Abstract
To investigate clinical and radiological features of IgG4-related disease (IgG4-RD) patients with intrathoracic involvement.
A prospective cohort study was performed and IgG4-RD patients were enrolled from January 2011 to March 2015 in Peking Union Medical College Hospital, in which the clinical and radiological characteristics of IgG4-RD patients with intrathoracic involvement were summarized.
Out of total 248 cases with IgG4-RD, 87 cases had intrathoracic lesions, including 58 male cases and 29 female cases, with average age of 54.19 ± 13.80 years. Hilar and mediastinal lymphadenopathy were the most common manifestations of IgG4-related intrathoracic disease, accounting for 52.9% (46/87). Other imaging findings of pulmonary disease included: solid nodular (25.3%), round-shaped ground-glass opacities (9.2%), alveolar-interstitial type (20.7%), bronchovascular type (23.0%), pleural effusion (4.6%), and pleural nodules or thickening (16.1%). Only 27 patients presented with respiratory symptoms, including cough, breathless, chest pain, and asthma. Compared with patients without intrathoracic disease, IgG4-related intrathoracic disease had higher IgG4 and C-reactive protein level, and higher incidence of allergy, fever, and multi-organ involvement. Most of lung interstitial disease, mediastinal mass, and bronchial thickening were sensitive to corticosteroid and immunosuppressant therapy, while 36.3% (8/22) of solitary nodular lesions were unresponsive to treatment. Eight patients were on no treatment, with 5 cases remained stable, 2 patients improved spontaneously, and 1 patient was lost follow-up.
Intrathoracic lesions are not rare in patients with IgG4-RD, involving bronchial thickening, nodules, ground glass opacity, pleural thickening/effusion, lymphadenopathy, etc. Efficacy of corticosteroid and immunosuppressant therapy were noted in most of patients with lung interstitial disease, mediastinal mass, and bronchial thickening.
INTRODUCTION
Immunoglobulin G4-related disease (IgG4-RD) is a systemic fibroinflammatory disease, characterized by elevated serum IgG4 levels and massive lymphoplasmacytic infiltration in involved lesions containing IgG4-positive plasma cells. Patients with IgG4-RD can have localized lesions or manifest diffuse systemic disease. Published studies have documented various organs involvement of IgG4-RD, presenting with the autoimmune pancreatitis, the sclerosing cholangitis, the sclerosing sialadenitis, the sclerosing dacryoadenitis, interstitial nephritis, lymphadenopathy, retroperitoneal fibrosis, IgG4-related hypophysitis, as well as the IgG4-related lung disease, etc.1–8
According to literatures, intrathoracic involvements of IgG4-RD can manifest various types, including interstitial lung disease, lung nodules, bronchial inflammation changes, mediastinal fibrosis as well as pleuritis. The whole picture of IgG4-RD associated intrathoracic manifestations remain not clear, though there were some studies reporting patients with this disease.1,2,9–16 In this article, our research goal is to explore the clinical and radiological features of patients with IgG4-RD associated intrathoracic manifestations.
METHODS
Enrollment
A multidisciplinary collaborative prospective cohort study of IgG4-RD patients has been conducted in Peking Union Medical College Hospital (PUMCH, Beijing, China) since January 2011.17–19 This study was approved by the Medical Ethics Committee of PUMCH. All patients signed written informed consent. Two hundred forty-eight newly diagnosed IgG4-RD patients were consecutively enrolled.
Patients were diagnosed as definite, probable, or possible IgG4-RD according to the 2011 comprehensive diagnostic criteria for IgG4-RD.20 Definite IgG4-RD must have the following characteristics: (1) organ enlargement, mass or nodular lesions, or organ dysfunction; (2) a serum IgG4 concentration >135 mg/dL; and (3) histopathological findings of >10 IgG4+ cells/high-power field (HPF) and an IgG4+/IgG+ cell ratio >40%. Possible IgG4-RD required (1) and (2), but with negative results on histopathology or without histopathological examination. Probable IgG4-RD required (1) and (3), but without increased serum IgG4.20 None of them met the criteria for other autoimmune diseases. None had malignant disease.
Out of these 248 patients, 87 cases had intrathoracic lesions, accounting for 35.1%. IgG4-RD-associated intrathoracic manifestations in this study included mediastinal lymphadenopathy, fibrosing mediastinitis, pleural lesions, airways or lung parenchymal disease, pericardial lesions, etc., verified by clinical manifestations, serological test, and imaging or pathological results.
