Abstract
Calcification of the middle cerebral artery (MCA) is uncommon in the healthy elderly. Whether calcification of the MCA is associated with cerebral ischemic stroke remains undetermined. We intended to investigate the association using Agatston calcium scoring of the MCA. This study retrospectively included 354 subjects with ischemic stroke in the MCA territory and 1518 control subjects who underwent computed tomography (CT) of the brain. We recorded major known risk factors for ischemic stroke, including age, gender, hypertension, diabetes mellitus, smoking, hyperlipidemia, and obesity, along with the MCA calcium burden, measured with the Agatston calcium scoring method. Univariate and modified logistic regression analyses were performed to examine the association between the MCA calcification and ischemic stroke.
The univariate analyses showed significant associations of ischemic stroke with age, hypertension, diabetes mellitus, smoking, total MCA Agatston score, and the presence of calcification on both or either side of the MCA. Subjects with the presence of MCA calcification on both or either side of the MCA were 8.46 times (95% confidence interval, 4.93–14.53; P < 0.001) more likely to have a cerebral infarct than subjects without MCA calcification after adjustment for the major known risk factors, including age, hypertension, diabetes mellitus, and smoking. However, a higher degree of MCA calcification reflected by the Agatston score was not associated with higher risk of MCA ischemic stroke after adjustment for the confounding factors and presence of MCA calcification. These results suggest that MCA calcification is associated with ischemic stroke in the MCA territory. Further prospective studies are required to verify the clinical implications of the MCA calcification.
INTRODUCTION
Atherosclerosis, a systemic disease characterized by deposition of fatty materials, inflammatory cells, and scar tissue within the arterial walls, is the major cause of cardiovascular and cerebrovascular events.1,2 In developed countries, atherosclerosis-related cardiovascular and cerebrovascular events are estimated to be the cause of death in ∼50% of cases.3 Although the cerebral and carotid atherosclerosis develops later than coronary atherosclerosis,4,5 stroke and myocardial infarction share common cardiovascular risk factors, such as hypertension, diabetes mellitus, smoking, and hyperlipidemia, and generally begin to occur at similar age with similar age-specific event rates.6,7
Intracranial atherosclerosis occurs in >80% of older white persons with significant associations with conventional cardiovascular risks factors.8 As coronary artery calcification is highly correlated with the atherosclerotic burden and risk for future cardiovascular events,9,10 intracranial artery calcification is reasonably considered a potential risk factor for cerebral ischemic stroke. A number of studies utilizing different methods to measure the calcium burden of the carotid arteries have shown discordant results.11–14 Some authors believed that calcifications stabilize plaques whereas others stated an increased risk of thromboembolic disease associated with the calcifications.15,16 In a recent large population-based cohort study using noncontrast computed tomography (CT) of the calcified plaques, Bos et al established intracranial carotid artery calcification as an independent risk factor for stroke.17
Although the middle cerebral artery (MCA) usually shows less calcium burden on CT than the intracranial carotid artery does,18 calcification of the MCA may play a crucial role due to its proximity to the ischemic event. Previous studies used a binary or a morphology-based qualitative grading method to measure intracranial calcifications.11,18–20 In coronary artery studies, a more sophisticated and quantitative measure of calcification using the Agatston score has been employed by computing the products of CT-density-based weighted scores and areas of calcified lesions.21 This scoring method can be easily applied semiautomatically to MCA calcifications whereas it is difficult to be applied to the intracranial internal carotid artery due to its proximity to the bony structures of the skull base.
In this study, we hypothesized that subjects with a higher burden of MCA calcification are more likely to have an ischemic stroke than those with lower or no burden. Therefore, the purpose of our study was to quantitatively investigate whether the MCA calcification is associated with ischemic cerebral stroke in the corresponding territory using the Agatston calcium scoring method.
METHODS
Subjects
This study was approved by the Institutional Review Board of Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, and the requirement for written informed consent from the subjects (or from the next of kin/caregiver) for use of the clinical records of the subjects was waived. All subject records/information was anonymized and deidentified before analysis. Our data are available upon request because of an ethical restriction of the institutional review board. Readers may contact the board (+886-2-87923311 ext. 10552) or the authors to request the data.
