Supplemental Digital Content is available in the text
Abstract
The direct anterior approach (DAA) to total hip arthroplasty has been promoted as a minimally invasive alternative to the lateral approach, which we sought to verify by systematically reviewing and meta-analyzing the literature comparing clinical, radiographic, and surgical outcomes.
Two reviewers independently searched PubMed, OVID, and Web of Science databases for randomized controlled trials (RCTs) and cohort studies comparing the DAA and lateral approach for total hip arthroplasty.
Quality of RCTs was assessed using the Jadad scoring system, quality of cohort studies, using the Minors system. Data were extracted and meta-analyzed or qualitatively synthesized for primary outcomes (function, complications, and hospitalization time) and several secondary outcomes.
Data were extracted from 12 trials involving 4901 arthroplasty procedures. Meta-analysis showed that DAA was associated with significantly shorter hospitalization than the lateral approach, as well as greater functional rehabilitation and lower perceived pain during the early postoperative period. On the other hand, DAA was associated with longer surgery time. The 2 approaches were associated with similar rates of perioperative surgical complications and transfusions, as well as similar radiographic analysis results.
Although DAA may provide shorter hospitalization and faster recovery during the early postoperative period, the available evidence is still insufficient to conclude whether the DAA or lateral approach is superior for total hip arthroplasty. More high-quality studies and subsequent meta-analyses are needed.
INTRODUCTION
Total hip arthroplasty is used widely around the world as one of the most effective procedures for relieving pain, restoring hip function, and improving quality of life in patients with painful or deformed hip joints.1,2 Improvements in hip arthroplasty procedures have led to faster functional recovery, shorter hospitalization, and higher patient satisfaction.3,4 Except for perioperative managements, different approaches can also affect the clinical outcomes.5,6 Total hip arthroplasty is often carried out using a conventional lateral approach and its modifications, which is the preferred procedure of approximately 42% of orthopedic surgeons worldwide.7 However, the requirement for muscle splitting in the lateral approach can lead to greater pain in the early postoperative period and longer hospitalization and rehabilitation periods.8–10
As an alternative procedure, the direct anterior approach (DAA) to total hip arthroplasty has been developed in recent years. This muscle-sparing procedure involves a shorter length of incision as well as less muscle and soft-tissue dissection,11,12 qualifying it as a truly minimally invasive procedure.13,14 Thus, DAA was thought to be associated with lower postoperative pain and faster recovery than the lateral approach.9,10,11,13,14 However, DAA is still evolving15 and its real clinical outcomes are full of controversial, especially when the DAA procedure is performed in learning curve.16 On one hand, a study of 419 consecutive patients undergoing either DAA or a lateral approach found DAA to be associated with lower perceived perioperative pain and shorter hospitalization,17 and another study showed superior 1-year postoperative outcomes with DAA.18 On the other hand, some studies have suggested that either there is no significant benefit of DAA over a lateral approach19 or factors rather than choice of direct or lateral approach may be more important for early recovery, such as patient selection, accelerated rehabilitation, and improved analgesia.20
It is a general agreement that the highest level-evidence assessment of clinical interventions should be evidence-based, rely on results from update meta-analyses. One meta-analysis has already concluded that DAA is not significantly better than a posterior approach,21 but as of this time, we are unaware of meta-analyses comparing DAA and the lateral approach. Therefore, we conducted this meta-analysis to fill the research gap. Specifically, we systematically reviewed randomized controlled trials (RCTs) and cohort studies comparing the DAA and lateral approach for total hip arthroplasty, and we meta-analyzed available data on a total of 9 categories of outcomes: functions, complications, length of stay, radiographic analysis, transfusions, pain, makers of muscle damage and inflammation, surgery time, and gait.
METHODS
Ethical approval for this study was deemed unnecessary because it was a review of existing literature and did not involve any handling of individual patient data.
Search Methodology
Two reviewers (CY and PDK) independently searched PubMed, OVID, and Web of Science databases in June 2015 without restrictions on publication date or language. Search terms included “total hip replacement,” “total hip arthroplasty,” “THA,” “THR,” “anterior,” “direct anterior,” “anterior supine intermuscular,” “Hueter approach,” and “Smith-Petersen.” Search terms were combined using the Boolean operators “AND” or “OR.” Reference lists of relevant articles were manually searched to identify additional trials.
Selection Criteria
A study was considered eligible for inclusion if it was an RCT or cohort study, compared DAA with a lateral approach, and reported data for at least one of the following outcomes: postoperative function, complications, hospitalization time, radiographic analysis, transfusion, pain, markers of muscle damage or inflammation, surgery time, and gait.
Studies were excluded from consideration if they were explicitly labeled as a “pilot study;” were based on a cross-sectional questionnaire, case report, or frozen cadavers; or involved bilateral total hip arthroplasty, hemiarthroplasty, or computed tomography-based or robot-assisted total hip arthroplasty.
Literature Selection
All potentially relevant studies were imported into Endnote X6 and duplicates were excluded. Then the same 2 researchers who had searched the databases excluded studies based on titles and abstracts. The 2 researchers read the full text of the remaining studies and excluded those that did not satisfy the selection criteria. Disagreements were resolved by discussion with a third researcher (FXP).
Data Extraction
The same 2 researchers independently extracted the following data from the final set of included studies: first author's name, country, publication year, any significant differences at baseline, sample size, follow-up period, and whether DAA surgeons were still on a learning curve. Data were also collected on the following primary outcomes: postoperative function, complications, and hospitalization time. Function and complications were selected as primary outcomes because they directly reflect efficacy and safety of the surgical approach. Hospitalization time was selected because it is one of the strongest determinants of rapid recovery after total hip arthroplasty,3,4 and it is therefore closely related to patient costs and satisfaction.
