Abstract
Bone grafting is a commonly used orthopedic surgical procedure that will provide bone formation in bone defects or regions of defective bone healing. A major complication following bone grafting is a postoperative recipient graft site infection that is associated with substantial mortality and increased use of medical resources. The purpose of the study was to identify the risk factors associated with infection after bone-grafting surgery.
Data from 1,303,347 patients listed in the Taiwan National Health Insurance Research Database (NHIRD) and admitted to hospitals from 1997 through 2012 who underwent primary bone grafting (mean age: 46.57 years old; mean length of hospital stay: 8.04 days) were analyzed. The incidence of infection by age, hospital stay, gender, income, chronic disease (tuberculosis [TB]; diabetes mellitus [DM]; acquired immunodeficiency syndrome [AIDS]), fracture complications (nonunion; delayed union fracture), types of graft and hospital was evaluated.
Three percent of the patients developed a postoperative recipient graft site infection. Multivariable analysis revealed that patients were more likely to develop a post bone-grafting surgery infection if they were older, had a longer hospital stay, were male, had a lower income, or had comorbid TB, DM, or AIDS. Patients were more likely to develop an infection if they had a nonunion, an alloplast graft, or treated in a local clinic.
Our findings should provide a clinically relevant reference for surgeons who perform bone grafting. Patients should be informed of the potential risks.
INTRODUCTION
Bone grafting is common in neurosurgery for spinal fusion and in orthopedic reconstruction surgery for revision hip replacement, repairing skeletal defects after a trauma, and for support when removing a tumor. Three types of bone graft are used: autograft (autologous graft), allograft, and alloplastic graft. An autograft is usually harvested from the patient's own iliac crest. An allograft is taken from a donor or cadaver.1,2 An alloplastic graft is a synthetic substitute, usually created from ceramics (calcium phosphate, calcium sulfate, or bioactive glass), polymer (derivative from acrylate), or growth factors (the family of bone morphogenetic proteins).3 Intraoperative complications might occur and affect subsequent tissue healing, motor function recovery, and the surgical outcome. Thus, bone grafting poses a significant health risk to the patient.
Approximately 500,000 surgical site infections caused by bacteria and viruses occur every year in the United States.4 Postoperative transmission of an infection can be devastating to the graft and the patient: it may lead to serious illness and even death.5 Patients with a preexisting illness are at a higher risk for an infection than are those who are otherwise healthy. Delayed union and nonunion fracture are two of the most common complications after orthopedic surgery, and both require additional reconstruction using bone grafts.6,7 Moreover, after bone surgery, patients with an immunocompromised disease, like diabetes mellitus (DM), have a greater risk of infection.8,9 Two other increasing chronic infectious diseases in Asia, tuberculosis (TB) and acquired immunodeficiency syndrome (AIDS), may compromise the immunity of patients and relate to the incidence of bone infection. Treating deep infection requires long-term antibiotic use and repetitive irrigation and debridement. Alternatively, a skin graft or flap might be required to improve the outcome after infection. For most patients, removing the graft might be the only way to fix the problem, because the fresh tissue may be the source or a nidus for infection recurrence. Nevertheless, there is no prior study that examines the risk factors of infection after bone-grafting surgery.
We examined the risk factors of infection in patients that underwent bone grafting in Taiwan. Data were collected from the Taiwan National Health Insurance Research Database (NHIRD) (http://nhird.nhri.org.tw/en/Background.html) and analyzed for all patients who were admitted to hospitals from 1997 through 2012 for primary bone-grafting treatment. The incidence of recipient graft site infection in patients who underwent bone grafting, and the risk factors associated with postoperative infection, were evaluated. This is the first large national database study of the factors associated with bone-grafting surgery.
