Abstract
A growing number of patients with chronic artery disease suffer from angina, despite the optimal medical management (ie, β-blockers, calcium channel blockers, and long-acting nitrates) and revascularization. Currently, enhanced external counterpulsation (EECP) therapy has been verified as a noninvasive, safe therapy for refractory angina. The study was designed to evaluate the efficacy of EECP in patients with chronic refractory angina according to Canadian Cardiovascular Society (CCS) angina class.
We identified systematic literature through MEDLINE, EMBASE, the Cochrane Clinical Trials Register Database, and the ClinicalTrials. gov Website from 1990 to 2015. Studies were considered eligible if they were prospective and reported data on CCS class before and after EECP treatment. Meta-analysis was performed to assess the efficacy of EECP therapy by at least 1 CCS angina class improvement, and proportion along with the 95% confidence interval (CI) was calculated. Statistical heterogeneity was calculated by I2 statistic and the Q statistic. Sensitivity analysis was addressed to test the influence of trials on the overall pooled results. Subgroup analysis was applied to explore potential reasons for heterogeneity.
Eighteen studies were enrolled in our meta-analysis. Pooled analysis showed 85% of patients underwent EECP had a reduction by at least one CCS class (95%CI 0.81–0.88, I2 = 58.5%, P < 0.001). The proportion of patients enrolled at primarily different studies with chronic heart failure (CHF) improved by at least 1 CCS class was about 84% after EECP (95%CI 0.81–0.88, I2 = 32.7%, P = 0.1668). After 3 large studies were excluded, the pooled proportion was 82% (95%CI 0.79–0.86, I2 = 18%, P = 0.2528). Funnel plot indicated that some asymmetry while the Begg and Egger bias statistic showed no publication bias (P = 0.1495 and 0.2859, respectively).
Our study confirmed that EECP provided an effective treatment for patients who were unresponsive to medical management and/or invasive therapy. However, the long-term benefits of EECP therapy needed further studies to evaluate in the management of chronic refractory angina.
INTRODUCTION
With the improvements in cardiovascular care, an increasing number of patients, particularly those with advanced coronary artery disease (CAD), have severe symptom of angina pectoris that intractable to treatment of optimal medical therapy. It is estimated that between 600,000 and 1.8 million patients in the United States suffer from chronic refractory angina with about 50,000 new cases emerging per year, and in continental Europe approximately 30,000 to 50,000 new cases are diagnosed each year.1 Due to the increase of CAD-related survival rate and population age, the incidence and prevalence of these patients will continue to rise. Therefore, the care of these patients is challenging. In order to better manage the population group, the definition of the refractory angina is vital important. The ESC Joint Study Group on the Treatment of Refractory Angina and Canadian Cardiovascular Society (CSS)/Canadian Pain Society Joint Guidelines defined this condition as “chronic duration more than 3 months characterized by the presence of angina caused by coronary insufficiency in the presence of CAD which is refractory to a combination of medical therapy, angioplasty/percutaneous interventions, and coronary bypass surgery in patients with evidence of ischemia.”1,2 As the conventional therapy has limitation, this is an urgent need to search for new treatment for patients. The current therapies of refractory angina including pharmacology (ie, Nicorandil, Ivabradine, Ranolozine, Allopurinol, Perhexiline), noninvasive therapy compromise enhanced external counterpulsation (EECP) and extracorporeal shockwave therapy, invasive therapy, neuromodulation, and others.3,4 According to current studies, EECP as a noninvasive therapy has been proven to be a promising treatment for relieving angina, and it has been given II a Class Recommendation in the 2013 ESC guidelines on the management of stable CAD.5
EECP therapy, a nonpharmacologic, noninvasive outpatient treatment, has been approved by the U.S. Food and Drug Administration (FDA) in patients with stable or unstable angina pectoris, congestive heart failure, acute myocardial infraction, and cardiogenic shock.6 Now this technique is used for patients with angina ineligible to conventional medical therapy who are not candidates for further revascularization procedures and those preferred to delay invasive treatment. Several trials have demonstrated that EECP reduced angina symptom by CCS,7–9 improved quality of life,8–10 increased exercise capacity9–12 as well as enhanced the time to exercise-induced ST-segment depression11–13 and to improve myocardial perfusion.11,12 In 1 trial, the persistent reduction free of major adverse cardiovascular events (MACE) for up to 5 years treatment.14
Despite the greatest improvement in treatment modalities for CAD more than 40 years, the data from different observation trials cannot provide strong evidence to prove the effectiveness of EECP. The CCS class of angina severity, ranging form class I to class IV, was widely used in clinic to evaluate activity status and has been recognized as a significant predictor of long-term mortality.15 The meta-analysis was to assess the efficacy of EECP on CCS angina class in patients with chronic refractory angina.
METHODS
Search Strategy
We searched MEDLINE (source, PubMed, 1990 to March 2015), EMBASE (1990 to March 2015), the Cochrane Clinical Trials Register Database (though March 2015), and the ClinicalTrials. gov Website (though March 2015) using the terms “enhanced external counterpulsation,” “EECP,” and “external counter-pulsation.” No language restriction was performed. In addition, we manually searched the abstracts of annual scientific sessions that relevant to the subject. Potentially relevant articles were then screened by at least 2 independent reviewers; disagreements were resolved by discussion or upon consensus from the 3rd reviewer.
