Abstract
We compared the short-term efficacy of rigid versus soft lateral wedge arch support (LWAS) insoles for patients with knee osteoarthritis (OA), as assessed using the International Classification of Functioning, Disability and Health (ICF) system, through a prospective, double-blind, randomized controlled trial.
Participants who fulfilled the combined radiographic and clinical criteria for knee OA, as defined by the American College of Rheumatology, were randomly prescribed 1 pair of rigid or soft LWAS insoles. Body functions and structures were evaluated according to Kellgren–Lawrence scores, the Foot Posture Index, Hospital Anxiety and Depression Scale scores, the pain–pressure threshold, postural stability, dynamic balance, and fall risk; activities and participation were assessed according to 10-m fast speed walking, stair climbing and chair rising times, and Chronic Pain Grade questionnaire responses; and knee OA-related health status was evaluated using the Knee Injury and Osteoarthritis Outcome Score (KOOS). Hospital Anxiety and Depression Scale scores, the pain–pressure threshold, physical activity, balance, Chronic Pain Grade questionnaire responses, and the KOOS were recorded before treatment and at 1-, 2-, and 3-month follow-ups.
We enrolled 90 participants, 70 women and 20 men, with mean ages of 60.6 ± 10.8 and 63.1 ± 10.8 years in the rigid and soft LWAS insole groups, respectively. Repeated-measures analysis of covariance revealed significant time × group effect improvements in pain (P = 0.008 for the KOOS), stair ascent time (P = 0.003), daily living function (P = 0.003 for the KOOS), sports and recreation function (P = 0.012 for the KOOS), and quality of life (P = 0.021 for the KOOS) in the soft LWAS insole group.
Patients with knee OA who used soft LWAS insoles for a short term showed more significant improvement than did those who used rigid LWAS insoles in pain, physical activity, daily living function, sports and recreation function, and quality of life, which belong to the body functions and structures and the activities and participation components in the ICF scheme.
Keywords: effect, insoles, knee, osteoarthritis
1. Introduction
Osteoarthritis (OA) is the most common arthritic complaint among adults and a leading cause of chronic physical disability.[1] The prevalence of knee OA in the general population has ranged from 8.1% to 10% in previous studies.[2,3] Older women have a significantly higher prevalence of knee OA compared with older men.[4,5] Differences in endogenous sex hormones, body composition, knee structure and biomechanics, and psychosocial characteristics may play a role in the increased risk of knee OA in women.[6–8] Patients with knee OA experience pain, swelling, muscular atrophy, and restricted movement; these problems may negatively affect physical activity, causing difficulties in activities of daily living and reducing quality of life.[9]
The main treatment for knee OA entails controlling pain and avoiding potential complications of therapy.[10] OA is frequently associated with coronary artery disease, diabetes, obesity, and hypertension, and might be related to metabolic syndrome.[11] Patients with knee OA are likely to be older and may experience comorbidities; this patient group is at a relatively high risk of adverse gastrointestinal and cardiovascular effects of medication and polypharmacy.[12] Therefore, nonoperative treatments, such as shoe insoles, knee braces, and gait modification strategies, are commonly prescribed for patients with knee OA[13,14]; among them, insoles have become frequently used in recent years.[15–18] In Taiwan, 49.5% to 51% of rehabilitation services at physical medicine and rehabilitation clinics are provided for musculoskeletal and soft tissue diseases,[19,20] and knee OA accounts for 4.6%.[20]
The increased external knee adduction moment throughout the stance phase of patients with knee OA increases their medial knee joint loading during gait. Lateral wedges shift the center of pressure laterally, reducing the external knee adduction moment and knee adduction angular impulses, alleviating pain, and improving function in patients with knee OA.[21,22] However, patients with knee OA exhibit more pronated feet than do healthy people.[23] Therefore, lateral wedge insoles may aggravate pronation and the ankle invertor moment.[24,25] An increased invertor moment may further increase the demand on those muscles, thus causing fatigue after prolonged use of the insoles.[26] The purposes of adding arch support to lateral wedge insoles are reducing ankle eversion and diminishing the ankle invertor moment.[26]
Although Abdallah et al reported that using lateral wedge arch support (LWAS) insoles did not immediately reduce the knee adduction moment significantly in patients with knee OA,[26] Yeh et al and Nakajima et al have demonstrated the immediate reduction of the peak external knee adduction moment and knee pain.[25,27] Our recent study demonstrated that rigid LWAS insoles maintain the subtalar joint in a neutral position, thus providing immediate improvement in physical activity and medium-term reduction in pain and improvement in physical activity and function.[28] However, because of the lack of a control group, we could not exclude the possibility that the improvement was caused by the natural recovery process.
The International Classification of Functioning, Disability and Health (ICF) describes functional health conditions from a biopsychosocial perspective.[29] Functional health status is reflected by the dynamic interaction of ICF components including body functions and structures, activities, participation, and personal and environmental factors.[30] Clinical investigations of the efficacy of OA therapies should include body functions and structures (e.g., pain, depression, and balance), and activities and participation (e.g., physical activity, activities of daily living, functional performance, and knee OA-related health status).
According to our research, no study has compared the efficacy of rigid LWAS insoles with that of soft LWAS insoles by applying ICF components to evaluate patients wearing self-selected comfortable shoes. The present study compared the short-term clinical efficacy of the 2 types of insoles for patients with knee OA by using the ICF system in a randomized, double-blind design. We hypothesized that the short-term use of both types of LWAS insoles would improve scores in measures of body functions and structures as well as activities and participation.
