Abstract
This study investigated whether spirituality/religiosity (S/R) plays an important role in the lives of cancer patients and in the work of health professionals who provide care for these patients. The correlations between spiritual quality of life (QOL) and the other QOL domain scores of patients and health professionals were also assessed. Moreover, QOL domain scores were compared between patients and health professionals. In this cross-sectional study, 1050 participants (525 oncology patients and 525 health professionals) were interviewed. Quality of life was assessed with the World Health Organization quality of life spiritual, religious, and personal beliefs (WHOQOL-SRPB). To compare the groups with respect to the instruments’ domains, a quantile regression and an analysis of covariance model were used. The WHOQOL-Bref and WHOQOL-SRPB domains were correlated by performing Pearson and partial correlation tests. It was demonstrated that 94.1% of patients considered it important that health professionals addressed their spiritual beliefs, and 99.2% of patients relied on S/R to face cancer. Approximately, 99.6% of the patients reported that S/R support is necessary during cancer treatment; 98.3% of health professionals agreed that spiritual and religious support was necessary for oncology patients. Positive correlations between spiritual QOL and the other QOL domains were observed. When compared among themselves, patients exhibited significantly higher levels of spiritual QOL. In conclusion, S/R was an important construct in the minds of cancer patients and health professionals. Both groups often use S/R resources in their daily lives, which seems to positively affect their perceptions of QOL. Further studies are needed to determine how health professionals effectively address S/R during oncology practice.
INTRODUCTION
Quality of life (QOL) assessment has gained increasing attention in recent decades, reflecting the transformation of discussions on the health-disease process to a comprehensive view of the human being. Quality of life has been conceptualized in a heterogeneous manner, but there is a common thread of subjective, multidimensional, and bipolar characteristics.1 Given the conceptual diversity, the World Health Organization (WHO)2 defined QOL as the “individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.” This concept is broad and may be affected in a complex manner by physical health, psychologic state, level of independence, social relationships, and the characteristics of the individual's environment. Thus, the perception of QOL differs among individuals, cultures, places, and times.3
Considering the multidimensionality of QOL, it is believed that the diagnosis of cancer, the reactive psychologic manifestations, and the subsequent clinical manifestations of the disease and its treatment may negatively impact the QOL of oncology patients.4 Likewise, QOL at work is a key factor in global QOL, as the work encompasses a central part of individuals’ lives. Health professions may promote progressive and cumulative biopsychosocial consequences and can be viewed as potentially unhealthy.5,6 Health professionals dedicated to oncology, face human suffering with higher frequency and intensity, making them potentially vulnerable to emotional disorders.7
Spirituality/religiosity (S/R) is one of the coping strategies most frequently used by cancer patients, especially during periods of increased emotional stress, such as after the initial diagnosis, during the beginning of chemotherapy, after discontinuation of anticancer treatment, and after being referred to palliative care, among other stressful situations.8,9 The use of S/R as a coping strategy may help minimize the feeling of fear throughout the course of the disease and, also, potentially interfere in clinical decision-making processes.10–12 Moreover, higher S/R scores are associated with better social relationships,13 and higher levels of hope and QOL.11,13–20 When asked, patients report that they would like their spirituality to be addressed, while receiving care from health professionals.10–12,21–23
Despite the recognition of the importance of caring for the spiritual needs of patients, most health professionals have not received specific training to provide such care; therefore, they frequently fail to provide spiritual and religious support during their consultations.22,24,25 Nearly all physicians and nurses reported that spiritual care should be provided by professional hospital chaplains and the patients’ spiritual community. When compared with the nurses’ opinions, physicians reported less often that spiritual care was one of the roles of health professionals.26 Oncology professionals, however, frequently seek S/R to cope with their physically and emotionally consuming work routine.11,27
The scientific interest in evaluating the association between S/R and QOL in an oncology context is relatively recent. To date, there have been few publications concerning the views of the 2 groups involved in the health-disease process: the cancer patient and the hospital health professional dedicated solely to oncology. More information regarding their views is needed to better define how to provide effective spiritual care in daily practice. We believe that differing perspectives about S/R may influence the care of cancer patients and the decision-making process as a whole, which justifies the current study.
We hypothesized that cancer patients would have higher spiritual QOL domain scores because of the implications of their disease, but lower scores in other QOL domains compared with the health professionals who provide care for oncology patients.