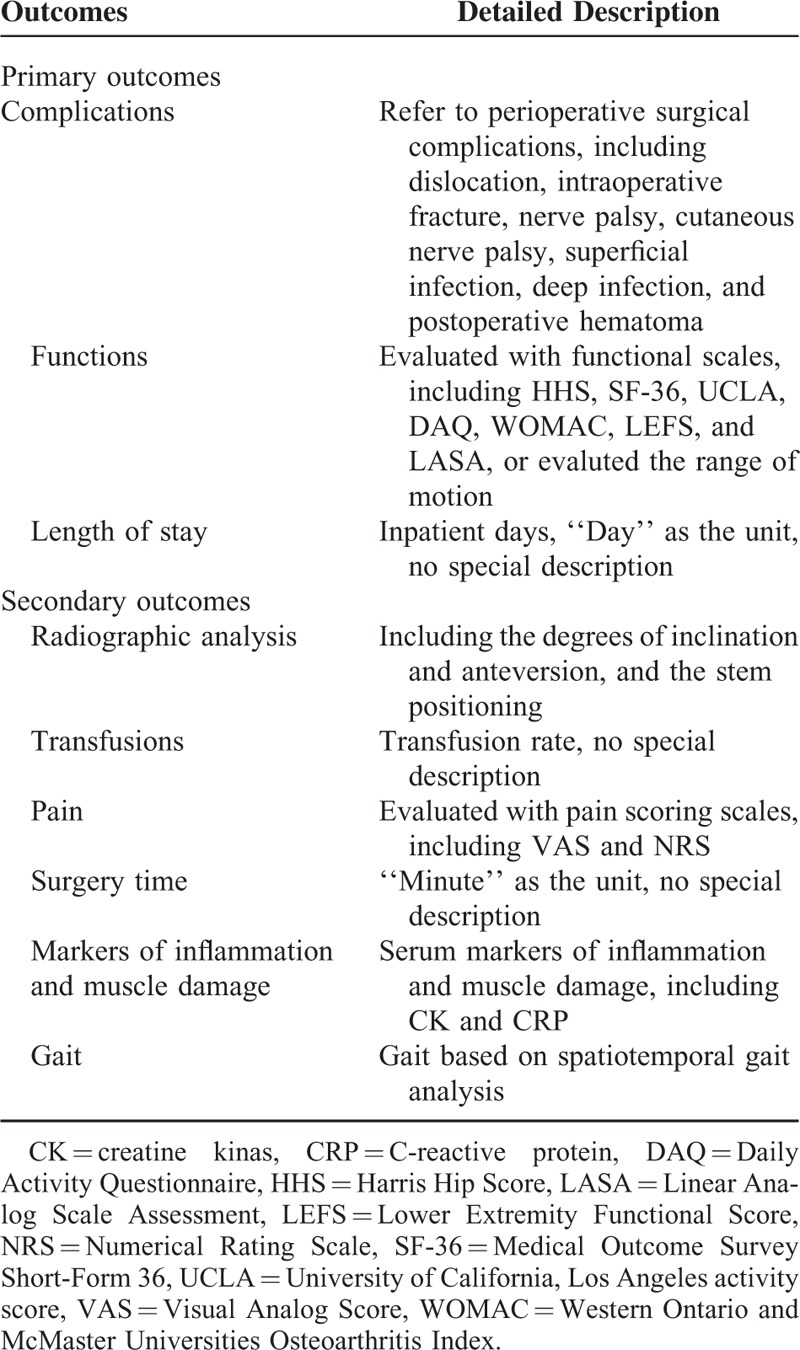
Data were also collected on the following secondary outcomes: radiographic analysis, transfusion, pain, markers of muscle damage and inflammation, surgery time, and gait. Table 1 provides detailed descriptions of each outcome.
TABLE 1.
The Detailed Description of Each Outcome Assessment
Assessment of Study Quality
Working independently, 2 researchers (CY and PDK) assessed the quality of included RCTs using the Jadad scoring system.22 This system assesses randomization, blinding, withdrawals, and dropouts, awarding a study a score of 0–5 points. The quality of cohort studies was assessed using the Minors scoring system,23 which is considered suitable for nonrandomized surgical intervention studies. This system awards a score of 0–2 points for each of 12 items according to whether the item was reported or not and whether it was treated adequately or not (see Supplemental Table, Supplemental Content, which provides a detailed description of the Jadad and Minors scales). Discrepancies between assessments by the 2 reviewers were resolved by discussion, with arbitration by a 3rd reviewer when necessary.
Statistical Analysis
Outcomes for which data could not be compared directly across studies were synthesized qualitatively, as were outcomes for which insufficient data were reported across studies. Outcomes for which sufficient, equivalent data were reported across studies were meta-analyzed using Forest plots generated with RevMan 5.2. Dichotomous data were expressed as proportions, such as rates of transfusions and complications; the intervention effect was expressed as a risk ratio. Continuous data reported in the same way across studies, such as for hospitalization time, were meta-analyzed in terms of the weighted mean difference (WMD) and associated 95% confidence interval (95%CI). Continuous data reported in different ways across studies were meta-analyzed in terms of the standardized mean difference (SMD). Continuous data reported as medians and ranges were transformed into means and standard deviations using Hozo formula.24
Pooled data were assessed for heterogeneity using the Chi-squared test and I2 tests. Heterogeneity was defined as absent when I2 was between 0 and 25%; low, between 25.1% and 50%; moderate, between 50.1% and 75%; or high, between 75.1% and 100%. Fixed-effects meta-analysis was performed when P ≥ 0.1 and I2 ≤ 50%; otherwise, random-effects meta-analysis was performed.
RESULTS
Search Results
Systematic search of Pubmed, OVID, and Web of Science turned up 4286 potentially eligible studies, and no additional records were found during manual searches of reference lists (See Supplemental Figures 1–3, Supplemental Contents, which illustrates the detailed search histories for each electronic database). After removing 1775 duplicate studies using Endnote X6, another 2354 studies were excluded based on their titles and abstracts. The remaining 157 studies were read in full, and 145 were excluded because they failed to satisfy the selection criteria. In the end, 12 studies were included in the systematic review and meta-analysis. Details of study identification, screening, and selection are given in Figure 1.
FIGURE 1.
