment (Banerjee, 2010; Gerlinger et al., 2012; Swanton, 2012). Tumour heterogeneity constitutes a challenge for cancer research and treatment. The immediate implication of intra tumour heterogeneity is that a specific clone of tumour cells as a result of its aggressive biological behaviour might be responsible for the ultimate outcome of the patient whilst it remains unrecognized by the tumour profiling techniques available at present. Inter tumour heterogeneity on the other hand implicates a change in characteristics between the primary tumour and its metastases. This potentially involves changes in drug sensitivity/resistance (Swanton, 2012).
Whilst developing more advanced tumour profiling techniques and clinically useful biomarkers to target therapy one wonders whether it would not be more effective in case of lymph node positive breast cancer (LNPBC) to direct adjuvant therapy towards the nature of the ALNM rather than that of the primary breast tumour removed by surgery. In order to explore this hypothesis we searched the literature for data on inter tumour heterogeneity in LNPBC.
Materials and Methods
2.1. Types of studies
Breast cancer studies reporting on the expression of ER or PR or her-2-neu in primary breast tumour and its metastases (synchronous and/or metachronous) were included. Both prospective and retrospective studies were included.
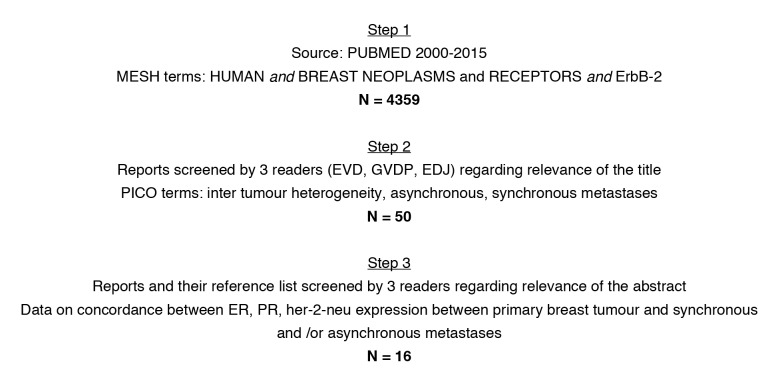
A comprehensive search was performed in Pubmed, articles published from 2000 until 2015, selected by 3 readers (EVD, GVDP, EDJ). The following MeSH headings were used: HUMAN and BREAST NEOPLASMS and RECEPTORS and ErbB-2. Only full text articles written in English were selected (Fig. 1).
Figure 1.
— Search strategy
2.2. Subjects
All women included in this analysis had a histological diagnosis of primary breast cancer and ipsilateral, synchronous ALNM. If studied, pathological information on possible asynchronous, distant metastasis was processed as well. No inclusion restrictions were retained regarding age, menopausal stage or type of treatment.
2.3. Types of outcome measurements
Hormone receptor analysis in the studies included was performed by immunohistochemistry, in which positive interpretation requires at least 1% of tumour cells showing positive nuclear staining of any intensity. Her-2-neu status was tested with two possible methods: immunohistochemistry and/or fluorescence in situ hybridization. Tumour heterogeneity was interpreted as a difference in expression of biomarkers.
Results
A summary of articles reporting on breast cancer and the concordance regarding ER, PR and her-2-neu expression between the primary breast tumour and synchronous or metachronous metastases is shown in Tables I and II. The majority of studies are retrospective, consists of small numbers of women and in most studies a central pathology review was performed. In general there is a shift in the ER/PR/her-2-neu profile in 10-20 % of synchronous ALNM and 20-40% of metachronous metastases. Both losses and/or gain of receptor expression were noticed. In metachronous metastases loss of receptor expression was more pronounced. Loss of ER, PR and/or her-2-neu expression occurred in 25%, 33% and 8% of cases respectively in these combined series, whilst gain of receptor expression was seen in 8%, 8% and 12% of cases respectively (Simmons et al., 2009; Hoefnagel et al., 2010; Jensen et al., 2012; Lindström et al., 2012; Ibrahim et al., 2013).
Table I.