Thus, the aim of this study was to evaluate the levels of spiritual QOL and their associations with the other QOL domains of cancer patients and of the health professionals who provide direct care to patients in a tertiary care cancer hospital. We also aimed to compare QOL domains (with a focus on spiritual domain) between patients and health professionals.
METHODS
Study Design and Site
This was a cross-sectional study in a tertiary care cancer hospital in São Paulo State, Brazil. The study was approved by the Institutional Research Ethics Committee of the Barretos Cancer Hospital (HCB 638/2012) and complied with the ethical standards of the Declaration of Helsinki and Brazilian National Health Council resolution no. 196/1996. All participants volunteered to participate in the study and signed an informed consent form after the study was described to them.
Study Population
Of 1076 potential candidates, 1050 were included in the study: 525 cancer patients and 525 health professionals. Patients were followed by the Departments of Clinical Oncology and Palliative Care. Health professionals included physicians, nurses, nurse technicians, physical therapists, pharmacists, psychologists, speech therapists, dentists, occupational therapists, social workers, and nutritionists who worked directly with the patients.
ELIGIBILITY CRITERIA
Patients
The inclusion criteria were patients over 18 years with a definite cancer diagnosis who were aware of the diagnosis and were undergoing adjuvant systemic treatment, palliative systemic treatment, or palliative care only.
Of the 537 patients invited to participate in the study, 12 were refused because of physical (n = 1) or emotional (n = 4) difficulties, pain (n = 1), lack of interest in the subject (n = 4), and lack of time (n = 2) (response rate = 97.7%). Please see the Supplemental Figure, which provides a flowchart of the study's recruitment process.
Health Professionals
Professionals over 18 years old who provided direct care to oncology patients were included. We excluded those professionals with a history of cancer within the last 10 years. 539 professionals were invited to participate in the study. There were 7 refusals because of lack of time (n = 2) or lack of interest in the subject (n = 5), and 7 professionals were excluded for having a history of cancer (response rate = 97.4%). See Supplemental Figure that provides a flowchart of the study's recruitment process.
SAMPLING METHOD
Charts of patients waiting for appointments at the outpatient clinic were randomly selected by the researchers.
The names of health professionals were obtained by simple random selection from the total number of those who worked directly with cancer patients in different departments of the institution.
Estimation of Sample Size
Based on the validation study of the WHOQOL-SRPB in Brazilian Portuguese,28 in which the mean of the instrument's domains was presented according to health status, the sample size for the comparison of groups was calculated by considering alpha and beta errors of 5% and 10%, respectively. When considering 5 points to represent a clinically relevant difference,29 we obtained minimal sample sizes for each domain of the WHOQOL-SRPB. For the current study, the largest one was calculated based on the spiritual connection domain using a sample size of 525 cancer patients and 525 health professionals. The formula used to calculate the sample size was:
 |
where n is the number of subjects required in each group, d is the standardized difference (target difference/standard deviation) and Cp, power is a constant defined by the values chosen for the P value and power.
Data Collection
The instruments for data collection were administered to patients before their medical appointments to ensure that the answers were not affected by any event or news received during the appointment. Surveys were administered by 3 trained researchers (MGC, BSRP, and EMB) and lasted 30 to 40 minutes for patients and 10 to 20 minutes for clinicians.
Instruments
Both groups answered a questionnaire concerning socioeconomic, clinical, and demographic characteristics, and a semistructured research instrument addressing religious affiliation, personal beliefs, and opinions regarding the importance of S/R in clinical practice developed specifically for this study. In addition, both groups answered the generic QOL instrument from the WHO (the WHOQOL-Bref) and the WHOQOL-SRPB instrument, which assessed the spirituality, religiousness and personal beliefs module developed by the WHO.
World Health Organization Quality of Life-Bref
This instrument consists of 4 domains and 26 questions addressing several aspects of everyday life. Scores range from 1 to 5, with 1 representing the worst and 5 the best perception of QOL. Total scores range from 0 to 100, with increasing numerical value indicating better quality of life. Respondents answer the QOL questions with reference to the prior 2 weeks.31 The internal consistency of the instrument in this study was α = 0.91 for patients and α = 0.87 for professionals.
World Health Organization Quality of Life-SRPB
This instrument consists of 8 domains and 32 items assessing S/R and personal beliefs. Individual items are rated on a Likert scale of 5 points, where 1 indicates negative perceptions and 5 indicates positive perceptions; thus, higher scores represent better spiritual QOL.32 The WHOQOL-SRPB was validated for Brazilian Portuguese in 2011 and demonstrated satisfactory psychometric qualities for healthy and ill men and women of different ages, beliefs, and sociocultural levels.28 The internal consistency of this instrument in our study was α = 0.96 for patients and α = 0.94 for professionals.