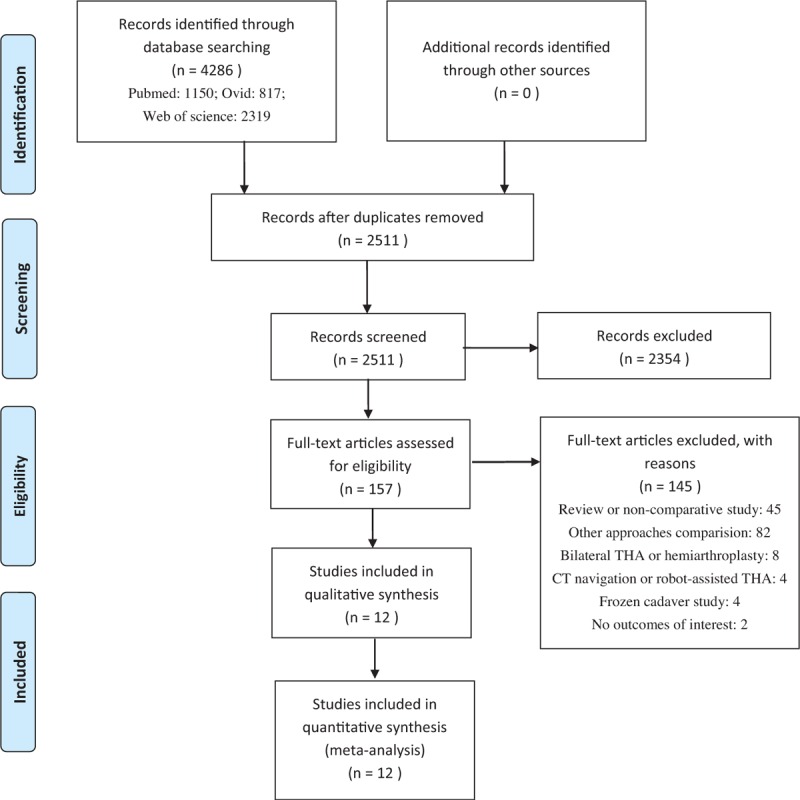
Flowchart of study selection.
Characteristics of Included Studies
The included 12 studies17–19,25–33 contained 2 RCTs25,26 and 10 nonrandomized cohort studies17–19,27–33 published within the last 6 years, altogether involving 2991 cases of DAA total hip arthroplasty and 1910 cases of lateral approach total hip arthroplasty. Three studies were performed in the US, 3 in Germany, 2 in Norway, 2 in Italy, and 1 each in Canada and Switzerland.
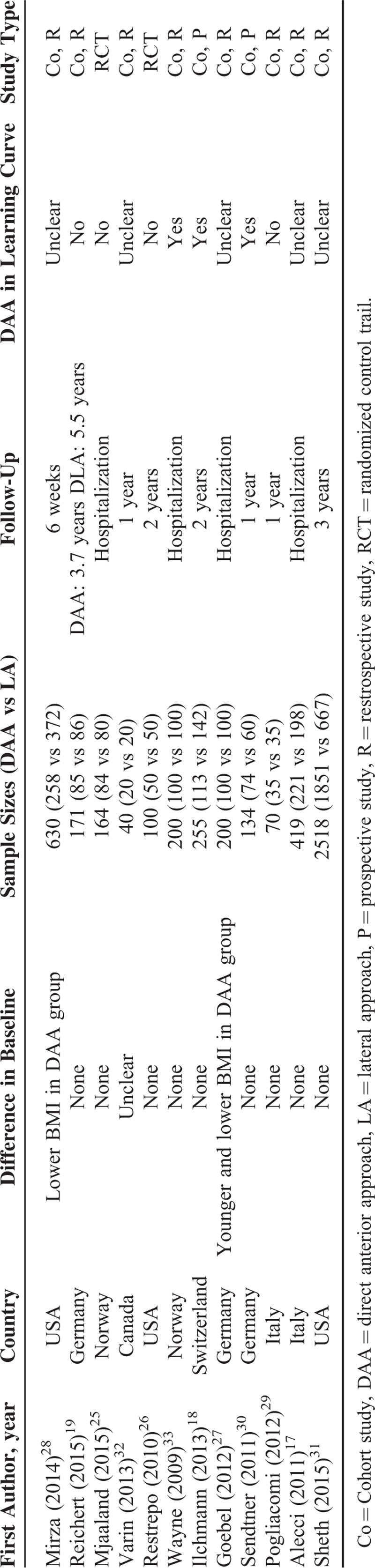
Minors quality scores for the 10 cohort studies ranged from 10 to 18 points of a possible 24, while Jadad quality scores for the 2 RCTs were 326 and 4 points25 of a possible 5. Eleven studies compared the DAA and lateral groups at baseline, and 9 studies found no significant differences.17–19,25–26,29–33 Seven studies carried out short- or intermediate-term follow-up lasting up to 1 year.18–19,26,29–32 Another study evaluated patients only at 6 weeks,28 and another 4 reported clinical outcomes only during postoperative hospitalization.17,25,27,33 Seven studies evaluated postoperative function:18–19,26–30 6 studies used patient-reported functional scales, and 1 study reported range of motion.27 Eight studies reported perioperative surgical complications.17–19,26,29–31,33 Six studies provided data on hospitalization time.17,26–29,33 Only 1 study each analyzed postoperative gait32 or assayed levels of markers of muscle damage and inflammation.25 Three studies explicitly stated that surgeons performed DAA while still on the learning curve,18,30,33 while 4 stated that the DAA surgeons had completed the learning curve.19,25,26,29 The remaining 5 studies did not explicitly mention a learning curve. Detailed study quality assessment and outcomes data can be found in Tables 2–4.
TABLE 2.