Inclusion and Exclusion Criteria
First, we conducted an initial screening of titles and/or abstracts. Second, reevaluation was performed on the basis of full-text review. The studies were included in our meta-analysis if they met the following criteria: the trial was a prospective design; the trial was conducted in patients with stable angina pectoris; the outcome interest was the adequate data on CCS angina class that reported before and after the 35 1-hour EECP sessions. Although meta-analysis of randomized controlled trials would provide more robust evidence, the feature of the EECP procedure makes it difficult, so the studies that we identified were prospectively planned studies. In order to avoid data duplication and artificial inflation such the sample size, we excluded studies from the International EECP Patient Registry (IEPR) and the EECP consortium. Data unpublished or published as case reports, case series, or abstracts were ruled out unless they met with the inclusion criteria mentioned. In addition, those studies reporting CCS in the form of mean baseline angina class before and after completion EECP treatment were also excluded.
Data Extraction
Data extraction was performed by 2 independent authors (CMZ and XJL) using a standardized data collection form. Disagreements between the reviewers were resolved through discussion or by the 3rd reviewer (XMW). For each study, the basic characteristics extracted included name of the first author, year of publication, location of the study, sampling size, study patient population, duration of patient follow-up, duration of EECP therapy, and adequate data on CCS.
Statistical Analysis
We used data from CCS class reported as the proportion of patients improving by at least 1 CCS angina class. Data were compared before and after EECP treatment. The impact of pooled proportion of EECP treatment was calculated using the Metaprop module in the R version 3.1.3 statistical software package. Proportion and 95%CI for outcome were separately calculated for each trial, and the proportion reported in each study was logit transformed prior to computing the pooled proportion.16,17 The selection of a Desimonian and Laird random-effect model versus Inverse of Variance fixed-effect model in the meta-analysis remains controversial. Tests of heterogeneity were applied to decide which method would be used to pool the results. Statistical heterogeneity was performed by I2 statistic (the percentage of total variation across studies that is due to heterogeneity rather than chance) and the Q statistic. When the I2 statistic was less than 50% and the P-value for the test of heterogeneity was ≧0.10, we used a fixed-effect model to compute the pooled total proportion, whereas the heterogeneity was considered statistical significance, and a random-effect model was addressed to compute the pooled total proportion.18
When heterogeneity was present, subgroup analyses were performed to explore potential reasons based on baseline CCS class and age at enrollment. In addition, to inspect differences in EECP therapy among differing patient demographic, we analyzed the studies that had at least 60% of patients having previously undergone percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) or having a previous myocardial infraction (MI). Moreover, the studies that had at least 30% of patients having diabetes mellitus (DM) were analyzed as well.
Sensitivity analysis was carried out to evaluate the influence of individual trials on the overall pooled results. Moreover, we excluded the studies that had large sample size to verify the robustness of the pooled proportion. To evaluate potential publication bias, funnel plots and the Begg rank correlation test and Egger linear regression test were used. P-value less than 0.10 level was considered significance.19
RESULTS
Search Results
We initially identified 762 potentially relevant articles. Seventy-one articles were considered to be of eligibility and were retrieved for full-test review. Fifty-three articles were excluded, and finally 18 studies20–37 reporting data on CCS class were included in our meta-analysis. A flow diagram of study selection is presented (Fig. 1).
FIGURE 1.
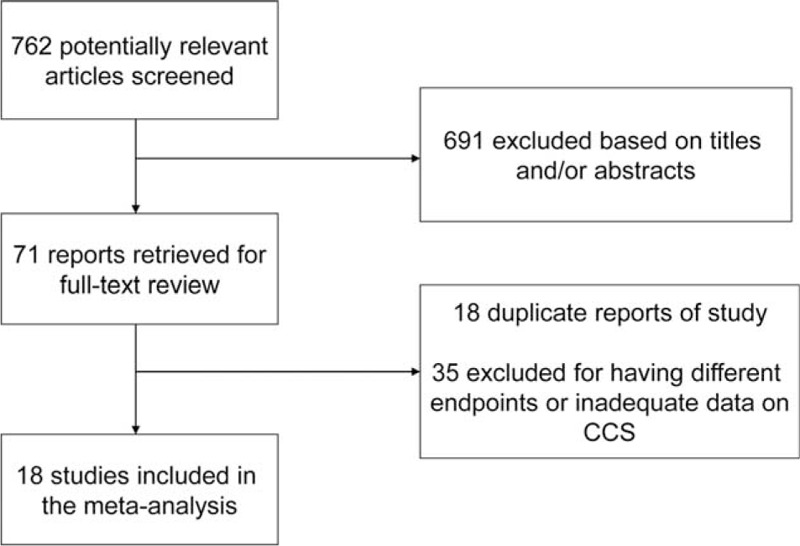
Flow diagram of study selection for meta-analysis.
