Abstract
The aim of this study is to report our 39 patients treated with anterior debridement and autologous iliac bone grafting with or without anterior instrumentation, which is the presumed treatment of choice for thoracic or lumbar spondylodiscitis.
Our patients underwent surgical treatment of spondylodiscitis using anterior debridement and autologous iliac bone grafting with or without anterior instrumentation and were analyzed with a mean follow-up of 8 years (range, 2–11 years). Kaneda 2-rod system instrumentation was used in 12 patients, in total. Clinical outcomes were assessed by the Frankel grade. Radiographic fusion was characterized based on 3-dimensional computed tomography.
Of the whole group, 20 patients suffered from tuberculous spondylodiscitis and 19 suffered from hematogenous spondylodiscitis. Pathogens responsible for pyogenic infection included Staphylococcus aureus (4 patients), Pseudomonas aeruginosa (3 patients), and Brucella melitensis (1 patient). Fifteen patients had thoracic involvement, 20 had lumbar involvement, and 4 had thoracolumbar junction involvement. Preoperative neurological deficits were noted in 13 of the 39 patients. In terms of Frankel grade, 8 patients have improved, 4 have remained the same, and 1 patient has worsened during the follow-up period. Imaging-documented fusion was achieved in 23 of 27 patients in the graft group (85% fusion rate) and 11 of 12 patients in the graft + Kaneda instrumentation group (91% fusion rate).
There was no instrumentation failure, loosening, or graft-related complication such as slippage or fracture of the graft. This approach demonstrated a good recovery rate of neurological functions and a high fusion rate.
INTRODUCTION
Spondylodiscitis is a devastating disease and it is associated with significant morbidity and mortality. There is still a high incidence of spondylodiscitis, especially in developing countries where involvement of the spine is more frequent than other skeletal sites.1
The purpose of this study is to report our experience with anterior debridement and autologous iliac bone grafting with or without anterior instrumentation, which is the presumed treatment of choice for spondylodiscitis, in a consecutive series of 39 patients with thoracic or lumbar spondylodiscitis, and to compare the clinical and imaging outcomes.
PATIENTS AND METHODS
From January 1998 to August 2008, analysis retrospectively included 39 patients affected by tuberculous or pyogenic spondylodiscitis of the thoracic or lumbar spine underwent anterior surgical treatment at İzmir Atatürk Research and Training Hospital. Because of the retrospective nature of the study, an ethical statement was not required. Previous spinal surgery and penetrating trauma to the vertebrae were excluded in this study. The study included only the patients with spontaneous spondylodiscitis. Demographic pattern, predisposing conditions, clinical presentation, co-morbidities, microbiology, type of surgery, clinical and radiological outcomes of the 39 patients were retrospectively reviewed. The mean follow-up period for the study group was 8 years (range, 2–11 years).
Patients with neurological deficits were graded according to Frankel's scale.2 Severe deficits were classified as complete (Frankel grade A) or incomplete (Frankel grades B and C). Paraparesis was defined as a Frankel grade D deficit. Frankel grade E was no motor or sensory deficit (Table 1).
TABLE 1.
Classification Neurological Lesions According to Frankel et al2

Each patient's white blood cell count (WBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were measured.
All patients were evaluated with plain radiographs, computed tomography (CT), and magnetic resonance imaging (MRI).
Surgical indications included failure of medical treatment (nonsignificant decrease of sedimentation and CRP, severe pain, and immobilization), vertebral destruction causing instability, neurological deficit, and abscess formation.
Preoperative antibiotics were administered in all patients.
An anterior debridement and fusion with or without instrumentation were performed. Anterior access to the spine was achieved through a left retroperitoneal or thoracotomy approach. After exposure of the anterior aspect of the affected disc, all of the diseased disc material together with the endplate cartilage was resected down to healthy bleeding bone. The entire vertebral body rather than its involved parts removed, even if only a single vertebral body had been involved. Radical debridement as much as possible was performed in all patients, including abscess drainage in the presence of abscess formation. Adequate decompression of the dural sac was ensured at the same time. Anterior fusion was performed using a tricortical autologous graft harvested from the iliac crest. In some patients at the levels just above and below the fused segments, we used the Kaneda 2-rod system instrumentation (Tıp-Med, İzmir, Turkey) for patients with 2-level spondylodiscitis at the thoracolumbar junction or for patients in the 2-level corpectomy.
Diagnostic cultures were obtained from the affected vertebral body and/or disc or contiguous tissues during surgery. All specimens were sent for Gram staining, aerobic and anaerobic culture, and sensitivity, fungal culture, and acid-fast staining.