Minors Score for Each Included Nonrandomized Study and Jadad Score for Each Included Randomized Study
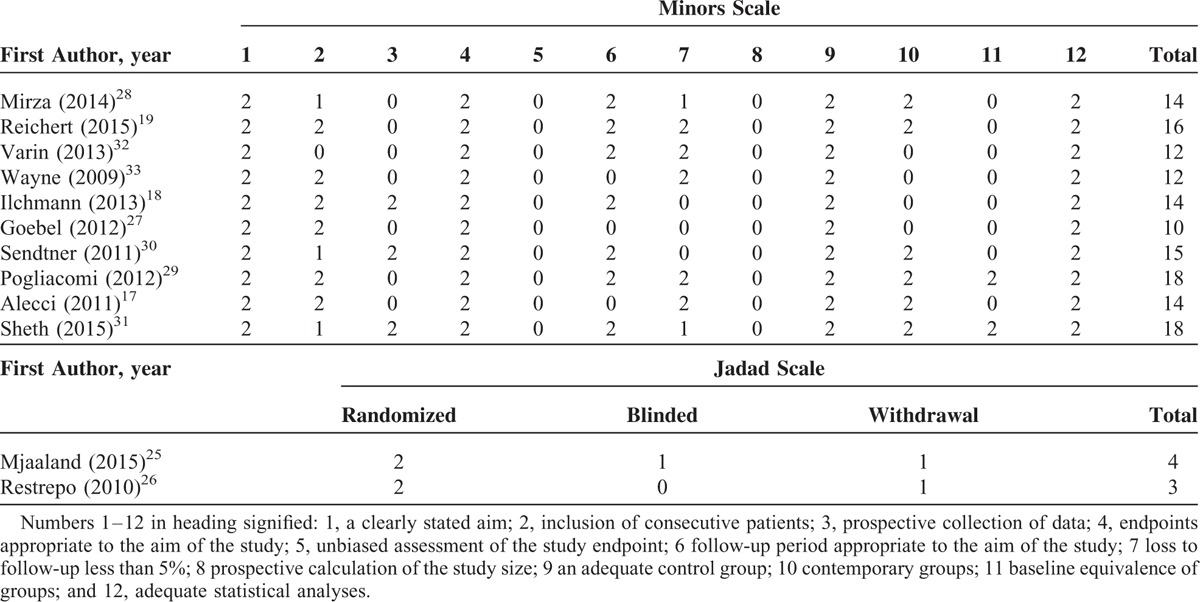
TABLE 4.
Summary of Significantly Different Outcomes Between Groups
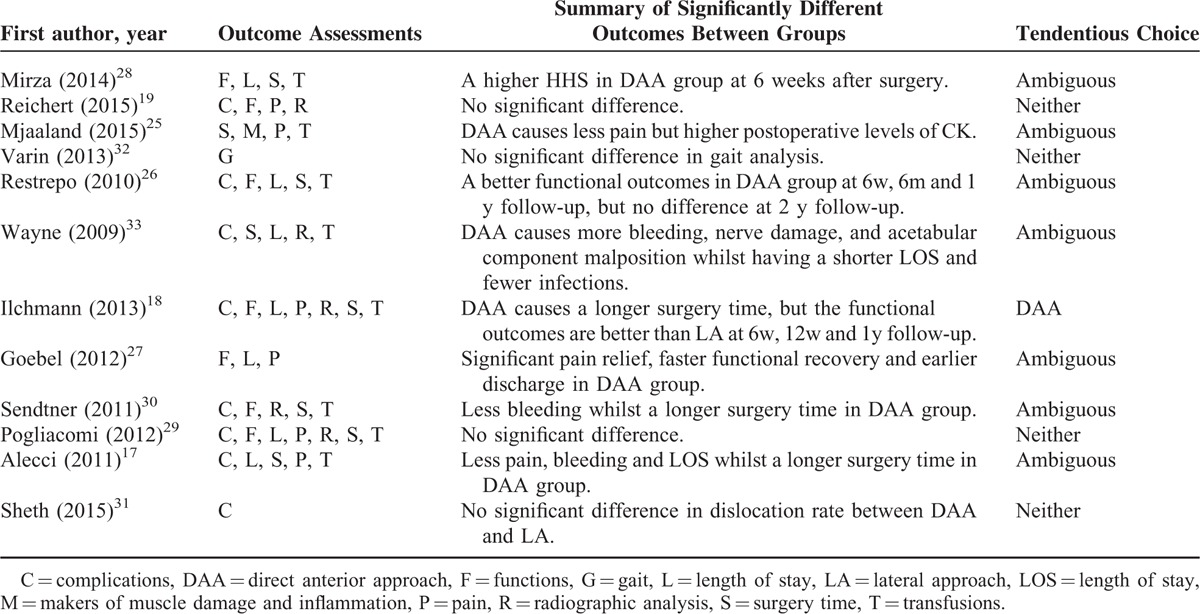
TABLE 3.
Characteristics of Included Studies
PRIMARY OUTCOMES
Postoperative Function
Seven studies involving 1560 cases of total hip arthroplasty reported functional outcomes18–19,26–30 (Table 5), though functional scales and follow-up periods varied substantially. Four of the 7 studies showed that DAA led to better functional outcomes.18,26–28 Mirza et al28 reported significantly higher 6-week Harris Hip Score (HHS) scores with DAA (P < 0.0001). Restrepo et al26 found that DAA led to significantly better scores on the HHS, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Short Form 36-Item Health Survey scale, Lower Extremity Functional Score, and Linear Analog Scale Assessment at 6 weeks, 6 months, and 1 year, although DAA and the lateral approach led to similar scores on these instruments at 2 years. Similarly, Ilchmann et al18 found significantly higher HHS scores with DAA at 6 weeks, 12 weeks, and 1 year, but similar HHS scores for DAA and the lateral approach at 2 years. Goebel et al27 found that mean time to achieve the therapeutic goal was shorter in the DAA group (6.4 vs 7.4 days).
TABLE 5.