Characteristics of Included Studies
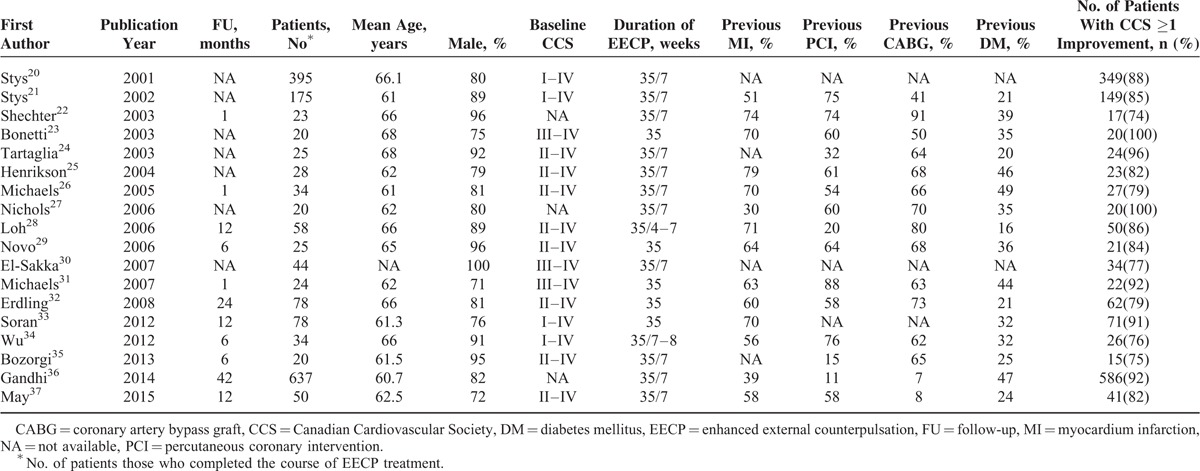
Baseline characteristics of the 18 studies with a total 1768 patients in this meta-analysis are shown in Table 1. The follow-up period varied from 1 to 42 months. The patient population were male predominately, and baseline CCS were I–IV, II–IV, and III–IV correspond to the 4,20,21,33,34 8,24–26,28,29,32,35,37 and 3 studies,23,30,31 respectively. The remaining studies on CCS were not reported.
TABLE 1.
Characteristics of Studies Included in the Meta-Analysis
Outcome Analysis
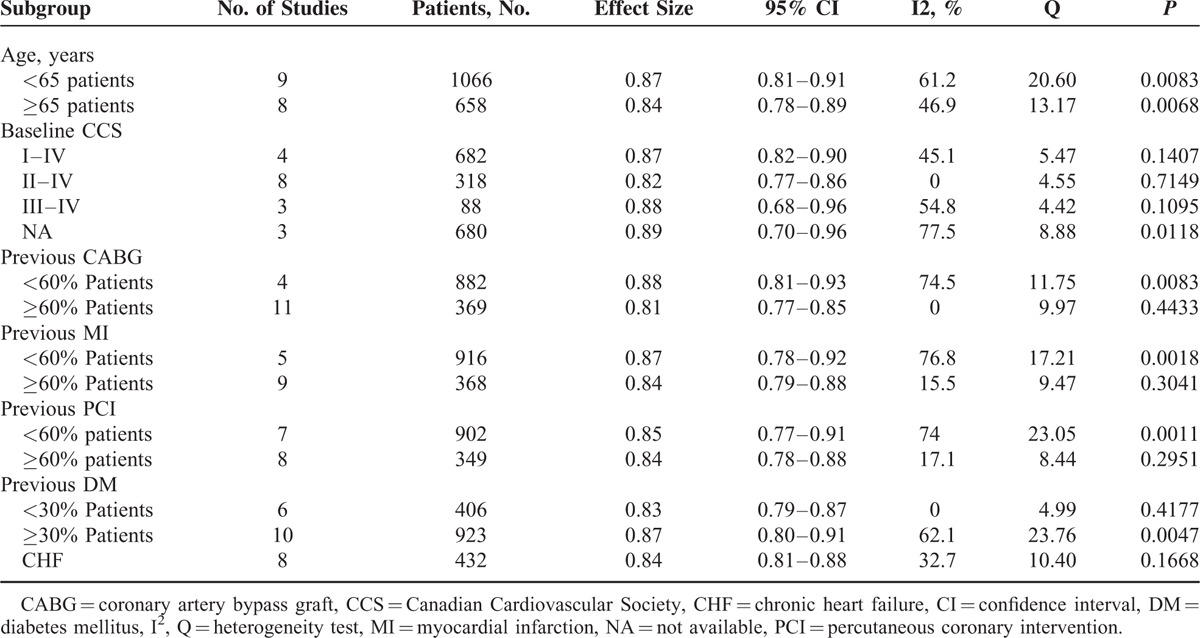
Our results suggested that angina class improved by at least 1 CCS class in 85% of patients from before to after EECP treatment (95% confidence interval [CI] 0.81–0.88, I2 = 58.5%, P < 0.001) (Fig. 2). The degree of benefit in studies enrolling patients with baseline CCS classes I–IV, II–IV, and III–IV were 87% (95%CI 0.82–0.90), 82% (95%CI 0.77–0.86), and 88% (95%CI 0.68–0.96), respectively (Table 2). The results of subgroup analysis by at least 60% enrollment patients were also shown in Table 2.
FIGURE 2.
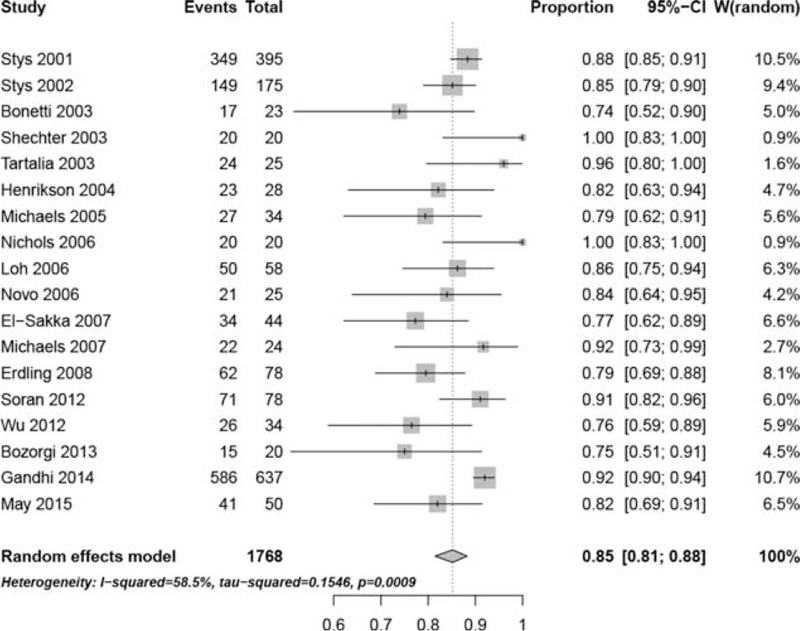
Forest plot of the overall pooled proportion and 95% confidence interval from 18 studies.