Statistical Analysis
The missing values for the WHOQOL-Bref and WHOQOL-SRPB were handled according to instructions from their manuals.33,34 To compare the groups with respect to the study variables (sex, age, marital status, education, financial income, and religion practice), WHOQOL-Bref and WHOQOL-SRPB domains, the χ2 test, and unpaired Student t-test were used. The WHOQOL SRPB scores were compared separately in subgroups of patients and health professionals using analysis of variance with Bonferroni multiple-comparisons test. Patients were categorized according to the general probability of death in curative anticancer therapy versus palliative anticancer treatment versus palliative care only; health professionals were categorized according to their theoretical daily contact with death as low (ambulatory, nuclear medicine department, and radiology department), medium (inpatient ward, Pediatric Department and Emergency Department), and high (Intensive Care and Palliative Care units). The quantile regression model35 was used to assess whether a specific quantile differed by the groups of interest (patients and health professionals). In addition to the quantile regression model, an analysis of covariance (ANCOVA) was also used. Regression analyses were conducted separately, with each WHOQOL domain as continuous dependent variable, and are presented in a summarized table. Both analyses were calculated after adjusting for age, sex, education level, family income, and religion practices. Based on a previous work,29 we considered clinically significant differences to be those with scores ≥5 points in a scale ranging from 0 to 100. An analysis of the correlation between the WHOQOL-Bref and WHOQOL-SRPB was performed by Pearson correlation. A correlation coefficient measures the strength of the relationship between 2 variables. Values can range from −1 to +1, and the closer it is to these extremes, the higher the association between variables will be. Negative coefficients mean that variables change in