2. Methods
This was a prospective, randomized, double-blind clinical study examining patients with knee OA. Participants with confirmed diagnoses of bilateral knee OA were recruited from the clinic of the Department of Physical Medicine and Rehabilitation at a teaching hospital in Taipei, Taiwan. All participants fulfilled the combined radiographic and clinical criteria for knee OA, as defined by the American College of Rheumatology.[31] Specifically, patients with Kellgren–Lawrence scores of 2 or higher in the medial compartment, based on anteroposterior radiographic views of both knees while bearing weight, were recruited for this study. The participants ranged in age from 40 to 85 years. We excluded patients with a self-reported history of malignancy, stroke, or knee implant operations and women who were pregnant or planned to become pregnant. The research was approved by the Institutional Review Board of Shin Kong Wu Ho-Su Memorial Hospital, and the study was performed in accordance with the World Medical Association Declaration of Helsinki. Informed consent was obtained from each participant. The trial was registered on ClinicalTrials.gov (registration number: NCT01765101; registration date: January 9, 2013) and conducted from January 2013 to December 2013.
2.1. Participant evaluation
Specific components of the ICF, namely, personal factors, body functions and structures (impairment), activities (limitations), and participation (restrictions), were evaluated as described herein.
2.2. Demographic data
Demographic data, namely, participant age, sex, education level, marital status, smoking and drinking habits, and comorbidities, were collected, and the body mass index was calculated.
2.3. Body functions and structures
Foot posture was evaluated using the Foot Posture Index,[32] which is used to assess weight-bearing foot posture in a standing position according to a composite score of clinical observational criteria. Foot posture can be classified as follows: highly pronated (+10 to +12), pronated (+6 to +9), normal (0 to +5), supinated (−1 to −4), and highly supinated (−5 to −12). The index exhibited high intrarater reliability.[29]
Psychological distress was assessed using the Hospital Anxiety and Depression Scale.[33] Questions focused on feelings, states, and symptoms experienced during the preceding week. The scale comprises two 7-item subscales designed to measure anxiety and depression. A score exceeding 7 indicates the presence of anxiety and/or depression. The scale showed high reliability and validity.[34]
The pain–pressure threshold was measured using a pressure algometer, which was placed over the medial knee joint, 2 to 3 cm medial to the medial–lateral corner of the patella, with a contact area of 1 cm2. Pressure was increased at a rate of 1 kg/s after force was vertically applied. The pain–pressure threshold was obtained by calculating the mean of 3 series of pain–pressure threshold assessments. The pain–pressure threshold was defined as the level of stimulation at which the participant first experiences a painful sensation.[25] The system exhibited high validity and reliability.[35]
Postural stability, dynamic balance, and fall risk were assessed using the Biodex Stability System,[36] which consists of an unstable platform for testing a patient's postural control and balance. The system can provide the degree of tilt of the platform along both the medial–lateral and anterior–posterior axes; thus, an overall stability index can be obtained. Higher scores indicate greater postural variability and less stability in balancing on the platform.[37] The Biodex Stability System evaluates dynamic balance by measuring limits of stability, which are recorded while the participants use their bodies to move a cursor on a monitor screen from a central box to peripheral boxes that appear randomly. Higher scores indicate greater control of dynamic balance.[38] The risk of falling was measured through 6 rounds of tests with varying levels of resistance. Higher scores indicate a greater risk of falling compared with those of sex- and age-matched normal controls.[38] The system has good inter-rater and intrarater reliability.[39,40] For safety, the participants adopted a bipedal stance on the platform, with their eyes open and feet bare. The feet positions were recorded to ensure the same stance throughout all future test sessions. Each participant was allowed 1 practice attempt, followed by 1 formal test for each assessment.
2.4. Activities and participation
Physical activity was measured through a 10-m walk test, a rising and sitting in a chair 5 times test, and a stair climb test. The tests were performed by asking participants to walk 10 m as fast as possible, to stand up and sit down on a standard chair 5 times without using their hands as quickly as possible, and to ascend and descend a flight of stairs (14 steps, and each step measured 18 cm in height) in the shortest time possible. The time taken to complete the tests was measured in seconds. A longer completion time indicates a greater limitation on physical activity.
The Chronic Pain Grade questionnaire containing 7 items was used to measure 3 subscales: pain intensity score, disability score, and disability point.[41] A higher score indicates greater symptoms and more severe disability. We used the disability score and disability point to assess for disability in the present study.
2.5. Knee OA-related health status
Participant perceptions of knee OA-related health status were assessed using the self-reported Knee Injury and Osteoarthritis Outcome Score (KOOS). A 5-point Likert scale was used to collect responses from the participants on 5 subscales: knee OA-related pain, other symptoms, daily living function, sports and recreation function, and knee-related quality of life.[42] Each scale ranges from 0 to 100, with 100 representing the least pain and dysfunction and 0 indicating the most pain and dysfunction. The system was reported to have high validity and reliability.[43]
2.6. Block randomization
After basic data were recorded and the aforementioned examinations were performed, the participants were allocated to either the rigid or the flexible LWAS insole group (Fig. 1). The principle of block randomization was used to assign the participants to the groups, with the block size being 4. Allocation was initially concealed. Sealed envelopes, 1 for each participant with the designated treatment group listed inside, were selected randomly when the participants were recruited for the study. One physician enrolled all participants, and another investigator generated the allocation sequence and assigned the participants to their groups.
Figure 1.