TABLE 2.
Subgroup Analysis
Sensitivity analysis was conducted to inspect the potential sources of heterogeneity. Exclusion of any single study did not remarkable alter the overall pooled proportion, with a range from 84% (95%CI 0.81–0.87, I2 = 30.6%) to 86% (95%CI 0.82–0.89, I2 = 56.5%) (Fig. 3).We excluded 3 large studies20,21,36 to compute the overall pooled proportion with a fixed effect model, the pooled proportion was 82% (95%CI 0.79–0.86, I2 = 18%, P = 0.2528) (Fig. 4).
FIGURE 3.
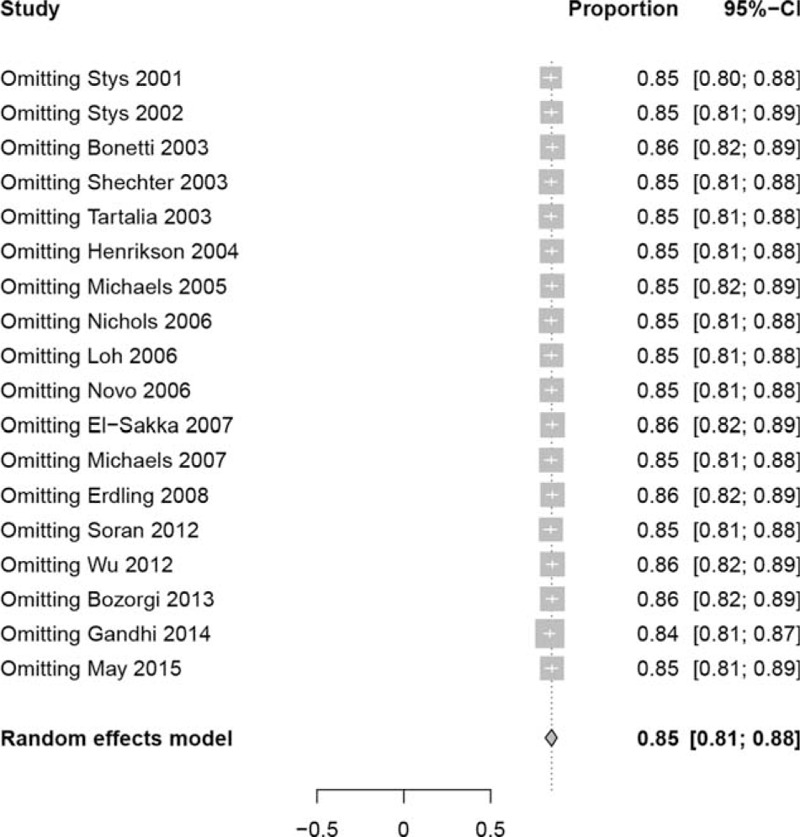
Sensitivity analysis of the efficacy of EECP therapy on CCS. CCS = Canadian Cardiovascular Society, EECP = enhanced external counterpulsation.
FIGURE 4.
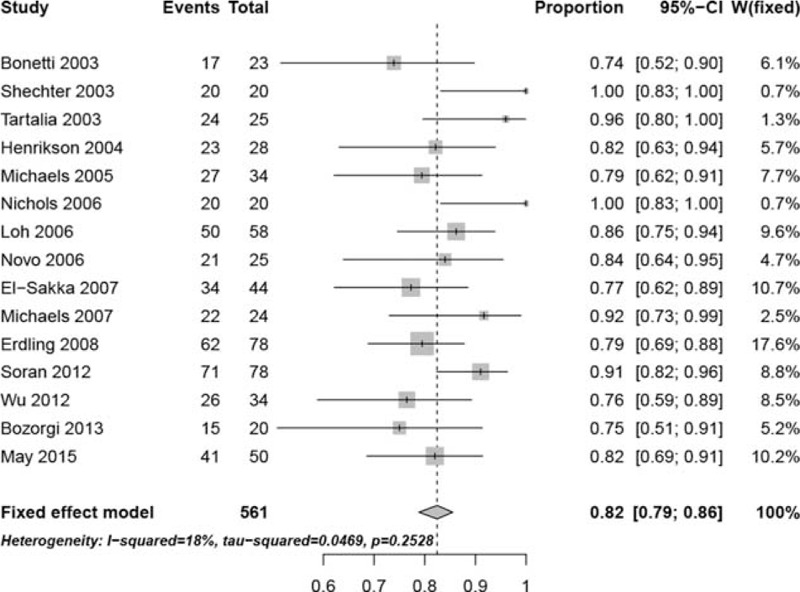
The meta-analysis of exclusion three large studies.
Publication Bias
To evaluate potential publication bias, funnel plot was drawn, and Begg rank correlation test as well as Egger linear regression test was conducted. Funnel plot (Fig. 5) showed some asymmetry, but the Begg rank correlation test and Egger linear regression test showed no publication bias (P = 0.1495 and 0.2859, respectively).