— ER, PR, and her-2-neu expression profiles: concordance (%) between the primary breast tumour and synchronous LNM.
| Author | Study structure | Number of patients | Biomarker | ||
| ER | PR | her-2-neu | |||
| Falck 2010 | Retrospective pT1-2 N1M0 |
425 | 93% | 84% | 97% |
| D’Andrea 2007 | Retrospective LNPBC (> 10 positive LN, M0) |
90 | 96.6% | 96.6% | 96.1% |
| Ieni 2014 | Retrospective LNPBC (M0) |
148 | - | - | 95.3% |
| Aitken 2010 | Retrospective High grade LNPBC (M0) |
385 | 71.6% | 76.5% | 91.1% |
| Adamczyk 2012 | Retrospective T1-3 N1M0 |
108 | 96.5% | 97.6% | 95.5% |
| Greer 2012 | Prospective LNP(macro)BC |
165 | 83% | 97% | 97% |
| Jensen 2012 | Retrospective | 53 | 96% | - | 100% |
| Carlsson 2004 | Retrospective M+ |
47 | - | - | 100% |
| Ataseven 2012 | Prospective LNPBC |
119 | 97.4% | 96.6% | 96.6% |
| Briffod 2000 | Fine needle aspiration cytology LNPBC |
38 | 94.7% | 86.8% | 92% |
| Aoyama 2010 | Retrospective LNPBC |
60 | - | - | 91.6% |
Table II.
— ER, PR, and her-2-neu expression profiles: concordance (%) between the primary breast tumour and metachronous metastasis.
| Author | Study structure | Number of patients | Biomarker | ||
| ER | PR | her-2-neu | |||
| Ibrahim 2013 | Retrospective | 120 | 83.6% | 58.3% | 82.5% |
| Hoefnagel 2010 | Retrospective | 233 | 89.7% | 70% | 94.8% |
| Lindström 2012 | Retrospective | 1010 | 66.4% | 68% | 84.3% |
| Jensen 2012 | Prospective | 119 | 88% | - | 91% |
| Simmons 2009 | Prospective | 25 | 60% | 60% | 92% |
Discussion
In this review of the literature we studied the reported changes in biological profile between the primary breast tumour and its metastases at the level of ER, PR and her-2-neu expression as biomarkers which to date are used in daily clinical practice to guide systemic adjuvant therapy in breast cancer. In general there was no significant change seen in biomarker profile between the primary breast tumour and its synchronous ALNM (Carlsson et al., 2004; D’ Andrea et al., 2007; Falck et al., 2010; Adamczyk et al., 2012; Ataseven et al., 2012; Greer et al., 2012; Jensen et al., 2012; Ieni et al., 2014). The results of Aitken et al. (2010) are in contrast to the concordance rates mentioned earlier as they found a disparate breast/node status for at least one biomarker (ER of PR) in almost 50% of cases, resulting in ALNM with worse prognostic profile illustrated by shifts to ER negativity and her-2-neu positivity. A study population consisting of highgrade primary breast tumours only is a possible explanation for these aberrant results. Systematic evaluation of these biomarkers in ALNM therefore is not recommended. On the contrary inter tumour heterogeneity between primary tumours of the breast and distant metachronous metastases are responsible for a significant change of tumour features (Table II). In the event of metachronous disease, the biomarker status of this new locus should be reassessed to optimize adjuvant therapy in order to improve patient outcome. Detection of loss of function in this new tumour locus reflected in a change/loss of an immunohistochemical biomarker should avoid ineffective therapy based on the biomarker signature of the primary breast tumour and direct therapy into different treatment strategies of proven efficacy.
Removal of involved lymph nodes is no longer believed to improve prognosis in breast cancer although their presence remains an important negative prognostic factor for relapse and death in breast cancer (Giuliano et al., 2011; Falck et al., 2013). It remains uncertain which role the tumour cells colonizing synchronous ALNM play in the mechanism of dissemination to organs at distance. Do tumour cells disseminate to distant organs via synchronous ALNM or does lymphogenic and hematogenic spread operate through different mechanisms? Tumour cells designed to metastasize hematogenously seem to be biologically different from the tumour cells found in ALNM (van de Vijver et al., 2002).
