Abstract
Toxoplasmosis is fatal in the immunocompromised individuals such as cancer patients with chemotherapy. Clinical toxoplasmosis in cancer patients is a great public health concern in China. We performed this meta-analysis to assess the seroprevalence and odds ratios (ORs) of Toxoplasma gondii in Chinese population with cancer compared with those without.
A methodical literature search was conducted with the help of the PubMed, Web of Knowledge, Embase, Chinese Web of Knowledge, Wanfang, and Chongqing VIP database. Case-control studies published from their inception until April 2015, reporting the seroprevalence of T. gondii in Chinese population with cancer, were covered as well. The nonweighted prevalence, pooled random-effects estimates of ORs, and 95% confidence intervals (CIs) were all calculated.
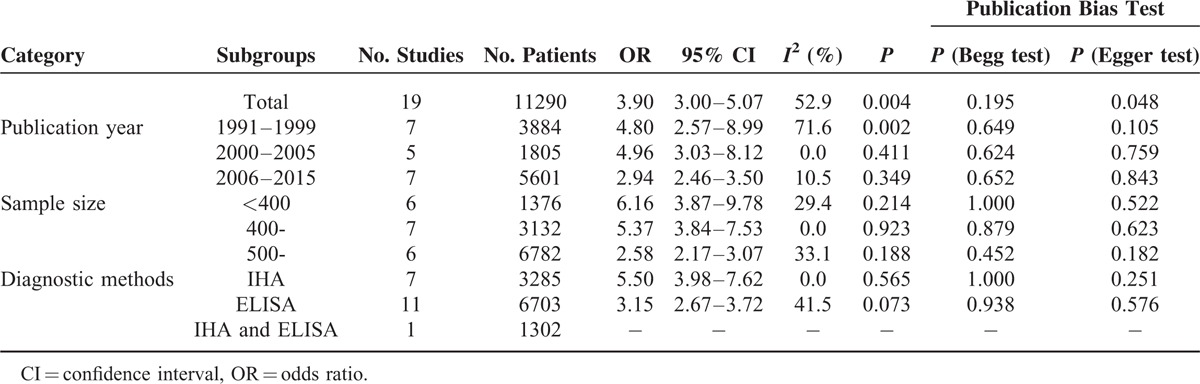
Nineteen studies including 4493 cases and 6797 controls were incorporated in the meta-analysis. The overall seroprevalence of T. gondii was higher in population with cancer compared with those without ((20.59% vs 6.31%, P < 0.001; OR 3.90, 95% CI 3.00–5.07). The OR of T. gondii in cancer patients is further subgrouped according to publication year, sample size, and diagnostic methods. The pooled OR estimates were 4.80 (95% CI 2.57–8.99) from 1991 to 1999, 4.96 (95% CI 3.03–8.12) during 2000 to 2005, and 2.94 (95% CI 2.46–3.50) during 2006 to 2015. The pooled OR estimates were 6.16 (95% CI 3.87–9.78) when the sample size was below 400, 5.37 (95% CI 3.84–7.53) when the sample size was between 400 and 500, and 2.58 (95% CI 2.17–3.07) when the sample size was above 500. The pooled OR estimates were 5.50 (95% CI 3.98–7.62) by using indirect hemagglutination assay method, and 3.15 (95% CI 2.67–3.72) by using enzyme-linked immunosorbent assay method.
The meta-analysis study found Chinese population with cancer had higher seroprevalence rates of T. gondii compared with those without.
INTRODUCTION
Toxoplasma gondii infects all warm-blooded vertebrates and imposes a major burden on human and animal health. Toxoplasmosis is one of the more common parasitic zoonoses with worldwide distribution caused by the protozoan parasite T. gondii,1 which infects one-third of the world's population.2 Humans become infected postnatally by ingesting tissue cysts from undercooked meat containing tissue cysts, ingesting food or drink contaminated with oocysts from infected cat feces and congenitally, or by accidentally ingesting from the environment.3T. gondii is transmitted to its final host through the consumption of an intermediate host, and can infect any warm-blooded vertebrate, including humans.4 Seroprevalence of Toxoplasma infection widely varies from around 6.1% to 74.5% among different regions of the world.5 In healthy humans, infection with T. gondii is usually asymptomatic. If T. gondii infects a pregnant woman with no previous exposure to the parasite, it can migrate through the placenta into the fetus and subsequently cause congenital toxoplasmosis.5 However, Toxoplasmosis is fatal in the immunocompromised individuals such as cancer patients with chemotherapy, HIV/AIDS patients, and organ-transplant recipients.6
Cancer is the leading cause of death in economically developed countries, and in developing countries it is the second leading cause of death.7 Deaths from cancer worldwide are projected to continue to rise, and the number of deaths will be up to 11 million deaths in 2030.8 China is the most populous nation in the world and the Chinese population has a high rate of cancer. In China, the numbers of new cases and deaths from cancer are increasing year by year. In 2008, it was 2.82 million (22.3% of world total) and 1.96 million (25.9%), and the number will forecast to 4.87 million and 3.60 million by 2030.9 Clinical toxoplasmosis in cancer patients is a great public health concern in China. Toxoplasmosis can lead to the active parasitemia and life-threatening disease due to the rupture of pre-existent cysts, contributing to worsening of the clinical condition.10 Hence, for this reason, a meta-analysis was carried out to assess the seroprevalence and odds ratios (ORs) of T. gondii in Chinese population with cancer compared with those without.