Fusion criteria, documented on 3-dimensional computed tomography (3D CT) studies, included: (1) the presence of bony trabeculation and (2) presence or lack of bony lucency at the iliac bone graft/vertebral body interface.
RESULTS
Twenty of the patients were female whereas 19 were male, with a mean age of 47 years ranging from 21 to 75 years. Of the whole group 20 patients (mean age, 49 years) suffered from tuberculous (specific) spondylodiscitis (Pott's disease) and 19 (mean age, 43 years) suffered from hematogenous spondylodiscitis. The patients 21 to 39 years old (n:11), 40 to 59 years old (n:19), and 60 years and older (n:9) had similar characteristics as did the patients with only 1 level involved (n:20) and the patients with 2 or 3 levels (n:19).
Clinical Presentation
There were 66 involved vertebral bodies in total, with single level involvement in 20 patients, 2 levels in 11 patients, and 3 levels in 8 patients. Fifteen patients had thoracic involvement, 20 had lumbar involvement, and 4 had thoracolumbar junction (T12-L1) involvement. The most commonly affected vertebra was L4, which was involved in 12 patients (30.7%). In 17 patients (43%), the infection extended deeply into the adjacent soft tissue with formation of paravertebral or psoas abscess. The duration of symptoms from onset to the time of diagnosis ranged from 1 week to 3 years (mean 15 weeks). Two patients with pyogenic spondylodiscitis and 3 patients with spinal tuberculosis have experienced the symptoms more than a year.
Local spinal pain was present in 37 of 39 patients (95%), with 18 (46%) also having radicular components. Radicular pain was unilateral in 10 patients and bilateral in 8 patients. Of the 13 patients (33%), 5 were Frankel C and 8 were Frankel D.
Of the whole group of patients 16 (41%) patients were in the reduced general condition because of associated illnesses, especially diabetes mellitus (11 patients). Other associated conditions were Cushing disease (1 patient) and chronic renal insufficiency (4 patients).
Laboratory Results
On presentation, preoperative laboratory studies showed an average WBC of 9.4 mm3 (range, 3.6–17.6) in the 20 patients with pyogenic spondylodiscitis and 8.9 mm3 (range, 5.3–14.8) in the 19 patients with tuberculous spondylodiscitis. Erythrocyte sedimentation rate was elevated in 18 of 20 patients with pyogenic spondylodiscitis, ranging from 2 to 140 mm with a mean of 95 mm in the 1st h. Erythrocyte sedimentation rate was normal in 7 patients and was raised in the other 12 patients with tuberculous spondylodiscitis, ranging from 28 to 129 after 1 h (mean, 70 mm). C-reactive protein levels were elevated (range, 2–156 mg/dL; mean, 33 mg/dL) in all of the patients.
Diagnostic Imaging
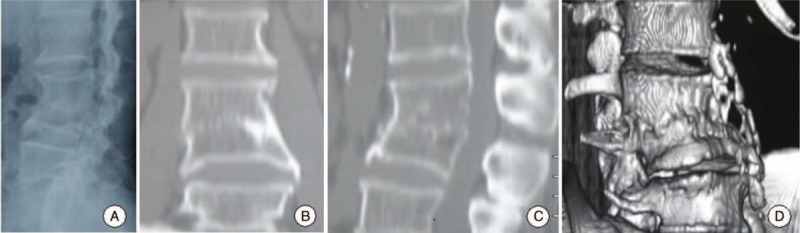
Plain radiographs revealed typical bony destruction with disc space narrowing and endplate erosion in the early stage of infection or vertebral body destruction in the next phase in 30 of the 39 patients. Computed tomography scans mostly revealed bony destruction and the absence of soft tissue masses. Vertebral collapse, destruction, paravertebral and/or psoas abscess, and spinal cord or dural sac compression due to abscess were seen on MRI (Fig. 1). Preoperative sagittal T1- and T2-weighted MRI shows the destruction from T10 to T11 vertebral bodies and discs and epidural abscess and spinal cord compression can be seen in Figure 1. The diagnosis was confirmed by CT in 34 patients and by MRI in 39 patients. MRI accurately identified paravertebral or psoas abscesses (17 patients).
FIGURE 1.

Preoperative 3D CT scan (A) and sagittal T1- and T2-weighted MRI (B, C) showing a destruction T10–11 disc space and vertebral bodies. Gadolinium enhancement sagittal and axial T1-weighted images reveal epidural abscess and spinal cord compression.CT = computed tomography, MRI = magnetic resonance imaging.