Imaging and Pathological Analysis
Computed tomography (CT) images were taken for all patients at initial visit and during follow-up. Patient thoracic/lung radiological records were reviewed by respiratory physicians or radiologists. Some patients underwent positron-emission tomography/computed tomography (PET-CT). Fifty-one samples were assessed histologically using hematoxylin and eosin (HE) staining and immunostaining for IgG and IgG4. Patients with suspected IgG4-RD-associated intrathoracic manifestations were discussed at an open panel conference.
Serological Aspects
IgG4 levels, IgG and IgE concentrations were tested at the time of diagnosis. In addition, titers of antinuclear antibody (ANA) and rheumatoid factor (RF) were recorded.
Statistical Analysis
Statistical analysis was performed using the chi-squared test or Mann–Whitney U test to analyze variables. A probability of P < 0.05 was considered to be statistically significant.
RESULTS
Clinical Features of Patients
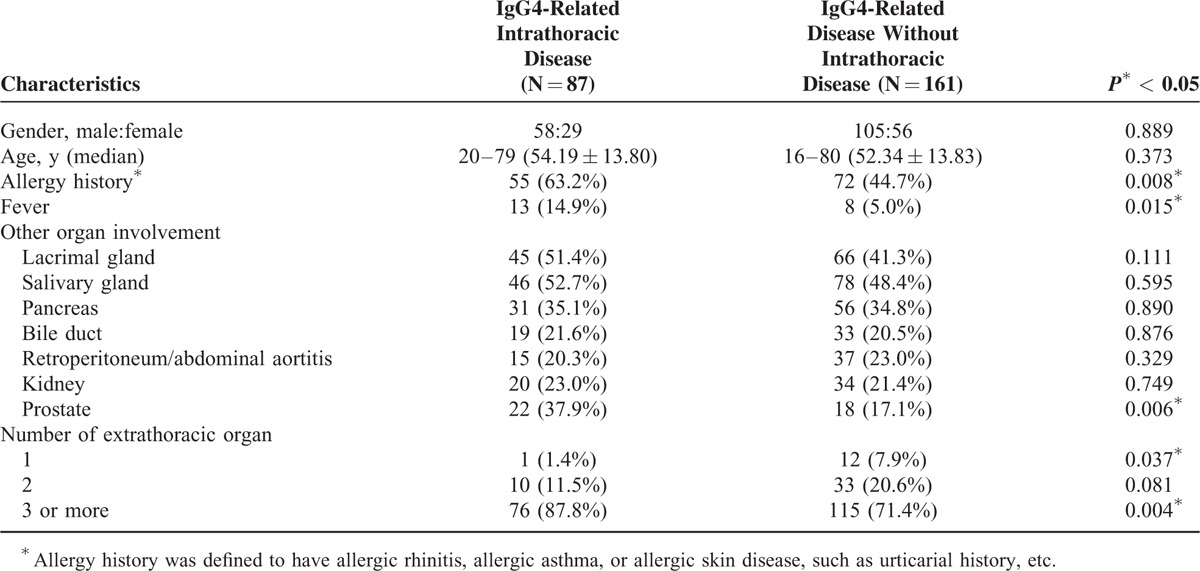
Two hundred forty-eight patients were diagnosed as IgG4-RD, with male to female ratio of 1.9:1.87 cases had intrathoracic manifestations, including 50 patients of definite, 1 patient of probable, and 36 cases of possible IgG4-RD. Patient profiles are summarized in Table 1. Respiratory symptoms were present in 27 patients, in which 23 cases had cough, 2 cases presented with dyspnea, and 2 cases complained chest pain. Of the 27 patients, 5 cases presented with asthma, who had extrathoracic involvements simultaneously. Respiratory lesions were revealed in the other nonsymptomatic 60 patients during imaging examination. Compared with IgG4-RD without intrathoracic disease, IgG4-related intrathoracic disease has higher possibility of allergy, fever and multi-organ involvements.
TABLE 1.
