Abstract
Purpose/Objectives
To characterize the perspectives of partners (husbands or significant others) of patients with breast cancer in the treatment decision-making process and to evaluate racial and ethnic differences in decision outcomes.
Design
A cross-sectional survey.
Setting
Los Angeles, CA, and Detroit, MI.
Sample
517 partners of a population-based sample of patients with breast cancer four years post-treatment.
Methods
A self-administered mailed questionnaire. Chi-square tests and logistic regression were used to assess associations between race and ethnicity and decision outcomes.
Main Research Variables
Decision regret and three elements of the decision process: information received, actual involvement, and desired involvement.
Findings
Most partners reported receiving sufficient information (77%), being involved in treatment decisions (74%), and having sufficient involvement (73%). Less-acculturated Hispanic partners were more likely than their Caucasian counterparts to report high decision regret (45% versus 14%, p < 0.001). Factors significantly associated (p < 0.05) with high decision regret were insufficient receipt of treatment information, low involvement in decision making, and a desire for more involvement.
Conclusions
Partners were generally positive regarding their perspectives about participating in the breast cancer treatment decision-making process. However, less acculturated Hispanic partners were most vulnerable to decision regret. In addition, high decision regret was associated with modifiable elements of the decision-making process.
Implications for Nursing
Attention should be paid to ensuring racial and ethnic minority partners are sufficiently involved in breast cancer treatment decisions and receive decision support.
Keywords: decision making, family and caregivers, breast cancer
A breast cancer diagnosis requires a series of complex treatment decisions related to type of treatment and side-effect profile. Research findings suggest that, for some women, these decisions are made with inadequate knowledge about the risks and benefits of treatment options (Fagerlin et al., 2006; Hawley, Fagerlin, Janz, & Katz, 2008; Janz et al., 2008). These decisions may be made in haste (Frosch & Elwyn, 2011) and can result in significant decision regret, distress, or remorse, which is true particularly for vulnerable patients such as racial and ethnic minorities (Brehaut et al., 2003; Hawley, Janz, et al., 2008; Sheehan, Sherman, Lam, & Boyages, 2007). The Institute of Medicine's (2001) definition of patient-centered care includes recognizing patients’ medical needs while also incorporating their preferences and allowing them to guide decisions. This definition has been expanded to highlight the importance of significant others in medical decision making (Conway et al., 2006; Edgman-Levitan, 2003; Epstein & Street, 2011; Johnson et al., 2008; Shaller, 2007). However, little empirical research exists focusing on the contribution of significant others to the breast cancer treatment decision-making process.
Although women with breast cancer have reported valuing the opinions of others across the continuum of breast cancer treatment (Gilbar & Gilbar, 2009; Hawley et al., 2009; Öhlén, Balneaves, Bottorff, & Brazier, 2006; Stiggelbout et al., 2007), studies suggest that the involvement and influence of others may vary among different racial and ethnic groups. For instance, the research team previously found that Latina patients more often reported strong influences of family and friends in treatment decisions; however, Caucasian patients more often reported the strong influence of their spouses (Hawley et al., 2009). Maly, Umezawa, Leake, and Silliman (2004) also found that Latina patients reported a stronger influence of family and friends than other racial and ethnic groups. In contrast, research findings suggested that African American patients more often turned to spiritual sources (e.g., attending church, church-sponsored groups) for decision-making support (Banning, 2011; Gallia & Pines, 2009) than other racial and ethnic groups.
Previous studies evaluating the impact of significant others in breast cancer treatment decision making are limited by small sample sizes and little racial and ethnic diversity (Duric et al., 2008; Gilbar & Gilbar, 2009). In addition, although previous studies have assessed partners’ experiences of breast cancer treatment (Sandham & Harcourt, 2007), no large studies have examined the perspectives of significant others related to a specific treatment decision-making process. Because no conceptual frameworks specifically outline the role of others in treatment decision making, the underlying conceptual framework for the current research is based on a larger conceptual framework developed by Northouse, Katapodi, Song, Zhang, and Mood (2010), which attempts to understand caregiving and communication among couples dealing with cancer. This larger framework suggests that both patient and partner factors contribute to positive communication and stronger relationships; the authors have adapted this framework to posit that both patient and partner factors contribute to positive decision making (i.e., greater decision satisfaction and less decision regret) in cancer treatment, and propose that more involved and engaged partners contribute to better patient decision outcomes. The current study is focused only on one component of the framework, specifically on developing a deeper understanding of partner perspectives regarding their role in the treatment decision-making process.
The authors surveyed the partners of a population-based sample of women with breast cancer with the following objectives: (a) to characterize racial and ethnic differences in partner-perceived experience with elements of the decision-making process; (b) to evaluate the racial and ethnic distribution of partner-reported decision regret; and (c) to evaluate associations between partner decision regret, race and ethnicity, and elements of the decision-making process. Future work that builds from the current study will evaluate the role of patient and partner factors on the use of different breast cancer treatments, enabling oncology nurses and other providers to deliver care that is centered more fully on the needs and preferences of patients and their partners.