SURGERY
Patients underwent single level discectomy + fusion (20 patients), 2-level discectomy + fusion (3 patients), single level corpectomy + fusion (4 patients), single level corpectomy + fusion + instrumentation (4 patients), 2 level corpectomy + fusion + instrumentation (8 patients). Kaneda 2-rod system instrumentation was used in 12 patients, in total. The surgical procedures are shown in Table 2.
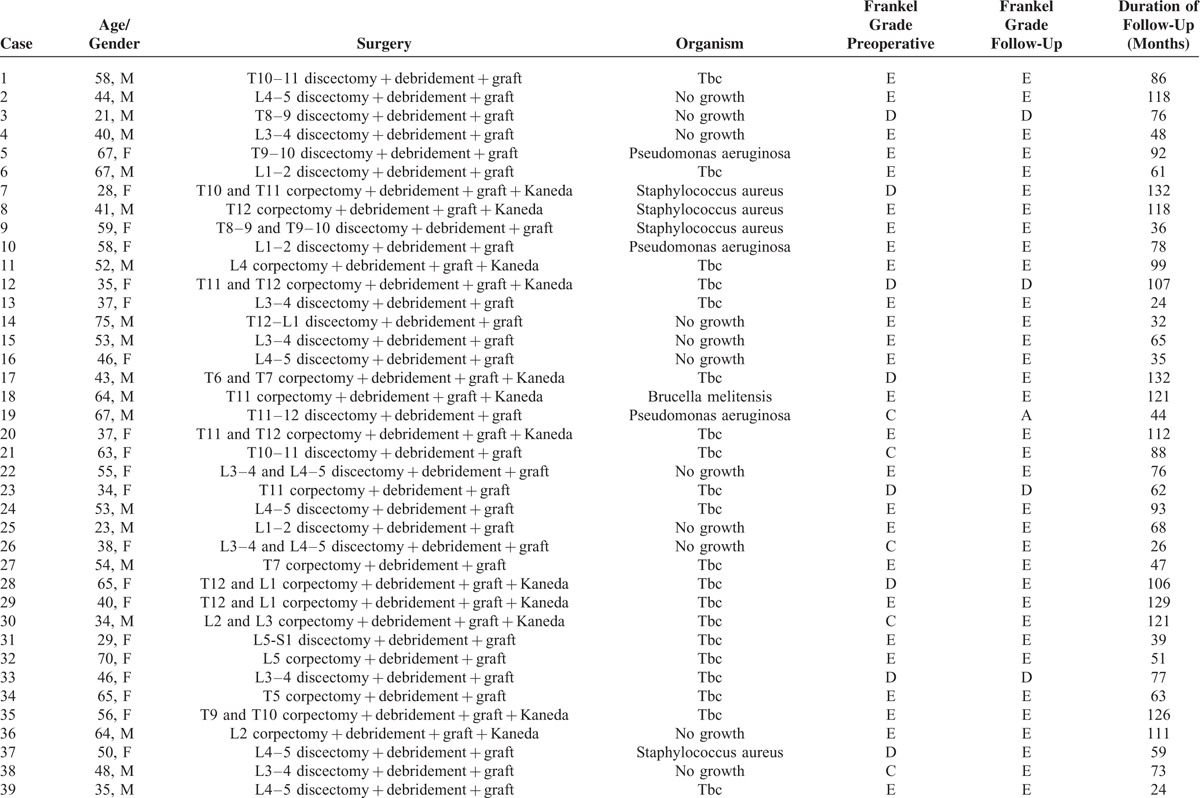
TABLE 2.
Length of Follow-Up, Preoparative, and End of Follow-Up, Frankel grades, Surgical Procedures, and Microbiological Organisms in 39 Patients
Microbiology and Isolation of the Organisms
Intraoperative specimen cultures were reported as positive in 11 of the 39 patients. A specific organism could be isolated in 8 (42%) of the 19 patients with pyogenic spondylodiscitis. Pathogenic bacteria responsible for pyogenic spondylodiscitis in this series included Staphylococcus aureus (4 patients), Pseudomonas aeruginosa (3 patients), and Brucella melitensis (1 patient). Blood cultures were positive in 4 patients. In 11 patients, no specific organism could be identified. Tuberculous spondylodiscitis (20 patients) could be bacteriologically proved in only 3 patients. In the remaining 17 patients tuberculous spondylodiscitis was histopathologically demonstrated. The etiological agents of spondylodiscitis are shown in Table 2.