MATERIALS AND METHODS
Ethical Approval
The ethical approval was not necessary in the review articles.
Strategy for Literature Search
The available literature on the seroprevalence of T. gondii in Chinese population with cancer were obtained by perusing through the PubMed, Web of Knowledge, Embase, Chinese Web of Knowledge, Wanfang, and Chongqing VIP database. The literature was restricted to the Chinese and/or English language, and searched from their inception until April 2015, with the search themes of “Toxoplasma gondii or toxoplasmosis or T. gondii”, combined with “cancer or oncology or malignant neoplasm or malignant tumor”.
Criteria for Inclusion and Exclusion
Strict criteria for inclusion and exclusion were used in this meta-analysis, and all selected studies had to meet the given inclusion criteria: studies using a case-control design in mainland China; the participants of cancer group must be patients diagnosed with cancer; participants of control group must be taken from normal population without cancer; sample size of case group must be more than 30 adults with cancer; and must provide information about the seroprevalence of T. gondii in cancer group and control group. Similarly, only those studies were excluded that were animal studies; repeated studies; review studies or abstracts; and the studies which included only cancer patients.
Any disagreements with the selected studies were resolved by discussion and the involvement of another author.
Data Extraction
Two investigators performed the data by using a standardized data extraction from each article. In case of a disagreement between the 2 researchers, a discussion would be carried out to arrive at an agreement. Information was extracted from each study: general information, including name of the first author, year of publication, total sample size, collection criteria of controls, number of patients with positive test results, and T. gondii diagnostic methods.
Quality Assessment
The Newcastle–Ottawa Scale11 was used to assess the quality of included studies.
Statistical Analysis
The association between the seroprevalence of T. gondii and cancer in Chinese population was estimated by means of ORs and corresponding 95% confidence intervals (CIs). The implication of the pooled OR was determined by Z test. The models used were the fixed-effects model or random-effects model. The model to be used was determined by whether or not there existed heterogeneity among studies.12,13 The stability of sensitivity was assessed by eliminating 1 single study each time.14 The potential of publication bias was examined by Begg funnel plot and Egger test.15–17 In this study, meta-analyses were conducted by using STATA version 12.0 software (Stata Corporation, College Station, TX), and P < 0.05 was considered to be statistically significant.
RESULTS
Search Result and Characteristic of Included Studies
The systematic literatures search yielded 683 relevant articles. After a careful examination of each article's abstract, 440 were considered as having potential value and the full texts were retrieved for detailed evaluation. Then 403 potentially relevant articles were excluded from the meta-analysis because of their obvious irrelevance to the purpose of this study. At the end, 19 studies including 4493 cases and 6797 controls, whose dates of publication were from their inception to April 2015, were deemed eligible and were incorporated in the meta-analysis.18–36Figure 1 shows the flow diagram for the selection of included studies. The individuality and characteristics of these articles are given in Table 1.
FIGURE 1.