METHODS
Data Source
Approximately 98% of Taiwan's population (ca. 23 million) participate in the National Health Insurance program (http://www.nhi.gov.tw/English/Index.aspx?menu=13&menu_id=486&WD_ID=486). The Taiwan NHIRD, which uses the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes,10 covers all inpatient medical claims data for enrolled residents. The established categories of expenditure were provided in inpatient expenditure by admission (DD files) (http://nhird.nhri.org.tw/date_01.html). The personal information of all patients was encrypted with a double scrambling protocol for research purposes to protect patient privacy. This study was approved by the Institutional Review Board of Jianan Psychiatric Center, and the protocol was evaluated by the National Health Research Institutes (NHRI), which consented to this planned analysis of the NHIRD (Agreement Number: NHIRD-103–161).
Study Design
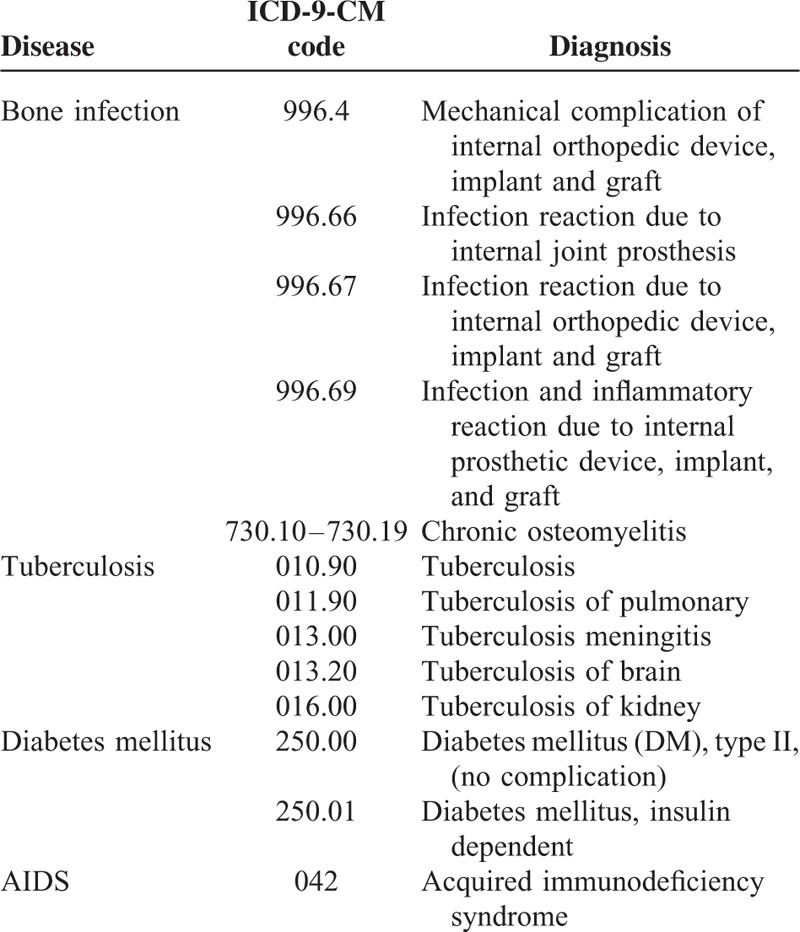
A population-based retrospective cohort study was conducted. We analyzed 1,303,347 NHIRD-registered cases of bone grafting between 1997 and 2012. The participant demographic characteristics, including age, gender, hospital stay, and low-income households, were identified at the index date. The risk factors included in this study were those that have been found to be associated with or possibly related to the development of bone infection. A diagnosis of bone infection was defined on the basis of deep infection after surgery (excluding superficial infection) as prescribed by the National Health Insurance system (ICD 9 codes 996.4, 996.66, 996.67, 996.69, and 730.10–730.19; Table 1). Data regarding deep infection-related surgeries (ICD 9 codes 77.1–77.9, 79.3, and 86.22) were collected. The preexisting comorbidities include DM, TB, and AIDS. They were identified from data of the NHIRD based mainly on ICD-9-CM diagnostic codes (Table 1). The diagnosis in this study were judged and determined by related specialists and physicians according to the standard criteria. The minimum living expense standard was defined as 60% of the average monthly disposable income for each region. Low-income households were defined as those with a monthly average per-member gross income of less than the monthly minimum living expense standard in the household's residence region. The ICD-9-CM procedure code used for alloplasts and allografts were the same (79.3); thus, grafts were grouped into three categories: alloplast/allograft, autograft, and combined (autograft plus alloplast/allograft). Union was defined based on combined clinical and radiographic criteria. The criterion for a nonunion fracture was an unhealed broken bone 9-month postfracture that had shown no healing progression between the affected ends of the bone for 3 months after any specific treatment.11 A fracture that failed to heal within the normal time for that fracture type and location was defined as a delayed union fracture. According to the chapter II, laws of medical care act, Ministry of Health and Welfare in Taiwan (http://law.moj.gov.tw/Eng/LawClass/LawContent.aspx?PCODE=L0020021), medical care institutions with wards for the inpatient care of patients shall be referred to as hospitals; those with only out-patient facilities shall be referred to as clinics. Clinics referred may set up no more than 9 beds for observation. In Taiwan, local clinics are set up with different specificities. Therefore, the data regarding to patients with bone infection can be collected from those local clinics specialized in orthopedics, general trauma, rehabilitation, infectious disease, etc.