Antibiotic Treatment
The initial antibiotic regimen used was vancomycin + ceftriaxone + rifampicin. Then, the antibiotic treatment was modified depending on the sensitivity of the isolated organisms. The patients with pyogenic spondylodiscitis were treated with an appropiate antibiotic through intravenous route for 6 weeks, followed by the oral intake of same antibiotic for 6 weeks. The patients with tuberculous spondylodiscitis were treated with standard doses of isoniazid, rifampicin, ethambutol, and pirazinamid for 2 months, followed by isoniazid combined with rifampicin for 10 months. One patient with brucellar spondylodiscitis was treated with either intramuscular streptomycin 1 g/day for 21 days and oral doxycyline 100 mg twice daily or oral rifampicin 900 mg once daily for 3 months.
COMPLICATIONS
Major venous vessel injury occurred during dissection around the anterior aspect of the spinal column due to extensive scarring and the inflammatory response elicited in the local tissue in 2 cases. These injuries were primarily repaired and no postoperative sequela was encountered. Other perioperative complications included left iliac artery occlusion and pleural effusion (2 patients). No patient had postoperative wound dehiscence.
Clinical Outcomes
Preoperative neurological deficits were noted in 13 of the 39 patients. In terms of Frankel grade, 8 patients have improved, 4 have remained the same, and 1 patient has worsened during the follow-up period. Eight had improvement of 1 grade (4 patients, from grade D to grade E) or more (4 patients, from grade C to grade E) on the Frankel scale. Four patients had remained the same (from grade D to grade D) and 1 patient had worsened (from grade C to grade A) (Fig. 2). One patient with nonspecific L3–4 spondylodiscitis, a 40-year-old man, who had been clinically and radiologically considered to be cured, experienced a late recurrence >1 year after his discharge. The patient refused a second operation. Another patient, a 35-year-old man was admitted to our clinic because of right leg pain and weakness of right lower extremity. His medical history was relevant for symptomatic chronic renal failure for the last 6 years and he had been undergoing hemodialysis 3 days a week. During surgery, debridement of the L4–5 space with epidural abscess drainage and iliac crest bone grafting were performed. Unfortunately, the patient died of renal failure 2 years later. A 67-year-old woman with Pseudomonas spondylodiscitis at the T9 to T10 level experienced recurrence within 2 months with new neurological compromise. Although this patient had initially presented with Frankel grade C, she had Frankel grade A 2 months after the surgery. The patient refused a second operation.
FIGURE 2.
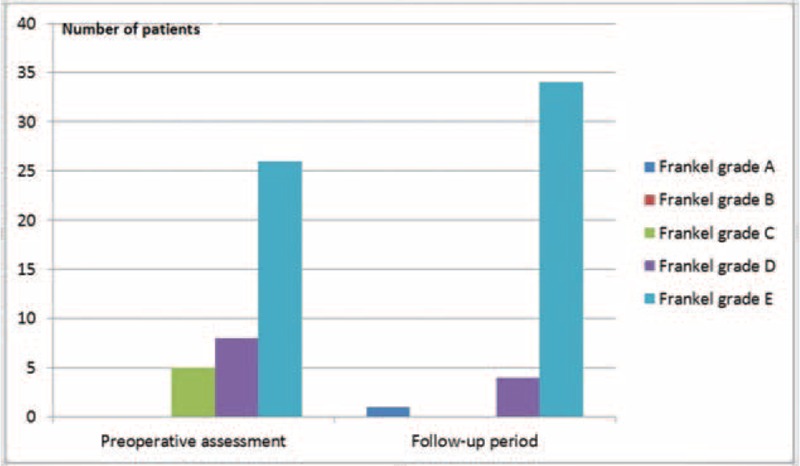
Frankel grades of the patients.
Data analysis was performed using SPSS for Windows, version 11.5. We used ANOVA and T test to compare differences in groups. P values used to determine whether the differences were statistically significant. A P value <0.05 was considered statistically significant. There was no significantly difference between preoperative and follow-up group (P = 0.113).
Radiographic Outcomes
Imaging-documented fusion was achived in 23 of 27 patients in the graft group (85% fusion rate) (Figs. 3 and 4) and 11 of 12 patients in the graft + Kaneda instrumentation group (91% fusion rate) (Figs. 5 and 6). There was no instrumentation failure, loosening, or graft-related complication such as slippage or fracture of the graft.
FIGURE 3.

Anteroposterior (A) and sagittal (B) CT scan and 3D CT scan (C, D) showing a stable fusion.CT = computed tomography.
FIGURE 4.
Plain lateral radiograph (A), anteroposterior-sagittal CT scan (B, C), and 3D CT scan showing anterior interbody fusion in lumbar spine. CT = computed tomography.