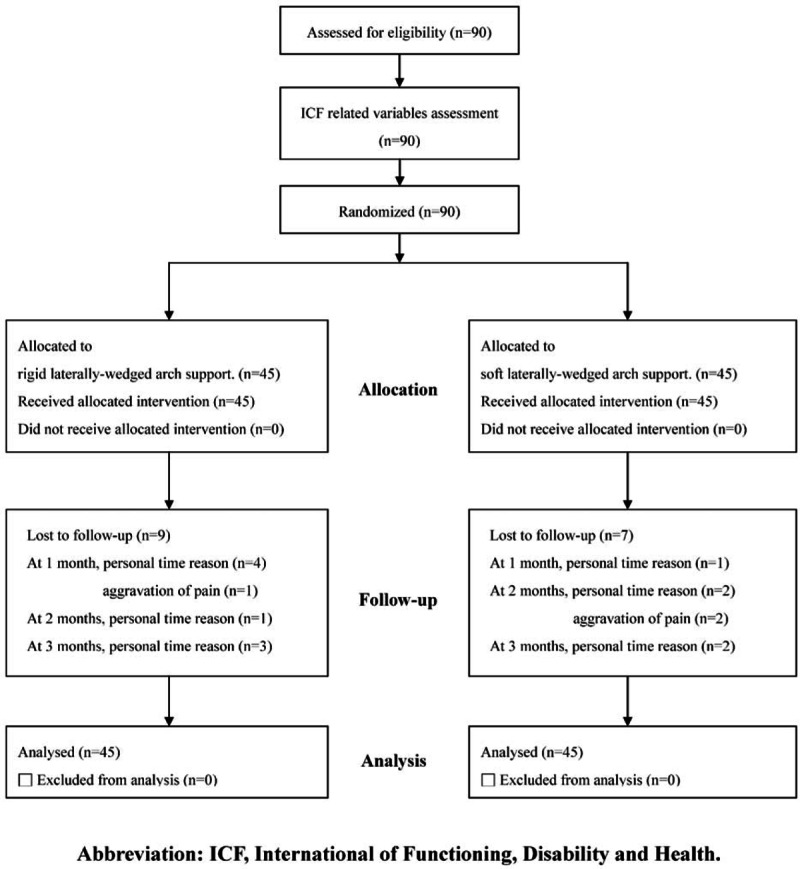
Flow diagram. ICF = International Classification of Functioning, Disability and Health.
2.7. Intervention
Each participant in the rigid LWAS insole group received a pair of thermoplastic insoles molded specifically for him or her by a qualified physiatrist. The insoles consisted of a 5° lateral wedge with an arch support composed of high-density ethyl vinyl acetate (ICB Medical, Australia), and the subtalar joint was maintained in a neutral position (Fig. 2). The procedure was detailed in a previous study.[28]
Figure 2.

Insole with a rigid lateral wedge and arch support.
Each participant in the soft LWAS insole group received a pair of ready-made insoles consisting of a soft 5° lateral wedge and an arch support composed of polyurethane (Lanew, Taiwan) (Fig. 3).
Figure 3.

Insole with a soft lateral wedge and arch support.
All participants were blinded to the type of insole prescribed and all interventions were provided by the same physiatrist. Both groups were instructed to wear the insoles inside self-selected comfortable shoes for 1 hour on the first day and thereafter increase their usage by 1 hour per day until they wore the insoles whenever they wore shoes.
2.8. Follow-up assessment
An investigator blinded to group allocation evaluated ICF-related variables at 4 consecutive time points: before treatment and after the participants had worn the insoles for 1, 2, and 3 months. Both the participants and the investigator were blinded to the insole status during the treatment and data collection periods. The KOOS pain score was used as the primary outcome.
2.9. Sample size
To detect an effect size of 0.77 at an α level of 0.05 and power of 0.9, we had to evaluate at least 74 participants (37 participants for each group). Considering the possibility of 20% of the participants withdrawing during follow-up, we initially selected 90 participants (45 participants for each group).
2.10. Statistical analysis
The χ2 or t test was used to analyze the data on demographics, body functions and structures, and activities and participation. The results are expressed as the mean ± standard deviation and 95% confidence intervals (CI). Repeated-measures analysis of covariance (ANCOVA) was used to assess the ICF-related variables (e.g., psychological distress, pain, balance, physical activity, disability, and knee OA-related health status) during follow-up assessments, with the baseline measurements used as covariates. The group effect, time effect, and group × time interaction effects for the 2 groups at the 3 postbaseline assessments were analyzed. The ANCOVA results are expressed as the F statistic, degrees of freedom, and P value. Intention-to-treat analysis (previous observation carried forward) was performed for all participants. The level of statistical significance was set at P < 0.05.
3. Results
We enrolled 90 participants, 70 women and 20 men, with mean ages of 60.6 ± 10.8 and 63.1 ± 10.8 years in the rigid and soft LWAS insole groups, respectively. Table 1 presents the participants’ demographic data. In the rigid LWAS insole group, 4 participants withdrew because of limited personal time, and 1 participant withdrew because of subjective aggravation of pain at the 1-month follow-up. Because of limited personal time, 1 and 3 participants withdrew at the 2- and 3-month follow-ups, respectively. In the soft LWAS insole group, 1 participant withdrew because of limited personal time at the 1-month follow-up. Two participants withdrew because of aggravation of pain and 2 participants withdrew because of limited personal time at the 2-month follow-up, and 2 participants withdrew because of limited personal time at the 3-month follow-up. Thus, a total of 74 participants completed the study (36 and 38 participants in the rigid and soft LWAS insole groups, respectively). The dropout rates were 20% and 15.6% in the rigid and soft LWAS insole groups, respectively. No significant differences were evident in the demographics of the participants who completed the study and those who withdrew (data not shown).
Table 1.
Basic demographics of participants.