Between 2006 and 2008, a total of 2260 consecutive subjects underwent noncontrast brain studies in our 64-slice multidetector-row CT examination suite (Brilliance 64, Philips Medical Systems, Best, the Netherlands) for a variety of clinical indications, which were mainly head trauma (562 subjects, 24.9%), stroke (485, 21.5%), headaches (462, 20.4%), dementia (388, 17.2%), brain tumors (87, 3.8%), and seizures (36, 1.6%). We excluded a total of 388 subjects (17.2%) mainly due to age <40 years old (314, 80.9%), followed by clinical history or imaging findings of intracranial hemorrhage (75, 19.3%), brain tumors (19, 4.9%), and brain infections (3, 0.8%). A total of 1872 subjects (865 women and 1007 men; mean age, 66 years; range, 41–99) were eligible for analysis. Subjects having matched clinical and imaging findings of cerebral infarct in the MCA territory were assigned to the MCA stroke group whereas the rest were assigned to the control group. Magnetic resonance (MR) imaging diagnosis of acute cerebral infarction was made by visualization of high signal intensities on diffusion-weighted images and corresponding low signal intensities on apparent diffusion coefficient maps. Two board-certificated neuroradiologists (HWK and CYC with 25 and 10 years of clinical experience in neuroimaging interpretation respectively), blinded to the clinical information of the subjects, reviewed all the CT and MR images from our picture archiving and communication system to record imaging evidences of cerebral infarct.
Major known risk factors of ischemic stroke were documented from medical record review and analysis of electronic health records in our hospital information system. Subjects were diagnosed as hypertensive if they presented systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg or if they were on any antihypertensive medication. Diabetes mellitus was diagnosed if the fasting serum glucose level was >7.8 mmol/L or if the subject was taking any antidiabetic medication. Subjects were marked smokers if smoking >1 cigarette/day over the preceding year before the ischemic stroke. The hyperlipidemia was defined based on the history of lipid-lowering therapy or serum total cholesterol level of >200 mg/dL. Obesity was recorded when the body mass index was 30 or greater.
CT Imaging and Agatston Calcium Scoring of the MCA
All CT examinations were performed with a standardized noncontrast protocol (120 kVp; 280 mA; collimation, 40 × 0.625 mm; table feed, 14.4 mm/rotation; pitch, 0.58). Image reconstructions were made with a field of view of 100 mm; matrix size, 512 × 512; slice thickness, 3.0 mm; increment, 0.5 mm.
For quantification of the MCA calcium burden, all reconstructions were transferred to an independent PC-based workstation (Syngo CaScoring Wizard, Siemens Medical Solutions, Erlangen, Germany). According to the Agatston method, CT density ≥ 130 Hounsfield units in ≥ 2 continuous pixels were automatically marked in color by the workstation. The 2 neuroradiologists defined the regions of interests (ROIs) by scrutinizing the bilateral MCAs on both axial and reconstructed coronal CT images (Figure 1). The Agatston score of each ROI in the bilateral MCAs was generated by the workstation and the scores from each MCA were summed. The bilateral MCA Agatston scores were then added up to a total MCA Agatston score. For subjects with multiple brain CT examinations, only the most recent ones were analyzed for the MCA calcium scoring.
FIGURE 1.
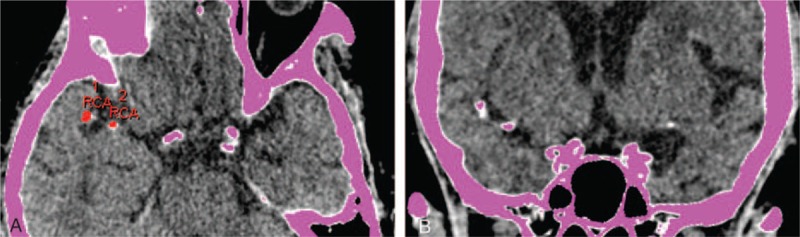
Agatston calcium scoring for a 70-year-old woman. (A) Axial and (B) coronal noncontrast CT images demonstrate 2 calcifications (RCA 1 and 2; Agatston score, 52.3) with density >130 Hounsfield units in 2 continuous pixels, automatically highlighted in pink color by the workstation. The RCA, an acronym of the right coronary artery, is referred to the right MCA in this study. CT = computed tomography, MCA = middle cerebral artery.