Methods
Sample and Data Collection
From June 2005 to February 2007, various women diagnosed with non-metastatic breast cancer reported to the Surveillance, Epidemiology, and End Results (SEER) registry locations in Los Angeles, CA, and Detroit, MI, and participated in a baseline survey about their breast cancer treatment experiences. African American and Latina (in Los Angeles) women were oversampled and Asian/Pacific Islander patients were excluded (because of simultaneous research studies). Of the 3,133 eligible women, 2,290 returned a survey on average nine months postdiagnosis (73% response rate). Respondents had to be able to complete the survey in English or Spanish; those with Spanish surnames and identified using a U.S. census list (Word & Perkins, 1996) were sent materials in both languages. Respondents from the 2005–2007 Time 1 survey were surveyed again about four years later (Time 2 survey). Of the original 2,290 respondents, 1,590 responded to the Time 2 survey (70% response rate). Details of the Time 1 survey have been previously published (Hawley et al., 2009; Hawley, Fagerlin, et al., 2008; Hawley, Janz, et al., 2008).
For this study, women who reported being married or partnered at both Time 1 and 2 were identified. From October 2010 to February 2012, a mailing was sent to these women requesting that they give the enclosed packet to their partners. The partner packet included an introductory letter signed by the study team, a survey, and a $10 cash gift. As with the patient surveys, all materials were sent in both English and Spanish to patients with Spanish surnames. A modified Dillman Method (Anema & Brown, 1995) was used to follow-up. If no response was received, partners were called a minimum of five times within 2–3 weeks of the mailing, sent second copies of materials, and eventually offered a phone interview (Spanish-speaking interviewers were offered).
The research followed established protocols of the SEER registries in Los Angeles and Detroit for population-based research. The study protocol was approved by the institutional review boards of the University of Michigan, Wayne State University, and the University of Southern California.
Measures
Elements of the decision-making process
Three components of partner perspectives were evaluated regarding partners’ experiences with the breast cancer treatment decision-making process: (a) sufficient receipt of information about risks and benefits of treatment options, (b) actual decision involvement, and (c) perception of sufficient decision involvement.
Sufficient information receipt
Partners responded to two items asking whether they had received enough information about: (a) the risks and benefits of surgical treatment options, and (b) the risks and benefits of radiation treatment. Because this question was focused on initial management of breast cancer, the risks and benefits of chemotherapy were not included in the question. A summary measure was created using these two items with a Cronbach alpha of 0.72. A dichotomous variable was then created to capture whether partners had not received sufficient information across both of the treatment options. Therefore, partners who responded “yes” to both information questions were classified as being sufficiently informed, and partners who responded “no” to either both or one information question were classified as not being sufficiently informed.
Actual decision involvement
Partner reports of their actual involvement in the decision-making process were measured as the mean response to two questions on a five-point Likert-type scale, from 1 (not at all involved) to 5 (very involved): “How involved were you in the decision about what surgery she would have (that is, lumpectomy or mastectomy)?” and “How involved were you in other treatment decisions (e.g., radiation therapy, chemotherapy)?” An overall summary measure was created, with higher scores indicating higher involvement. This measure had a Cronbach alpha of 0.92. The authors were primarily interested in the factors associated with low levels of involvement; therefore, that variable was dichotomized into low versus high based on the distribution of the scale.
Sufficient decision involvement
A third decision-making process variable addressed whether partners felt their actual involvement in treatment decisions (regardless of whether it was low or high) was sufficient for them. This was assessed using a two-item scale where each item had a “yes or no” response option: “Would you have liked to have been more involved in the decision about what surgery she would have (that is, lumpectomy or mastectomy)?” and “Would you have liked to have been more involved in other treatment decisions (e.g., radiation therapy, chemotherapy)?”. An overall summary measure was created, with higher scores indicating less sufficient involvement. This measure had a Cronbach alpha of 0.9. Consistent with the approach to partner level of involvement, the authors were interested in the factors associated with being insufficiently involved. Partners who responded “yes” to either both or one question were classified as being insufficiently involved, and partners who responded “no” to both questions were classified as being sufficiently involved.
Decision regret
Partner-reported decision regret was evaluated by adapting the validated decision regret scale (Cronbach alpha = 0.81–0.92) (Brehaut et al., 2003) used by the research team in prior work with patient populations (Alderman et al., 2009; Hawley, Janz, et al., 2008). The scale included five items using a five-point Likert-type response scale ranging from 1 (strongly disagree) to 5 (strongly agree): (a) I wish she would have made a different decision about what type of surgery to have, (b) I wish she would have chosen a different surgeon to perform her surgery, (c) I wish she would have taken more time to make decisions about her treatment, (d) I wish she would have consulted more doctors about her treatment before making a decision, and (e) I would have her do everything the same (reverse coded). The decision-regret scale had a Cronbach alpha of 0.85, with higher values indicating higher decision regret. For the purposes of the current study, the authors were interested in factors associated with high decision regret, and created a dichotomous measure of decision regret (low versus high) based on an 80% cutoff.
