ABSTRACT
Background
Burnout is a common issue in internal medicine residents, and its impact on medical errors and professionalism is an important subject of investigation.
Objective
To evaluate differences in medical errors and professionalism in internal medicine residents with and without burnout.
Methods
A single institution observational cohort study was conducted between June 2011 and July 2012. Burnout was measured using the Maslach Burnout Inventory to generate subscores for the following 3 domains: emotional exhaustion, depersonalization, and sense of personal accomplishment. By convention, burnout was defined as a high emotional exhaustion or depersonalization subscore. Medication prescription error rate was the chosen measure of medical errors. Professionalism was measured cumulatively through examining discharge summaries completed within 48 hours, outpatient charts completed within 72 hours, and the average time to review outpatient laboratory tests.
Results
Of a total of 54 eligible first-year residents, 53 (98%) and 32 (59%) completed the initial and follow-up surveys, respectively. Residents with year-end burnout had a lower rate of medication prescription errors (0.553 versus 0.780, P = .007). Discharge summaries completed within 48 hours of discharge (83.8% versus 84.0%, P = .93), outpatient charts completed within 72 hours of encounter (93.7% versus 94.3%, P = .31), and time (minutes) to review outpatient laboratory test results (72.3 versus 26.9, P = .28) were similar between residents with and without year-end burnout.
Conclusions
This study found a small decrease in medical errors in residents with year-end burnout compared to burnout-free residents and no difference in selected measures of professionalism.
Introduction
Burnout in internal medicine (IM) resident physicians occurs commonly1–3 and may lead to depression and suboptimal medical care.1,3 Recently, there has been increasing attention to medical errors4,5 and professionalism in physicians.6–8 The Accreditation Council for Graduate Medical Education (ACGME) has addressed these concerns by mandating core competencies in practice-based learning and improvement and professionalism.9
The relationship between resident burnout, medical errors, and professionalism remains uncertain. Most studies of this population have relied on self-reported data. Few have examined objective correlates of burnout. One study measuring objective outcomes found that, while depressed pediatrics residents made more medical errors than their nondepressed peers, burnout was not associated with increased medical errors.10 Self-perceived medical errors have been correlated with burnout in IM residents,11 and self-reported unprofessional conduct has been associated with burnout in medical students.12 We conducted a study to examine our hypothesis that burnout in first-year IM residents correlates with selected objective measures of medical errors and professionalism.
Methods
All 54 first-year IM residents at the Icahn School of Medicine at Mount Sinai between June 2011 and July 2012 were eligible for this study. Internal medicine interns received surveys containing basic demographic information and the Maslach Burnout Inventory (MBI). Surveys were distributed first during orientation in June 2011 and a second time at year-end meetings and clinical sessions between April and June 2012.
Burnout was quantified using the MBI. This tool includes 22 questions covering 3 domains: emotional exhaustion, depersonalization, and sense of personal accomplishment. By convention, we defined burnout as a high emotional exhaustion or high depersonalization subscore using the MBI scaling algorithm. The instrument has some validity evidence for this population, setting, and purpose, based on a previously published study of 1104 medical personnel. It is commonly used for measuring burnout in medical trainees.13
We chose to measure inpatient medication prescription errors among first-year IM residents. Based on definitions from the published literature, prescription errors were defined as medication orders with the potential to cause adverse drug events.10 If followed, these medication orders may lead to dangerous interactions, inappropriate dosing, and incorrect or duplicate administration. At our hospital, a pharmacist reviews all electronic medication orders prior to dispensing medications and annotates orders that require additional clarification for safety. We reviewed all annotated orders by IM residents in our study and tallied those that had potential to cause an adverse drug event. This was measured per resident as a rate per 100 prescriptions.
Professionalism was assessed through 3 quality metrics: the percentage of inpatient discharge summaries completed within 48 hours of discharge; the percentage of outpatient charts completed within 72 hours of encounter; and the time to review outpatient laboratory studies in the electronic health record once resulted. The rationale for using these variables is that our residents are aware of the expectation to address these measures and should know that failure to do so would constitute an example of unprofessional behavior.
The authors obtained approval from our institution's Human Subject Research Review Board.
Our error and professionalism results were collected cumulatively between July 1, 2011, and June 30, 2012, and were compared between residents with and without burnout at the end of the study period. SAS statistical software version 9.3 for Windows (SAS Institute Inc, Cary, NC) was used to conduct t test comparisons to identify statistically significant differences between burnout and nonburnout groups after a Bonferroni correction (P < .013).
Results
Of the 54 eligible first-year residents, 53 (98%) completed an initial survey and 32 (59%) completed a follow-up survey. Burnout prevalence was 36% (19 of 53) at the beginning of intern year and 75% (24 of 32) at year-end.