opposite ways. Correlation coefficients of >0.6, 0.4 to 0.6, and <0.4 were considered strong, moderate, and poor correlations, respectively.36 In addition, a partial correlation analysis was further performed. It was used to quantify the relationship between 2 variables while maintaining the effects of a set of independent variables constant. In all analyses, a significance level of P < .05 was employed. Quantile regression model and ANCOVA were conducted using R Statistical Software (The R Foundation for Statistical Computing, Vienna, Austria). The other statistical analyses were performed with SPSS software version 20.0 (Chicago, IL).
RESULTS
Most patients were men (n = 282, 53.7%), between 30 and 60 years old (n = 294, 56.0%), and married (n = 344, 65.5%). Most patients had children (n = 458, 87.2%), less than 8 years of education (n = 333, 63.4%), and a family income between 1× and 2× the minimum wage (n = 349, 66.5%). Most of the patients were professionally inactive (n = 472, 89.9%). Among all participants, 40.6% (n = 213) considered their health to be good, and 53.7% (n = 282) were functionally classified as Eastern Cooperative Oncology Group performance status 1 (Table 1).
TABLE 1.
Clinical and Demographic Characteristics of Cancer Patients and Health Professionals
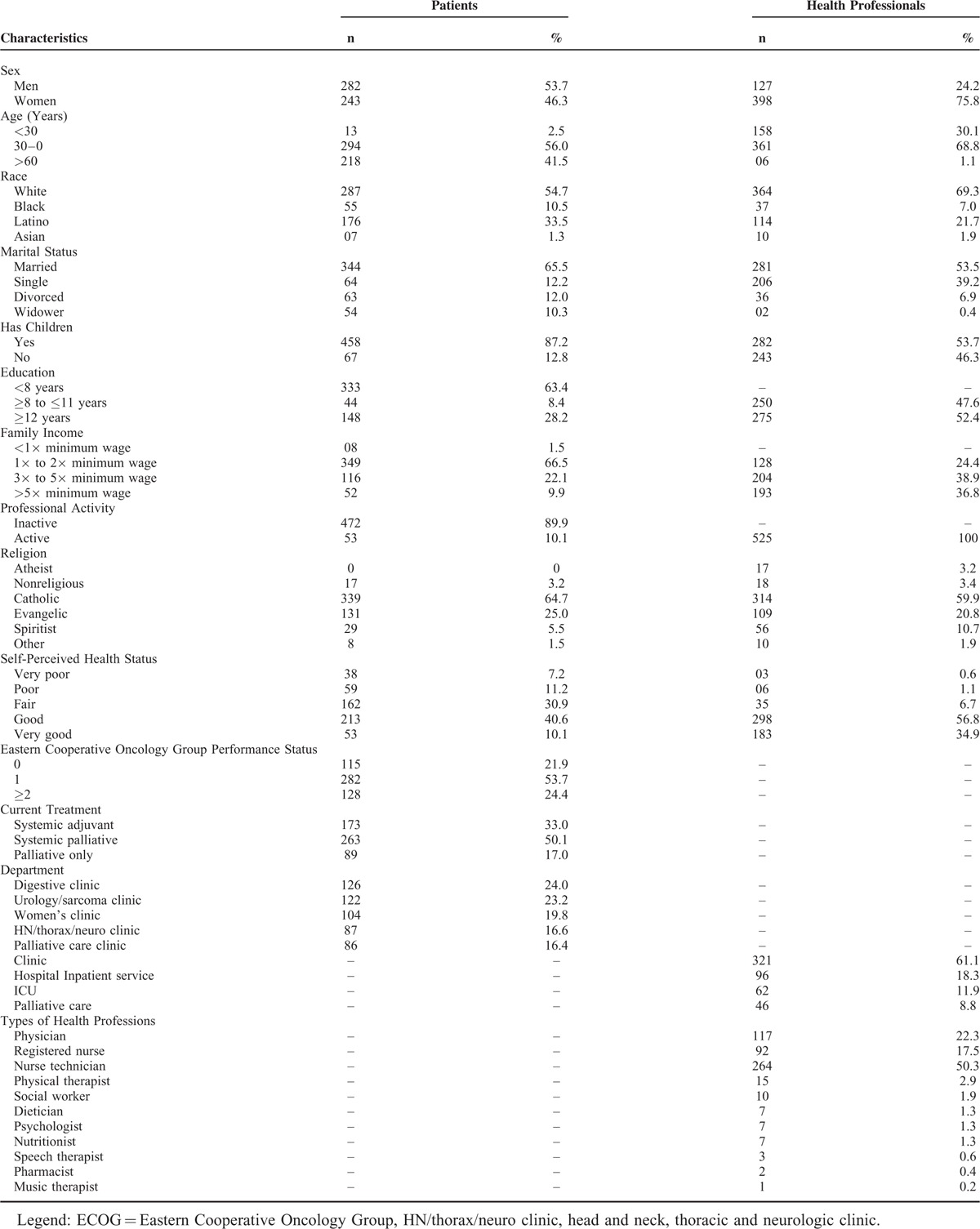
Among health professionals, the majority were women (n = 398, 75.8%), between 30 and 60 years old (n = 361, 68.8%), white (n = 364, 69.3%), and married (n = 281, 53.5%), and most had children (n = 282, 53.7%), over 12 years of education (n = 275, 52.4%), and a family income between 3× and 5× the minimum wage (n = 204, 38.9%). Regarding the types of health professions, the majority were physicians (n = 117, 22.3%), registered nurses (n = 92, 17.5%), and nurse technicians (n = 264, 50.3%). All of the professionals were professionally active (n = 525, 100%), and the majority considered their health to be good (n = 298, 56.8%) and worked at the clinics of the institution (n = 321, 61.1 %; Table 1).