Individual characteristics
Partners reported their race (Caucasian, African American, American Indian or Alaska Native, Asian or Pacific Islander, or other), and if they were Hispanic/Latino. To measure acculturation for Hispanics, the Short Acculturation Scale for Hispanics (SASH) was included in surveys sent to those with Spanish surnames (Marín, Sabogal, VanOss Marín, Otero-Sabogal, & Pérez-Stable, 1987). This method has reliably identified level of acculturation (Cronbach alpha = 0.9 overall for both language versions) among Spanish-speaking patients with cancer in previous studies (Hamilton et al., 2009; Hawley et al., 2009; Hawley, Janz, et al., 2008; Mujahid et al., 2009). The four-item SASH measures language preference (Spanish versus English) in different contexts: (a) reading or speaking, (b) thinking, (c) at home, and (d) with friends. The SASH is on a five-point Likert-type scale from 1 (only English) to 5 (only Spanish). A mean language preference score was calculated, and scores were dichotomized into a final acculturation variable; scores of four or greater were categorized as “less acculturated,” and scores of less than four were categorized as “more acculturated.” Conceptually, the SASH supports acculturation as a unidimensional construct: less-acculturated Hispanics are more immersed in their culture of origin, and more-acculturated Hispanics are more immersed in the dominant or host culture (Cabassa, 2003; Cuellar, Arnold, & Maldonado, 1995). Race and ethnicity were categorized into the following groups: Caucasian, African American, less-acculturated Hispanics, more-acculturated Hispanics, and other.
Additional demographics included age, annual household income, employment status, and education. Analyses also assessed partners’ self-reported attendance at the breast cancer appointments, which was assessed with a single item on a five-point Likert-type scale ranging from 1 (not at all) to 5 (a lot): “How often did you go with her to her doctor appointments where discussions about her treatment plan were discussed?” Response categories were dichotomized: attended rarely (score 1–3) versus attended often (score 4–5).
Statistical Analyses
Descriptive statistics were used to characterize the distribution of sociodemographic variables and to describe racial and ethnic differences in decision-making process variables and high decision regret. The authors examined the relationship among high decision regret (versus low), race and ethnicity, and the decision-making process variables using multivariable regression, designing three models. Model 1 evaluated the association between high decision regret and race and ethnicity controlling for other sociodemographic variables. Model 2 included all variables in Model 1, plus sufficient information receipt. Model 3 included all variables in Models 1 and 2, and added the remaining decision-making process variables (actual decision involvement and sufficient involvement). In each model, analyses controlled for the type of surgical treatment (i.e., mastectomy, double mastectomy, or lumpectomy) received by the patient. The authors reran all models, including revised measures of decision involvement (actual and sufficient), which excluded the chemotherapy question because the question about sufficient information did not ask about chemotherapy. All analyses were conducted using STATA®, version 11.0.
Results
Sample
The final sample for analysis comprised 517 partners (73% response rate) (see Table 1). The majority were men who had attended at least some college. Sixty-eight percent of partners reported attending appointments often.
Table 1.
Sample Characteristics (N = 517)
| Characteristic | n | % |
|---|---|---|
| Age (years)a | ||
| 49 and younger | 61 | 12 |
| 50–64 | 208 | 40 |
| 65 and older | 232 | 45 |
| Race and ethnicity | ||
| Caucasian | 295 | 59 |
| African American | 66 | 13 |
| Hispanic (high acculturation) | 54 | 11 |
| Hispanic (low acculturation) | 69 | 14 |
| Other | 19 | 4 |
| Level of education | ||
| Some high school or less | 72 | 14 |
| High school graduate | 84 | 17 |
| Some college | 149 | 30 |
| College graduate or more | 191 | 38 |
| Employment status | ||
| Full-time | 214 | 42 |
| Part-time | 36 | 7 |
| Retired | 211 | 41 |
| Unemployed, student, or disabled | 48 | 9 |
| Annual income ($) | ||
| Less than 40,000 | 112 | 25 |
| 40,000–89,999 | 173 | 39 |
| 90,000 or greater | 162 | 36 |
| Attendance at appointment | ||
| Often | 344 | 68 |
| Rarely | 163 | 32 |
X̄ = 62.3, SD = 11.1
Note. Because of missing values, not all totals equal N.
Note. Because of rounding, not all percentages total 100.
Racial and Ethnic Differences in Decision-Making Process Variables
Partner perspectives about their experiences with the treatment decision-making process included (a) sufficient receipt of information about risks and benefits of treatment options, (b) involvement in the treatment decisions, and (c) feeling sufficiently involved in the treatment decisions. Overall, the majority of partners reported that they received sufficient information about breast cancer treatment (77%), were involved in the treatment decisions (72%), and that their involvement was sufficient (73%). In addition, 68% of partners reported attending visits with the patient often, and this did not significantly differ by race and ethnicity.