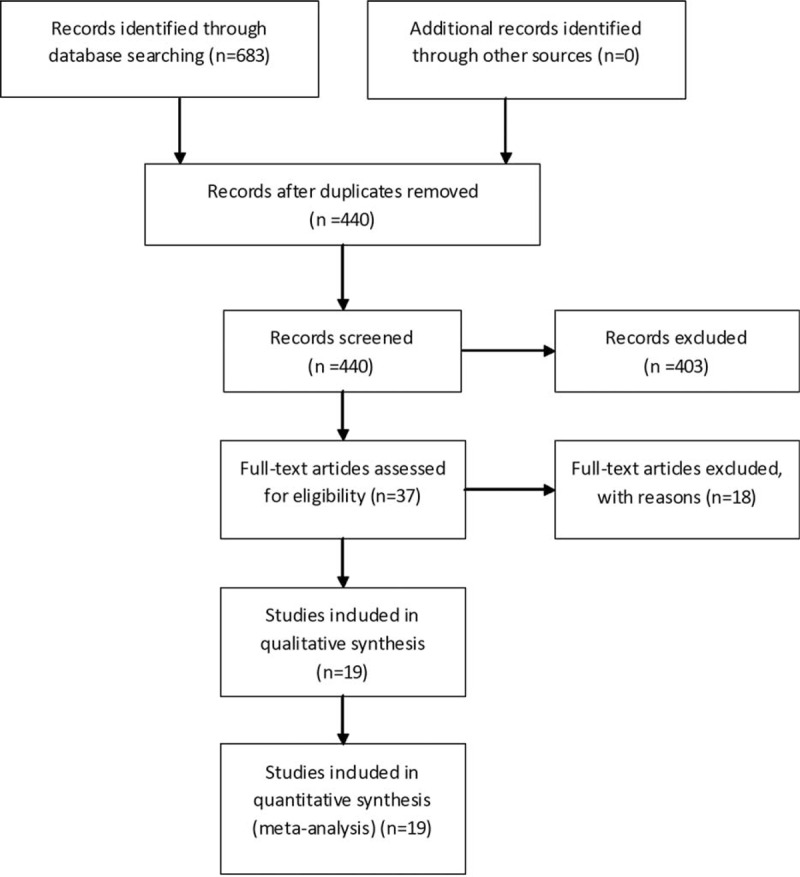
Flow diagram of included/excluded studies.
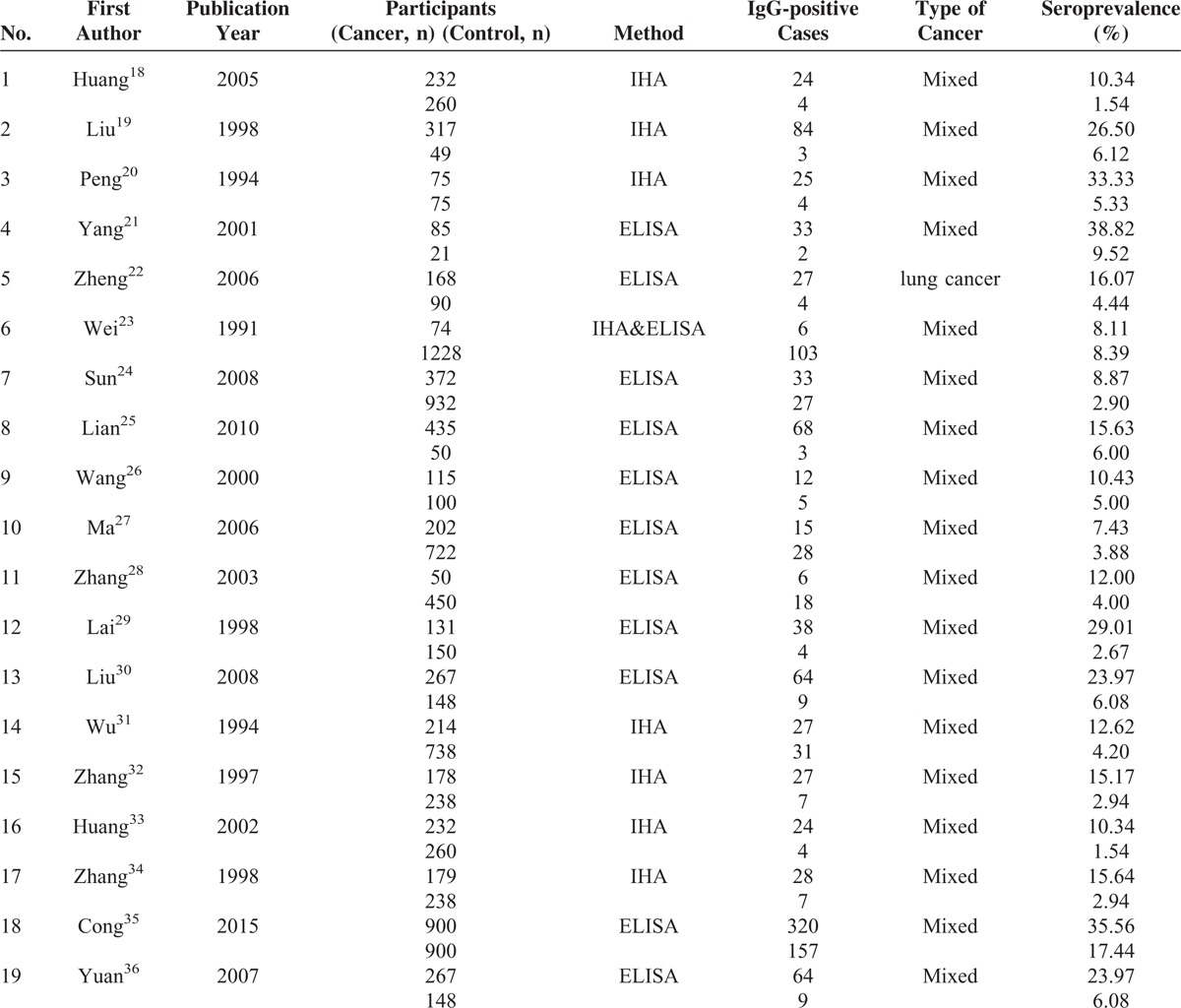
TABLE 1.