FIGURE 5.
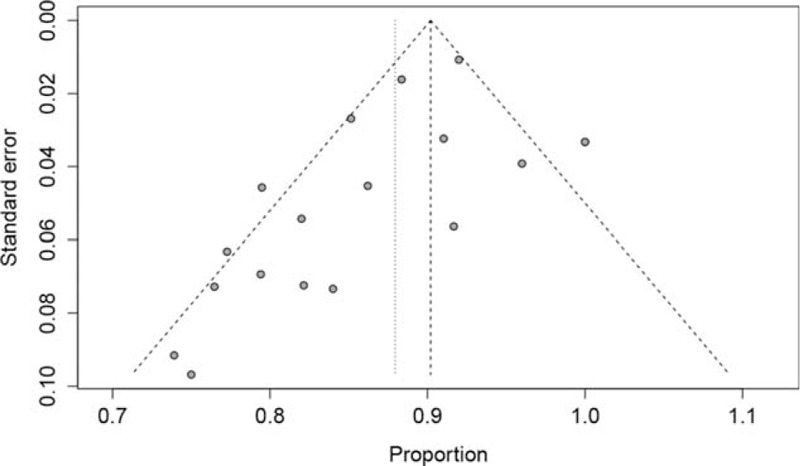
Funnel plot applied to evaluate publication bias.
DISCUSSION
The EECP therapy has been studied for almost a half century now. It is considered as a valuable, safe, and low-cost outpatient treatment for refractory angina. The technique of EECP consists of 3 pairs of pneumatic cuffs that were wrapped around the lower extremities, lower and upper thighs, and buttocks. The cuffs are inflated sequentially, applying 250 to 300 mmHg of external pressure during early of diastole, producing an improvement in coronary perfusion and thus increasing both venous return38 and cardiac output.39 On the onset of systole, the cuffs are then deflated reducing peripheral resistance and left ventricular afterload. A typically treatment sessions are 1 hour daily over 7 weeks for a total treatment course of 35 hours. A finger plethysmogram and electrocardiograph are utilized to monitor parameters.
Previous publication of EECP therapy on CCS class showed that 86% of 949 patients improved by at least 1 CCS functional class.40 In our meta-analysis, 85% of the patients undergoing EECP treatment had a reduction by at least 1 CCS class. The result was consistent with another report from an EECP consortium.41 In that study, an improvement was found in 74% of 2289 patients who were in CCS angina classes III–IV at baseline by one functional class. Nearly 40% of the patients in class III and IV improved 2 or more classes. It was to our interest that both men and women responded to the EECP treatment equally. It indicated that this treatment could be generalized to include women and advanced those who had chronic refractory angina. Because this population group were at increased complications and many had less durable results with CABG or angioplasty. The age may influence the effectiveness of patients to EECP treatment, so subgroup analysis based on age was performed in our meta-analysis. Compared with the elder group (≧65 years), patients younger than 65 years did not show a significant improvement on CCS class post-EECP (84 vs 87%). However, there was a trend that the younger benefited the most. One study41 suggested that the group of patients younger than 57 years derived greater likelihood of improvement from EECP. Indeed, elderly patients may have comorbid diseases, including DM, hypertension, and chronic heart failure (CHF), which decrease the ability to recruit and/or develop collaterals. Moreover, the possible explanations and conclusions need further studies to verify. Previous studies28,33,37 showed that about more than 70% of the patients retainted improvement in CCS after 1-year follow-up. Erdling et al32 and Michaels et al.7 reported a reduction by ≧1 angina class that sustained at 2 years. The later study suggested that 50% had an improvement in the quality-of-life post-EECP that was also lasted at 2 years. Besides the prior publication36 that the patients were followed up for 3.5 years indicated that about 66.4% sustained EECP treatment benefit. Even so, further studies were warranted to assess the long-term effects of EECP therapy.
Which group of patients did obtain utmost benefit from EECP treatment? Our results indicated that a greater degree of benefit in those having a higher baseline CCS class. In the International EECP Patient Registry (IEPR) examined the benefit and safety of EECP therapy in 978 patients with no exclusion criteria performed, approximately 85% of the patients treated were in CCS class III–IV with no candidate for further invasive revascularization and 81% of patients had a reduction by at least 1 CCS immediately after treatment with lower adverse effect.42 Lawson et al43 studied 112 patients with CCS II angina versus 1346 patients with class III–IV angina using data from IEPR. Compared with 78% of patients in CCS III–IV who had at least 1 CCS class improved post-treatment, the patients in class II was 61% (P < 0.01). At 2 years follow-up, MACE or repeat EECP treatment remained significantly, 70 versus 81%, respectively (P < 0.05). Although the greatest improvement was obtained in the patients most severely disabled at 2 years post-EECP, the patients who had mild angina benefited from EECP as well. The IEPR data were also used to examine the effect of EECP in 548 patients with a history of CHF.44 The heart failure cohort was older, with more females, a greater duration of CAD, more prior infarcts and revascularization. Compared with the cohort without a history of CHF, patients in the CHF cohort with CHF maintained their reduction in angina, but they were significantly more likely to have experienced an MACE end point at 6 months follow-up. In prior publication, EECP has increased maximal oxygen up-take and exercise tolerance in patients with CHF.45 Linnemeier et al46 reported effect of EECP in patients with DM. Despite a high-risk profile among the DM group than nondiabetes (ND), post-EECP angina reduction was reported on the CCS class in the majority of patients (DM vs ND, 69 vs 72%, P = NS). Quality of life was significantly improved and 1-year mortality was similar to coronary intervention.