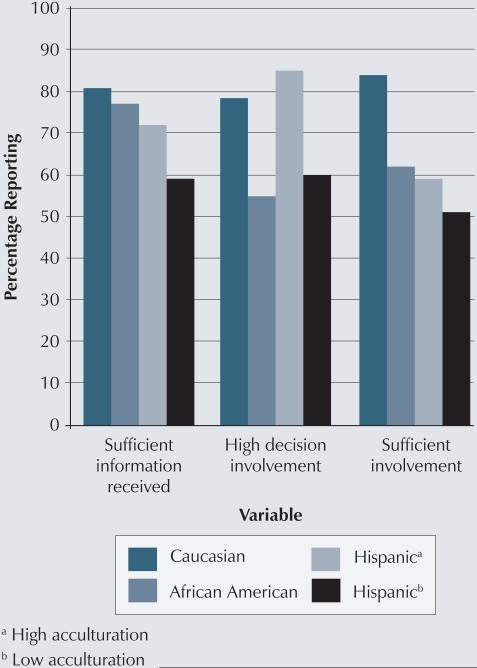
Despite these generally positive appraisals of the decision process, significant racial and ethnic differences existed across each decision-making process variable, specifically Hispanic partners (see Figure 1). For instance, 59% of less-acculturated Hispanic partners reported sufficient information receipt compared to 82% of Caucasians, 77% of African Americans, and 72% of more-acculturated Hispanic partners (χ2 = 18.7, p = 0.001). Partner reports of decision involvement varied, with more-acculturated Hispanic partners reporting high involvement more often (85%) than all other groups (79% for Caucasian partners, 60% for less-acculturated Hispanic partners, and 57% for African American partners) (χ2 = 25.7, p < 0.001). Regardless of actual involvement, Caucasian partners reported being sufficiently involved most often (84%), followed by African Americans (64%), more-acculturated Hispanics (59%), and less-acculturated Hispanics (52%) (χ2 = 44.2, p < 0.001).
Figure 1.
Decision-Making Process Variables by Race and Ethnicity
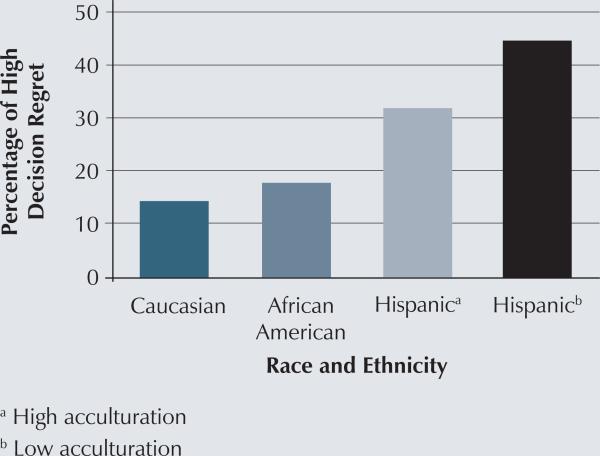
Racial and Ethnic Differences in High Decision Regret
Twenty-two percent of partners reported high decision regret surrounding breast cancer treatment decision making. However, as seen in Figure 2, high decision regret was reported disproportionately across racial and ethnic groups.
Figure 2.
Proportion of Partners Reporting High Decision Regret by Race and Ethnicity
Factors Associated With High Decision Regret
Table 2 presents the logistic regression results assessing the association among high decision regret, race and ethnicity, and the other decision-making process variables, controlling for demographics and attendance at appointments. Model 1 found that, when compared to their Caucasian counterparts, less-acculturated Hispanic partners were more than three times as likely to report high (versus low) decision regret (overall regret [OR] = 3.59, 95% CI [1.48, 8.7], p = 0.005) controlling for other demographic factors and attendance at appointments. In Model 2, which added the sufficient information receipt variable, less-acculturated Hispanic partners were still significantly more likely to report higher decision regret than Caucasian partners (OR = 3.06, 95% CI [1.23, 7.64], p = 0.016). Partners with insufficient treatment information were more likely to have high (versus low) decision regret (OR = 3.14, 95% CI [1.83, 5.39], p < 0.001). After including all decision-making process variables in the model (Model 3), less-acculturated Hispanic partners remained more likely to report high decision regret than Caucasian partners (OR = 2.94, 95% CI [1.13, 7.64], p = 0.027). Insufficient information receipt remained significantly associated with high decision regret (OR = 2.56, 95% CI [1.44, 4.55], p = 0.001). In addition, partners who reported both low actual involvement and insufficient involvement were more likely to report high (versus low) decision regret (OR = 2.22, 95% CI [1.19, 4.14], p = 0.012 and OR = 2.27, 95% CI [1.28, 4.02], p = 0.005, respectively). When the authors ran the models using the revised measures of involvement that excluded chemotherapy, they did not obtain significantly different results between the groups that did and did not include the chemotherapy question.
Table 2.