Characteristics of Included Studies
Risk of Bias Assessment
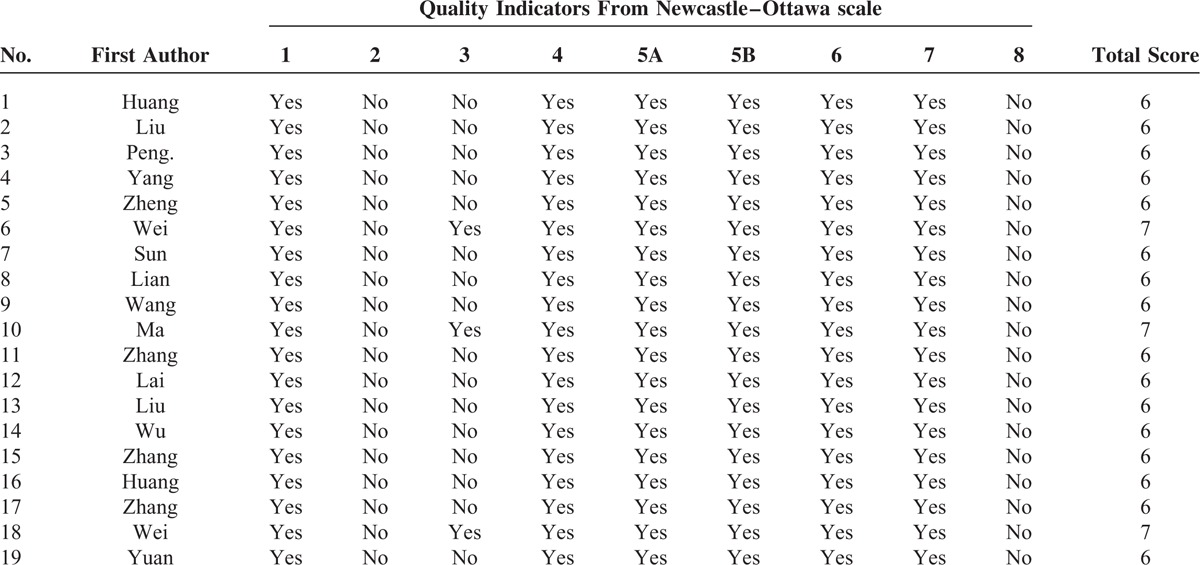
The quality of included studies is presented in Table 2. The higher scores reflect the better study quality, and the average scores of the included studies were above 6.
TABLE 2.
Assessment of Study Quality
Prevalence Rates of Seroprevalence of Toxoplasma gondii in Cancer Patients
The overall seroprevalence of T. gondii was higher in a population with cancer compared with a population without (P < 0.001). The overall seroprevalence of T. gondii was 20.59% in the Chinese population with cancer, and the seroprevalence of T. gondii was 6.31% in the noncancer group.
Odds Ratios of Toxoplasma gondii in Cancer Patients
A pooled random-effects meta-analysis was conducted using data from 19 studies, which estimated the levels of T. gondii in Chinese population with cancer compared with that without. This analysis included data for 4493 cases with cancer and 6797 controls without cancer. As shown in Figure 2, the odds of T. gondii was associated with a 3.90-fold increased risk of cancer patients when compared with the control group (OR 3.90, 95% CI 3.00–5.07). However, the heterogeneity analysis of the effect sizes of depression (Q = 38.22, P = 0.004, I2 = 52.9%) showed that there was a relatively high-level heterogeneity in our meta-analysis.