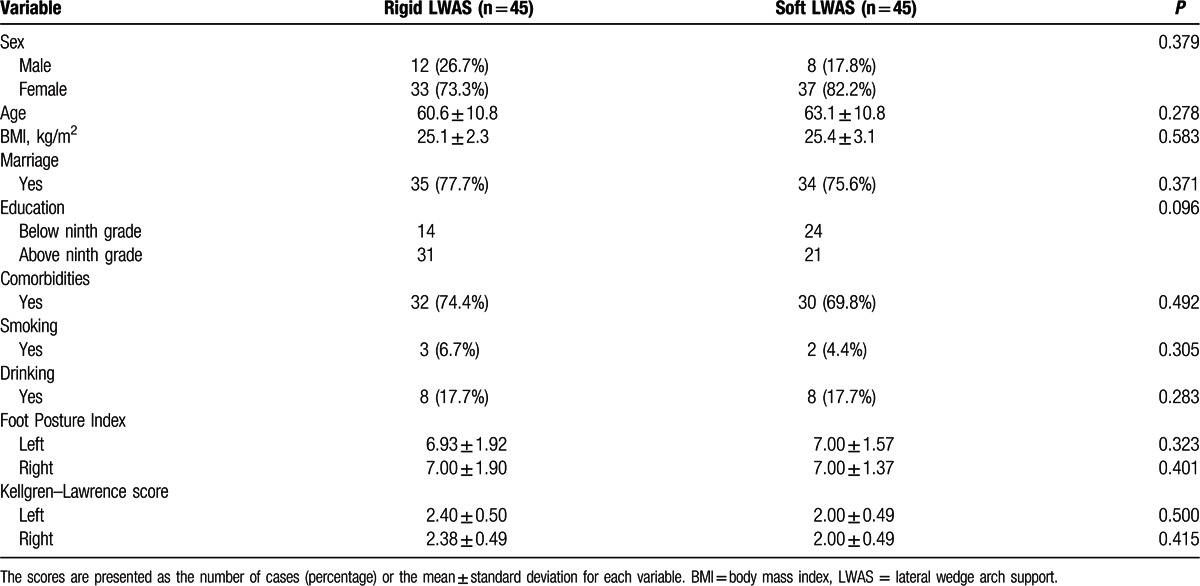
The scores in each outcome measure at each time point for each group and the mean differences between groups based on 95% CI are summarized in Tables 2 and 3. No significant differences were found between the groups in baseline scores for psychological distress (anxiety and depression), the pain–pressure threshold, postural stability and balance, physical activity (10-m fast speed walking, stair climbing, and chair rising times), disability severity, or the pain, symptoms, daily living function, sports and recreation function, and quality of life subscales of the KOOS. Table 2 lists the results of repeated-measures ANCOVA for the short-term effects of variables related to body functions and structures, and Table 3 presents the variables related to activities and participation. Compared with the results of baseline assessments, statistically significant group × time interaction improvements were noted in the soft LWAS group in pain (P = 0.008 for the KOOS), stair ascent time (P = 0.003), daily living function (P = 0.003 for the KOOS), sports and recreation function (P = 0.012 for the KOOS), and knee OA-related quality of life (P = 0.021 for the KOOS). Changes in the KOOS and stair ascent time of the 2 groups are shown in Fig. 4.
Table 2.
Body function scores.
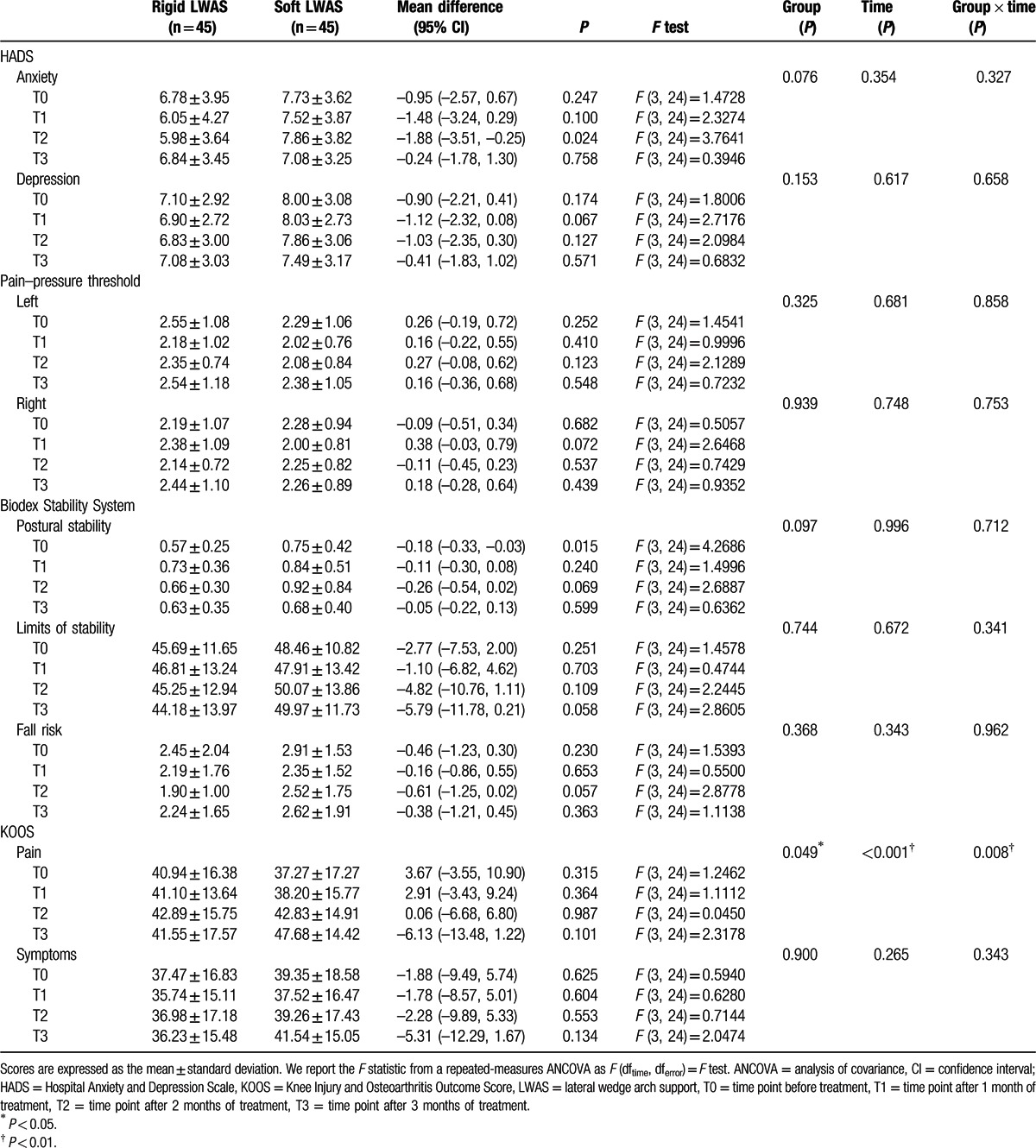
Table 3.
Activities and participation of participants.