Association of Partner High Decision Regret, Race and Ethnicity, and Elements of Decision Making
| Model 1a (N = 447) |
Model 2b (N = 447) |
Model 3c (N = 438) |
|
|---|---|---|---|
| Variable | OR (95% CI) High Versus Low | OR (95% CI) High Versus Low | OR (95% CI) High Versus Low |
| Race and ethnicity | |||
| Caucasian | Referent | Referent | Referent |
| African American | 0.86 [0.37, 1.98] | 0.84 [0.36, 1.96] | 0.64 [0.27, 1.56] |
| Hispanic (high acculturation) | 2.03 [0.79, 5.2] | 1.74 [0.66, 4.59] | 1.76 [0.65, 4.82] |
| Hispanic (low acculturation) | 3.59 [1.48, 8.7]** | 3.06 [1.23, 7.64]* | 2.94 [1.13, 7.64]* |
| Sufficient information receipt | |||
| Yes | Referent | Referent | |
| No | 3.14 [1.83, 5.39]*** | 2.56 [1.44, 4.55]** | |
| Decision involvement | |||
| High | Referent | ||
| Low | 2.22 [1.19, 4.14]* | ||
| Sufficient involvement | |||
| Yes | Referent | ||
| No | 2.27 [1.28, 4.02]** |
p < 0.05
p < 0.01
p < 0.001
Demographics
Demographics and information
Demographics, information, and involvement
CI—confidence interval; OR—overall regret
Note. Models controlled for attendance at appointments, employment, income, education, age, study site, and patient treatment.
Discussion
To the authors’ knowledge, this study is the first to evaluate the perspectives of partners of women with breast cancer regarding their role in treatment decision making using a large and racially and ethnically diverse population-based sample. The results suggest that most partners positively appraised their experiences across elements of the treatment decision-making process, as the majority reported receiving sufficient information, having a high amount of actual involvement in the decision process, and feeling that this amount of involvement was sufficient for them. In addition, 21% reported high decision regret. These findings are consistent with results from smaller and less racially and ethnically diverse studies in which husbands or partners felt it was important to receive adequate information about treatments (Adams, Boulton, & Watson, 2009; Hilton, Crawford, & Tarko, 2000; Kilpatrick, Kristjanson, Tataryn, & Fraser, 1998; Meissner, Anderson, & Odenkirchen, 1990; Rees & Bath, 2000; Sandham & Harcourt, 2007). However, few studies assess partner appraisals of their own involvement in treatment decision making with which to compare the current results.
However, the results suggest that racial and ethnic variation does exist in the experiences of partners with minority partners appearing most vulnerable to poor decision outcomes, particularly less-acculturated Hispanics. These results were consistent with those obtained in previous research, where the authors found that the less-acculturated Latina patients most often reported low decision involvement and high decision regret (Hawley, Janz, et al., 2008). The less-acculturated Hispanic partners, who were primarily Spanish speaking, may have had difficulty understanding the treatment information provided during the decision-making process. In addition, the information provided may not have been culturally sensitive or linguistically appropriate, which are important elements in effective health information (Arora et al., 2002; Aziz & Rowland, 2002; Moore & Butow, 2004).
To the best of the researchers’ knowledge, this study is the first to describe partner-reported decision regret related to specific elements of decision making for treatment of breast cancer and to link this regret with elements of decision making. Understanding decision outcomes, including decision regret, of the partners of women with breast cancer has important implications for effective coping and communication between women and their partners following treatment completion. Helping ensure that both partners and women with breast cancer have positive decision-making processes and low levels of decision regret may be one method for ensuring less distress in these couples. The framework for the current study focused on partner factors in positive breast cancer treatment decision making; in particular, how more involved and engaged partners contribute to better patient decision outcomes, as part of a larger conceptual framework of patient and partner factors (Northouse et al., 2010). The results linked high decision regret with modifiable elements of decision making, which support that framework. In particular, receiving sufficient information and obtaining the right amount of involvement in decision making suggest a mechanism for achieving low decision regret in partners as well as women with breast cancer. Oncology clinicians, including nurses and physicians, need to understand the associations among these decision elements so that they can recommend that couples engage in focused discussion of decision options prior to making a final treatment choice.
The majority of educational interventions and decision aids in breast cancer have been focused on patients alone. However, Northouse et al. (2010) found that an intervention delivered to a person with cancer and his or her spouse resulted in positive impact on communication between the couple. Cochrane, Lewis, and Griffith (2011) suggested that delivering an intervention focused on helping the patient understand and deal with the breast cancer diagnosis and treatment delivered directly to the partner or spouse of a patient with cancer can have a positive benefit on the patient. The current results suggest the need to study the concordance between the perspective of the woman with cancer and the perspective of the partner to better inform decision-making interventions that are delivered to people with cancer and partners together.