FIGURE 2.
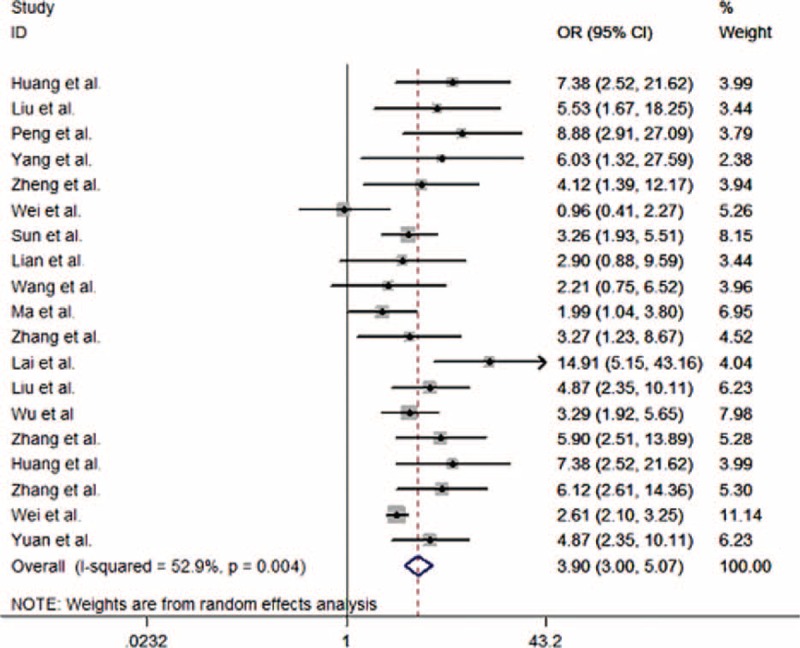
Forest plot for the meta-analysis of Toxoplasma gondii in Chinese population with and without cancer.
Subgroup Analyses
The OR of T. gondii in cancer patients was further subgrouped according to publication year, sample size, and diagnostic methods, and the OR of these subgroups is presented in Table 3. The pooled OR estimates were 4.80 (95% CI 2.57–8.99) from 1991 to 1999, 4.96 (95% CI 3.03–8.12) during 2000 to 2005, and 2.94 (95% CI 2.46–3.50) during 2006 to 2015. It was also apparent that the pooled OR estimate decreased with the increase in sample size. For instance, the pooled OR estimates were 6.16 (95% CI 3.87–9.78) when the sample size was below 400, 5.37 (95% CI 3.84–7.53) when the sample size was between 400 and 500, and 2.58 (95% CI 2.17–3.07) when the sample size was above 500. The pooled OR estimates were 5.50 (95% CI 3.98–7.62) by using indirect hemagglutination assay (IHA) method, and 3.15 (95% CI 2.67–3.72) by using enzyme-linked immunosorbent assay (ELISA) method. Information regarding the heterogeneity of the data as well as the publication bias is depicted in Table 3.
TABLE 3.
Odds Ratios of Toxoplasma gondii in Chinese Population With and Without Cancer (Subgroup Analyses)
Publication Bias
Begg test and Egger test were used to give value to the publication bias. No significant bias in the included studies (P = 0.195) was revealed using the modified Begg linear regression test (Figure 3). However, a significant publication bias in the included studies was observed using the Egger test (P = 0.048) (Table 3).
FIGURE 3.
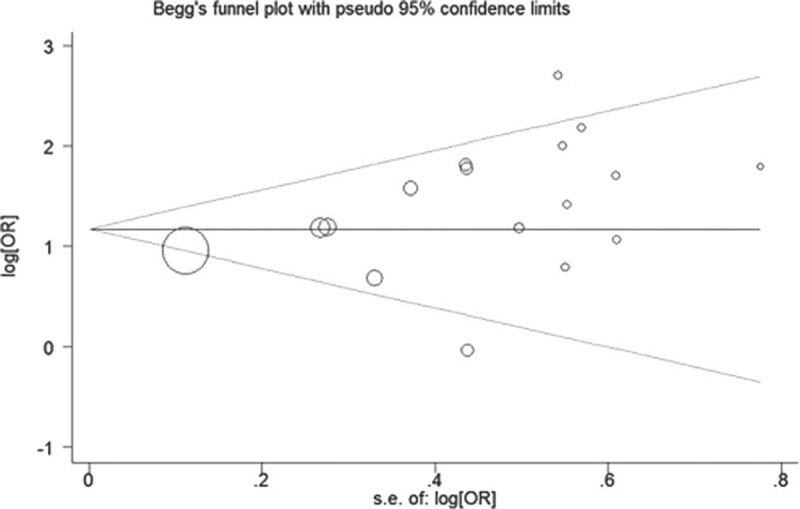
Begg funnel plot for publication bias test.