Statistical Analysis
The hemisphere of cerebral infarct was attributed to the left, right, or both MCA territories. The between-group differences in risk factors for ischemic stroke were evaluated for statistical significance with the Mann–Whitney U test for continuous variables and with the Fisher exact test for categorical variables because the data were not normally distributed. Significant risk factors in the univariate tests were included as predictors in modified logistic regression models, which had more accurate regression parameter estimates by reference to valid information identities.22 In these models, ischemic strokes on both or either side of the MCA territories were considered the response variable and odds ratios and 95% confidence intervals (CI) of the risk factors were estimated. The adjusted effect of the individual MCA calcification on ipsilateral cerebral infarct was evaluated in the modified logistic regression models. The intraclass correlation coefficient was used to evaluate inter-rater agreement of the selected ROIs. The statistical significance was evaluated using the 2-tailed test in the univariate analyses and Type-III likelihood ratio statistic for each predictor in the model along with the Wald CI for the parameter estimates in the modified logistic regression model, both with the nominal Type-I error at the 5% level. All the statistical analyses were performed with an IBM SPSS Statistics for Mac (version 20; IBM Corp., Armonk, NY).
RESULTS
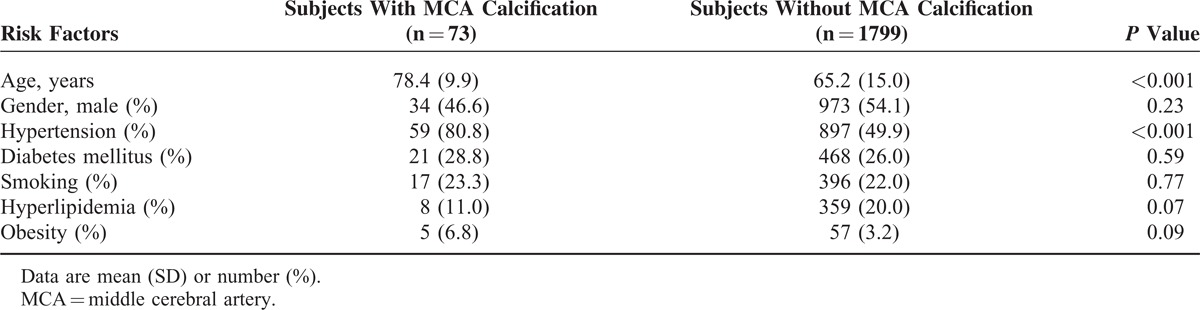
The baseline characteristics of the study group are shown in Table 1. Of the 1872 subjects in our study, the most prevalent major known risk factor in our subjects was hypertension (51.1%), followed by diabetes mellitus (26.1%), smoking (22.1%), hyperlipidemia (19.6%), and obesity (3.3%). A total of 354 (18.9%) subjects (mean age, 72 years; range, 41–99 years) were in the MCA stroke group and 1518 (81.1%) subjects (mean age, 64 years, range 41–99 years) were in the control group. In the MCA stroke group, 237 (66.9%) subjects underwent MR imaging for confirmation of the cerebral infarct within a median of 1 day (interquartile range, 0–3) after the brain CT study. Among those, 157 (66.2%) subjects showed acute cerebral infarcts in the MCA territory whereas 80 (33.8%) showed old infarcts in the territory matching clinical histories and symptoms. A total of 73 out of 1872 (3.9%) subjects had calcifications on both or either side of the MCA in a wide range of total MCA Agatston scores (median, 3.8; range, 0.1–436.1). The inter-rater reliability index of the total MCA Agatston scores was high (intraclass correlation coefficient = 0.998). The univariate analyses showed significant associations of ischemic stroke with age, hypertension, diabetes mellitus, smoking, total MCA Agatston score, and presence of calcification on both or either side of the MCA, disregarding laterality of the MCA calcification and hemispheric infarct. Among the documented risk factors for ischemic stroke, MCA calcifications were significantly associated with age and hypertension and marginally associated with hyperlipidemia and obesity (Table 2).