The current study has some limitations that should be noted. The cross-sectional design did not allow for examining whether partner perceptions of the decision-making process are related to decision regret over time, an important area for future research given the temporal nature of decision regret (Gilovich & Medvec, 1995). The authors also could not tell if respondents were reporting their regret with the decision process itself, as intended, or their regret with how they contributed to the decision process. The responses may be subject to recall bias given the timing of the survey. The sufficient information receipt measure was focused on initial management of cancer, and did not include knowledge about risks and benefits associated with chemotherapy. In addition, results were obtained from partners in two geographic areas and cannot be generalized to all partners of women with breast cancer, particularly those in rural locations. Although the authors obtained a high response rate from partners (73%), the overall sample of partners was still relatively small (N = 517). Finally, although this was the first study to use the SEER registry to identify and survey a nonpatient sample, the authors only included partners and did not recruit others who may be involved in the decision-making process (e.g., children, siblings, close friends), particularly for unmarried patients.
Implications for Nursing Practice
Despite the limitations, the results have implications for nursing practice. The current findings suggest that, because racial and ethnic variation exists in the involvement and role of partners in decision making, oncology clinicians caring for diverse populations should consider the cultural appropriateness of their educational materials (Betancourt, Green, Carrillo, & Park, 2005). In addition, because research also has shown variability in preferences for and actual involvement across racial and ethnic groups (Betancourt et al., 2005; Maly, Umezawa, Ratliff, & Leake, 2006; Surbone, 2008), oncology clinicians may need to assess the desire for partner involvement in treatment decisions among patients and partners early in the decision process.
The results also provide support for the delivery of decision support interventions to the partners of patients with breast cancer or to patient-partner dyads. In-corporating sufficient information about treatment options as well as focusing decision support interventions on how patients and partners can obtain their desired amount of involvement in the decision process may reduce decision regret in couples, which ultimately may lead to better communication, less psychosocial distress, and better quality of life for both patients and their partners (Cochrane et al., 2011; Lewis et al., 2008; Northouse et al., 2010). The current study could be an opportunity for oncology nurses to improve the decision-making process for patients and partners.
Knowledge Translation.
Most partners of patients with breast cancer positively appraise their role in the treatment decision process.
Oncology clinicians should be aware that racial and ethnic variation exists in partner involvement throughout the decision-making process, with less acculturated Latinos reporting least involvement and most decision regret.
Decision-support interventions may need to target patients with breast cancer and their partners to be most effective for improving the decision process.
Footnotes
No financial relationships to disclose.
Contributor Information
Sarah E. Lillie, Minneapolis Veterans Affairs Medical Center in Minnesota.
Nancy K. Janz, Department of Health Behavior and Health Education, at the University of Michigan in Ann Arbor.
Christopher R. Friese, School of Nursing, at the University of Michigan in Ann Arbor.
John J. Graff, Cancer Institute of New Jersey and Robert Wood Johnson Medical School in New Brunswick, NJ.
Kendra Schwartz, Department of Family Medicine at Wayne State University in Detroit, MI.
Ann S. Hamilton, Department of Preventive Medicine at the University of Southern California in Los Angeles.
Brittany Bartol Gay, Department of Internal Medicine at the University of Michigan.
Steven J. Katz, Department of Internal Medicine at the University of Michigan and Ann Arbor Veterans Affairs Healthcare System..
Sarah T. Hawley, Department of Internal Medicine at the University of Michigan and Ann Arbor Veterans Affairs Healthcare System..
References
- Adams E, Boulton M, Watson E. The information needs of partners and family members of cancer patients: A systematic literature review. Patient Education and Counseling. 2009;77:179–186. doi: 10.1016/j.pec.2009.03.027. [DOI] [PubMed] [Google Scholar]
- Alderman AK, Hawley ST, Janz NK, Mujahid MS, Morrow M, Hamilton AS, Katz SJ. Racial and ethnic disparities in the use of postmastectomy breast reconstruction: Results from a population-based study. Journal of Clinical Oncology. 2009;27:5325–5330. doi: 10.1200/JCO.2009.22.2455. doi:10.1200/JCO.2009.22.2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anema MG, Brown BE. Increasing survey responses using the total design method. Journal of Continuing Education in Nursing. 1995;26:109–114. doi: 10.3928/0022-0124-19950501-06. [DOI] [PubMed] [Google Scholar]
- Arora NK, Johnson P, Gustafson DH, McTavish F, Hawkins RP, Pingree S. Barriers to information access, perceived health competence, and psychosocial health outcomes: Test of a mediation model in a breast cancer sample. Patient Education and Counseling. 2002;47:37–46. doi: 10.1016/s0738-3991(01)00170-7. doi:10.1016/S0738-3991(01)00170-7. [DOI] [PubMed] [Google Scholar]
- Aziz NM, Rowland JH. Cancer survivorship research among ethnic minority and medically underserved groups. Oncology Nursing Forum. 2002;29:789–801. doi: 10.1188/02.ONF.789-801. doi:10.1188/02.ONF.789-801. [DOI] [PubMed] [Google Scholar]
- Banning M. Black women and breast health: A review of the literature. European Journal of Oncology Nursing. 2011;15:16–22. doi: 10.1016/j.ejon.2010.05.005. [DOI] [PubMed] [Google Scholar]
- Betancourt JR, Green AR, Carrillo JE, Park ER. Cultural competence and health care disparities: Key perspectives and trends. Health Affairs. 2005;24:499–505. doi: 10.1377/hlthaff.24.2.499. doi:10.1377/hlthaff.24.2.499. [DOI] [PubMed] [Google Scholar]
- Brehaut JC, O'Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, Feldman-Stewart D. Validation of a decision regret scale. Medical Decision Making. 2003;23:281–292. doi: 10.1177/0272989X03256005. [DOI] [PubMed] [Google Scholar]
- Cabassa LJ. Measuring acculturation: Where we are and where we need to go. Hispanic Journal of Behavioral Sciences. 2003;25:127–146. doi:10.1177/0739986303025002001. [Google Scholar]
- Cochrane BB, Lewis FM, Griffith KA. Exploring a diffusion of benefit: Does a woman with breast cancer derive benefit from an intervention delivered to her partner? Oncology Nursing Forum. 2011;38:207–214. doi: 10.1188/11.ONF.207-214. doi:10.1188/11.ONF.207-214. [DOI] [PubMed] [Google Scholar]
- Conway J, Johnson B, Edgman-Levitan S, Schlucter J, Ford D, Sodomka P, Simmons L. Partnering with patients and families to design a patient- and family-centered health care system: A roadmap for the future. 2006 Retrieved from http://www.ipfcc.org/pdf/Roadmap.pdf.
- Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: A revision of the original ARSMA scale. Hispanic Journal of Behavioral Sciences. 1995;17:275–304. [Google Scholar]
- Duric VM, Butow PN, Sharpe L, Heritier S, Boyle F, Beith J, Stockler MR. Comparing patients’ and their partners’ preferences for adjuvant chemotherapy in early breast cancer. Breast Cancer Research and Treatment. 2008;72:239–245. doi: 10.1016/j.pec.2008.02.021. [DOI] [PubMed] [Google Scholar]
- Edgman-Levitan S. Healing partnerships: The importance of including family and friends. In: Frampton S, Gilpin L, Charmel P, editors. Putting patients first. Jossey-Bass; San Francisco, CA: 2003. pp. 51–69. [Google Scholar]
- Epstein RM, Street RL. The values and value of patient-centered care. Annals of Family Medicine. 2011;9:100–103. doi: 10.1370/afm.1239. doi:10.1370/ afm.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerlin A, Lakhani I, Lantz PM, Janz NK, Morrow M, Schwartz K, Katz SJ. An informed decision? Breast cancer patients and their knowledge about treatment. Patient Education and Counseling. 2006;64:303–312. doi: 10.1016/j.pec.2006.03.010. doi:10.1016/j.pec.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Frosch DL, Elwyn G. I believe, therefore I do. Journal of General Internal Medicine. 2011;26:2–4. doi: 10.1007/s11606-010-1560-1. doi:10.1007/s11606-010-1560-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallia KS, Pines EW. Narrative identity and spirituality of African American church women surviving breast cancer survivors. Journal of Cultural Diversity. 2009;16:50–55. [Google Scholar]
- Gilbar R, Gilbar O. The medical decision-making process and the family: The case of breast cancer patients and their husbands. Bioethics. 2009;23:183–192. doi: 10.1111/j.1467-8519.2008.00650.x. doi:10.1111/j.1467-8519.2008.00650.x. [DOI] [PubMed] [Google Scholar]
- Gilovich T, Medvec VH. The experience of regret: What, when, and why. Psychological Review. 1995;102:379–395. doi: 10.1037/0033-295x.102.2.379. doi:10.1037/0033 -295X.102.2.379. [DOI] [PubMed] [Google Scholar]
- Hamilton AS, Hofer TP, Hawley ST, Morrell D, Leventhal M, Deapen D, Katz SJ. Latinas and breast cancer outcomes: Population-based sampling, ethnic identity, and acculturation assessment. Cancer Epidemiology, Biomarkers and Prevention. 2009;18:2022–2029. doi: 10.1158/1055-9965.EPI-09-0238. doi:10.1158/1055-9965.EPI-09-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley ST, Fagerlin A, Janz NK, Katz SJ. Racial/ethnic disparities in knowledge about risks and benefits of breast cancer treatment: Does it matter where you go? Health Services Research. 2008;43:1366–1387. doi: 10.1111/j.1475-6773.2008.00843.x. doi:10.1111/j.1475-6773.2008.00843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley ST, Griggs JJ, Hamilton AS, Graff JJ, Janz NK, Morrow M, Katz SJ. Decision involvement and receipt of mastectomy among racially and ethnically diverse breast cancer patients. Journal of the National Cancer Institute. 2009;101:1337–1347. doi: 10.1093/jnci/djp271. doi:10.1093/jnci/djp271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley ST, Janz NK, Hamilton A, Griggs JJ, Aldeman AK, Mujahid M, Katz SJ. Latina patient perspectives about informed treatment decision making for breast cancer. Patient Education and Counseling. 2008;73:363–370. doi: 10.1016/j.pec.2008.07.036. doi:10.1016/j.pec.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilton BA, Crawford JA, Tarko MA. Men's perspectives on individual and family coping with their wives’ breast cancer and chemotherapy. Western Journal of Nursing Research. 2000;22:438–459. doi: 10.1177/019394590002200405. doi:10.1177/019394590002200405. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Crossing the quality chasm: A new health system for the 21st century. National Academies Press; Washington, DC: 2001. [PubMed] [Google Scholar]
- Janz NK, Mujahid MS, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ. Racial/ethnic differences in adequacy of information and support for women with breast cancer. Cancer. 2008;113:1058–1067. doi: 10.1002/cncr.23660. doi:10.1002/cncr.23660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson B, Abraham M, Conway J, Simmons L, Edgman-Levitan S, Sodomka P, Ford D. Partnering with patients and families to design a patient- and family-centered health care system: Recommendations and promising practices. 2008 Retrieved from http://www.ipfcc.org/pdf/PartneringwithPatientsandFamilies.pdf.