DISCUSSION
Toxoplasma gondii is an extremely successful protozoal parasite, which infects almost all mammalian species including humans.37 Although most infections are clinically asymptomatic, in immunocompromised patients, it can cause severe disease manifestations and even death.38 It is a big problem that the cancer patients were seropositive for T. gondii tested. The cancer may induce severe opportunistic parasitic disease in antitumor treatment process. This is the first meta-analysis that aimed to assess the seroprevalence and ORs of T. gondii in Chinese population with cancer compared with that without. In this review, 19 studies including 4493 cases and 6797 controls were incorporated, and we found the overall seroprevalence of T. gondii was higher in a population with cancer compared with that without in the Chinese population. The overall seroprevalence of T. gondii was 20.59% in the Chinese population with cancer. The results were higher than some studies assessing the nation-wide prevalence (7.88%)39 and the prevalence of psychiatric patients (11.3%) in China.40 Meanwhile, the results were similar to this situation in foreign countries.41–43
This systematic review showed the level of T. gondii was significantly higher in cancer patients when compared with those without (OR 3.90, 95% CI 3.00–5.07). The cancer patients with low immune function were significantly more susceptible than those without.44
The serological tests are regarded as the gold standard and are used for diagnosis of T. gondii infection. The most common methods of diagnosis are SFT, indirect immunofluorescence assay, direct agglutination test, latex agglutination test, ELISA, improved self-adaptive Genetic Algorithms, and the IgG avidity test.5 This review revealed that IHA and ELISA techniques are the most common method used for T. gondii detection in China. Both humoral and cell-mediated mechanisms are included in the immunologic response to T. gondii infection.45
We must become aware of the heterogeneity that is present in our study, so subgroup analyses were done to explore potential sources of heterogeneity including publication year, sample size, and diagnostic methods. In the subgroup analyses, the pooled OR estimates were 4.80 from 1991 to 1999, 4.96 during 2000 to 2005, and 2.94 during 2006 to 2015. It was also apparent that the pooled OR estimates decreased with the increase of sample size. For instance, the pooled OR estimates were 6.16 when the sample size was below 400, 5.37 when the sample size was between 400 and 500, and 2.58 when the sample size was above 500. The pooled OR estimates were 5.50 by using IHA method and 3.15 by using ELISA method. When we grouped items according to publication year, sample size, and diagnostic methods, then the heterogeneity of different sample sizes and diagnostic methods decreased, so differences in sample size and diagnostic methods may cause this heterogeneity.
The study faces numerous possible drawbacks which may influence the result. First, we confined our studies published in English and Chinese, and this did not include the unpublished researches; in this way related unpublished studies may be left out and this method could direct to the oversight of some related studies. Second, the heterogeneity is present in our study. Third, the present meta-analysis was based on case-control studies. The case-control study is a type of observational study and it may also be more difficult to establish the timeline of exposure to disease outcome. So we could not determine the causation between the development of cancer and T. gondii infection. Finally, no significant bias in the included studies (P = 0.195) was revealed using the modified Begg linear regression test. However, a significant publication bias in the included studies was observed using the Egger test (P = 0.048). Apart from these drawbacks, there exist some key benefits in the analysis. This is the first meta-analysis that aimed to assess the seroprevalence and OR of T. gondii in the Chinese population with cancer compared with those without. Likewise, the relationship between the development of cancer and T. gondii infection is statistically more persuasive than any single study.
CONCLUSIONS
The Chinese population with cancer had higher seroprevalence rates of T. gondii compared with those without.
Acknowledgments
We thank all our colleagues working in the Department of Epidemiology and Health Statistics, School of public health of Central South University.
Author contributions: LC and CJ conceived and designed the study, performed the experiments, and drafted the manuscript. ZL performed the experiments and participated in the analysis and interpretation of data. PC performed the statistical analysis and helped to draft the manuscript. All authors have read and approved the final manuscript.
Footnotes
Abbreviations: CI = confidential interval, ORs = odds ratios.
Funding: The authors have no funding or support to report.
Conflicts of interest: The authors have declared that no conflicts of interest exist.