Fidler (2003) revisited the ‘seed and soil’ hypothesis describing the process of metastasis and explaining why specific tumour types (the ‘seed’) spread to specific organs (the ‘soil’). It is clear now that throughout the process of tumour progression cells acquire genetic variations and instability, which determines whether their phenotype predisposes to dissemination. In the event of dissemination, the locus of metastasis is not random and not only depending on anatomical barriers. The microenvironment of each organ is different. Different cell surface receptors and variable growth factors are responsible for a tumour cell specific and host specific response. This revisited ‘seed and soil’ hypothesis explains why tumour cells emerging in synchronous ALNM have a phenotype different from those in metachronous metastases. The reason for high concordance in biomarker expression between the primary breast tumour and the synchronous ALNM is less clear: the migration of tumour cells to the axilla is either based on a different mechanism than the one that dictates dissemination to distant loci. Therefore other biomarkers remaining unrevealed to date may differentiate between tumour cells present in the primary breast tumour and the synchronous ALNM.
However to date no studies have been conducted examining differences in outcome of breast cancer therapy comparing systemic therapy directed against the biomarker expression in synchronous ALNM versus the biomarker expression in primary breast tumour.
To interfere with disease progression targets other than tumour cells in synchronous ALNM could be explored: the xenograft model to study tumour behaviour in the laboratory, molecular imaging with biomarkers to locate and bio-type metastatic tumour and the concept of circulating tumour cells to improve therapy in an early stage of disease.
An in vivo mouse-hosted patient derived xenograft (PDX) is likely to reflect tumour biology better than in vitro cell lines derived from tumours. The study of tumour behaviour and tumour heterogeneity should be more accurate in PDX. It is a promising model for basic research in oncology and phase I interventional studies with new compounds (Willey et al., 2015). For instance tumour grafting in the mammary glands of mice gives rise to metastasis with patterns similar to those observed in the original breast cancer patients (DeRose et al., 2011). Likewise, aurora kinase inhibitor, a cell-cycle regulator, was tested in triple negative breast cancer xenografts to study its potential as a new anticancer drug (Romanelli et al., 2012).
Non-invasive assessment of receptor status by molecular imaging via PET or SPECT whether or not combined with CT or MRI may become a way of identifying therapeutic anchors in the individual patient. Developing isotopic marked target molecules against ER, PR, her-2-neu or other clinically useful molecular targets (radiopharmaceuticals) could reveal receptor status of tumour sites in particular tumour deposits not amenable for biopsy. Biomarker specific targeting agents are labelled with positron or gamma-emitting radionuclides, optical dyes or paramagnetic contrast molecules for PET, SPECT and MRI respectively (Capala and Bouchelouche, 2010; Sörensen et al., 2014).
The phenomenon of circulating tumour cells (CTCs) was described as early as in the 1800’s (Recamier, 1829).
Cristofanilli et al. (2004) tested the hypothesis that levels of CTCs can predict survival in metastatic breast cancer and concluded that the number of CTCs before treatment is an independent predictor of progression-free survival and overall survival in patients with metastatic breast cancer. Detection, quantification and characterization of CTCs open new perspectives on cancer dissemination and treatment. In the current staging of breast cancer the finding of CTCs is referred to as a stage cM0 (i+). Studies on CTCs and breast cancer are in phase 3, offering major perspectives for both biological and clinical research on the metastatic process (Bidard et al., 2013). Hypothetically CTCs could be a marker of ‘active’ disease and a precursor of metastatic disease. Biomarker expression in CTCs was described by Mikulová et al. (2014). They were able to detect CTCs in 31% of 54 patients with early stage breast cancer and found a 20% discordance in her-2-neu expression between primary breast tumour and CTCs.
In conclusion, tumour heterogeneity constitutes a challenge for cancer research and therapy. We reviewed the data on the ER, PR and her-2-neu expression both in the primary breast tumour and its synchronous ALNM and metachronous metastases as the most used biomarkers in breast cancer in daily clinical practice to date. A high concordance between primary breast tumour and synchronous ALNM was seen. Therefore determination of ER, PR, her-2-neu on synchronous ALNM to tune systemic therapy and therefore outcome is not contributing. Since tumour heterogeneity between the primary breast tumour and metachronous metastasis is ascertained, distant metastasis should be biopsied and their biomarker profile direct therapeutic planning. The process of dissemination of tumour cells and implications for cancer treatment however remains unclear. To date we know that ALNM in breast cancer are important for prognosis, their removal does not impact on survival and their biological profile does not predict the biological characteristics of metachronous metastasis. Both the exploration of new biomarkers in ALNM and the biological profile of CTCs therefore could be the next step in our understanding of inter tumour heterogeneity and its therapeutic consequences.