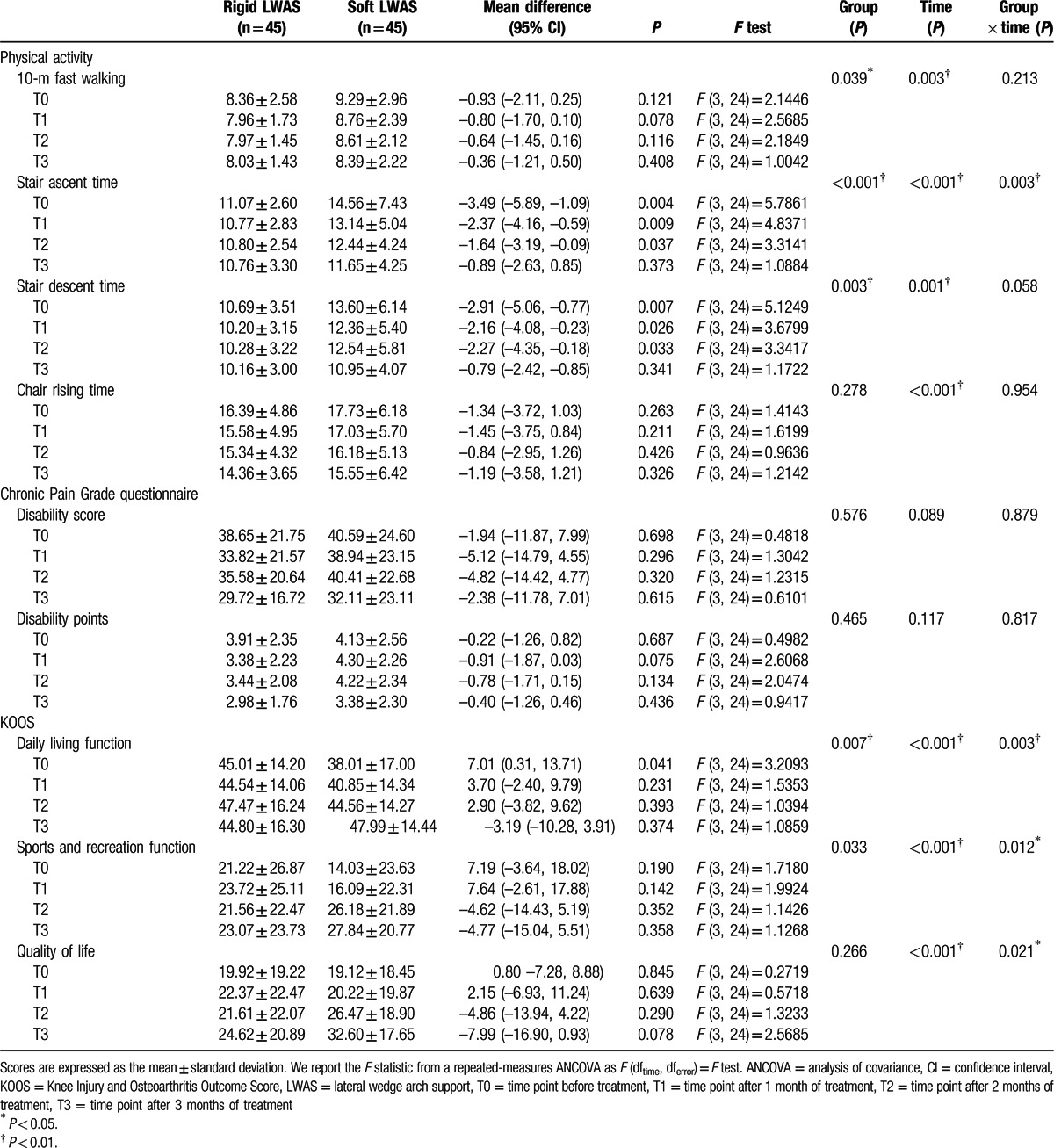
Figure 4.
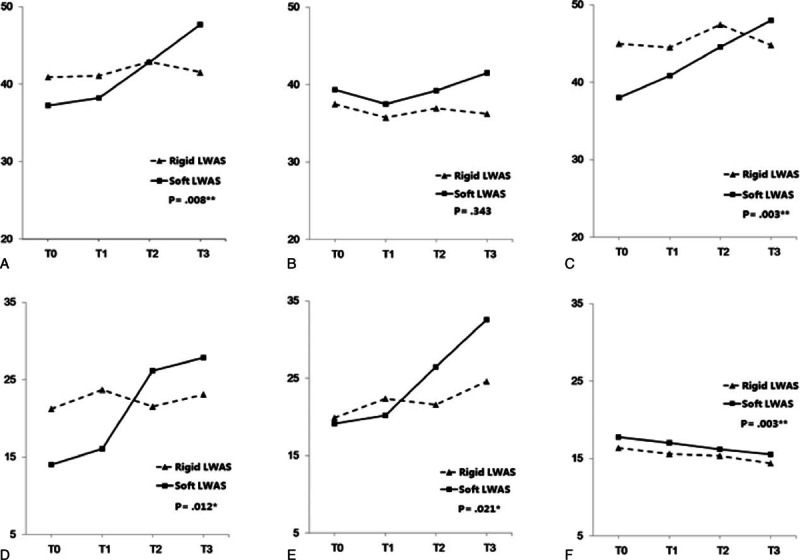
Changes in KOOS and stair ascent time. Triangles and squares represent the rigid and flexible LWAS insole groups, respectively. (A) KOOS pain subscale; (B) KOOS other symptoms subscale; (C) KOOS daily living function subscale; (D) KOOS sports and recreation function subscale; (E) KOOS knee-related quality of life subscale; and (F) stair ascent time. KOOS = Knee Injury and Osteoarthritis Outcome Score, LWAS = lateral wedge arch support, T0 = time point before treatment, T1 = time point after 1 month of treatment, T2 = time point after 2 months of treatment, T3 = time point after 3 months of treatment. Group × time interaction effects: (∗) P < 0.05; (∗∗) P < 0.01.