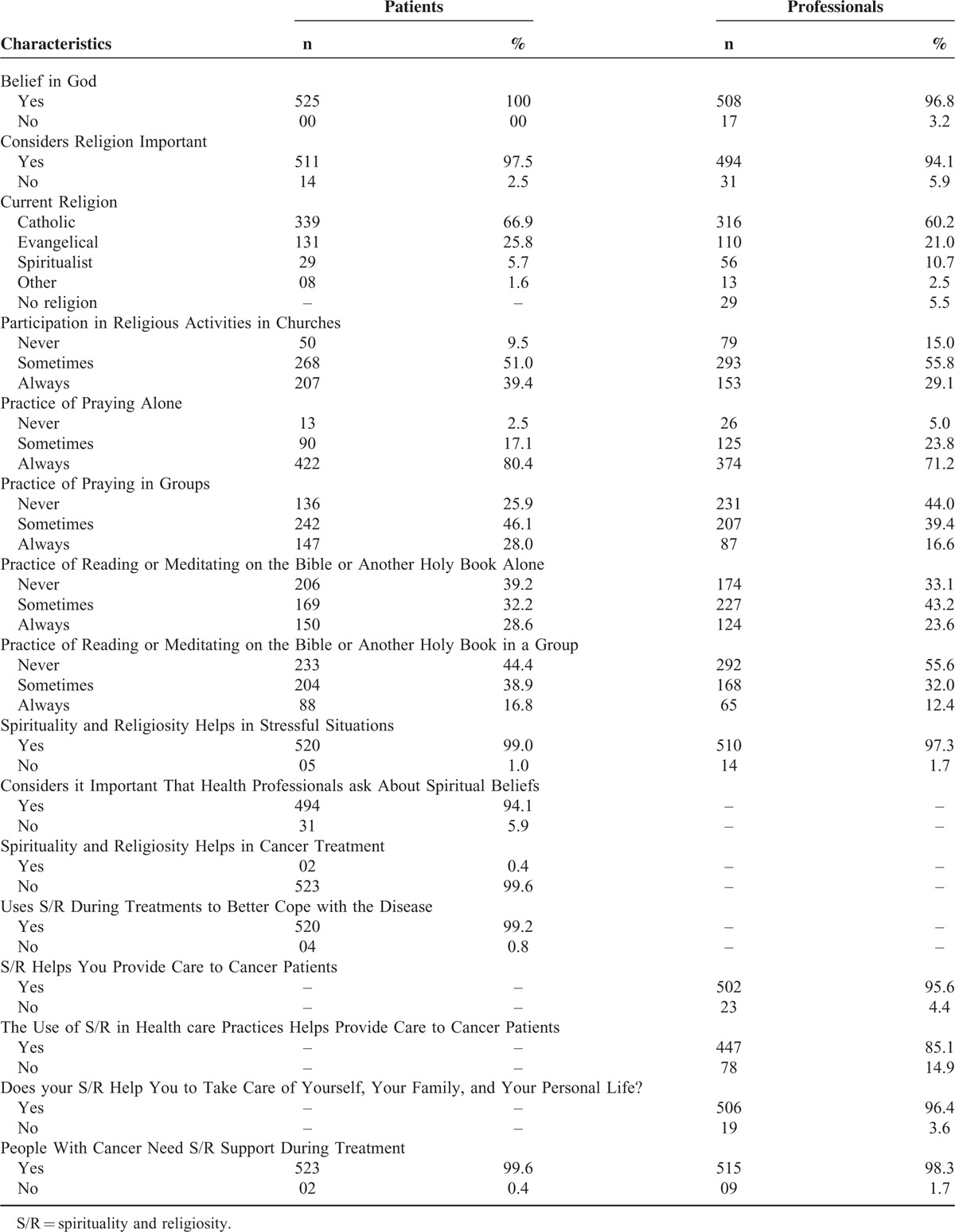
The characteristics of the spiritual, religious, and personal beliefs of both groups were evaluated. Most individuals were Catholic (patients: 66.9%, n = 339; professionals: 60.2%, n = 316), claimed to believe in god (patients: 100%, n = 525; professionals: 96.8%, n = 508), and believed that S/R helped them during stressful situations (patients: 99%, n = 520; professionals: 97.3%, n = 510). Among patients, 494 (94.1%) considered it important that health professionals asked them about their spiritual beliefs, 520 (99.2%) claimed to use S/R during treatment to better cope with the disease, and 523 (99.6%) reported that people with cancer require spiritual/religious support during cancer treatment. Similarly, 515 (98.3%) of health professionals agreed that spiritual and religious support was necessary for oncology patients (Table 2).
TABLE 2.