TABLE 1.
Disease Definition and Diagnostic Codes
Statistical Analysis
SPSS 18.0 for Windows (SPSS Inc., Chicago, Illinois) was used for all statistical analyses. Descriptive statistics were analyzed for all variables using frequency, percentage, mean, and standard deviation (SD). Bivariate analyses were used to determine appropriate variables to include in the multivariate models. Only variables that were significantly associated with bone infection (P < 0.05) were entered simultaneously into multivariate logistic regression models. The effects of outcome variables were measured using the adjusted odds ratio (AOR) with a 95% confidence interval (CI). The statistical analysis has been examined by the epidemiologist, Dr. C.Y. Li, who is also one of the authors of this article.
RESULTS
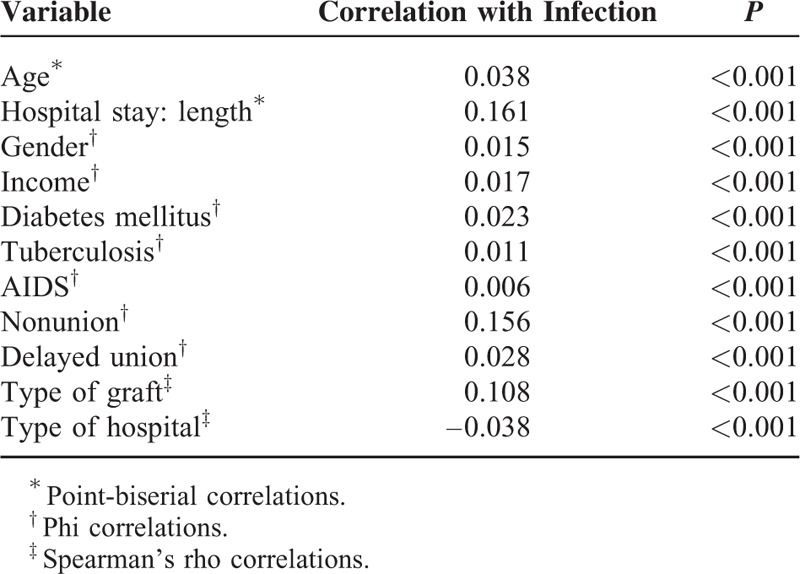
We enrolled 1,303,347 cases (mean age: 46.57 ± 22.16 years old; mean length of hospital stay: 8.04 ± 7.73 days; male: 58.4%; low income: 1.3%) (Table 2). The infection rate after bone graft surgery was 3.05%. The infection rate of male and female was 3.3 and 2.7%, respectively. Comorbid diseases included DM (83,416), TB (1,353), and AIDS (19). The infection rate of bone-grafting cases with DM, TB, and AIDS was 4.6, 6.6, and 31.6%, respectively. Nonunion (40,199) was more frequent than delayed union (13,673). Most (1,201,359) of the grafts were alloplasts or allografts. More patients went to district hospitals (485,171) and regional hospitals (453,723) for surgery (Table 2). All variables but “Previous Bone Graft Surgery” were significantly correlated with surgical site infection after bone grafting (Table 3).