Background of Patients With IgG4-Related Intrathoracic Disease
Intrathoracic Involvement in IgG4-Related Sclerosing Disease
Intrathoracic involvement in IgG4-RD has been described in the lung parenchyma, airways and pleura, as well as pericardium and mediastinum. Of 87 patients, 3 patients manifesting asthma had normal CT findings, while single or multiple manifestations can be identified in other patients. Hilar and mediastinal lymphadenopathy were the most common manifestations in Ig G4-related intrathoracic disease, accounting for 52.9% (46/87), in which 21 cases had lymphadenopathy alone. Lung solid nodular and bronchovascular type were also frequent in IgG4-related intrathoracic disease, accounting 25.3% (22/87) and 23.0% (20/87), respectively. Seven cases have pericardium involvement and 3 patients with fibrosing mediastinitis manifested with mediastinal mass in CT images (Table 2). Twenty-one patients underwent PET-CT imaging, which revealed increased uptake of 18F-FDG in intrathoracic lesions.
TABLE 2.
Chest CT Findings of Patients With IgG4-Related Intrathoracic Disease at Baseline
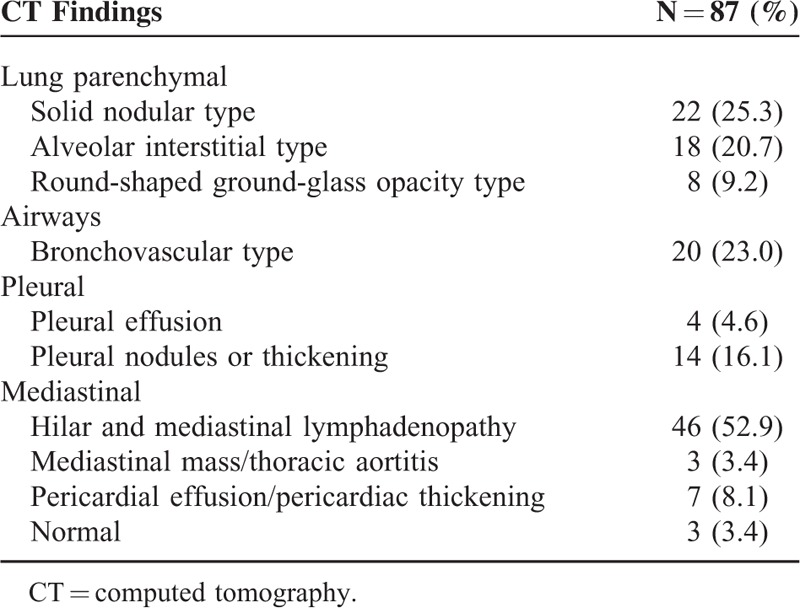
Radiographically, there are 4 major subtypes of IgG4-RD with lung involvement according to thoracic CT imaging: solid nodular type (solitary nodular lesions including mass); round-shaped ground-glass opacity (GGO) type, characterized by multiple round-shaped GGOs; alveolar interstitial type showing honeycombing, bronchiectasis or diffuse GGOs; and bronchovascular type presenting with thickening of bronchovascular bundles and/or interlobular septa.9Figure 1 shows radiologically detectable abnormalities at lungs.
FIGURE 1.
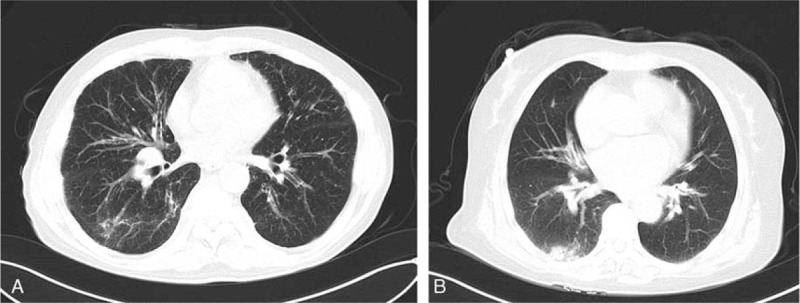
(A) Chest computed tomography (CT) image of a 62-year-old man shows alveolar interstitial manifestation and bronchial thickening in the right lung. (B) Thoracic CT image of a 69-year-old woman shows subpleural alveolar interstitial manifestation in the right inferior lung and thickening of the bronchial wall in the left lung.