To the best of our knowledge, no head-to-head prospective, randomized, controlled studies have been performed to compare the effect of elective invasive produces with EECP treatment on CCS class. One study compared patients enrolled in the IEPR with National Heart, Lung, and Blood Institute Dynamic Registry of patients who underwent elective PCI. After 1-year follow-up, the survival rate was similar in both cohorts.47 The data were come from 2 registries enrolling at primarily different centers, so presence of the potential bias was inevitable. In another report, 4454 of patients with prior PCI and/or CABG compared with 215 of patients who were suitable for PCI and/or CABG, but chose EECP as their initial revascularization treatment.48 After EECP treatment, improvements in CCS, anginal episodes, and nitroglycerin use were seen in 2 cohorts, which sustained 6 months.
The mechanism underlying the benefit of EECP-derived is under investigation. The possible mechanisms include improvement in endothelial function, development of collateralization, regression of atherosclerosis, and peripheral “training effects” similar to exercise.6 The acute hemodynamic effect produced shear stress which could lead to increased endothelial cell production of nitric oxide (NO) and prostacyclin, powerful factors of vasodilatation. The studies reported that the level of NO increased, brain natriuretic peptide and serum enthelin-1 concentration reduced after EECP treatment.12,49 Sessa et al50 found that chronic exercise promotes NO synthesis gene expression and coronary NO production in dog model. This process was initiated post-EECP with improved their exercise tolerance. Masuda et al12 showed an improvement in both resting and post-exercise perfusion. This may indirectly promote by opening preexist collaterals or developing new ones via increased transmyocardial pressure gradients during EECP.51,52
LIMITATIONS
Firstly, the aim of this meta-analysis was to assess the effect of immediately after EECP treatment. Therefore, the long-term maintenance of improved on CCS needs further investigation. Secondly, because the nature of EECP procedure makes performing a randomized, controlled, blinded trial difficult. We enrolled studies with the feature of prospective, nonrandomized-controlled. The first and an only multicenter, prospective, randomized, blinded placebo (sham) controlled trial was conducted in MUST-EECP.13 In addition, EECP, as a new treatment for refractory angina, attracted patients more enthusiasm, so the device placebo effect cannot be excluded. In generally, more further randomized controlled trails are necessary to assess the impact of EECP for the treatment of patients with chronic CAD.
CONCLUSIONS
Our meta-analysis suggested that 85% of the patients those underwent EECP therapy improved by at least 1 CCS class immediately post-EECP treatment. The CCS angina class is a relatively minor predictor of prognosis and freedom from events, so our results are noteworthy and the studies evaluated long-term benefit of EECP therapy are warranted. Currently, EECP treatment provides a safe, well-tolerated, valuable option for patients who were unresponsive to maximal medical management and/or invasive therapy. Of note, in combination with other antianginal drugs, the FDA approved Ranolazine to treatment for chronic angina in 2002.
Acknowledgments
The authors thank the National Natural Science Foundation of China (No. 81270175, No.81470404) and the Natural Science Foundation of Shandong Province, China (No.ZR2014HM107) for the support.
Footnotes
Abbreviations: CABG = coronary artery bypass graft, CAD = coronary artery disease, CCS = Canadian Cardiovascular Society, CHF = chronic heart failure, CI = confidence interval, DM = diabetes mellitus, EECP = enhanced external counterpulsation, MACE = major adverse cardiovascular events, NO = nitric oxide, PCI = percutaneous coronary intervention.
This work was supported by the National Natural Science Foundation of China (No. 81270175, No.81470404) and the Natural Science Foundation of Shandong Province, China (No.ZR2014HM107).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.McGillion M, Arthur HM, Cook A, et al. Management of patients with refractory angina: Canadian Cardiovascular Society/Canadian Pain Society Joint Guidelines. Can J Cardiol. England: 2012 Canadian Cardiovascular Society. Published by Elsevier Inc;2012:S20–S41. [DOI] [PubMed] [Google Scholar]
- 2.Mannheimer C, Camici P, Chester MR, et al. The problem of chronic refractory angina; report from the esc joint study group on the treatment of refractory angina. Eur heart J 2002; 355–370.England. [DOI] [PubMed] [Google Scholar]
- 3.Henry TD, Satran D, Jolicoeur EM. Treatment of refractory angina in patients not suitable for revascularization. Nat Rev Cardiol 2014; 11:78–95. [DOI] [PubMed] [Google Scholar]
- 4.Manchanda A, Aggarwal A, Aggarwal N, et al. Management of refractory angina pectoris. Cardiol J 2011; 18:343–351. [PubMed] [Google Scholar]
- 5.Montalescot G, Sechtem U, Achenbach S, et al. 2013 esc guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the european society of cardiology. Eur Heart J 2013; 34:2949–3003. [DOI] [PubMed] [Google Scholar]
- 6.Soran O. Treatment options for refractory angina pectoris: enhanced external counterpulsation therapy. Curr Treat Options Cardiovasc Med 2009; 11:54–60. [DOI] [PubMed] [Google Scholar]