Summary of Functional Outcomes
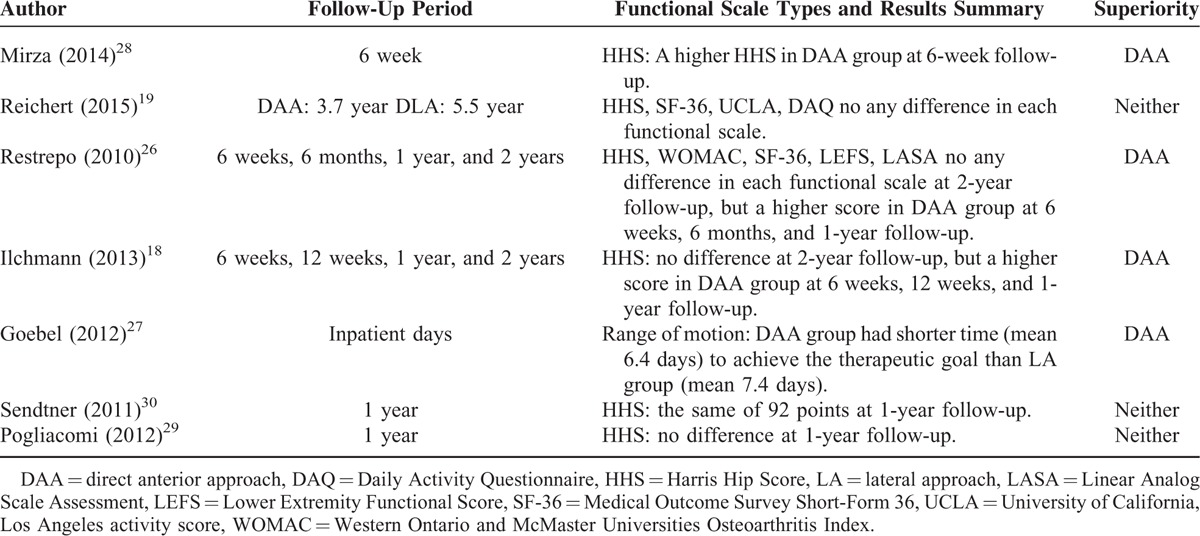
In contrast, 3 studies found no significant differences in functional outcomes between DAA and the lateral approach at 1 year29–30 or 3.7 year.19
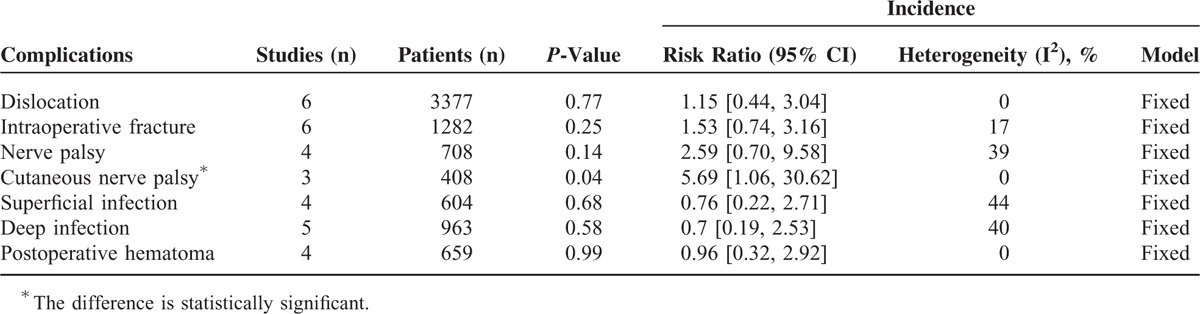
Perioperative Complications
Eight studies reported the occurrence of 7 types of perioperative surgical complications.17–19,26,29–31,33 Meta-analysis showed that both DAA and the lateral approach were associated with similar risk of dislocation, intraoperative fracture, nerve palsy, superficial infection, deep infection, and postoperative hematoma (Table 6). In contrast, DAA was associated with higher risk of cutaneous nerve palsy (RR 5.69, 95%CI 1.06–30.62, P = 0.04).
TABLE 6.
The Results of Meta-Analyses in Complications
Hospitalization Time
Six studies reported data on this outcome.17,26–29,33 Meta-analysis showed that hospitalization time after DAA was shorter by a mean of 1.19 days (95%CI −2.08 to −0.3, P = 0.009) than after the lateral approach (Fig. 2). This meta-analysis involved a random-effects model because of significant heterogeneity among the studies (I2 = 96%).
FIGURE 2.
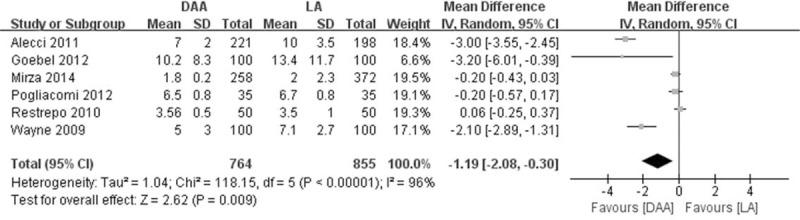
Forest plot of hospitalization time for patients after DAA or lateral approach total hip arthroplasty. DAA = direct anterior approach, df = degrees of freedom, IV = inverse variance, random = random-effects modeling, SD = standard deviation.
Secondary Outcomes
DAA and lateral approach groups showed similar rates of transfusion (RR 0.78, 95%CI 0.60–1.02, P = 0.07; Fig. 3), while surgery time was longer with DAA by a WMD of 7.99 min (95%CI 2.38–13.6, P = 0.005; Fig. 4). Radiographic analyses indicated that the 2 approaches were associated with similar degrees of inclination (WMD 0.00°, 95%CI −1.15 to 1.15, P = 1.00) and anteversion (WMD 3.05°, 95% CI −6.65 to 12.75, P = 0.54) (Figs. 5–6), as well as similar rates of varus or valgus stem positioning (RR 0.92, 95%CI 0.68–1.26, P = 0.62; Fig. 7).
FIGURE 3.