Laboratory Findings
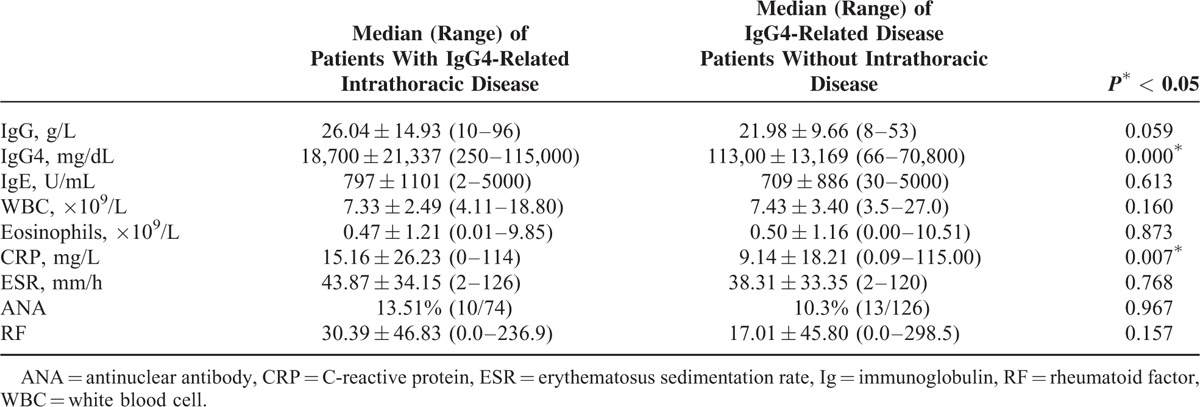
Summaries of laboratory findings of 87 patients are shown in Table 3, including white blood cell count, erythematosus sedimentation rate, C-reactive protein (CRP), serum IgG level, IgG4 level, as well IgE level. Compared with those without intrathoracic disease, the patients with IgG4-related intrathoracic disease had statistically significant higher concentrations of IgG4 and CRP (P < 0.05).
TABLE 3.
Laboratory Characteristics of Patients With IgG4-Related Intrathoracic Disease
Histopathological Findings
Tissue biopsy was performed in 51 patients, including salivary glands, lacrimal glands, pancreatic glands, lymph node, lung, sinus, retroperitoneal tissue, intracranial tissue, etc. Histological examination on HE staining was performed in all tissue samples, as well as immunohistochemical staining with anti-CD38, anti-CD138, anti-IgG, and anti-IgG4 mAb. In all cases, massive lymphocytes and plasma cells infiltration as well as fibrosis were revealed. The characteristic features were markedly increased IgG4-positive plasma cells (>10 plasma cells/HPF), with the ratio of IgG4+/IgG+ cells >40%. Out of 51 patients who underwent tissue biopsy, 10 patients had thoracic biopsy, including 6 of lung tissue/nodules, 3 of mediastinal tissue, 1 of pleural membrane, all biopsies were compatible with IgG4-RD. Figure 2 shows a typical finding of a 37-year-old lung involved IgG4-RD patient, presenting with cough and hemoptysis, who had surgical lung and transbronchial biopsy.
FIGURE 2.
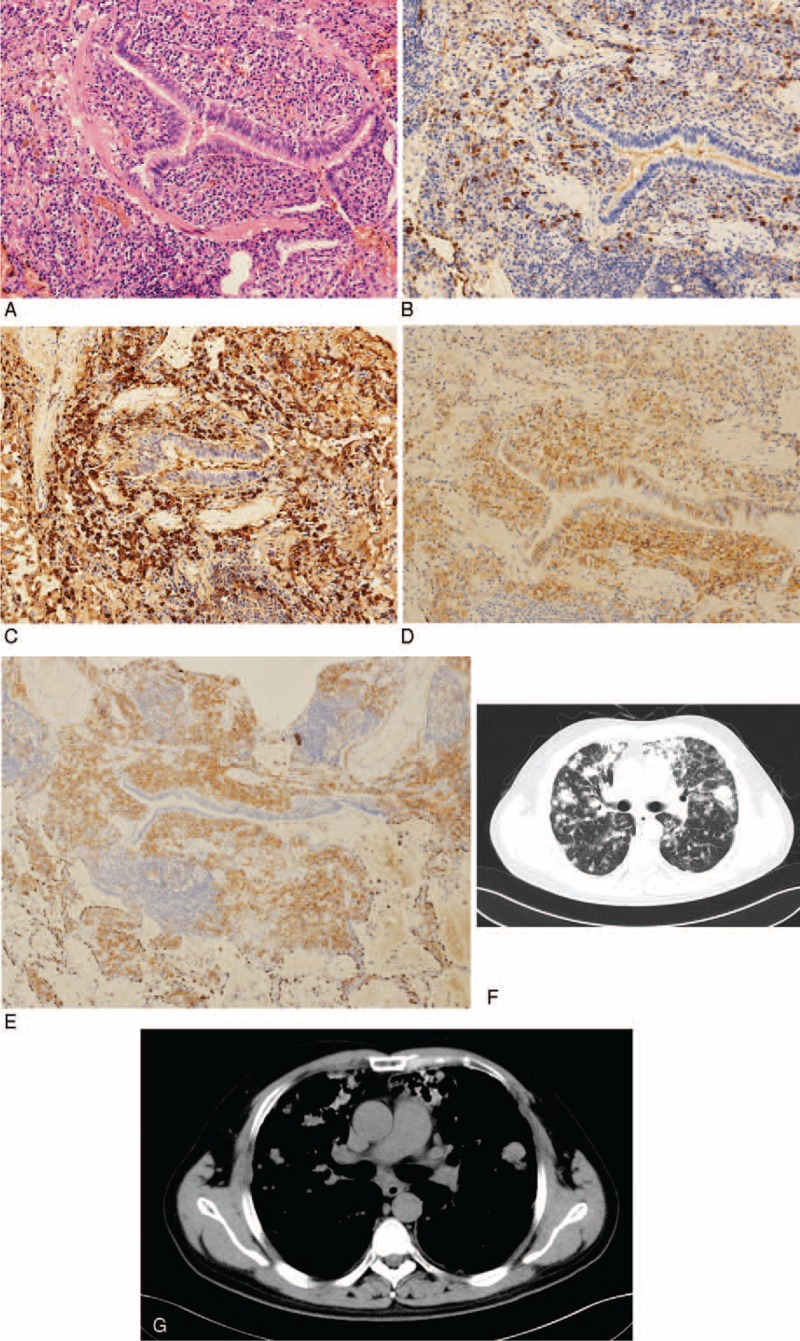
Lung biopsy of a 37-year-old man shows lymphocytes cells infiltration at the peripheral bronchus (hematoxylin and eosin staining, original magnification [A]: ×150). (B–E) Immunohistochemistry shows CD138+, IgG4 (+ >50 per high-power field), IgG4/IgG 46% (B: IgG4 × 150, C: IgG × 150, D: CD138 × 150, E: CD38 × 150). (F and G) Chest computed tomography image of the same man shows diffuse lung parenchymal lesions, including multiple ground-glass opacity and solid nodular manifestations in bilateral lungs.