TABLE 1.
Characteristics of the Subjects in the Study
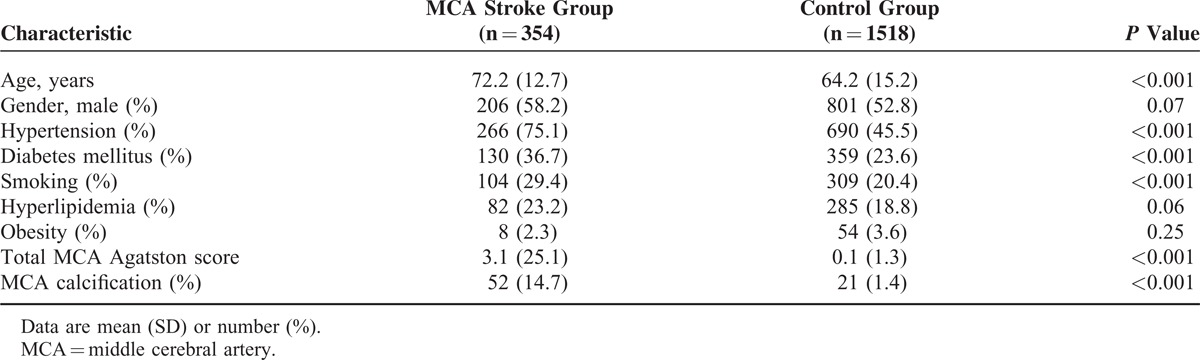
TABLE 2.
Associations of MCA Calcification and Risk Factors for Ischemic Stroke
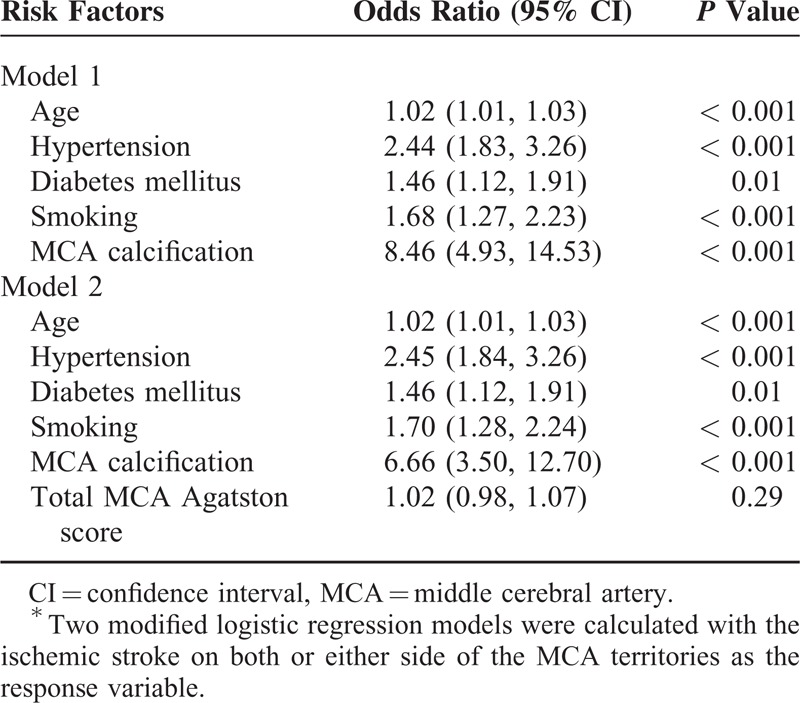
The modified logistic regression models showed significant associations between ischemic stroke and the significant risk factors identified in the univariate analyses. Considering interactions between the confounders in logistic regression models, we found no interaction between the age and the gender (P = 0.53) whereas hypertension, diabetes mellitus, and smoking significantly attenuated the association between age and ischemic infarct (odds ratios, 1.06 vs 1.04, P = 0.02; 1.06 vs 1.02, P < 0.001; 1.06 vs 1.03, P = 0.02 respectively). After adjustment for age, hypertension, diabetes mellitus, and smoking, subjects with the presence of MCA calcification on both or either side of the MCA were 8.46 times (95% CI, 4.93–14.53; P < 0.001) more likely to have a cerebral infarct than subjects without MCA calcification (Table 3, Model 1). A higher degree of MCA calcification reflected by the Agatston score was not significantly associated with higher risk of MCA ischemic stroke after adjustment for the confounding factors and the presence of MCA calcification (95% CI, 0.98–1.07; P = 0.29; Table 3, Model 2).