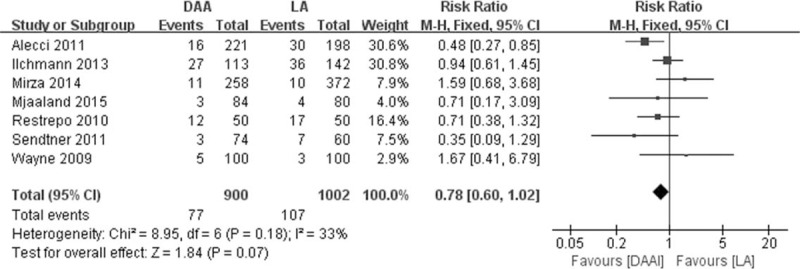
Forest plot of transfusion rates among patients after DAA or lateral approach total hip arthroplasty. DAA = direct anterior approach, df = degrees of freedom, fixed = fixed-effects modeling, M-H = Mantel–Haenszel.
FIGURE 4.
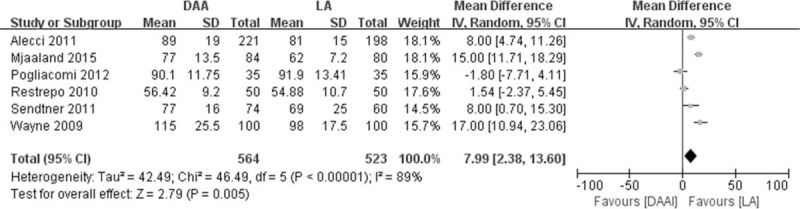
Forest plot of surgery time for patients receiving DAA or lateral approach total hip arthroplasty. DAA = direct anterior approach, df = degrees of freedom, IV = inverse variance, random = random-effects modeling, SD = standard deviation.
FIGURE 5.
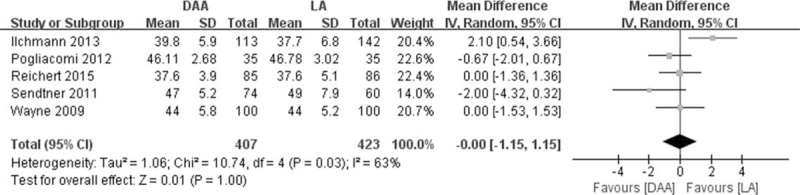
Forest plot of radiographic inclination angle in patients after DAA or lateral approach total hip arthroplasty. DAA = direct anterior approach, df = degrees of freedom, IV = inverse variance, random = random-effects modeling, SD = standard deviation.
FIGURE 6.
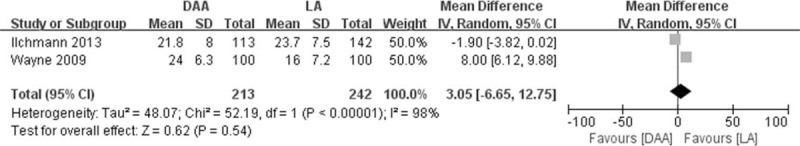
Forest plot of radiographic anteversion angle in patients after DAA or lateral approach total hip arthroplasty. DAA = direct anterior approach, df = degrees of freedom, IV = inverse variance, random = random-effects modeling, SD = standard deviation.
FIGURE 7.
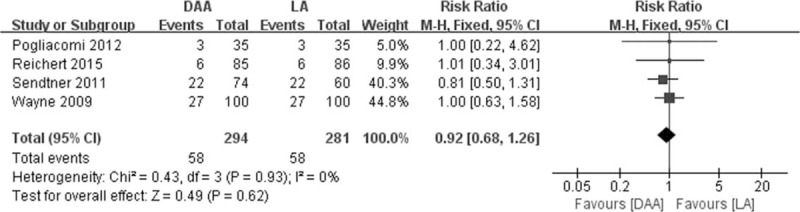
Forest plot of rates of varus/valgus stem positioning in radiographic analysis of patients after DAA or lateral approach total hip arthroplasty. DAA = direct anterior approach, df = degrees of freedom, fixed = fixed-effects modeling, M-H = Mantel–Haenszel.
Six studies evaluated postoperative pain using pain scales,17–19,25,27,29 though the scales and evaluation time points varied considerably. Four studies reported significantly better pain scores after DAA.17–18,25,27 One RCT25 by Mjaaland et al and 1 cohort study27 by Goebel et al associated DAA with lower scores on the visual analogue scale during postoperative hospitalization. Alecci et al17 found a lower pain score on the numerical rating scale (NRS) on the first day after DAA (1.4 vs 2.5 points). Ilchmann et al18 reported lower visual analogue scale pain scores in the DAA group at 6 and 12 weeks. The remaining 2 studies found no significant differences in pain scores between groups at 1 year29 or 3.7 years.19
One study compared DAA and the lateral approach in terms of postoperative serum levels of creatine kinase and C-reactive protein, which serve as markers of inflammation and muscle damage.25 Creatine kinase levels immediately after arthroplasty and on postoperative day 4 were significantly higher in the DAA group, while C-reactive protein levels were similar between the 2 groups at all time points examined.25 One study compared the 2 approaches using spatiotemporal gait analysis and found no significant difference.32
DISCUSSION
This is the first systematic review and meta-analysis to compare DAA and lateral approach total hip arthroplasty in terms of clinical, radiographic, and surgical outcomes. The available evidence suggests that DAA may be associated with better early postoperative functional rehabilitation, lower levels of perceived pain, and shorter hospitalization time. On the other hand, DAA may be associated with longer surgery time. The 2 arthroplasty approaches appear to be associated with similar rates of perioperative surgical complications and transfusion, similar results on radiographic and gait analyses, and similar serum levels of inflammation and muscle damage markers. We conclude that the available evidence does not allow us to determine whether DAA or the lateral approach is superior; more large, well-designed studies are needed to explore the results of this meta-analysis in greater detail.