TABLE 2.
Characteristics of Patients Who Underwent a Bone Graft
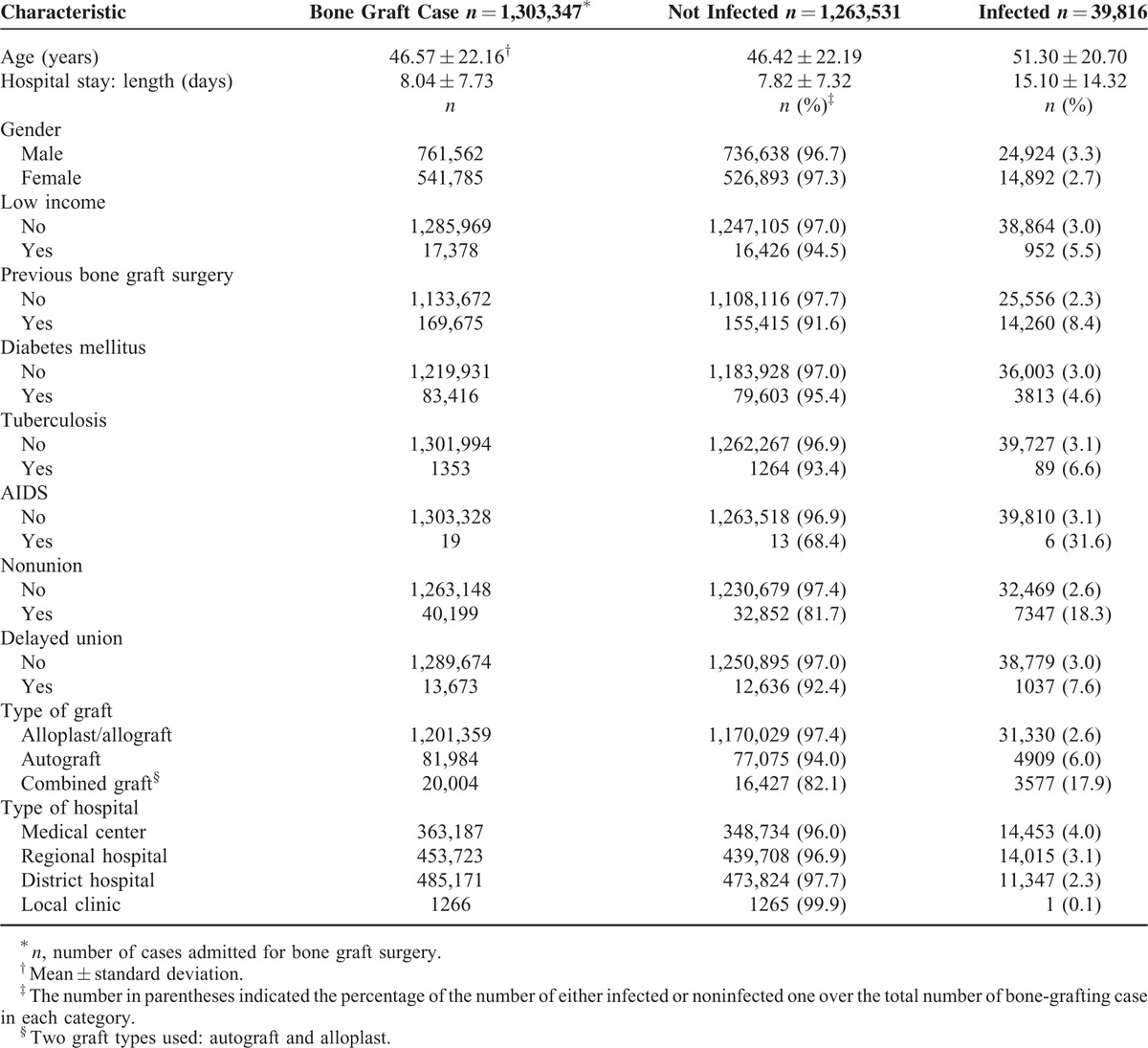
TABLE 3.