Clinical Outcomes
Patients were followed up for a median 24 months (range 3–48 months). Since the efficacies of immunosuppressive agents have not been evaluated in prospective trials, we usually treat those patients with multi-organ (including vital organs) involvements with corticosteroid and immunosuppressive treatment. Patients with active multi-organ involvements but resistant to corticosteroid and immunosuppressive treatment accepted rituximab treatment. There are 8 cases with stable manifestations did not receive treatment.
Seventy-two patients received corticosteroid therapy, with a median initial dose of prednisone of 40 mg/d (range 30–60 mg/d). Forty-eight patients received combination therapy of immunosuppressants, including cyclophosphamide, mycophenolate mofetil, azathioprine, methotrexate, tripterygium wilfordii, tamoxifen, etc. Cyclophosphamide was the most frequently used immunosuppressant, adding up to 32 cases. Five patients only have immunosuppressant therapy. One refractory patient received rituximab.
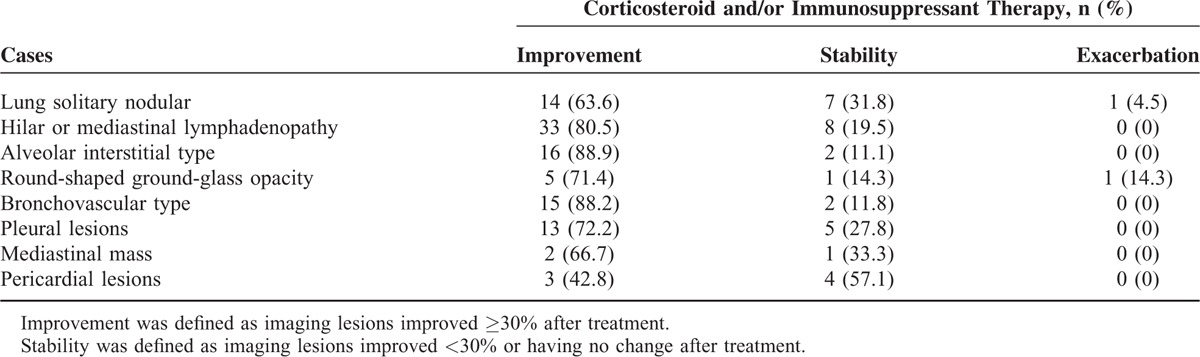
In 81.0% patients (64/79), the intrathoracic lesions improved after treatment and low dose of prednisone (≤10 mg/d) with or without immunosuppressants were used as the maintain therapy. Figure 3 shows improvement after treatment in a typical lung involved IgG4-RD patient. However, the improvement of extrathoracic lesions, such as salivary glands, lacrimal glands, pancreatitis, etc., was more significant than intrathoracic lesions. No obvious improvement was found in 8 patients with lung solitary nodular lesions, 8 patients with hilar or mediastinal lymphadenopathy, 2 cases with lung interstitial disease, and 2 cases with bronchial thickening, even though their extrathoracic lesions responded well (Table 4). Figure 3 shows radiological improvement of 1 IgG4-RD patient with bronchial thickening after treatment.