REFERENCES
- 1.Tentera AM, Heckerotha AR, Weissb LM. Toxoplasma gondii: from animals to humans. Int J Parasitol 2000; 30:1217–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montoya JG, Liesenfeld O. Toxoplasmosis. Lancet 2004; 363:1965–1976. [DOI] [PubMed] [Google Scholar]
- 3.Dubey JP, Jones JL. Toxoplasma gondii infection in humans and animals in the United States. Int J Parasitol 2008; 38:1257–1278. [DOI] [PubMed] [Google Scholar]
- 4.Vittecoq M, Elguero E, Lafferty KD, et al. Brain cancer mortality rates increase with Toxoplasma gondii seroprevalence in France: infection. Genet Evol 2012; 12:496–498. [DOI] [PubMed] [Google Scholar]
- 5.Sakikawa M, Noda S, Hanaoka M, et al. Anti-Toxoplasma antibody prevalence, primary infection rate, and risk factors in a study of toxoplasmosis in 4,466 pregnant women in Japan. Clin Vaccine Immunol 2012; 19:365–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang L, He LY, Meng DD, et al. Seroprevalence and genetic characterization of Toxoplasma gondii in cancer patients in Anhui Province, Eastern China. Parasites Vectors 2015; 8:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J 2011; 61:69–90. [DOI] [PubMed] [Google Scholar]
- 8.Cannon1 G, Gupta P, Gomes F, et al. Prevention of cancer and non-communicable diseases. Asian Pac J Cancer Prevent 2012; 13:3–11. [PubMed] [Google Scholar]
- 9.Yang YL, Liu L, Wang Y, et al. The prevalence of depression and anxiety among Chinese adults with cancer: a systematic review and meta-analysis. BMC Cancer 2013; 13:393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubey JP. History of the discovery of the life cycle of Toxoplasma gondii. Int J Parasitol 2009; 39:877–882. [DOI] [PubMed] [Google Scholar]
- 11.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta analyses. Available at: http://www.lri.ca/programs/clinical_epidemiology/oxford.asp Accessed April 29, 2015. [Google Scholar]
- 12.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brittain EH, Fay MP, Follmann DAA. valid formulation of the analysis of noninferiority trials under random effects meta-analysis. Biostatistics 2012; 13:637–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chootrakool H, Shi JQ, Yue R. Meta-analysis and sensitivity analysis for multi-arm trials with selection bias. Stat Med 2011; 30:1183–1198. [DOI] [PubMed] [Google Scholar]
- 15.Munafò MR, Clark TG, Flint J. Assessing publication bias in genetic association studies: evidence from a recent meta-analysis. Psychiatry Res 2004; 129:39–44. [DOI] [PubMed] [Google Scholar]
- 16.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994; 50:1088–1101. [PubMed] [Google Scholar]
- 17.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res ed) 1997; 315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang L, Li YB, Zhao R, Wang SJ. The application of dot immunogold filtration assay for the detection of antibody Toxoplasma gondii IgG inserum of the tumor patient. Acta Parasitol Med Entomol Sin 2005; 12:17–19. [Google Scholar]
- 19.Liu AQ, Li YJ. Study on malignant tumor patients accompanied with Toxoplasma gondii infection. Chin J Zoonoses 1998; 14:73–74. [Google Scholar]
- 20.Peng LJ, Bao YY, Xu LF, et al. Study on malignant tumor accompanied with Toxoplasma gondii infection. Parasitic Dis Control Res 1994; 23:21–23. [Google Scholar]
- 21.Yang ZJ, Wang CB, Hou XF. Analysis on malignant tumor patients accompanied with Toxoplasma gondii infection. Henan J Oncol 2001; 14:135–136. [Google Scholar]
- 22.Zheng SL, Yang QS, Ma XH. The relationship between non small cell lung cancer and Toxoplasma infection. Chin J Pathophysiol 2006; 22:1031–1032. [Google Scholar]
- 23.Wei RM, Ding ZY, Xu XP, Zeng XJ. The survey of toxoplasma infection on special crowd of situation in Jiangxi province. Chin J Zoonoses 1991; 7:31–32. [Google Scholar]
- 24.Sun YF, Jia N, Du HF, et al. The analysis of antibody IgG of patients suffering different kinds of malignant tumor in Lanzhou area tested by ELISA. China Med Herald 2008; 5:120–121. [Google Scholar]