We found a significant correlation (figure) between the cumulative rate of medication prescription errors and year-end burnout. Residents with year-end burnout had a lower cumulative error rate relative to their burnout-free counterparts (0.553 versus 0.780, P = .007).
Figure.
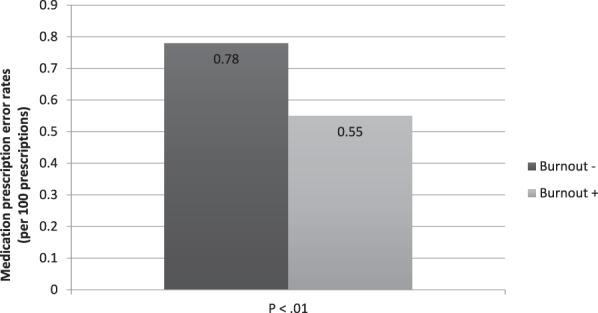
Medication Prescription Error Rates Measured Per 100 Prescriptions
Note: Bars distinguish between internal medicine residents without burnout (dark) and with burnout (light) at year-end.
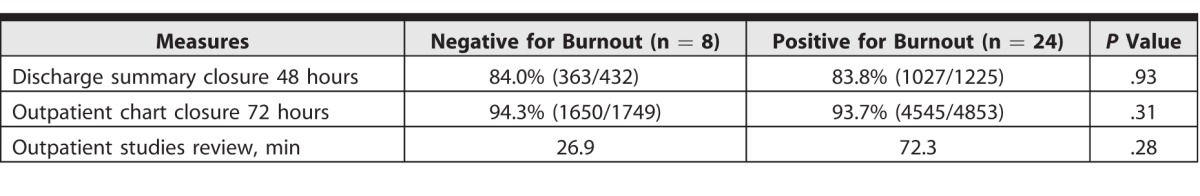
Residents with year-end burnout showed no significant differences (table) in the 3 measured domains of professionalism, compared with their burnout-free counterparts: percentage of discharge summaries completed within 48 hours of discharge (83.8% [1027 of 1225] versus 84.0% [363 of 432], P = .93); percentage of outpatient clinic charts closed within 72 hours of patient encounter (93.7% [4545 of 4853] versus 94.3% [1650 of 1749], P = .31); and time (minutes) to review outpatient diagnostic studies (72.3 versus 26.9, P = .28).
Table.
Data Summary for Chosen Measures of Professionalism at Year-End
We found similar results in the relationship between our cumulative performance measures and burnout measured at the onset of residency. There were also no differences noted when comparing residents who started and remained burnout-free with residents who began burnout-free and developed burnout over the course of the year.
Discussion
To the best of our knowledge, this is the first study examining the effect of burnout on objective medical errors and professionalism in IM residents. We found no correlation between resident burnout and our chosen measures of professionalism. Burnout was associated with a small decrease in the rate of medical errors; however, the rate was so low that the clinical significance is unclear. Our findings differ with other studies that found either no correlation10 or an increased rate of self-reported medical errors in burnt-out IM residents.3,11
One explanation for our findings is our chosen definition of medical errors. Other studies have defined medical errors as adverse events directly affecting patient care or related to errors in judgment.14–16 We chose our measure based on a preexisting pharmacy annotation system that tracked potential medication errors. Another hypothesis to consider in future studies is the possibility that committing medical errors can lead to stress and burnout.
One possibility for the lack of an observed correlation between burnout and professionalism is the adequacy of our professionalism assessment. There are many tools to assess professionalism.17,18 The 360 evaluation, for instance, utilizes multidisciplinary assessments to evaluate resident performance and has the potential for use in future research.19,20 Another possibility is that professionalism might be a characteristic that degrades last when residents experience burnout.21 There could also exist a relationship between burnout and professionalism in which unprofessional behavior leads to burnout. Our results could also represent a true finding: burnout in IM residents is not associated with increased medical errors or unprofessional behaviors.
Our study also showed a high rate of burnout at the onset of internship in IM residents. This finding is consistent with results in previous studies involving interns and fourth-year medical students.22,23
Limitations of our investigation include a small study population, single center study site, and loss of nearly 50% of the study to follow-up. We also observed a high burnout rate that limited our analysis due to the small burnout-free comparison group. Another limitation relates to the MBI, which in measuring depersonalization may actually detect a normal healthy amount of emotional detachment that young physicians need to develop in order to become effective providers. The instrument may therefore overestimate burnout in this population.1,2,21 Future study efforts that improve survey response rates might address this issue.