FIGURE 3.
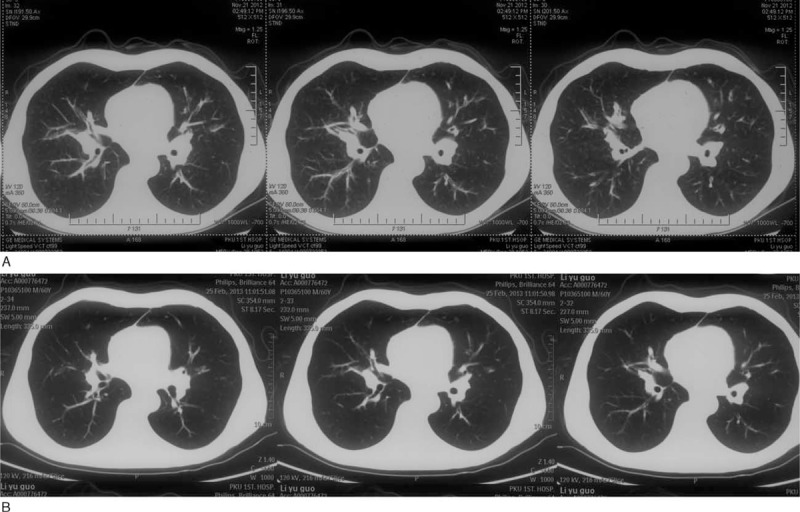
(A) Chest CT image of a 60-year-old man shows bronchial thickening in the bilateral hilar region at diagnosis. (B) Chest CT image of the same man shows obvious improvement after 3 mo treatment. CT = computed tomography.
TABLE 4.
Clinical Outcomes of Corticosteroid Therapy and/or Immunosuppressant Therapy on Patients With IgG4-Related Intrathoracic Disease
Eight patients did not receive corticosteroid or immunosuppressant therapy, including 5 patients presenting with only mediastinal lymphadenopathy, and 3 patients with mild tracheobronchial thickening. Except 1 was lost follow-up, others showed stable during follow-up. No deaths occurred.
DISCUSSION
Since IgG4-RD was recognized, many cases of lung involvement with IgG4-RD have been reported4,9–16; however, it is not clear how to diagnose IgG4-RD-related lung disease, because the lesions can manifest various performances. Therefore, we collected the clinical and radiological records of patients with suspected IgG4-associated intrathoracic disease, in order to determine the characteristics of patients with this disease.
In previous reports, according to chest CT performance, IgG4-related intrathoracic disease could be divided into mediastinal lesions (mediastinal lymphadenopathy and sclerosing mediastinitis) and lung disease; the latter was further categorized into 4 subtypes: alveolar interstitial type, bronchovascular type, round-shaped GGO, and solid nodular in lung or subpleural area.1,15 Based on the thoracic imaging findings, the corresponding pathological changes of IgG4-RD-associated intrathoracic disease might be interpreted as distribution of inflammatory (characterized by lymphocytes and IgG4 + plasma cells infiltration) and fibrotic lesions along the intrathoracic connective tissue and lymphatic tissue, which included bronchial vascular bundles, interlobular septa, and alveolar interstitium, as well as mediastinal or hilar lymph nodes. However, it was difficult to categorize simply because some of our patients presented with mixed performance of these features. Hilar and mediastinal lymphadenopathy was the most common manifestation in our study, accounting for 52.9%. Solid nodular type and bronchovascular type were also the frequent manifestations in IgG4-related lung disease, occupying 25.3% and 23.0%, respectively.