- 25.Lian XW, Li KS, Du HF, et al. The contrast analysis of antibody IgG and IgM of Patients with malignant tumor in Lanzhou area. Health Vocational Educ 2010; 28:117–118. [Google Scholar]
- 26.Wang BL, Pan XZ, Yin YK, Weng XH. Investigation of anti-Toxoplasma gondii antibodies in immunodeficient patients. Chin J Parasitol Parasit Dis 2000; 18:224–226. [PubMed] [Google Scholar]
- 27.Ma XB, Cai L, Zhang BX, et al. A survey on Toxoplasma gondii infection of human in Shanghai. Shanghai J Prevent Med 2006; 18:483–486. [Google Scholar]
- 28.Zhang LX, Huang WG, Yuan JF. Study on Toxoplasma infections in Wuxi. Chin J Schistosomiasis Control 2003; 15:466–467. [Google Scholar]
- 29.Lai XQ, Zhu JY, Wei QD. Investigation of anti-Toxoplasma gondii antibodies of patients with malignant tumors in Yuexi area. Guangdong Med J 1998; 19:281–282. [Google Scholar]
- 30.Liu Q, Yuan ZG, Gao SY, Liu B, Liu XF. Detection of antibody IgG against Toxoplasma gondii from pregnant/parturient women and cancer patients in Changchun region. J Pathogen Biol 2008; 3:122–123. [Google Scholar]
- 31.Wu ZQ, Yang SS, Wu SP, Wang PS, Zhang AL. The serum epidemiological analysis of Toxoplasma infection in patients with cancer and diabetes. Chin J Parasitic Dis Control 1994; 7:72–73. [Google Scholar]
- 32.Zhang WZ, Zhao JL, Yin WD, Qu M. Survey on Toxoplasma antibody in sera of tumor. J Zhangjiakou Med Coll 1997; 14:5–6. [Google Scholar]
- 33.Huang L, Li YB, Zhang W. Analysis of antibody examination of the tumor patient combined gondii infection. Ningxia Med J 2002; 24:335–336. [Google Scholar]
- 34.Zhang WZ, Zhao JL, Yin WD, Qu M. Survey on Toxoplasma antibody in sera of tumor. Chin J Parasitic Dis Control 1998; 11:354. [Google Scholar]
- 35.Cong W, Liu GH, Meng QF, et al. Toxoplasma gondii infection in cancer patients: prevalence, risk factors, genotypes and association with clinical diagnosis. Cancer Lett 2015; 359:307–333. [DOI] [PubMed] [Google Scholar]
- 36.Yuan ZG, Gao SY, Liu Q, et al. Toxoplasma gondii antibodies in cancer patients. Cancer Lett 2007; 254:71–74. [DOI] [PubMed] [Google Scholar]
- 37.Schlüter D, Däubener W, Scharesd G, et al. Animals are key to human toxoplasmosis. Int J Med Microbiol 2014; 304:917–929. [DOI] [PubMed] [Google Scholar]
- 38.Verma R, Khanna P. Development of Toxoplasma gondii vaccine. Human Vaccines Immunother 2013; 9:291–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Coordinating Office of the National Survey on the important human parasitic disease. A national survey on current status of the important human parasitic disease in human population. Chin J Parasitol Parasitic Dis 2005; 23:332–340. [PubMed] [Google Scholar]
- 40.Xiao Y, Yin JG, Jiang N, et al. Seroepidemiology of human Toxoplasma gondii infection in China. BMC Infect Dis 2010; 10:4.Doi: 10.1186/1471-2334-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sucilathangam G, Palaniappan N, Sreekumar C, Anna T. Serological survey of toxoplasmosis in a district in Tamil Nadu: hospital-based study. Indian J Med Res 2013; 137:560–563. [PMC free article] [PubMed] [Google Scholar]
- 42.Thomas F, Lafferty KD, Brodeur J, et al. Incidence of adult brain cancers is higher in countries where the protozoan parasite Toxoplasma gondii is common. Biol Lett 2012; 8:101–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahmadpour E, Daryani A, Sharif M, et al. Toxoplasmosis in immunocompromised patients in Iran: a systematic review and meta-analysis. J Infect Dev Ctries 2014; 8:1503–1510. [DOI] [PubMed] [Google Scholar]
- 44.Benson VS, Green J, Beral V. The relationship between owning a cat and the risk of developing a brain cancer in a prospective study of UK women: comment on Thomas et al. Biology Lett 2012; 8:1040–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Beazley DM, Egerman RS. Toxoplasmosis. Semin Perinatol 1998; 22:332–338. [DOI] [PubMed] [Google Scholar]