FIGURE 5.

Plain lateral radiograph (A) and 3D CT scan (B) showing a bony fusion in thoracolumbar junction and Kaneda instrumentation from T11 to L2. CT = computed tomography.
FIGURE 6.
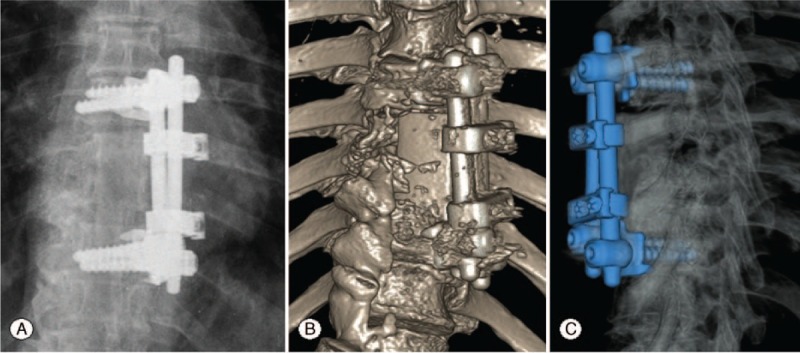
Plain lateral radiograph (A) and 3D CT scan (B, C) showing a anterior fusion and Kaneda instrumentation from T8 to T11. CT = computed tomography.
DISCUSSION
Spondylodiscitis is a relatively rare condition that makes up 2% to 7% of osteomyelitis cases. However, the incidence of the disease has increased in the recent years. This increase is attributed to prolonging of average age, malnutrition, immunosupression caused by AIDS or chemotherapy, diabetes mellitus, chronic renal failure, alcohol intake, chronic use of steroids, and septicemia.2–7 Diabetes mellitus is the most frequent accompanying disease in patients with spondylodiscitis due to miscellaneous bacteria. Diabetes mellitus is a well-recognized risk factor for sepsis and is, in part, due to sustained hyperglycemia retarding neutrophil chemotaxis. Patients with chronic renal failure are at a higher risk of tuberculosis compared to the general population. All of the spondylodiscitis patients with accompanying chronic renal failure developed spondylodiscitis caused by tuberculosis. Patients of chronic renal failure are well-recognized to be at an increased risk of bacteremia due to their uremia-induced immunosupression and repeated dialysis and hospitalizations.3,8Although the comparison of surgical and nonsurgical patients is subjective but the most common predisposing condition was diabetes mellitus in our study (11 patients). Other associated conditions were chronic renal failure (4 patients) and Cushing disease (1 patient). Spinal infections may also be caused by penetrating trauma or spinal surgeries.3,5
The clinical symptoms of spondylodiscitis are nonspecific. The most frequent symptoms are back pain and paravertebral muscle spasm, as confirmed in our study.4,5 The rate of patients with neurological involvement is in the range of 10% to 50%. Neurological deficit is one of the most important symptoms of tuberculous spondylodiscitis. The delay between the onset of initial symptoms and the diagnosis is 2 to 6 months reportedly.3,5 In this series, there were 13 patients (33%) who were subject to neurological deficits. In our experience, patients came under observation 1 week to 3 years (mean 15 weeks) after beginning of back pain.
Rise in ESR and CRP is seen in >90% of spondylodiscitis patients. Leucocytosis occurs in <50%. Lestini and Bell9 suggested that CRP is superior to ESR in the evaluation of spinal infection as it rises more quickly and is less influenced by other plasma factors. In our study, ESR was raised in 30 (77%) patients. The CRP level was elevated in all cases and revealed to be the most valuable laboratory parameter.
Plain radiographs have low sensitivity in the early stages of spondylodiscitis, as abnormalities usually develop later on. In 75% of spondylodiscitis cases, the first alterations are visible on the segment involved after 2 to 4 weeks from the onset of the infectious process. The abnormalities are disc space narrowing, blurring of the endplates, and loss of height of the affected vertebral bodies. In untreated cases bony sclerosis appears at 10 to 12 weeks.4,5,8,10 Computed tomography scans are also sensitive in detecting signs of spondylodiscitis but do not demonstrate the soft tissue anatomy well. Abnormalities are visible in the first 2 weeks in half of the patients.5,8 Magnetic resonance imaging is the most sensitive means of confirming an early diagnosis for spondylodiscitis and it has foremost importance in diagnostic procedure of this disease. With 96% sensitivity, 94% specificity, and 92% accuracy, MRI shows pathological alterations with improved anatomic detail.4,5,10,11 All of the patients in our study had plain radiographs, CT and MRI. Interestingly, 77% of the cases in our series that had plain radiographs also had signs of spondylodiscitis.