4. Discussion
This is the first study to apply the ICF system to patients with knee OA in a randomized, double-blind trial to compare the short-term clinical effects of wearing rigid and soft LWAS insoles. The use of soft LWAS insoles resulted in a significant short-term reduction in pain and improvements in stair ascent time, daily living function, sports and recreation function, and knee-related quality of life. The ICF system classifies these variables as belonging to the components of body functions and structures and activities and participation. In contrast to our assumption, the short-term use of rigid LWAS insoles did not improve the scores of ICF-related items.
Patients with knee OA typically experience pain and psychological distress (e.g., anxiety and depression).[44] Pain associated with knee OA may interfere with the ability to perform activities of daily living.[44,45] Poor performance in activities of daily living and sports and recreation function may exacerbate the disabilities of patients and increase their economic burden.[46] Our previous study showed that patients with knee OA scored lower in postural stability and quality of life measures than did age-matched controls.[9] The present study demonstrated that the short-term use of soft LWAS insoles could alleviate pain and improve physical activity, daily living function, sports and recreation function, and knee-related quality of life in patients with knee OA.
During the midstance phase of normal gait, an estimated 60% to 75% of a person's body weight is distributed over the medial knee joint.[47] Patients with knee OA exhibit a greater knee adduction moment when walking than do age-matched controls.[48] Wedge insoles can realign the foot in either the varus or the valgus plane from 5° to 10°.[23] Lateral wedge insoles alleviate pain by reducing the external knee adduction moment[16] and diminishing the medial knee joint load.[15] Lateral wedge insoles also may activate muscles and change the spatial position of the lower limb,[15] can retard foot supination and accentuate foot pronation, and may aggravate pronation in an already overpronated ankle and foot.[23] Wedges might inhibit normal foot and ankle biomechanics, through mechanisms such as increasing the ankle invertor moment,[24] and thus exacerbate OA symptoms.[50]
Arch support insoles are commonly used clinically and improve foot alignment, shock attenuation, support, and stability during walking and running.[49,51,52] A 4% to 6% increase in the peak knee adduction moment during walking and running was observed in healthy young adults wearing arch support insoles.[51] However, no immediate change was reported in knee pain, the adduction moment, or the adduction angular moment with the use of arch support insoles in athletic shoes by patients with knee OA.[53] Differences in ages, populations (healthy adults vs. patients with knee OA), and types of shoes might have affected the results of these studies.
LWAS insoles reduce the peak knee external adduction moment in patients with knee OA by laterally shifting the center of pressure to reduce the frontal plane ground reaction force and lever arm.[26] They also change the step width, progression angle, and valgus angle at the subtalar joint, enabling users to walk more naturally.[28] Although arches added to lateral wedge insoles are aimed at reducing ankle eversion, wearing LWAS insoles did not reduce the ankle invertor moment to a normal level in 1 study.[26] Previous studies have revealed that a larger angle in a lateral wedge insole increases the unloading force at the knee joint, causing greater ankle and foot discomfort.[16,54] Therefore, in this study, we provided the participants with insoles with a 5° lateral wedge and arch support.
People generally prefer wearing different shoes at various times, depending on personal preference and comfort. There are numerous shoe types, such as soft, lightweight, conventional walking, stability, and athletic shoes.[55] We allowed the participants to wear self-selected comfortable shoes in the present study. Soft shoes have the biomechanical advantages of barefoot walking, such as the absence of a lifted heel and stiff soles, and thus effectively reduce knee joint loads in patients with knee OA.[55] Soft insoles might have the same benefits as do soft shoes, thereby improving physical activity and knee OA-related health status, including pain, daily living function, sports and recreation function, and quality of life. Additional studies examining various insole and shoe type combinations are recommended.
Although our research represents a reasonable initial foray into the effects of LWAS insoles in patients with knee OA, we acknowledge that many factors, such as the rigidity of insoles, whether insoles are custom molded or ready-made, height of the medial arch, angle of the lateral wedge, insole construction, usage duration, shoe type, and age factors, affect the results. Therefore, the long-term effects of different types of insoles in patients with knee OA require further investigation.
The main strength of this study was its use of reliable and patient-centered objective and subjective measurements based on the ICF model and recorded using a double-blind, randomized design. The ICF model provides clinicians with knowledge on specific components relevant to the observed therapeutic effects of the LWAS insoles.
This study was subject to several limitations. First, we did not evaluate the biomechanical effects of the insoles; this topic warrants further investigation. Second, we followed the participants for only 3 months; whether the observed short-term benefits of the soft LWAS insoles continue after prolonged use is unclear. Third, factors such as insole construction, arch support height, lateral wedge angle, and shoe type might affect the study results. Long-term follow-up studies comparing different types of insoles and shoes are warranted. Finally, the total number of patients (90) was not high, with 78% being women, and 17.8% of dropout rate. Therefore, our study provides only preliminary but valuable data that should be validated in a larger study. Future studies should have a larger sample size and use a community-based sample to confirm the generalizability of our results.
5. Conclusions
Patients with knee OA who received short-term therapy with soft LWAS insoles experienced significant pain alleviation and improvements in physical activity, daily living function, sports and recreation function, and quality of life. These variables are classified in the body functions and structures and the activities and participation components in the ICF scheme. Additional clinical trials evaluating the biomechanical effects and the long-term efficacy of different types of insoles in patients with knee OA are necessary.
Footnotes
Abbreviations: ANCOVA = analysis of covariance, CI = confidence intervals, ICF = International Classification of Functioning, Disability and Health, KOOS = Knee Injury and Osteoarthritis Outcome Score, LWAS = lateral wedge arch support, OA = osteoarthritis.
Trial registration number: ClinicalTrials.gov NTC01765101.