Bivariate Associations Between Variables and Bone Infection
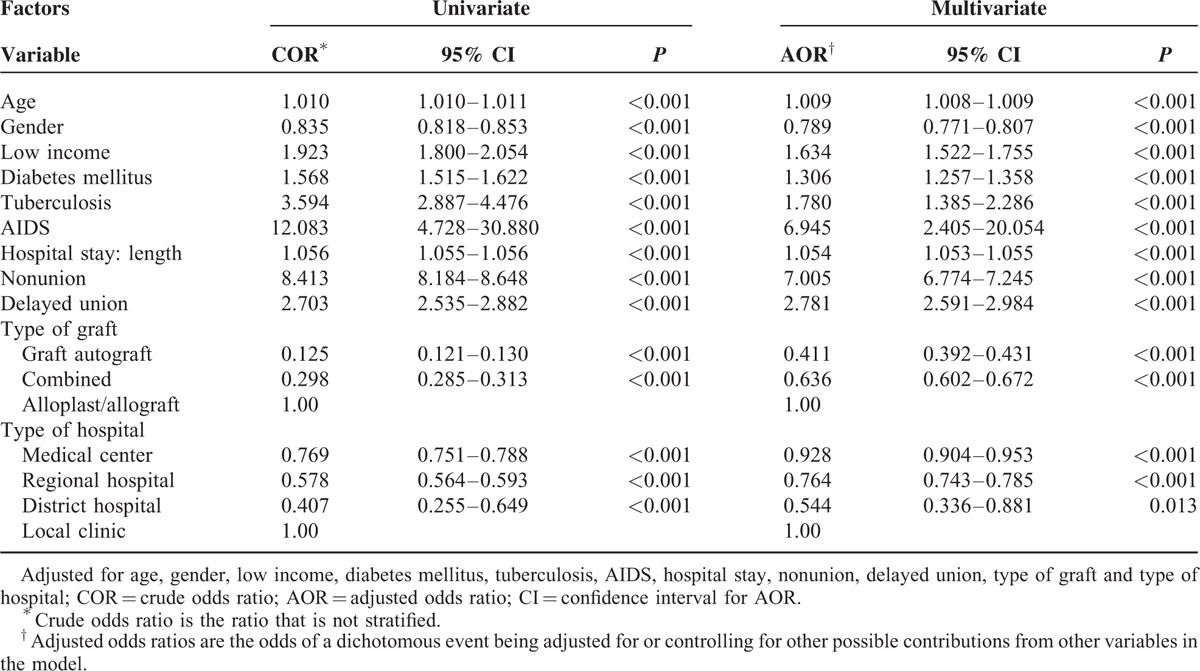
Univariate and multivariate analyses both showed that the likelihood of postoperative infection was significantly positively dependent upon the patient-related factors of age, gender, income, and comorbid diseases (Table 4). Patients more easily developed surgical site infections if they were older, were male, had a lower income, and had comorbid diseases. Patients with comorbid AIDS had the highest odds of infection (AOR = 6.945, 95% CI = 2.405–20.054, P < 0.001). Univariate and multivariate analyses also showed that the likelihood of postoperative infection was significantly dependent upon the surgery-related factors of hospital stay length and fracture, graft, and hospital type. Patients with a history of nonunion have relatively high odds of developing a surgical site infection (AOR = 7.005, 95% CI = 6.774–7.245, P < 0.001); our data also indicated that patients who underwent an autograft were the least likely to develop a postoperative infection. The AOR of patients who had their bone grafts done in medical centers was 0.928 compared with those who had them done in local clinics (95% CI = 0.904–0.953, P < 0.001). The AOR of patients who had their bone grafts done in regional hospitals was 0.764 compared with those who had them done in local clinics (95% CI = 0.743–0.785, P < 0.001). The AOR of patients who had their bone grafts done in district hospitals was 0.544 compared with those who had them done in local clinics (95% CI = 0.336–0.881, P = 0.013). The relative risk factor of surgical site infection was the highest for bone grafts done in local clinics, followed by those done in medical centers, regional hospitals, and district hospitals. To our surprise, the odds of infection in the medical centers were the second highest.