TABLE 3.
MCA Calcification and Risk Factors for Ischemic Stroke in Modified Logistic Regression Analyses by Subject∗
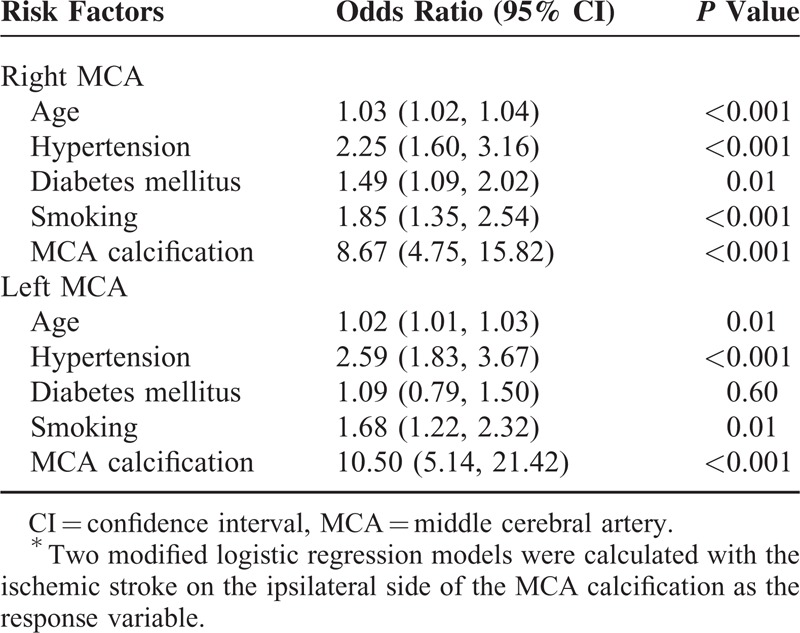
Among the 73 subjects with MCA calcifications, 52 (71.2%) showed calcifications on the right side, 37 (50.7%) on the left side, and 16 (21.9%) on both sides. The adjusted odds ratios for the cerebral infarct on the ipsilateral side of the MCA calcification were 8.67 (95% CI, 4.75–15.82; P < 0.001) on the right and 10.50 (95% CI, 5.14–21.42; P < 0.001) on the left, even after controlling for the familywise Type-I error rate at 0.05 via Bonferroni correction (Table 4).
TABLE 4.
MCA Calcification and Risk Factors for Ischemic Stroke in Modified Logistic Regression Analysis by Vessel∗
DISCUSSION
Our results provide 2 important clinical implications. First, the MCA calcification was significantly associated with cerebral infarct in the corresponding territories after adjustment for the major known risk factors, including age, hypertension, diabetes mellitus, and smoking. Second, a higher degree of MCA calcification reflected by the Agatston score was not significantly associated with higher risk of MCA ischemic stroke after adjustment for the confounding factors and the presence of MCA calcification.