- 7.Michaels AD, Linnemeier G, Soran O, et al. Two-year outcomes after enhanced external counterpulsation for stable angina pectoris (from the international eecp patient registry iepr). Am J Cardiol 2004; 93:461–464. [DOI] [PubMed] [Google Scholar]
- 8.Soran O, Kennard ED, Kfoury AG, et al. Two-year clinical outcomes after enhanced external counterpulsation (eecp) therapy in patients with refractory angina pectoris and left ventricular dysfunction (report from the international eecp patient registry). Am J Cardiol 2006; 97:17–20. [DOI] [PubMed] [Google Scholar]
- 9.Yavari M, Montazeri HR. Effects of enhanced external counterpulsation on anginal symptoms and improvements in objective measures of myocardial ischaemia. Cardiovasc J Afr 2007; 18:154–156. [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar A, Aronow WS, Vadnerkar A, et al. Effect of enhanced external counterpulsation on clinical symptoms, quality of life, 6-minute walking distance, and echocardiographic measurements of left ventricular systolic and diastolic function after 35 days of treatment and at 1-year follow up in 47 patients with chronic refractory angina pectoris. Am J Ther 2009; 16:116–118. [DOI] [PubMed] [Google Scholar]
- 11.Urano H, Ikeda H, Ueno T, et al. Enhanced external counterpulsation improves exercise tolerance, reduces exercise-induced myocardial ischemia and improves left ventricular diastolic filling in patients with coronary artery disease. J Am Coll Cardiol 2001; 93–99.United States. [DOI] [PubMed] [Google Scholar]
- 12.Masuda D, Nohara R, Hirai T, et al. Enhanced external counterpulsation improved myocardial perfusion and coronary flow reserve in patients with chronic stable angina-evaluation by n-13-ammonia positron emission tomography. Eur Heart J 2001; 22:1451–1458. [DOI] [PubMed] [Google Scholar]
- 13.Arora RR, Chou TM, Jain D, et al. The multicenter study of enhanced external counterpulsation (must-eecp): effect of eecp on exercise-induced myocardial ischemia and anginal episodes. J Am Coll Cardiol 1999; 33:1833–1840. [DOI] [PubMed] [Google Scholar]
- 14.Lawson WE, Hui JCK, Cohn PF. Long-term prognosis of patients with angina treated with enhanced external counterpulsation: five-year follow-up study. Clin Cardiol 2000; 23:254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaul P, Naylor CD, Armstrong PW, et al. Assessment of activity status and survival according to the canadian cardiovascular society angina classification. Can J Cardiol 2009; 25:E225–E231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wan Y, Hu Q, Li T, et al. Prevalence of autism spectrum disorders among children in china: a systematic review. Shanghai Arch Psychiatry 2013; 70–80.China. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luo M, Tan H, Zhou Q, et al. Implement meta-analysis of a single rate in the R software. J Evidence-Based Med 2013; 13:181–184.188 (in Chinese). [Google Scholar]
- 18.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. Br Med J 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stys T, Lawson WE, Hui JCK, et al. Acute hemodynamic effects and angina improvement with enhanced external counterpulsation. Angiology 2001; 52:653–658. [DOI] [PubMed] [Google Scholar]
- 21.Stys TP, Lawson WE, Hui JCK, et al. Effects of enhanced external counterpulsation on stress radionuclide coronary perfusion and exercise capacity in chronic stable angina pectoris. Am J Cardiol 2002; 89:822–824. [DOI] [PubMed] [Google Scholar]
- 22.Shechter M, Matetzky S, Feinberg MS, et al. External counterpulsation therapy improves endothelial function in patients with refractory angina pectoris. J Am Coll Cardiol 2003; 42:2090–2095. [DOI] [PubMed] [Google Scholar]
- 23.Bonetti PO, Barsness GW, Keelan PC, et al. Enhanced external counterpulsation improves endothelial function in patients with symptomatic coronary artery disease. J Am Coll Cardiol 2003; 41:1761–1768. [DOI] [PubMed] [Google Scholar]
- 24.Tartaglia J, Stenerson J, Charney R, et al. Exercise capability and myocardial perfusion in chronic angina patients treated with enhanced external counterpulsation. Clin Cardiol 2003; 26:287–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henrikson CA, Chandra-Strobos N. Enhanced external counterpulsation therapy: significant clinical improvement without electrophysiologic remodeling. Ann Noninvasive Electrocardiol 2004; 9:265–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Michaels AD, Raisinghani A, Soran O, et al. The effects of enhanced external counterpulsation on myocardial perfusion in patients with stable angina: a multicenter radionuclide study. Am Heart J 2005; 150:1066–1073. [DOI] [PubMed] [Google Scholar]
- 27.Nichols WW, Estrada JC, Braith RW, et al. Enhanced external counterpulsation treatment improves arterial wall properties and wave reflection characteristics in patients with refractory angina. J Am Coll Cardiol 2006; 48:1208–1214. [DOI] [PubMed] [Google Scholar]
- 28.Loh PH, Louis AA, Windram J, et al. The immediate and long-term outcome of enhanced external counterpulsation in treatment of chronic stable refractory angina. J Inter Med 2006; 259:276–284. [DOI] [PubMed] [Google Scholar]
- 29.Novo G, Bagger JP, Carta R, et al. Enhanced external counterpulsation for treatment of refractory angina pectoris. J Cardiovasc Med 2006; 7:335–339. [DOI] [PubMed] [Google Scholar]