In theory, many clinicians perform DAA because it avoids the inevitable muscle-splitting in the lateral approach, which can prolong hospitalization and complicate functional rehabilitation in the early postoperative period.9,10 DAA, in contrast, does not require exposing or lacerating the gluteus minimus and medius muscles.34 Although DAA can damage the tensor fascia lata, this may have only a minor effect on early rehabilitation.18 As a result, DAA can lead to more rapid functional recovery and shorter hospitalization times than other approaches.10,14
Our meta-analysis of available clinical evidence suggests that in practice, the benefits of DAA over the lateral approach are less clear. Although several studies in our systematic review consistently showed better outcomes with DAA during functional rehabilitation within 1 year of surgery,18,26–28 including a reduction in mean hospitalization stay by more than 1 day, other studies failed to show any differences in functional recovery at follow-up times beyond 1 year.19,29–30 It may be that the benefits of DAA occur primarily during the early postoperative period. Consistent with this idea, numerous studies in our systematic review reported significantly lower levels of perceived pain after DAA within early postoperative period.17–18,25,27 These results may help explain why several studies have reported more rapid functional rehabilitation with DAA.
Although some studies have associated DAA with fairly low complication rates,35,36 others have reported fairly high rates.37,38 Our meta-analysis suggests that the rates of most complications are similar for DAA and the lateral approach, with at least 1 exception: risk of cutaneous nerve palsy is 5.69-fold higher with DAA. This cutaneous nerve palsy is likely to come from the lateral femoral cutaneous nerve, but none of the studies reporting this complication described it in sufficient detail to indicate whether it referred only to skin numbness lateral to the incision or to complete nerve palsy of the entire lateral thigh. This is an important question because many clinicians do not consider skin numbness a complication of total hip arthroplasty unless it is particularly bothersome to the patient. We suggest that our meta-analysis finding of greater risk of cutaneous nerve palsy with DAA may not be clinically significant, and further study is needed to examine this in greater detail.
The study by Mjaaland et al25 in our systematic review reported similar serum levels of C-reactive protein in patients treated by DAA or lateral approach, which is consistent with another study not included in our systematic review because it compared DAA with a posterior approach.39 These results may mean that the inflammatory cascade associated with total hip arthroplasty is influenced primarily by bone removal and implant placement, not by the surgical approach.39 Mjaaland et al25 also reported higher serum levels of creatine kinase in patients with DAA, which does not make sense given the observed similarity in C-reactive protein levels. Those authors suggested that this result was due to a type 2 error.
Unfortunately, our meta-analysis was unable to isolate the influence of the DAA learning curve on the results. It is difficult to estimate what proportion of DAA total hip arthroplasties in our systematic review were performed within or beyond the curve, since studies not included in our systematic review have reported 30 to 200 DAA procedures beyond the learning curve.35,40,41 Only 7 of the 12 trials in our review explicitly addressed the learning curve, preventing us from performing subgroup meta-analyses. This is an important limitation in other meta-analyses of DAA as well.21,41 The results of our meta-analysis may also reflect confounding by other factors such as patient characteristics42 and perioperative management.3 We were unable to control for these factors because of incomplete reporting by the studies in our review.
In summary, our study preliminary shows that although DAA may provide shorter hospitalization and faster recovery during the early postoperative period, the available evidence is still insufficient to conclude whether the DAA or lateral approach is superior for total hip arthroplasty. Our results highlight the need for large, high-quality studies that investigate outcomes of DAA and that can be incorporated into future meta-analyses.
Supplementary Material
Acknowledgments
The authors thank China Health Ministry Program (201302007) for the support.
Footnotes
Abbreviations: DAA = direct anterior approach, DAQ = daily activity questionnaire, HHS = harris hip score, LASA = linear analog scale assessment, LEFS = lower extremity functional score, LOS = length of stay, NRS = numerical rating score, SF-36 = short form 36-item health survey, UCLA = University of California, Los Angeles activity score, VAS = visual analog score, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
PK contributed equally to this work.
CY and PDK: conducted the systematic review and meta-analysis, and drafted and revised the manuscript. FXP: conceived the systematic review and meta-analysis and serves as guarantor of the paper, taking responsibility for the integrity of the work as a whole from inception to published article.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Ethgen O, Bruyère O, Richy F, et al. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 2004; 86-A:963. [DOI] [PubMed] [Google Scholar]
- 2.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res 2006; 443:266–272. [DOI] [PubMed] [Google Scholar]
- 3.Husted H, Holm G. Fast track in total hip and knee arthroplasty – experiences from Hvidovre University Hospital. Denmark Injury 2006; 37: 5 Suppl:S31–S35. [DOI] [PubMed] [Google Scholar]
- 4.Sculco PK, Pagnano MW. Perioperative solutions for rapid recovery joint arthroplasty: get ahead and stay ahead. J Arthroplasty 2015; 30:518–520. [DOI] [PubMed] [Google Scholar]
- 5.Lamontagne M, Varin D. Beaulperative solutions for rapid recovery joint arthroploplasty better restore stair climbing gait mechanics? J Orthop Res 2011; 29:1412–1417. [DOI] [PubMed] [Google Scholar]
- 6.Petis S, Howard JL, Lanting BL, et al. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg 2015; 58:128–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chechik O, Khashan M, Lador R, et al. Surgical approach and prosthesis fixation in hip arthroplasty world wide. Arch Orthop Trauma Surg 2013; 133:1595–1600. [DOI] [PubMed] [Google Scholar]
- 8.Valente G, Taddei F, Jonkers I. Influence of weak hip abductor muscles on joint contact forces during normal walking: probabilistic modeling analysis. J Biomech 2013; 46:2186–2193. [DOI] [PubMed] [Google Scholar]