TABLE 4.
Factors Associated with Infection After a Bone Graft
DISCUSSION
In this study, we evaluated various risk factors of surgical site infection in patients who undergo bone grafting. Among the 1,303,347 cases that had undergone a bone-grafting operation, 39,816 cases developed a postoperative infection. The infection rate was 3.05%, lower than the 5.4% allograft infection rate in 128 patients reported by Delloye et al.12 Our infection rate was also lower than the 7.8% rate in 140 patients after cranioplasty.13 Our infection rate might be lower because our patients were recruited from the general population and because we did not restrict enrollment based on the surgery site or the graft materials used.
Surprisingly, except for local clinics, the smallest units where the AOR was highest, the second highest one was in the medical centers, the largest units, followed by the regional hospitals and district hospitals. The commonsense and intuitive order should have been local, district, and regional hospitals, and then medical centers, that is, the smallest rate of infection should have been at the largest unit. This paradoxical finding might be explained by a national study14 of nosocomial infection, which found that the infection rate was highest in medical centers (0.42%) followed by regional hospitals (0.34%). It may also explain why staying 1 extra day in a hospitals increased by 1.054 times the odds of developing a surgical site infection. Patients given an autograft were less likely to develop an infection than those who were given a combined graft or an alloplast/allograft. Similar results were reported in a study on anterior cruciate ligament reconstruction:9 bone-tendon-bone autografts were associated with a lower risk of postoperative infection than were allografts and combined grafts. The principles involved in successful bone grafts include osteoconduction (guiding the reparative growth of the natural bone), osteoinduction (encouraging undifferentiated cells to become active osteoblasts), and osteogenesis (living bone cells in the graft material contribute to bone remodeling).15 Osteogenesis occurs only when using autografts; therefore, using an autograft is preferable. However, an autograft might lead to complications such as pain, infection, scarring, and blood loss, as well as a variable quantity of bone to harvest from each patient. The alternative is an allograft, but that lacks osteoactive capacity and risks carrying infectious agents or leading to an immune rejection. Other approaches have used alloplasts, which are various types of organic and synthetic substitutes for bone, and they have focused on improving the efficacy of bone grafts or other scaffolds by incorporating bone progenitor cells and growth factors to stimulate cell proliferation. Based on our study, in addition to using an autograft alone, the combined use of an alloplast with an autograft might help reduce infection. We collected data without exclusion of prior infection history. Although the bone grafting was performed when no sign of infection or the infection was totally under control in surgical sites, an exclusion of these patients with prior infection would underestimate the infection rate. The debridement of wound infection would not be considered to use bone grafts. However, in rare cases, when repetitively deep infection occurred, a vascular bone graft might be applied from the donor site of patients for bone grafting. In that case, this type of bone graft belonged to autograft that was the least likely to develop a postoperative infection compared to the other two groups in our study. Nevertheless, preexisting complications can increase the risk of infection; for example, a nonunion increases it 7.005 times and a delayed union increases it 2.781 times after bone grafting. Both of these remain major complications after skeletal trauma. Careful attention is required when doing a bone graft, particularly in patients with these histories.