Funding: This study was supported by research grants from Shin Kong Wu Ho-Su Memorial Hospital (SKH-8302-100-DR-21, SKH-8302-102-DR-32, SKH-8302-103-DR-36, SKH-8302-104-DR-29, and SKH-8302-105-DR-24) and the Ministry of Science and Technology, Taiwan (NSC 102-2628-B-002-036-MY3, NSC 102-2314-B-341-001, MOST-103-2314-B-341-002, and MOST-104-2314-B-341-001).
The authors have no conflicts of interest to disclose.
References
- 1.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 disease and injuries 1990–2010: a systematic analysis for the Global Burden of Diseases Study 2010. Lancet 2012; 380:2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang X, Wang S, Zhan S, et al. The prevalence of symptomatic knee osteoarthritis in China: results from the China Health and Retirement Longitudinal Study. Arthritis Rheumatol 2016; 68:648–653. [DOI] [PubMed] [Google Scholar]
- 3.Hiligsmann M, Cooper C, Arden N, et al. Health economics in the field of osteoarthritis: an expert's consensus paper from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Semin Arthritis Rheum 2013; 43:303–313. [DOI] [PubMed] [Google Scholar]
- 4.Woo J, Leung J, Lau E. Prevalence and correlates of musculoskeletal pain in Chinese elderly and the impact on 4-year physical function and quality of life. Public Health 2009; 123:549–556. [DOI] [PubMed] [Google Scholar]
- 5.Srikanth VK, Fryer JL, Zhai G, et al. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage 2005; 13:769–781. [DOI] [PubMed] [Google Scholar]
- 6.Glass N, Segal NA, Sluka KA, et al. Examining sex differences in knee pain: the multicenter osteoarthritis study. Osteoarthritis Cartilage 2014; 22:1100–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith SL, Woodburn J, Steultjens MP. Electromechanical delay and rate of force development in individuals with knee osteoarthritis. Osteoarthritis Cartilage 2016; 24:S122. [Google Scholar]
- 8.Jin X, Wang B, Wang X, et al. Associations between endogenous sex hormones and MRI structural changes in patients with symptomatic knee osteoarthritis. Osteoarthritis Cartilage 2016; 24:S358–S359. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh RL, Lee WC, Lo MT, et al. Postural stability in patients with knee osteoarthritis: comparison with controls and evaluation of relationships between International Classification of Functioning, Disability, and Health. Arch Phys Med Rehabil 2013; 94:340–346. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT, Lawrence RC, Hochberg MC, et al. Osteoarthritis: new insights. Part 2: treatment approaches. Ann Intern Med 2000; 133:726–737. [DOI] [PubMed] [Google Scholar]
- 11.Sellam J, Berenbaum F. Is osteoarthritis a metabolic disease? Joint Bone Spine 2013; 80:568–573.Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64:465–74. [DOI] [PubMed] [Google Scholar]
- 12.Simic M, Wrigley TV, Hinman RS, et al. Altering foot progression angle in people with medial knee osteoarthritis: the effects of varying toe-in and toe-out angles are mediated by pain and malalignment. Osteoarthritis Cartilage 2013; 21:1272–1280. [DOI] [PubMed] [Google Scholar]
- 13.Raja K, Dewan N. Efficacy of knee braces and foot orthoses in conservative management of knee osteoarthritis: a systematic review. Am J Phys Med Rehabil 2011; 90:247–262. [DOI] [PubMed] [Google Scholar]
- 14.Yasuda K, Sasaki T. The mechanics of treatment of the osteoarthritic knee with a wedged insole. Clin Orthop Relat Res 1987; 215:162–172. [PubMed] [Google Scholar]
- 15.Kerrigan DC, Lelas JL, Goggins J, et al. Effectiveness of a lateral-wedge insole on knee varus torque in patients with knee osteoarthritis. Arch Phys Med Rehabil 2002; 83:889–893. [DOI] [PubMed] [Google Scholar]
- 16.Hinman RS, Bennell KL. Advances in insoles and shoes for knee osteoarthritis. Curr Opin Rheumatol 2009; 21:164–170. [DOI] [PubMed] [Google Scholar]
- 17.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008; 16:137–162. [DOI] [PubMed] [Google Scholar]
- 18.Hinman RS, Bowles KA, Metcalf BB, et al. Lateral wedge insoles for medial knee osteoarthritis: effects on lower limb frontal plane biomechanics. Clin Biomech 2012; 27:27–33. [DOI] [PubMed] [Google Scholar]
- 19.Hsieh RL, Lein IN, Hsieh LF, et al. Study on disease classification of rehabilitation patients in eight hospitals at northern and western Taiwan. J Rehabil Med Assoc 1996; 24:35–40. [Google Scholar]
- 20.Chung-Po S, Ssu-Yuan C, Tyng-Guey W, et al. Primary reasons for rehabilitation service referrals: the recent experience of a medical center in Taiwan. Taiwan J Phys Med Rehabil 2010; 38:229–236. [Google Scholar]
- 21.Jones RK, Nester CJ, Richards JD, et al. A comparison of the biomechanical effects of valgus knee braces and lateral wedged insoles in patients with knee osteoarthritis. Gait Posture 2013; 37:368–372. [DOI] [PubMed] [Google Scholar]
- 22.Levinger P, Menz HB, Fotoohabadi MR, et al. Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res 2010; 3:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baker K, Goggins J, Xie H, et al. A randomized crossover trial of a wedged insole for treatment of knee osteoarthritis. Arthritis Rheum 2007; 56:1198–1203. [DOI] [PubMed] [Google Scholar]
- 24.Butler RJ, Barrios JA, Royer T, et al. Effect of laterally wedged foot orthoses on rearfoot and hip mechanics in patients with medial knee osteoarthritis. Prosthet Orthot Int 2009; 33:107–116. [DOI] [PubMed] [Google Scholar]
- 25.Yeh HC, Chen LF, Hsu WC, et al. Immediate efficacy of laterally wedged insoles with arch support on walking in persons with bilateral medial knee osteoarthritis. Arch Phys Med Rehabil 2014; 95:2420–2427. [DOI] [PubMed] [Google Scholar]