Blood culture can be very useful in the diagnosis of pyogenic spondylodiscitis and positive identification in about half of the cases.12–14 In our patients of pyogenic spondylodiscitis, the rate of positive blood cultures was 21%, which is lower than that in other series. Open biopsy provides positive cultures in >75% of the cases.12,14–16 In our series, biopsy was performed intraoperatively in all cases; of these, 28% were culture positive which is lower than that in many other series. Also, ESR was higher in our patients with pyogenic spondylodiscitis.
Early treatment of sponylodiscitis may decrease morbidity and mortality. Most of spondylodiscitis cases can be treated with immobilization and intravenous antibiotics. Surgical indications included failure of medical treatment, severe pain, vertebral destruction causing instability, neurological deficit, and abscess formation. Different surgical techniques have been described for the treatment of spondylodiscitis. Some authors described anterior, posterior, or combined approaches in single or 2 staged procedures.6,7,17–24
The main factors which affect the decision on the surgical approach in the presence of spinal infections include the age, general health status of the patient, localization of the infection, stabilization, and the need for fusion; furthermore, the experience of the surgeon in using the surgical approaches and stabilization methods is also important.25 Decompression is achieved by easily accessing the lesions that are localized in the posterior part through laminectomy and sufficient amount of biopsy material can be taken. However, if the lesion is localized in the anterior part, it is difficult to access the lesion and take the biopsy material and it may also cause instability because the posterior elements will be removed; therefore laminectomy is contraindicated. If laminectomy is performed for the patients whose vertebral body is widely involved, the existing deformity may deteriorate and instability may be caused. Minimally invasive systems (eg with the VIPER-system) can be used to provide temporary stabilization in some cases that spinal instability occured.26,27 These systems diminish the major surgical stress and provide mobilization and can be performed percutaneous.
The anterior approach to the spine was first described as early as 1750 by Geraud22 Hodgson and Stock23 used an anterior approach for decompression and autologous bone grafting and reported that 94% of patients made a complete recovery for the treatment of Pott's disease in 1960. The most important advantages of the anterior procedure are that it does allow radical resection of the infectious focus and does enable satisfactory interbody fusion. Patients had rapid infection resolution and early and frequent bony fusions. Richardson et al24 used the transthoracal approach for Pott disease. The anterior approach decreases postoperative pain and provides early ambulation and protects posterior ligamentous structures. Thoracotomy provides a good exposure from T5 to T12 and contralateral hemitorax must be choosen in patients who had previous chest operation to reducebleeding, atelectasis, and pneuomotorax.28 To minimize the risk of cordal ischemia the artery of Adamkiewicz have to be kept in mind. The artery of Adamkiewicz is located on the left side in ∼80% of cases. This artery arises from T9 to T12. Benli et al29 reported 100 patients with tuberculous spondylodiscitis of the thoracic and lumbar regions. Their results demonstrated that the use of anterior instrumentation and anterior radical debridement was safe and effective. Ozdemir et al30 demonstrated a 96% fusion rate in 28 patients treated with anterior fusion with fibula allograft and anterior instrumentation for Pott's disease. The limitation of the previous studies for anterior approach associated with spondylodiscitis was the subjectivity of criteria used for the evaluation of fusion, although they were based on radiographic and clinical evaluation. The fusion mass was evaluated by 3D CT in our study. Thus, this limitation was eliminated. In this study, the successful interbody fusion rate was achived in 34 patients (87% fusion rate). Imaging-documented fusion was achieved in 85% of the patients in the graft group and 91% of those in the graft + Kaneda instrumentation group.
Sahoo et al reported a 55.5% fusion rate via posterior approach surgery.31 Zaveri and Mehta reported 13 of 15 patients had fusion by the posterior approach and instrumentation.32
The anterior spine approach is a safe procedure when carefully coordinated by thoracic surgeons and spine surgeons.28–33 In review of 1223 anterior spinal fusions, Faciszewski et al34 reported an 11.5% rate of complications solely attributable to the anterior approach. Benli et al29 reported that there were no apparent pseudoarthroses and implant failures in 100 patients with tuberculous spondylodiscitis. There had been a 2 major venous vessel injury during surgery in our patients. But, these injuries primarily repaired. Other perioperative complications included left iliac artery occlusion and pleural effusion. There was no instrumentation or graft-related complication.