Our study indicated that patients 1 year older were 1.009 times more likely to develop a postoperative infection than patients 1 year younger. Moreover, patients with comorbid chronic or infectious diseases were more likely to develop an infection. DM is a recognized important risk factor for a variety of intracellular bacterial infections. Oxidative stress in the tissue of patients with DM reduces the phagocytic and antibacterial activity of neutrophils and macrophages and provides an intracellular niche for the pathogen to replicate.16 Immunosuppression makes it easier for patients to become infected. It should not, therefore, be surprising that patients with comorbid AIDS are 6.945 times more likely to become infected after bone-grafting surgery. Notably, patients with comorbid TB, another infectious disease with a rapidly rising incidence worldwide, are 1.780 times more likely to become infected than those without TB. CD4+ T cells are protective against Mycobacterium tuberculosis: CD4+ T cell depletion is responsible for the increased susceptibility to develop active M tuberculosis in HIV-infected patients.17 Although the role of CD8+ T cells in TB is less clear than the role of CD4+ T cells, they are generally considered to contribute to optimal immunity and protection.18 These results suggested that compromised immunity because of aging and comorbid disease are determining risk factors of bone-graft infection. Compromised immunity contributes to the double burden of chronic disease and surgical site infection. How other noninfectious comorbid diseases were involved in bone-graft infection required for further investigation. We also found that low-income earners were 1.634 times more likely compared with higher income earners to develop an infection. Consistent with this risk factor for other bone surgery,19,20 economic stress might physically and psychologically make patients less aware of the state of their individual health.
The National Health Insurance Bureau has established a uniform system to control the quality of medical services, and the quality of the coded data in the present study was reliable.21,22 Compared with self-reported surveys, the methodology used in this study reduced the patients’ recall bias and thereby increased its accuracy. Nevertheless, the NHIRD provides only insurance-related data; information such as education level and marital status are not provided. Second, the limited data acquired made it difficult to explain the different infection rate between males and females. Suzuki et al. identified that several risk factors were associated with infection after total knee arthroplasty surgery, including previous history of open reduction internal fixation, remnants of prior internal fixation material, and male gender.23 Male gender was significantly correlated with postoperative infection. This is probably why the mortality rate was higher for male patients orthopedic and trauma admissions.24 Compliance with the doctor's prescribed medication regimen may be different between men and women.
In conclusion, we surveyed the epidemiology of surgical site infection in patients who had undergone bone grafting in Taiwan between 1997 and 2012. Our findings revealed the risk factors of a postoperative bone graft infection. They consists of the patient-related factors like age, income, gender, and chronic diseases, and the surgery-related factors like the length of hospital stay, disease complications, type of graft used, and type of hospital in which the surgery was done. As the frequency of using different types of bone grafts for orthopedic reconstructive surgery increase, our findings should provide an understanding of the risk factors associated with infection and should be a valuable reference for orthopedic surgeons.
Footnotes
Abbreviations: AIDS = acquired immunodeficiency syndrome, AOR = adjusted odds ratio, CI = confidence interval, COR = crude odds ratio, DM = diabetes mellitus, ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification, NHIRD = National Health Insurance Research Database, NHRI = National Health Research Institutes, SD = standard deviation, TB = tuberculosis.
This study is based in part on data from the NHIRD provided by the National Health Insurance Administration, Ministry of Health and Welfare and managed by National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of National Health Insurance Administration, Ministry of Health and Welfare or National Health Research Institutes. This work was supported by grants from the National Science Council (NSC 102–2314-B-273 -002 -MY3), Taiwan.