Atherosclerosis is a systemic disease, commonly present in the aorta, coronary artery, and carotid arteries. Many risk factors have been shown to correlate with coronary artery calcification, including old age, elevated serum cholesterol, elevated triglycerides, diminished high-density lipoprotein cholesterol, hypertension, diabetes mellitus, smoking, and obesity.23–25 In line with the findings in the literature, our results showed significant correlations between MCA calcification and the risk factors for ischemic stroke, including old age and hypertension. The predictive value of arterial calcification for stroke has been established in studies focusing on the coronary arteries, aortic arch, and extracranial and intracranial carotid arteries.17,26,27 Our results further extend these evidence to the MCA and support a systemic effect of cardiovascular risk factors, by which calcified plaques, advanced stages of atherosclerosis, play a significant role in stroke events.
This study, to the best of our knowledge, is the first to apply the quantitative Agatston score to investigate the correlation between the MCA calcification and the corresponding ischemic stroke. The scoring method is advantageous in reflecting the calcium burden on the artery of interest as a whole rather than a focal morphological abnormality. In the study of Nandalur et al, the degree of calcification in the extracranial carotid artery is significantly associated with luminal stenosis and ischemic symptoms.28 Large randomized trials have also shown the association of carotid stenosis and stroke as well as the benefit of carotid endarterectomy.29–31 In contrast to the effect of arterial calcifications in the coronary and carotid arteries, the implication of atherosclerosis of the MCA is less investigated. This issue is particularly important in populations of Chinese and African ancestries in whom stenosis of the large intracranial artery is a common cause of ischemic stroke.32–34 In a study of intracranial arterial calcifications, Kassab et al found that the presence of calcification on head CT appears to correlate with the presence of intracranial stenosis on catheter angiography.35 Accordingly, the MCA calcification is a reasonable risk factor of ischemic stroke in the corresponding cerebral territories, a hypothesis supported by the results of our study. Among the documented risk factors in our study, the presence of MCA calcification was a less common but strong risk factor associated with ischemic stroke. The findings may imply a contribution to ischemic stroke from a calcification-related stenosis of the MCA, which may lead to regional hemodynamic disturbance.36 However, the degree of MCA calcification reflected by the calcium scores represented only 1 important characteristic of the atherosclerotic plaque. Therefore, in patients with the strong risk factor, MCA calcification, increased MCA calcium burden might not necessarily parallel increased degree of arterial stenosis or the risk of ischemic stroke. In the study of Kassab et al, the calcium grade of the intracranial artery, semi-quantified with a 5-point system, is not unexceptionally consistent with the dichotomous degree of stenosis.35 In clinical practice, we do not suggest performing calcium quantification because the significant high risk of ischemic infarct could have already been implied by the presence of MCA calcification itself.
The strength of our study was the application of the accurate and objective Agatston scoring method to measure the MCA calcium burden. Furthermore, we assessed clinical and brain CT findings to categorize subjects, a method to unravel a direct causal relationship between MCA calcification and ischemic stroke in the corresponding territories. However, the number of subjects with MCA calcification was relatively small because of its low prevalence rate. The limitations of our study were basically due to the retrospective design and the fact that the included subjects were from only 1 local medical center. Although all subjects with indications for brain CT were included in our study, there remained a probability of selection bias. In addition, some significant but less common risk factors for ischemic stroke, such as mitral stenosis, sickle cell disease, and hyperhomocysteinemia, were not evaluated in our study. The Agatston calcium scoring method used in our study was semiautomatic and required manual selection of the MCA calcification. However, the neuroradiologists generally had no difficulty in selecting ROIs for the segmentation of the calcification on CT images. Another potential limitation was the fact that the cerebral embolic infarct may mimic thrombotic infarct and confound the analysis. Furthermore, an evaluation of the noncalcified plaque and the correlation between MCA calcium burden and luminal stenosis requires administration of contrast material, not included in our routine stroke workup, was not available in our study.
CONCLUSIONS
In conclusion, our study shows that MCA calcification is associated with ischemic stroke after adjustment for age, hypertension, diabetes mellitus, and smoking. Further prospective studies are required to verify the clinical implications of the MCA calcification.
ACKNOWLEDGMENTS
We are grateful to those who contributed to the collection of data: Wan-Ting Liou, Wei-Ting Ding, Ju-Ping Chung, and Yueh-E Chiu.