Dramatic neurological recovery after anterior surgical decompression may occur. Liebergall et al35 described 12 patients, all of whom underwent anterior surgery for severe neurological deficit. All had significant improvement of at least 1 grade on the Frankel scale. In Benli's series29 there were 44 patients (44%) who were subject to neurological symptoms. In the follow-up period, 40 of them achieved full (91%) and 4 achieved partial recovery (9%). Preoperative neurological deficits were noted in 13 of the 39 patients (33%) in our study. In terms of Frankel grade, 8 of the patients have improved during the follow-up period (62%) and 4 have remained the same since last follow-up (31%). One patient with P. spondylodiscitis worsened 2Frankel grades during follow-up (7%).
CONCLUSION
Treatment of pyogenic and tuberculous spondylodiscitis with or without anterior instrumentation along with anterior debridement and autologous iliac bone fusion provides a high fusion rate. At the same time, this approach appears a safe method associated with a low rate of complications. This technique demonstrated a good recovery rate of neurological functions. Most patients improved significantly not only their general conditions but also neurological status after anterior surgery without any serious complications in our study.
Footnotes
Abbreviations: CRP = C-reactive protein, CT = computed tomography, ESR = erythrocyte sedimentation rate, MRI = magnetic resonance imaging, WBC = white blood cell count.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Zhao J, Lian XF, Hou TS, et al. Anterior debridement and bone grafting of spinal tuberculosis with one-stage instrumentation anteriorly or posteriorly. Int Orthop 2007; 31:859–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frankel HL, Hancock DO, Hyslop G. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplagia. Paraplegia 1969; 7:179–192. [DOI] [PubMed] [Google Scholar]
- 3.Turunc T, Demiroglu YZ, Uncu H, et al. A comparative analysis of tuberculous, brucellar and pyogenic spontaneous spondylodiscitis patients. J Infect 2007; 55:158–163. [DOI] [PubMed] [Google Scholar]
- 4.Cottle L, Riordan T. Infectious spondylodiscitis. J Infect 2008; 56:401–412. [DOI] [PubMed] [Google Scholar]
- 5.Bettini N, Girardo M, Dema E, et al. Evaluation of conservative treatment of non spesific spondylodiscitis. Eur Spine J 2009; 18:S143–S150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hempelmann RG, Mater E, Schön R. Septic hematogenous lumbar spondylodiscitis in elderly patients with multiple risk factors: efficacy of posterior stabilization and interbody fusion with iliac crest bone graft. Eur Spine J 2010; 19:1720–1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mann S, Schütze M, Sola S, et al. Nonspesific pyogenic spondylodiscitis: clinical manifestations, surgical treatment, and outcome in 24 patients. Neurosurg Focus 2004; 17:E3. [DOI] [PubMed] [Google Scholar]
- 8.Al-Nammari SS, Lucas JD, Lam KS. Hematogenous methicillin-resistant Staphylococcus aureus spondylodiscitis. Spine 2007; 32:2480–2486. [DOI] [PubMed] [Google Scholar]
- 9.Lestini WF, Bell GR. Spinal infection: patient evaluation. Semin Spine Surg 1996; 8:81–94. [Google Scholar]
- 10.Varma R, Lander P, Assaf A. Imaging of pyogenic infectious spondylodiscitis. Radiol Clin North Am 2001; 39:203–213. [DOI] [PubMed] [Google Scholar]
- 11.Ledermann HP, Schweitzer ME, Morrison WB, et al. MR imaging findings in spinal infections: rules or myths? Radiology 2003; 228:506–514. [DOI] [PubMed] [Google Scholar]
- 12.Jimenez-Mejias ME, Colmenero J, Sanchez-Lora FJ. Postoperative spondylodiscitis: etiology, clinical findings, prognosis, and comparision with nonoperative pyogenic spondylodiscitis. Clin Infect Dis 1999; 29:339–345. [DOI] [PubMed] [Google Scholar]
- 13.Khan IA, Vaccaro AR, Zlotolow DA. Management of vertebral diskitis and osteomyelitis. Orthopedics 1999; 22:1668–1679. [DOI] [PubMed] [Google Scholar]
- 14.Lam KS, Webb JK. Discitis. Hosp Med 2004; 65:280–286. [DOI] [PubMed] [Google Scholar]