Our patients with IgG4-related intrathoracic disease had mild and nonspecific clinical symptoms. Respiratory symptoms were present in 27 patients, including cough, dyspnea, chest pain, etc., whereas the remaining 60 patients presented with abnormal thoracic imaging but lack of respiratory symptoms. Compared with IgG4-RD without intrathoracic disease, IgG4-related intrathoracic disease has higher possibility of allergy, fever, and inclined to have more than 3 extrathoracic organs involved. Moreover, laboratory examinations revealed significantly increased serum concentrations of IgG4 and CRP in IgG4-related intrathoracic disease. Therefore, patients with IgG4-RD might have more serious condition than that without intrathoracic involvement, though they had mild respiratory manifestations.
The data on the use of corticosteroid or immunosuppressive agents in the treatment of IgG4-related intrathoracic disease were relatively small. According to the international consensus guidance statement on the management and treatment of IgG4-RD, glucocorticoids are the first-line agent for remission induction, of which prednisone at a dosage of 30 to 40 mg/d is a common initial treatment.21 However, the optimal dose for IgG4-related lung disease and the course of corticosteroid therapy remains unclear. The exact regimen of corticosteroids has not been defined but in this study, for most patients, oral prednisone was administrated at an initial dosage of 0.5 to 1 mg/kg d. After 4 weeks, the prednisone dose tapered and was gradually reduced to 10 mg/d in a few months. Maintenance of low dose prednisone at 5 mg to 10 mg/d had been applied in the majority of patients for a long time. To avoid relapse or recurrence, the disease was closely monitored during follow-up and treatment regimen was adjusted according to the change of the disease. For some patients, the immunosuppressive agents were used in combination with corticosteroid, of which cyclophosphamide was frequently used in our study, which seemed beneficial. Pulmonary solitary nodules were more refractory to corticosteroid and immunosuppressant therapy, accounting for 36.4% (8/22), whereas only 2 patients with lung interstitial disease and 2 patients with bronchial thickening were unresponsive to therapy. However, in this study, the majority of extrathoracic lesions responded well to treatment. In addition, although a small number of patients with mild intrathoracic manifestations did not receive corticosteroid or immunosuppressant treatment, they achieved spontaneous remission or remained stable during the follow-up. In summary, corticosteroid and immunosuppressant therapy were considered effective treatment for IgG4-RD, though in some patients, intrathoracic lesions did not respond to corticosteroid therapy as well as extrathoracic lesions.
This study has some limitations. First, our findings are based on the results from a single-center, which might led to some bias. It remains to be determined whether our results can be generalized to other ethnicities or populations of different backgrounds. Second, the number of patients who underwent lung biopsy was relatively small, most patients were pathologically diagnosed with outside thoracic tissue; because of difficulty in tissue biopsy in some patients, they only fulfilled criteria of clinically characteristic organ swelling/masses and elevated serum IgG4. Therefore, the intrathoracic lesions in IgG4-RD might be over-estimated according to symptoms and imaging findings; confirming intrathoracic involvement in IgG4-RD is still challenging, especially in those with no improvement after treatment. Thirdly, in this study, only few patients underwent respiratory function test, so we cannot evaluate the impact of the disease on pulmonary function.
In conclusion, intrathoracic involvement in IgG4-RD has the following characters: Respiratory symptoms in IgG4-related intrathoracic disease included cough, dyspnea asthma, chest pain, etc., which were generally mild; inflammatory markers, such as CRP and IgG4 were higher in IgG4-related intrathoracic disease than those without intrathoracic disease; IgG4-RD involves almost all intrathoracic organs, including lymph nodes, alveolar interstitium, interlobular septa, and bronchovascular bundles, manifested mostly as hilar and mediastinal lymphadenopathy, followed with lung nodule, interstitial lung disease and bronchial thickening; and most of lung interstitial disease, mediastinal mass and bronchial thickening were sensitive to corticosteroid and immunosuppressant therapy.
Footnotes
Abbreviations: ANA = antinuclear antibody, CRP = C-reactive protein, CT = computed tomography, GGO = ground-glass opacity, HE = hematoxylin and eosin, IgG4-RD = immunoglobulin G4-related disease, PET-CT = positron-emission tomography/computed tomography, PUMCH = Peking Union Medical College Hospital, RF = rheumatoid factor.
YF and JS contributed equally to the work.