Conclusion
Our study found a small decrease in medical errors in residents with burnout compared to burnout-free residents; however, there was no difference in selected measures of professionalism. Future studies will likely benefit from larger, more diverse, multicenter investigations that examine additional objective measures.
References
- 1. Ripp J, Babyatsky M, Fallar R, et al. The incidence and predictors of job burnout in first-year internal medicine residents: a five-institution study. Acad Med. 2011; 86 10: 1304– 1310. [DOI] [PubMed] [Google Scholar]
- 2. Rosen IM, Gimotty PA, Shea JA, et al. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006; 81 1: 82– 85. [DOI] [PubMed] [Google Scholar]
- 3. Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002; 136 5: 358– 367. [DOI] [PubMed] [Google Scholar]
- 4. Gupta S. More treatment, more mistakes. The New York Times. July 31, 2012. http://www.nytimes.com/2012/08/01/opinion/more-treatment-more-mistakes.html?_r=0. Accessed March 2, 2016. [Google Scholar]
- 5. Marshall AP. How many die from medical mistakes in US hospitals? National Public Radio. September 20, 2013. http://www.npr.org/sections/health-shots/2013/09/20/224507654/how-many-die-from-medical-mistakes-in-u-s-hospitals. Accessed March 2, 2016. [Google Scholar]
- 6. Parker-Pope T. How professional is your doctor? The New York Times. December 3, 2007. http://well.blogs.nytimes.com/2007/12/03/how-professional-is-your-doctor/. Accessed March 2, 2016. [Google Scholar]
- 7. Chassin MR, Baker DW. Aiming higher to enhance professionalism: beyond accreditation and certification. JAMA. 2015; 313 18: 1795– 1796. [DOI] [PubMed] [Google Scholar]
- 8. Nasca TJ. Professionalism and its implications for governance and accountability of graduate medical education in the United States. JAMA. 2015; 313 18: 1801– 1802. [DOI] [PubMed] [Google Scholar]
- 9. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in clinical informatics. http://www.acgme.org/portals/0/pfassets/programrequirements/381_clinical_informatics_2016.pdf. Accessed June 16, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008; 336 7642: 488– 491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006; 296 9: 1071– 1078. [DOI] [PubMed] [Google Scholar]
- 12. Dyrbye LN, Massie FS, Jr, , Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010; 304 11: 1173– 1180. [DOI] [PubMed] [Google Scholar]
- 13. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 14. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014; 371 19: 1803– 1812. [DOI] [PubMed] [Google Scholar]
- 15. Garrouste-Orgeas M, Soufir L, Tabah A, et al. A multifaceted program for improving quality of care in intensive care units: IATROREF study. Crit Care Med. 2012; 40 2: 468– 476. [DOI] [PubMed] [Google Scholar]
- 16. Khoo EM, Sararaks S, Lee WK, et al. Reducing medical errors in primary care using a pragmatic complex intervention. Asia Pac J Public Health. 2015; 27 6: 670– 677. [DOI] [PubMed] [Google Scholar]
- 17. Lynch DC, Surdyk PM, Eiser AR. Assessing professionalism: a review of the literature. Med Teach. 2004; 26 4: 366– 373. [DOI] [PubMed] [Google Scholar]
- 18. Accreditation Council for Graduate Medical Education. The ACGME 2011 Duty Hour Standards: Enhancing Quality of Care, Supervision, and Resident Professional Development. https://www.acgme.org/acgmeweb/Portals/0/PDFs/jgme-monograph[1].pdf. Accessed March 2, 2016. [Google Scholar]
- 19. Brinkman WB, Geraghty SR, Lanphear BP, et al. Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial. Arch Pediatr Adolesc Med. 2007; 161 1: 44– 49. [DOI] [PubMed] [Google Scholar]
- 20. Lockyer J. Multisource feedback in the assessment of physician competencies. J Contin Educ Health Prof. 2003; 23 1: 4– 12. [DOI] [PubMed] [Google Scholar]
- 21. Orton P, Orton C, Pereira Gray D. Depersonalised doctors: a cross-sectional study of 564 doctors, 760 consultations and 1876 patient reports in UK general practice. BMJ Open. 2012; 2: e000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ripp J, Fallar R, Babyatsky M, et al. Prevalence of resident burnout at the start of training. Teach Learn Med. 2010; 22 3: 172– 175. [DOI] [PubMed] [Google Scholar]
- 23. Dyrbye LN, Thomas MR, Huntington JL, et al. Personal life events and medical student burnout: a multicenter study. Acad Med. 2006; 81 4: 374– 384. [DOI] [PubMed] [Google Scholar]