- 15.An HS, Seldomridge JA. Spinal infections. Clin Orthop Relat Res 2006; 444:27–33. [DOI] [PubMed] [Google Scholar]
- 16.Perronne C, Saba J, Behloul Z, et al. Pyogenic and tuberculous spondylodiscitis (vertebral osteomyelitis) in 80 adult patients. Clin Infect Dis 1994; 19:746–750. [DOI] [PubMed] [Google Scholar]
- 17.Cavusoglu H, Kaya RA, Türkmenoglu ON, et al. A long-term follow-up study of anterior tibial allografting and instrumentation in the management of thoracolumbar tuberculous spondylitis. J Neurosurg Spine 2008; 8:30–38. [DOI] [PubMed] [Google Scholar]
- 18.Fukuta S, Miyamoto K, Masuda T. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic pondylitis. Spine 2003; 28:e302–e308. [DOI] [PubMed] [Google Scholar]
- 19.Guzey FK, Emel E, Bas NS. Thoracic and lumbar tuberculous spondlotis treated by posteior debridement, graft placement, and instrumentation: a retrospective analysis in 19 cases. J Neurosurg Spine 2005; 3:450–458. [DOI] [PubMed] [Google Scholar]
- 20.Snell BE, Nasr FF, Wolfla CE. Sıngle-stage thoracolumbar vertebrectomy with circumferential reconstruction and arthrodesis: surgical technique and results in 15 patients. Neurosurgery 2006; 58:263–268. [DOI] [PubMed] [Google Scholar]
- 21.Pee YH, Park JD, Choi YG, et al. Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone strut versus cage. J Neurosurg Spine 2008; 8:405–412. [DOI] [PubMed] [Google Scholar]
- 22.Dick JC, Brodke DS, Zdeblick TA, et al. Anterior instrumentation of the thoracolumbar spine: a biomechanical comparison. Spine 1997; 22:744–750. [DOI] [PubMed] [Google Scholar]
- 23.Hodgson AR, Stock FE. Anterior spine fusion for the treatment of tuberculosis of the spine. The operative findings and results of treatment of the first one hundred cases. J Bone Joint Surg Am 1960; 42:295–310. [Google Scholar]
- 24.Richardson JD, Campbell DL, Grover FL. Transthoracic approach for Pott's disease. Ann Thorac Surg 1976; 21:552–556. [DOI] [PubMed] [Google Scholar]
- 25.Sharif HS. Role of MR imaging in the management of spinal infections. Am J Roentgenol 1992; 158:1333–1345. [DOI] [PubMed] [Google Scholar]
- 26.Kretzer RM, Molina C, Hu N, et al. A Comparative Biomechanical Analysis of Stand Alone Versus Facet Screw and Pedicle Screw Augmented Lateral Interbody Arthrodesis: An In Vitro Human Cadaveric Model. J Spinal Disord Tech. 2013 Nov 7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Oh HS, Kim JS, Lee SH, et al. Comparison between the accuracy of percutaneous and open pedicle screw fixations in lumbosacral fusion. Spine J 2013; 13:1751–1757. [DOI] [PubMed] [Google Scholar]
- 28.Pettiford BL, Schuchert MJ, Jeyabalan G. Technical challenges and utility of anterior exposure for thoracic spine pathology. Ann Thorac Surg 2008; 86:1762–1768. [DOI] [PubMed] [Google Scholar]
- 29.Benli IT, Kaya A, Acaroglu E. Anterior instrumentation in tuberculous spondylitis. Is it effective and safe? Clin Orthop Relat Res 2007; 460:108–116. [DOI] [PubMed] [Google Scholar]
- 30.Ozdemir HM, Us AK, Ogun T. The role of anterior spinal instrumentation and allograft fibula for the treatment of Pott's disease. Spine 2003; 28:474–479. [DOI] [PubMed] [Google Scholar]
- 31.Sahoo MM, Mahapatra SK, Sethi GC, et al. Posterior-only approach surgery for fixation and decompression of thoracolumbar spinal tuberculosis: a retrospective study. J Spinal Disord Tech 2012; 25:E217–E223. [DOI] [PubMed] [Google Scholar]
- 32.Zaveri GR, Mehta SS. Surgical treatment of lumbar tuberculous spondylodiscitis by transforaminal lumbar interbody fusion (TLIF) and posterior instrumentation. J Spinal Disord Tech 2009; 22:257–262. [DOI] [PubMed] [Google Scholar]
- 33.De Giacomo T, Francioni F, Diso D. Anterior approach to the thoracic spine. Interact Cardiovasc Thorac Surg 2011; 12:692–695. [DOI] [PubMed] [Google Scholar]
- 34.Faciszewski T, Winter RB, Lonstein JE, et al. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine 1995; 20:1592–1599. [DOI] [PubMed] [Google Scholar]
- 35.Liebergall M, Chaimsky G, Lowe J, et al. Pyogenic vertebral osteomyelitis with paralysis. Clin Orthop 1991; 269:142–149. [PubMed] [Google Scholar]