Footnotes
Abbreviations: CT = computed tomography, MCA = middle cerebral artery, ROI = region of interest.
Competing Interests: The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Mann JM, Davies MJ. Vulnerable plaque. Relation of characteristics to degree of stenosis in human coronary arteries. Circulation 1996; 94:928–931. [DOI] [PubMed] [Google Scholar]
- 2.Lusis AJ. Atherosclerosis. Nature 2000; 407:233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011; 123:e18–e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathur KS, Kashyap SK, Kumar V. Correlation of the extent and severity of atherosclerosis in the coronary and cerebral arteries. Circulation 1963; 27:929–934. [DOI] [PubMed] [Google Scholar]
- 5.Solberg LA, McGarry PA, Moossy J, et al. Distribution of cerebral atherosclerosis by geographic location, race, and sex. Lab Invest 1968; 18:604–612. [PubMed] [Google Scholar]
- 6.Gentil A, Bejot Y, Lorgis L, et al. Comparative epidemiology of stroke and acute myocardial infarction: the Dijon Vascular project (Diva). J Neurol Neurosurg Psychiatry 2009; 80:1006–1011. [DOI] [PubMed] [Google Scholar]
- 7.Rothwell PM, Coull AJ, Silver LE, et al. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study). Lancet 2005; 366:1773–1783. [DOI] [PubMed] [Google Scholar]
- 8.Bos D, van der Rijk MJ, Geeraedts TE, et al. Intracranial carotid artery atherosclerosis: prevalence and risk factors in the general population. Stroke 2012; 43:1878–1884. [DOI] [PubMed] [Google Scholar]
- 9.Pletcher MJ, Tice JA, Pignone M, et al. Using the coronary artery calcium score to predict coronary heart disease events: a systematic review and meta-analysis. Arch Intern Med 2004; 164:1285–1292. [DOI] [PubMed] [Google Scholar]
- 10.Rumberger JA, Simons DB, Fitzpatrick LA, et al. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation 1995; 92:2157–2162. [DOI] [PubMed] [Google Scholar]
- 11.Babiarz LS, Yousem DM, Bilker W, et al. Middle cerebral artery infarction: relationship of cavernous carotid artery calcification. AJNR Am J Neuroradiol 2005; 26:1505–1511. [PMC free article] [PubMed] [Google Scholar]
- 12.Taoka T, Iwasaki S, Nakagawa H, et al. Evaluation of arteriosclerotic changes in the intracranial carotid artery using the calcium score obtained on plain cranial computed tomography scan: correlation with angiographic changes and clinical outcome. J Comput Assist Tomogr 2006; 30:624–628. [DOI] [PubMed] [Google Scholar]
- 13.de Weert TT, Cakir H, Rozie S, et al. Intracranial internal carotid artery calcifications: association with vascular risk factors and ischemic cerebrovascular disease. AJNR Am J Neuroradiol 2009; 30:177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bugnicourt JM, Chillon JM, Massy ZA, et al. High prevalence of intracranial artery calcification in stroke patients with CKD: a retrospective study. Clin J Am Soc Nephrol 2009; 4:284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burke AP, Weber DK, Kolodgie FD, et al. Pathophysiology of calcium deposition in coronary arteries. Herz 2001; 26:239–244. [DOI] [PubMed] [Google Scholar]
- 16.Hunt KJ, Pankow JS, Offenbacher S, et al. B-mode ultrasound-detected carotid artery lesions with and without acoustic shadowing and their association with markers of inflammation and endothelial activation: the atherosclerosis risk in communities study. Atherosclerosis 2002; 162:145–155. [DOI] [PubMed] [Google Scholar]
- 17.Bos D, Portegies ML, van der Lugt A, et al. Intracranial carotid artery atherosclerosis and the risk of stroke in whites: the Rotterdam Study. JAMA Neurol 2014; 71:405–411. [DOI] [PubMed] [Google Scholar]