F-HL and P-CS contributed equally to this article.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Stevenson S. Biology of bone grafts. Orthop Clin North Am 1999; 30:543–552. [DOI] [PubMed] [Google Scholar]
- 2.Garbuz DS, Masri BA, Czitrom AA. Biology of allografting. Orthop Clin North Am 1998; 29:199–204. [DOI] [PubMed] [Google Scholar]
- 3.Damien CJ, Parsons JR. Bone graft and bone graft substitutes: a review of current technology and applications. J Appl Biomater 1991; 2:187–208. [DOI] [PubMed] [Google Scholar]
- 4.Perencevich EN, Sands KE, Cosgrove SE, et al. Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis 2003; 9:196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Update: allograft-associated bacterial infections–United States, 2002. MMWR Morb Mortal Wkly Rep 2002; 51:207–210. [PubMed] [Google Scholar]
- 6.Lash NJ, Feller JA, Batty LM, et al. Bone grafts and bone substitutes for opening-wedge osteotomies of the knee: a systematic review. Arthroscopy 2015; 31:720–730. [DOI] [PubMed] [Google Scholar]
- 7.Bus MP, Dijkstra PD, van de Sande MA, et al. Intercalary allograft reconstructions following resection of primary bone tumors: a nationwide multicenter study. J Bone Joint Surg Am 2014; 96:e26. [DOI] [PubMed] [Google Scholar]
- 8.Wukich DK, Lowery NJ, McMillen RL, et al. Postoperative infection rates in foot and ankle surgery: a comparison of patients with and without diabetes mellitus. J Bone Joint Surg Am 2010; 92:287–295. [DOI] [PubMed] [Google Scholar]
- 9.Brophy RH, Wright RW, Huston LJ, et al. Factors associated with infection following anterior cruciate ligament reconstruction. J Bone Joint Surg Am 2015; 97:450–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lovaasen KR, Schwerdtfeger J. ICD-9-CM Coding: Theory and Practice. Philadelphia: WB Saunders; 2007. [Google Scholar]
- 11.Einhorn TA. Enhancement of fracture-healing. J Bone Joint Surg Am 1995; 77:940–956. [DOI] [PubMed] [Google Scholar]
- 12.Delloye C, van Cauter M, Dufrane D, et al. Local complications of massive bone allografts: an appraisal of their prevalence in 128 patients. Acta Orthop Belg 2014; 80:196–204. [PubMed] [Google Scholar]
- 13.Lee CH, Chung YS, Lee SH, et al. Analysis of the factors influencing bone graft infection after cranioplasty. J Trauma Acute Care Surg 2012; 73:255–260. [DOI] [PubMed] [Google Scholar]
- 14.Chang SC, Tsai CL, Wang JT, et al. Nosocomial infections in medical centers and regional hospitals between 1999 and 2002 in Taiwan (in Chinese). Infect Control J 2004; 14:1–11. [Google Scholar]
- 15.Samartzis D, Shen FH, Goldberg EJ, et al. Is autograft the gold standard in achieving radiographic fusion in one-level anterior cervical discectomy and fusion with rigid anterior plate fixation? Spine 2005; 30:1756–1761. [DOI] [PubMed] [Google Scholar]
- 16.Hodgson K, Morris J, Bridson T, et al. Immunological mechanisms contributing to the double burden of diabetes and intracellular bacterial infections. Immunology 2015; 144:171–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geldmacher C, Zumla A, Hoelscher M. Interaction between HIV and Mycobacterium tuberculosis: HIV-1-induced CD4 T-cell depletion and the development of active tuberculosis. Curr Opin HIV AIDS 2012; 7:268–275. [DOI] [PubMed] [Google Scholar]
- 18.Brighenti S, Andersson J. Induction and regulation of CD8+ cytolytic T cells in human tuberculosis and HIV infection. Biochem Biophys Res Commun 2010; 396:50–57. [DOI] [PubMed] [Google Scholar]
- 19.Mahomed NN, Barrett JA, Katz JN, et al. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am 2003; 85-A:27–32. [DOI] [PubMed] [Google Scholar]
- 20.Petrigliano FA, Bezrukov N, Gamradt SC, et al. Factors predicting complication and reoperation rates following surgical fixation of proximal humeral fractures. Bone Joint Surg Am 2014; 96:1544–1551. [DOI] [PubMed] [Google Scholar]
- 21.Yang NP, Chan CL, Yu IL, et al. Estimated prevalence of orthopaedic fractures in Taiwan: a cross-sectional study based on nationwide insurance data. Injury 2010; 41:1266–1272. [DOI] [PubMed] [Google Scholar]
- 22.Yang NP, Chen HC, Phan DV, et al. Epidemiological survey of orthopedic joint dislocations based on nationwide insurance data in Taiwan, 2000-2005. BMC Muscoskel Disord 2011; 12:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suzuki G, Saito S, Ishii T, et al. Previous fracture surgery is a major risk factor of infection after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2011; 19:2040–2044. [DOI] [PubMed] [Google Scholar]
- 24.Orimolade EA, Akinyoola AL, Ikem IC, et al. Mortality among orthopaedic and traumatology admissions: a ten year review. East Afr J Public Health 2010; 7:361–366. [DOI] [PubMed] [Google Scholar]