This work was supported by National Natural Science Foundation of China (no. 81172858, 81373190, 81471614, and 81571587).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Matsui S, Hebisawa A, Sakai F, et al. Immunoglobulin G4-related lung disease: clinicoradiological and pathological features. Respirology 2013; 18:480–487. [DOI] [PubMed] [Google Scholar]
- 2.Matsui S, Taki H, Shinoda K, et al. Respiratory involvement in IgG4-related Mikulicz's disease. Mod Rheumatol 2012; 22:31–39. [DOI] [PubMed] [Google Scholar]
- 3.Inoue D, Yoshida K, Yoneda N, et al. IgG4-related disease: dataset of 235 consecutive patients. Medicine (Baltimore) 2015; 94:e680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taniguchi T, Ko M, Seko S, et al. Interstitial pneumonia associated with autoimmune pancreatitis. Gut 2004; 53:770–771. [PMC free article] [PubMed] [Google Scholar]
- 5.Zen Y, Nakanuma YL. IgG4-related disease: a cross-sectional study of 114 cases. Am J Surg Pathol 2010; 34:1812–1819. [DOI] [PubMed] [Google Scholar]
- 6.Deshpande V, Gupta R, Sainani N, et al. Subclassification of autoimmune pancreatitis: a histologic classification with clinical significance. Am J Surg Pathol 2011; 35:26–35. [DOI] [PubMed] [Google Scholar]
- 7.Ghazzale A, Chari ST, Zhang L, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterol 2008; 134:706–715. [DOI] [PubMed] [Google Scholar]
- 8.Naitoh I, Nakazawa T, Ohara H, et al. Clinical significance of extrapancreatic lesions in autoimmune pancreatitis. Pancreas 2010; 39:e1–e5. [DOI] [PubMed] [Google Scholar]
- 9.Takato H, Yasui M, Ichikawa Y, et al. Nonspecific interstitial pneumonia with abundant IgG4-positive cells infiltration, which was thought as pulmonary involvement of IgG4-related autoimmune disease. Intern Med 2008; 47:291–294. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki H, Watanabe M, Ara T, et al. Immunoglobulin G4-related lung disease accompanied by organizing pneumonia. Intern Med 2013; 52:2105–2111. [DOI] [PubMed] [Google Scholar]
- 11.Wibmer T, Kropf-Sanchen C, Rüdiger S, et al. Isolated IgG4-related interstitial lung disease: unusual histological and radiological features of a pathologically proven case. Multidiscip Respir Med 2013; 8:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujiu K, Sakuma H, Miyamoto H, et al. Immunoglobulin G4-related inflammatory pseudotumor of the lung. Gen Thorac Cardiovasc Surg 2010; 58:144–148. [DOI] [PubMed] [Google Scholar]
- 13.Hui P, Mattman A, Wilcox PG, et al. Immunoglobulin G4-related lung disease: a disease with many different faces. Can Respir J 2013; 20:335–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahn JH, Hong SI, Cho DH, et al. A case of IgG4-related lung disease presenting as interstitial lung disease. Tuberc Respir Dis (Seoul) 2014; 77:85–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inoue D, Zen Y, Abo H, et al. Immunoglobulin G4-related lung disease: CT findings with pathologic correlations. Radiology 2009; 251:260–270. [DOI] [PubMed] [Google Scholar]
- 16.Yi ES, Sekiguchi H, Peikert T, et al. Pathologic manifestations of immunoglobulin (Ig)G4-related lung disease. Semin Diagn Pathol 2012; 29:219–225. [DOI] [PubMed] [Google Scholar]
- 17.Chen H, Lin W, Wang Q, et al. IgG4-related disease in a Chinese cohort: a prospective study. Scand J Rheumatol 2014; 43:70–74. [DOI] [PubMed] [Google Scholar]
- 18.Zhang J, Chen H, Ma Y, et al. Characterizing IgG4-related disease with 18F-FDG PET/CT: a prospective cohort study. Eur J Nucl Med Mol Imaging 2014; 41:1624–1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin W, Lu S, Chen H, et al. Clinical characteristics of immunoglobulin G4-related disease: a prospective study of 118 Chinese patients. Rheumatology (Oxford) 2015; pii:kev203.[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 20.Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol 2012; 22:21–30. [DOI] [PubMed] [Google Scholar]
- 21.Khosroshahi A, Wallace ZS, Crowe JL, et al. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015. doi:10.1002/art.39132. [DOI] [PubMed] [Google Scholar]