References
- 1.Adamczyk A, Niemiec J, Ambicka A, et al. Expression of ER/PR/HER2, basal markers and adhesion molecules in primary breast cancer and in lymph nodes metastases: a comparative immunohistochemical analysis. Pol J Pathol. 2012;63(4):228–234. doi: 10.5114/pjp.2012.32769. [DOI] [PubMed] [Google Scholar]
- 2.Aitken SJ, Thomas JS, Langdon SP, et al. Quantitative analysis of changes in ER, PR and HER2 expression in primary breast cancer and paired nodal metastases. Ann Oncol. 2010;21(6):1254–1261. doi: 10.1093/annonc/mdp427. [DOI] [PubMed] [Google Scholar]
- 3.Aoyama K, Kamio T, Nishikawa T, et al. A comparison of HER2/neu gene amplification and its protein overexpression between primary breast cancer and metastatic lymph nodes. Jpn J Clin Oncol. 2010;40(7):613–619. doi: 10.1093/jjco/hyq019. [DOI] [PubMed] [Google Scholar]
- 4.Ataseven B, Gologan D, Gunesch A, et al. HER2/neu, Topoisomerase 2a, Estrogen and Progesterone Receptors: Discordance between Primary Breast Cancer and Metastatic Axillary Lymph Node in Expression and Amplification Characteristics. Breast Care (Basel) 2012;7(6):465–470. doi: 10.1159/000345467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banerjee D. Reinventing diagnostics for personalized therapy in oncology. Cancers (Basel) 2010;2(2):1066–1091. doi: 10.3390/cancers2021066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bidard FC, Fehm T, Ignatiadis M, et al. Clinical application of circulating tumor cells in breast cancer: overview of the current interventional trials. Cancer Metastasis Rev. 2013;32(1):179–188. doi: 10.1007/s10555-012-9398-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briffod M, Hacene K, Le Doussal V, et al. Immunohistochemistry on cell blocks from fine-needle cytopunctures of primary breast carcinomas and lymph node metastases. Mod Pathol. 2000;13(8):841–850. doi: 10.1038/modpathol.3880149. [DOI] [PubMed] [Google Scholar]
- 8.Capala J, Bouchelouche K. Molecular imaging of HER2-positive breast cancer: a step toward an individualized ‘image and treat’ strategy. Curr Opin Oncol. 2010;22(6):559–566. doi: 10.1097/CCO.0b013e32833f8c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlsson J, Nordgren H, Sjöström J. HER2 expression in breast cancer primary tumours and corresponding metastases. Original data and literature review. Br J Cancer. 2004;90(12):2344–2348. doi: 10.1038/sj.bjc.6601881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cristofanilli M, Budd GT, Ellis MJ, et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med. 2004;351(8):781–791. doi: 10.1056/NEJMoa040766. [DOI] [PubMed] [Google Scholar]
- 11.D’Andrea MR, Limiti MR, Bari M, et al. Correlation between genetic and biological aspects in primary non-metastatic breast cancers and corresponding synchronous axillary lymph node metastasis. Breast Cancer Res Treat. 2007;101(3):279–284. doi: 10.1007/s10549-006-9300-2. [DOI] [PubMed] [Google Scholar]
- 12.DeRose YS, Wang G, Lin Y-C, et al. Tumor grafts derived from women with breast cancer authentically reflect tumor pathology, growth, metastasis and disease outcomes. Nat Med. 2011:1514–1520. doi: 10.1038/nm.2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falck AK, Bendahl PO, Chebil G, et al. Biomarker expression and St Gallen molecular subtype classification in primary tumours, synchronous lymph node metastases and asynchronous relapses in primary breast cancer patients with 10 years’ follow-up. Breast Cancer Res Treat. 2013;140(1):93–104. doi: 10.1007/s10549-013-2617-8. [DOI] [PubMed] [Google Scholar]
- 14.Falck AK, Fernö M, Bendahl PO, et al. Does analysis of biomarkers in tumor cells in lymph node metastases give additional prognostic information in primary breast cancer? World J Surg. 2010;34(7):1434–1441. doi: 10.1007/s00268-010-0499-z. [DOI] [PubMed] [Google Scholar]
- 15.Fidler IJ. The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer. 2003;3(6):453–458. doi: 10.1038/nrc1098. [DOI] [PubMed] [Google Scholar]