- 30.El-Sakka AI, Morsy AM, Fagih BI. Enhanced external counterpulsation in patients with coronary artery disease-associated erectile dysfunction. Part ii: Impact of disease duration and treatment courses. J Sex Med 2007; 4:1448–1453. [DOI] [PubMed] [Google Scholar]
- 31.Michaels AD, Bart BA, Pinto T, et al. The effects of enhanced external counterpulsation on time- and frequency-domain measures of heart rate variability. J Electrocardiol 2007; 515–521.United States. [DOI] [PubMed] [Google Scholar]
- 32.Erdling A, Bondesson S, Pettersson T, et al. Enhanced external counter pulsation in treatment of refractory angina pectoris: two year outcome and baseline factors associated with treatment failure. BMC Cardiovasc Disord 2008; 8:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Soran O, Ikizler C, Sengul A, et al. Comparison of long term clinical outcomes, event free survival rates of patients undergoing enhanced external counterpulsation for coronary artery disease in the united states and turkey. Turk Kardiyol Dern Ars 2012; 40:323–330. [DOI] [PubMed] [Google Scholar]
- 34.Wu E, Martensson J, Brostrom A. Enhanced external counterpulsation in patients with refractory angina pectoris: a pilot study with six months follow-up regarding physical capacity and health-related quality of life. Eur J Cardiovasc Nurs 2013; 12:437–445. [DOI] [PubMed] [Google Scholar]
- 35.Bozorgi A, Mehrabi Nasab E, Sardari A, et al. Effect of enhanced external counterpulsation (eecp) on exercise time duration and functional capacity in patients with refractory angina pectoris. J Tehran Heart Cent 2014; 9:33–37. [PMC free article] [PubMed] [Google Scholar]
- 36.Gandhi P, Subramanian R, Mittal M. Primary utilization of eecp in chronic stable angina patients with left ventricular dysfunction and long time follow up. Global Heart 2014; 9:e194. [Google Scholar]
- 37.May O, Lynggaard V, Mortensen JCA, et al. Enhanced external counterpulsation – effect on angina pectoris, qol and exercise capacity after 1 year. Scand Cardiovasc J 2015; 49:1–6. [DOI] [PubMed] [Google Scholar]
- 38.Taguchi I, Ogawa K, Oida A, et al. Comparison of hemodynamic effects of enhanced external counterpulsation and intra-aortic balloon pumping in patients with acute myocardial infarction. Am J Cardiol 2000; 86:1139–1141. [DOI] [PubMed] [Google Scholar]
- 39.Bonetti PO, Holmes DR, Lerman A, et al. Enhanced external counterpulsation for ischemic heart disease – what's behind the curtain? J Am Coll Cardiol 2003; 41:1918–1925. [DOI] [PubMed] [Google Scholar]
- 40.Shah SA, Shapiro RJ, Mehta R, et al. Impact of enhanced external counterpulsation on canadian cardiovascular society angina class in patients with chronic stable angina: a meta-analysis. Pharmacotherapy 2010; 30:639–645. [DOI] [PubMed] [Google Scholar]
- 41.Lawson WE, Hui JCK, Lang G. Treatment benefit in the enhanced external counterpulsation consortium. Cardiology 2000; 94:31–35. [DOI] [PubMed] [Google Scholar]
- 42.Barsness G, Feldman AM, Holmes DR, et al. The international eecp patient registry (iepr): design, methods, baseline characteristics, and acute results. Clin Cardiol 2001; 24:435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lawson WE, Hui JCK, Kennard ED, et al. Two-year outcomes in patients with mild refractory angina treated with enhanced external counterpulsation. Clin Cardiol 2006; 29:69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lawson WE, Kennard ED, Holubkov R, et al. Benefit and safety of enhanced external counterpulsation in treating coronary artery disease patients with a history of congestive heart failure. Cardiology 2001; 96:78–84. [DOI] [PubMed] [Google Scholar]
- 45.Soran O, Fleishman B, Demarco T, et al. Enhanced external counterpulsation in patients with heart failure: a multicenter feasibility study. Congest Heart Fail (Greenwich, Conn) 2002; 8:204–227. [DOI] [PubMed] [Google Scholar]
- 46.Linnemeier G, Rutter MK, Barsness G, et al. Enhanced external counterpulsation for the relief of angina in patients with diabetes: safety, efficacy and 1-year clinical outcomes. Am Heart J 2003; 146:453–458. [DOI] [PubMed] [Google Scholar]
- 47.Holubkov R, Kennard ED, Foris JM, et al. Comparison of patients undergoing enhanced external counterpulsation and percutaneous coronary intervention for stable angina pectoris. Am J Cardiol 2002; 89:1182–1186. [DOI] [PubMed] [Google Scholar]
- 48.Fitzgerald CP, Lawson WE, Hui JC, et al. Enhanced external counterpulsation as initial revascularization treatment for angina refractory to medical therapy. Cardiology 2003; 129–135.Switzerland. [DOI] [PubMed] [Google Scholar]
- 49.Akhtar M, Wu G-F, Du Z-M, et al. Effect of external counterpulsation on plasma nitric oxide and endothelin-1 levels. Am J Cardiol 2006; 98:28–30. [DOI] [PubMed] [Google Scholar]
- 50.Sessa WC, Pritchard K, Seyedi N, et al. Chronic exercise in dogs increases coronary vascular nitric oxide production and endothelial cell nitric oxide synthase gene expression. Circ Res 1994; 74:349–353. [DOI] [PubMed] [Google Scholar]
- 51.Flynn MS, Kern MJ, Donohue TJ, et al. Alterations of coronary collateral blood flow velocity during intraaortic balloon pumping. Am J Cardiol 1993; 71:1451–1455. [DOI] [PubMed] [Google Scholar]
- 52.Kern MJ, Aguirre FV, Tatineni S, et al. Enhanced coronary blood flow velocity during intraaortic balloon counterpulsation in critically ill patients. J Am Coll Cardiol 1993; 21:359–368. [DOI] [PubMed] [Google Scholar]