- 26.Abdallah AA, Radwan AY. Biomechanical changes accompanying unilateral and bilateral use of laterally wedged insoles with medial arch supports in patients with medial knee osteoarthritis. Clin Biomech (Bristol, Avon) 2011; 26:783–789. [DOI] [PubMed] [Google Scholar]
- 27.Nakajima K, Kakihana W, Nakagawa T, et al. Addition of an arch support improves the biomechanical effect of a laterally wedged insole. Gait Posture 2009; 29:208–213. [DOI] [PubMed] [Google Scholar]
- 28.Hsieh RL, Lee WC. Immediate and medium-term effects of custom-moulded insoles on pain, physical function, physical activity, and balance control in patients with knee osteoarthritis. J Rehabil Med 2014; 46:159–165. [DOI] [PubMed] [Google Scholar]
- 29.WHO. International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 30.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 1986; 29:1039–1049. [DOI] [PubMed] [Google Scholar]
- 31.Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin Biomech 2006; 21:89–98. [DOI] [PubMed] [Google Scholar]
- 32.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67:361–370. [DOI] [PubMed] [Google Scholar]
- 33.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002; 52:69–77. [DOI] [PubMed] [Google Scholar]
- 34.Abrishami A, Chan J, Chung F, et al. Preoperative pain sensitivity and its correlation with postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 2011; 114:445–457. [DOI] [PubMed] [Google Scholar]
- 35.Kinser AM, Sands WA, Stone MH. Reliability and validity of a pressure algometer. J Strength Cond Res 2009; 23:312–314. [DOI] [PubMed] [Google Scholar]
- 36.Biodex. Biodex Balance System: Clinical Resource Manual. Shirley: Biodex Medical System, Inc; 1999. [Google Scholar]
- 37.Pien LC, Chu H, Chen WC, et al. Reliability and validity of a Chinese version of the Multidimensional Fatigue Symptom Inventory-Short Form (MFSI-SF-C). J Clin Nurs 2011; 20:2224–2232. [DOI] [PubMed] [Google Scholar]
- 38.Tseng WC, Hsieh RL. Effects of short-term active video game play on community adults: under International Classification of Functioning, Disability and Health consideration. Chin Med J (Engl) 2013; 126:2313–2319. [PubMed] [Google Scholar]
- 39.Schmitz R, Arnold B. Intertester and intratester reliability of a dynamic balance protocol using the Biodex Stability System. J Sport Rehabil 1998; 7:95–101. [Google Scholar]
- 40.Cachupe WJC, Shifflett B, Kahanov L, et al. Reliability of Biodex balance system measures. Meas Phys Educ Exerc Sci 2001; 5:97–108. [Google Scholar]
- 41.Smith BH, Penny KI, Purves AM, et al. The Chronic Pain Grade questionnaire: validation and reliability in postal research. Pain 1997; 71:141–147. [DOI] [PubMed] [Google Scholar]
- 42.Roos EM, Lohmander LS. The Knee Injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 2003; 1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xie F, Li SC, Roos EM, et al. Cross-cultural adaptation and validation of Singapore English and Chinese versions of the Knee Injury and Osteoarthritis Outcome Score (KOOS) in Asians with knee osteoarthritis in Singapore. Osteoarthritis Cartilage 2006; 14:1098–1103. [DOI] [PubMed] [Google Scholar]
- 44.Somers TJ, Keefe FJ, Godiwala N, et al. Psychosocial factors and the pain experience of osteoarthritis patients: new findings and new directions. Curr Opin Rheumatol 2009; 21:501–506. [DOI] [PubMed] [Google Scholar]
- 45.Dekker J, van Dijk GM, Veenhof C. Risk factors for functional decline in osteoarthritis of the hip or knee. Curr Opin Rheumatol 2009; 21:520–524. [DOI] [PubMed] [Google Scholar]
- 46.Danter JH. Alleviating the pain of arthralgias. Nurse Pract 2009; 34:40–46. [DOI] [PubMed] [Google Scholar]
- 47.Krohn K. Footwear alterations and bracing as treatments for knee osteoarthritis. Curr Opin Rheumatol 2005; 17:653–656. [DOI] [PubMed] [Google Scholar]
- 48.Hurwitz D, Ryals A, Case J, et al. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res 2002; 20:101–107. [DOI] [PubMed] [Google Scholar]
- 49.Iorio R, Healy WL. Unicompartmental arthritis of the knee. J Bone Joint Surg Am 2003; 85-A:1351–1364. [DOI] [PubMed] [Google Scholar]
- 50.Yonclas PP, Nadler RR, Moran ME, et al. Orthotics and assistive devices in the treatment of upper and lower limb osteoarthritis: an update. Am J Phys Med Rehabil 2006; 85:S82–S97. [DOI] [PubMed] [Google Scholar]
- 51.Franz JR, Dicharry J, Riley PO, et al. The influence of arch supports on knee torques relevant to knee osteoarthritis. Med Sci Sports Exerc 2008; 40:913–917. [DOI] [PubMed] [Google Scholar]
- 52.Windle CM, Gregory SM, Dixon SJ. The shock attenuation characteristics of four different insoles when worn in a military boot during running and marching. Gait Posture 1999; 9:31–37. [DOI] [PubMed] [Google Scholar]
- 53.Hinman RS, Bardin L, Simic M, et al. Medial arch supports do not significantly alter the knee adduction moment in people with knee osteoarthritis. Osteoarthritis Cartilage 2013; 21:28–34. [DOI] [PubMed] [Google Scholar]
- 54.Shelburne KB, Torry MR, Steadman JR, et al. Effects of foot orthoses and valgus bracing on the knee adduction moment and medial joint load during gait. Clin Biomech (Bristol, Avon) 2008; 23:814–821. [DOI] [PubMed] [Google Scholar]
- 55.Shakoor N, Lidtke RH, Sengupta M, et al. Effects of specialized footwear on joint loads in osteoarthritis of the knee. Arthritis Rheum 2008; 59:1214–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]