- 16.Gerlinger M, Rowan AJ, Horswell S, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med. 2012;366(10):883–892. doi: 10.1056/NEJMoa1113205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giuliano ae, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305(6):569–575. doi: 10.1001/jama.2011.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldhirsch A, Winer EP, Coates AS, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206–2223. doi: 10.1093/annonc/mdt303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greer LT, Balayla J, Garcia-Velasco JA. Should immunohistochemical (IHC) markers be performed on axillary lymph node metastases in view of the lack of concordance between the primary tumor and axillary lymph node metastases? J Am Coll Surg. 2012;215(3): [Google Scholar]
- 20.Hoefnagel LD, van de Vijver MJ, van Slooten HJ, et al. Receptor conversion in distant breast cancer metastases. Breast Cancer Res. 2010;12(5): doi: 10.1186/bcr2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ibrahim T, Farolfi A, Scarpi E, et al. Hormonal receptor, human epidermal growth factor receptor-2, and Ki67 discordance between primary breast cancer and paired metastases: clinical impact. Oncology. 2013;84(3):150–157. doi: 10.1159/000345795. [DOI] [PubMed] [Google Scholar]
- 22.Ieni A, Barresi V, Caltabiano R, et al. Discordance rate of HER2 status in primary breast carcinomas versus synchronous axillary lymph node metastases: a multicenter retrospective investigation. Onco Targets Ther. 2014;7:1267–1272. doi: 10.2147/OTT.S65294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jensen JD, Knoop A, Ewertz M, et al. ER, HER2, and TOP2A expression in primary tumor, synchronous axillary nodes, and asynchronous metastases in breast cancer. Breast Cancer Res Treat. 2012;132(2):511–521. doi: 10.1007/s10549-011-1610-3. [DOI] [PubMed] [Google Scholar]
- 24.Lindström LS, Karlsson E, Wilking UM, et al. Clinically used breast cancer markers such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 are unstable throughout tumor progression. J Clin Oncol. 2012;30(21):2601–2608. doi: 10.1200/JCO.2011.37.2482. [DOI] [PubMed] [Google Scholar]
- 25.Mikulová V, Cabiňaková M, Janatková I, et al. Detection of circulating tumor cells during follow-up of patients with early breast cancer: Clinical utility for monitoring of therapy efficacy. Scand J Clin Lab Invest. 2014;74(2):132–142. doi: 10.3109/00365513.2013.864784. [DOI] [PubMed] [Google Scholar]
- 26.Recamier JC. L’histoire de le Meme Maladie. Gabor. 1829:110. doi: 10.1016/j.rbmo.2012.06.012. [DOI] [Google Scholar]
- 27.Romanelli A, Clark A, Assayag F, et al. Inhibiting aurora kinases reduces tumor growth and suppresses tumor recurrence after chemotherapy in patient-derived triplenegative breast cancer xenografts. Mol Cancer Ther. 2012;11(12):2693–2703. doi: 10.1158/1535-7163.MCT-12-0441-T. [DOI] [PubMed] [Google Scholar]
- 28.Simmons C, Miller N, Geddie W, et al. Does confirmatory tumor biopsy alter the management of breast cancer patients with distant metastases? Ann Oncol. 2009;20(9):1499–1504. doi: 10.1007/s00404-013-3020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sörensen J, Sandberg D, Sandström M, et al. First-in-human molecular imaging of HER2 expression in breast cancer metastases using the 111In-ABY-025 affibody molecule. J Nucl Med. 2014;55(5):730–735. doi: 10.2967/jnumed.113.131243. [DOI] [PubMed] [Google Scholar]
- 30.Swanton C. Intratumor heterogeneity: evolution through space and time. Cancer Res. 2012;72(19):4875–4882. doi: 10.1158/0008-5472.CAN-12-2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van de Vijver MJ, He YD, van't Veer LJ, et al. A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002;347(25):1999–2009. doi: 10.1056/NEJMoa021967. [DOI] [PubMed] [Google Scholar]
- 32.Willey CD, Gilvert AN, Anderson JC, et al. Patient-Derived Xenografts as a Model System for Radiation Research. Semin Radiat Oncol. 2015;25(4):273–280. doi: 10.1016/j.semradonc.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stewart BW, Wild CP, editors. World Health Organization. 2014. World Cancer Report 2014. [Google Scholar]