- Kilpatrick MG, Kristjanson LJ, Tataryn DJ, Fraser VH. Information needs of husbands of women with breast cancer. Oncology Nursing Forum. 1998;25:1595–1601. [PubMed] [Google Scholar]
- Lewis FM, Cochrane BB, Fletcher KA, Zahlis EH, Shands ME, Gralow JR, Schmitz K. Helping her heal: A pilot study of an educational counseling intervention for spouses of women with breast cancer. Psycho-Oncology. 2008;17:131–137. doi: 10.1002/pon.1203. doi:10.1002/pon.1203. [DOI] [PubMed] [Google Scholar]
- Maly RC, Umezawa Y, Leake B, Silliman RA. Determinants of participation in treatment decision-making by older breast cancer patients. Breast Cancer Research and Treatment. 2004;85:201–209. doi: 10.1023/B:BREA.0000025408.46234.66. [DOI] [PubMed] [Google Scholar]
- Maly RC, Umezawa Y, Ratliff CT, Leake B. Racial/ethnic group differences in treatment decision making and treatment received among older breast carcinoma patients. Cancer. 2006;106:957–965. doi: 10.1002/cncr.21680. [DOI] [PubMed] [Google Scholar]
- Marín G, Sabogal F, VanOss Marín B, Otero-Sabogal F, Pérez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9:183–205. [Google Scholar]
- Meissner HI, Anderson DM, Odenkirchen JC. Meeting information needs of significant others: Use of the Cancer Information Service. Patient Education and Counseling. 1990;15:171–179. doi: 10.1016/0738-3991(90)90060-x. [DOI] [PubMed] [Google Scholar]
- Moore RJ, Butow P. Culture and oncology: Impact of context effects. Kluwer Academic; New York, NY: 2004. [Google Scholar]
- Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Research and Treatment. 2009;119:213–220. doi: 10.1007/s10549-009-0389-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians. 2010;60:317–339. doi: 10.3322/caac.20081. doi:10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öhlén J, Balneaves LG, Bottorff JL, Brazier ASA. The influence of significant others in complementary and alternative medicine decisions by cancer patients. Social Science and Medicine. 2006;63:1625–1636. doi: 10.1016/j.socscimed.2006.03.050. doi:10.1016/j.socscimed.2006.03.050. [DOI] [PubMed] [Google Scholar]
- Rees CE, Bath PA. Exploring the information flow: Partners of women with breast cancer, patients, and healthcare professionals. Oncology Nursing Forum. 2000;27:1267–1275. [PubMed] [Google Scholar]
- Sandham C, Harcourt D. Partner experiences of breast reconstruction post mastectomy. European Journal of Oncology Nursing. 2007;11:66–73. doi: 10.1016/j.ejon.2006.05.004. doi:10.1016/j.ejon.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Shaller D. Patient-centered care: What does it take? The Commonwealth Fund; Washington, DC: 2007. [Google Scholar]
- Sheehan J, Sherman KA, Lam T, Boyages J. Association of information satisfaction, psychological distress, and monitoring coping style with post-decision regret following breast reconstruction. Psycho-Oncology. 2007;16:342–351. doi: 10.1002/pon.1067. doi:10.1002/pon.1067. [DOI] [PubMed] [Google Scholar]
- Stiggelbout AM, Jansen SJT, Otten W, Baas-Thijssen MCM, van Slooten H, Van de Velde CJH. How important is the opinion of significant others to cancer patients’ adjuvant chemotherapy decision-making? Supportive Care in Cancer. 2007;15:319–325. doi: 10.1007/s00520-006-0149-z. doi:10.1007/s00520-006-0149-z. [DOI] [PubMed] [Google Scholar]
- Surbone A. Cultural aspects of communication in cancer care. Supportive Care in Cancer. 2008;16:235–240. doi: 10.1007/s00520-007-0366-0. [DOI] [PubMed] [Google Scholar]
- Word D, Perkins JR. Building a Spanish surname list for the 1990's—A new approach to an old problem. U.S. Census Bureau; Washington, DC: 1996. [Google Scholar]