- 18.Mak HK, Wong CW, Yau KK, et al. Computed tomography evaluation of intracranial atherosclerosis in Chinese patients with transient ischemic attack or minor ischemic stroke—its distribution and association with vascular risk factors. J Stroke Cerebrovasc Dis 2009; 18:158–163. [DOI] [PubMed] [Google Scholar]
- 19.Chen XY, Lam WW, Ng HK, et al. The frequency and determinants of calcification in intracranial arteries in Chinese patients who underwent computed tomography examinations. Cerebrovasc Dis 2006; 21:91–97. [DOI] [PubMed] [Google Scholar]
- 20.Babiarz LS, Yousem DM, Wasserman BA, et al. Cavernous carotid artery calcification and white matter ischemia. AJNR Am J Neuroradiol 2003; 24:872–877. [PMC free article] [PubMed] [Google Scholar]
- 21.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15:827–832. [DOI] [PubMed] [Google Scholar]
- 22.Cheng PE, Liou M, Aston JAD. Likelihood ratio tests with three-way tables. J Am Stat Assoc 2012; 105:740–749. [Google Scholar]
- 23.Wexler L, Brundage B, Crouse J, et al. Coronary artery calcification: pathophysiology, epidemiology, imaging methods, and clinical implications. A statement for health professionals from the American Heart Association. Writing Group Circulation 1996; 94:1175–1192. [DOI] [PubMed] [Google Scholar]
- 24.Breen JF, Sheedy PF, 2nd, Schwartz RS, et al. Coronary artery calcification detected with ultrafast CT as an indication of coronary artery disease. Radiology 1992; 185:435–439. [DOI] [PubMed] [Google Scholar]
- 25.Clarkson TB, Prichard RW, Morgan TM, et al. Remodeling of coronary arteries in human and nonhuman primates. JAMA 1994; 271:289–294. [PubMed] [Google Scholar]
- 26.Bos D, Ikram MA, Elias-Smale SE, et al. Calcification in major vessel beds relates to vascular brain disease. Arterioscler Thromb Vasc Biol 2011; 31:2331–2337. [DOI] [PubMed] [Google Scholar]
- 27.Hermann DM, Gronewold J, Lehmann N, et al. Coronary artery calcification is an independent stroke predictor in the general population. Stroke 2013; 44:1008–1013. [DOI] [PubMed] [Google Scholar]
- 28.Nandalur KR, Baskurt E, Hagspiel KD, et al. Carotid artery calcification on CT may independently predict stroke risk. AJR Am J Roentgenol 2006; 186:547–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991; 325:445–453. [DOI] [PubMed] [Google Scholar]
- 30.MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70–99%) or with mild (0–29%) carotid stenosis. European Carotid Surgery Trialists’ Collaborative Group. Lancet 1991; 337:1235–1243. [PubMed] [Google Scholar]
- 31.Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA 1995; 273:1421–1428. [PubMed] [Google Scholar]
- 32.Caplan LR, Gorelick PB, Hier DB. Race, sex and occlusive cerebrovascular disease: a review. Stroke 1986; 17:648–655. [DOI] [PubMed] [Google Scholar]
- 33.Huang YN, Gao S, Li SW, et al. Vascular lesions in Chinese patients with transient ischemic attacks. Neurology 1997; 48:524–525. [DOI] [PubMed] [Google Scholar]
- 34.Chen XY, Wong KS, Lam WW, et al. Middle cerebral artery atherosclerosis: histological comparison between plaques associated with and not associated with infarct in a postmortem study. Cerebrovasc Dis 2008; 25:74–80. [DOI] [PubMed] [Google Scholar]
- 35.Kassab MY, Gupta R, Majid A, et al. Extent of intra-arterial calcification on head CT is predictive of the degree of intracranial atherosclerosis on digital subtraction angiography. Cerebrovasc Dis 2009; 28:45–48. [DOI] [PubMed] [Google Scholar]
- 36.Woodcock RJ, Jr, Goldstein JH, Kallmes DF, et al. Angiographic correlation of CT calcification in the carotid siphon. AJNR Am J Neuroradiol 1999; 20:495–499. [PMC free article] [PubMed] [Google Scholar]