- 9.Mirza AJ, Lombardi AV, Jr, Morris MJ, et al. A mini-anterior approach to the hip for total joint replacement: optimising results: improving hip joint replacement. Bone Joint J 2014; 96-B (11 Supple A):32–35. [DOI] [PubMed] [Google Scholar]
- 10.Martin CT, Pugely AJ, Gao Y, et al. Comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplasty 2013; 28:849–854. [DOI] [PubMed] [Google Scholar]
- 11.Horne PH, Olson SA. Direct anterior approach for total hip arthroplasty using the fracture table. Curr Rev Musculoskelet Med 2011; 4:139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oinuma K, Eingartner C, Saito Y, et al. Total hip arthroplasty by a minimally invasive, direct anterior approach. Oper Orthop Traumatol 2007; 19:310. [DOI] [PubMed] [Google Scholar]
- 13.Berend KR, Lombardi AV, Jr, Seng BE, et al. Enhanced early outcomes with the anterior supine inter-muscular approach in primary total hip arthroplasty. J Bone Joint Surg Am 2009; 91:107. [DOI] [PubMed] [Google Scholar]
- 14.Vail TP, Callaghan JJ. Minimal incision total hip arthroplasty. J Am Acad Orthop Surg 2007; 15:707. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez JA, Cooper HJ, Robinson J. Direct anterior approach to THR: what it is and what it is not. Curr Rev Musculoskelet Med 2013; 6:276–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res 2005; 441:115. [DOI] [PubMed] [Google Scholar]
- 17.Alecci V, Valente M, Crucil M, et al. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol 2011; 12:123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ilchmann T, Gersbach S, Zwicky L, et al. Standard transgluteal versus minimal invasive anterior approach in hip arthroplasty: a prospective, consecutive cohort study. Orthop Rev (Pavia) 2013; 5:e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reichert JC, Volkmann MR, Koppmair M, et al. Comparative retrospective study of the direct anterior and transgluteal approaches for primary total hip arthroplasty. Int Orthop 2015; 39:2309–2313. [DOI] [PubMed] [Google Scholar]
- 20.Kim S, Losina E, Solomon DH, et al. Effectiveness of clinical pathways for total knee and total hip arthroplasty: literature review. J Arthroplasty 2003; 18:69. [DOI] [PubMed] [Google Scholar]
- 21.Higgins BT, Barlow DR, Heagerty NE, et al. Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty 2015; 30:419–434. [DOI] [PubMed] [Google Scholar]
- 22.Jadad AR, Moore A, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17:1–12. [DOI] [PubMed] [Google Scholar]
- 23.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003; 73:712–716. [DOI] [PubMed] [Google Scholar]
- 24.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005; 5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mjaaland KE, Kivle K, Svenningsen S, et al. Comparison of markers for muscle damage, inflammation, and pain using minimally invasive direct anterior versus direct lateral approach in total hip arthroplasty: A prospective, randomized, controlled trial. J Orthop Res 2015; 33:1305–1310. [DOI] [PubMed] [Google Scholar]
- 26.Restrepo C, Parvizi J, Pour AE, et al. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty 2010; 25:671–679.e1. [DOI] [PubMed] [Google Scholar]
- 27.Goebel S, Steinert AF, Schillinger J, et al. Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop 2012; 36:491–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mirza AJ, Lombardi AV, Jr, Morris MJ, et al. A mini-anterior approach to the hip for total joint replacement: optimising results: improving hip joint replacement outcomes. Bone Joint J 2014; 96-B (11 Supple A):32–35. [DOI] [PubMed] [Google Scholar]
- 29.Pogliacomi F, De Filippo M, Paraskevopoulos A, et al. Mini-incision direct lateral approach versus anterior mini-invasive approach in total hip replacement: results 1 year after surgery. Acta Biomed 2012; 83:114–121. [PubMed] [Google Scholar]
- 30.Sendtner E, Borowiak K, Schuster T, et al. Tackling the learning curve: comparison between the anterior, minimally invasive (Micro-hip® and the lateral, transgluteal (Bauer) approach for primary total hip replacement. Arch Orthop Trauma Surg 2011; 131:597–602. [DOI] [PubMed] [Google Scholar]
- 31.Sheth D, Cafri G, Inacio MC, et al. Anterior and anterolateral approaches for tha are associated with lower dislocation risk without higher revision risk. Clin Orthop Relat Res 2015; 473:3401–3408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varin D, Lamontagne M, Beaulint]ton EW. Ne anterior approach for THA provide closer-to-normal lower-limb motion? J Arthroplasty 2013; 28:1401–1407. [DOI] [PubMed] [Google Scholar]
- 33.Wayne N, Stoewe R. Primary total hip arthroplasty: a comparison of the lateral Hardinge approach to an anterior mini-invasive approach. Orthop Rev (Pavia) 2009; 1:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bremer AK1, Kalberer F, Pfirrmann CW, et al. Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. J Bone Joint Surg Br 2011; 93:886–889. [DOI] [PubMed] [Google Scholar]
- 35.Bhandari M, Matta JM, Dodgin D, et al. Anterior Total Hip Arthroplasty Collaborative Investigators Outcomes following the single incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am 2009; 40:329–342. [DOI] [PubMed] [Google Scholar]
- 36.Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopedic fracture table. Clin Orthop Relat Res 2005; 441:115–124. [DOI] [PubMed] [Google Scholar]
- 37.Woolson ST, Pouliot MA, Huddleston JI. Primary total hip arthroplasty using an anterior approach and a fracture table: short term results from a community hospital. J Arthroplasty 2009; 24:999–1005. [DOI] [PubMed] [Google Scholar]
- 38.Jewett BA, Collis DK. High complication rate with anterior total hip arthroplasties on a fracture table. Clin Orthop Relat Res 2011; 469:503–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bergin PF, Doppelt JD, Kephart CJ, et al. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am 2011; 93:1392–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Masonis J, Thompson C, Odum S. Safe and accurate: learning the direct anterior total hip arthroplasty. Orthopedics 2008; 31: [PubMed] [Google Scholar]
- 41.De Geest T, Fennema P, Lenaerts G, et al. Adverse effects associated with the direct anterior approach for total hip arthroplasty: a Bayesian meta-analysis. Arch Orthop Trauma Surg 2015; 135:1183–1192. [DOI] [PubMed] [Google Scholar]
- 42.Roué J, de Thomasson E, Carlier AM, Mazel C. Influence of body mass index on outcome of total hip arthroplasty via a minimally invasive anterior approach. Rev Chir Orthop Reparatrice Appar Mot 2007; 93:165–170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