Spiritual, Religious and Personal Beliefs of Cancer Patients (n = 525) and Health Professionals (n = 525)
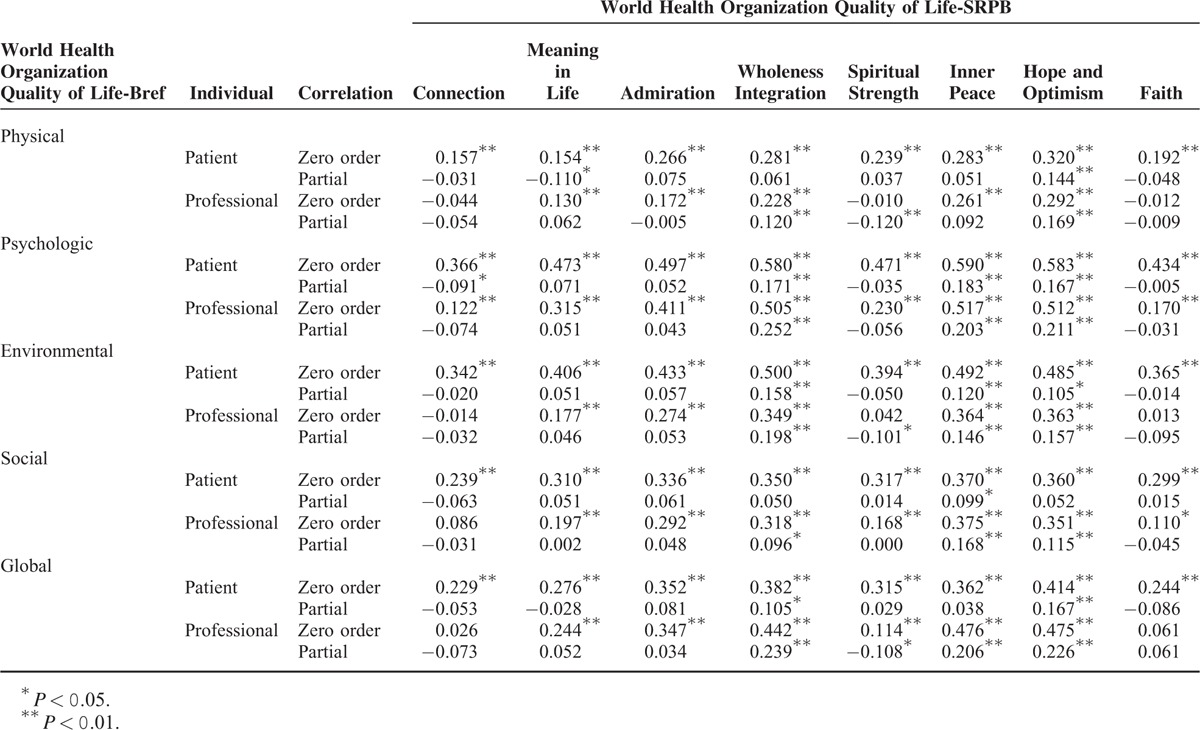
Moderate correlations were observed among most of the WHOQOL-SRPB domains and the psychologic (wholeness and integration r = 0.580, inner peace r = 0.590, hope and optimism r = 0.583, global r = 0.598) and environmental (wholeness and integration r = 0.500, global r = 0.512) domains of the WHOQOL-Bref according to patient scores. Among health professionals, moderate correlations were observed between wholeness and integration (r = 0.505), inner peace (r = 0.517), and hope and optimism (r = 0.512) of the WHOQOL-SRPB and the psychologic domain of the WHOQOL-Bref (Table 3). Considering that the spiritual QOL domains should interfere with each other in the relationship with WHOQOL-Bref domain scores, a partial correlation analysis was conducted. The partial correlation coefficients were lower than the Pearson correlation coefficients. Interestingly, the domains of most important partial correlations were whole and integration, inner peace and hope and optimism, both in patients and health professionals (Table 3 and Supplementary Table 1). The relationship between spiritual QOL as a whole (SRPB Global score) and WHOQOL-Bref domains was as follows: physical (patient r = 0.285, P < .001; professionals r = 0.148, P = .001), psychologic (patient r = 0.594, P < .001; professionals r = 0.428, P < .001), social (patient r = 0.387, P < .001; professionals r = 0.294, P < .001), environmental (patient r = 0.511, P < .001; professionals r = 0.225, P < .001), and global (patient r = 0.381, P < .001; professionals r = 0.328, P < .001).
TABLE 3.
Correlation Coefficients Between World Health Organization Quality of Life-Bref and World Health Organization Quality of Life-SRPB Scores in Patients and Health Professionals
Compared with the patients, the health professionals were predominantly women, younger and with higher educational status. Regarding religious practices, Catholics and Evangelicals were the most common in both groups; however, professionals presented higher numbers of atheists and spiritualists compared with patients (Table 4). Patients exhibited higher mean scores in the psychologic (76.3 versus 73.6; P = .002), social (77.6 versus 74.3; P = .001), environmental (75.8 versus 66.9; P < .001), and global (78.0 versus 71.9; P < .001) domains of the WHOQOL-Bref compared with professionals. On the contrary, professionals presented higher mean scores of the physical domain in comparison with patients (70.9 versus 74.7; P < .001). All domains of the WHOQOL-SRPB exhibited higher scores in patients compared with professionals (Table 4).
TABLE 4.
Clinical Characteristics and Mean Scores of Quality of Life and Spirituality/Religiosity of Cancer Patients (n = 525) and Health Professionals (n = 525)
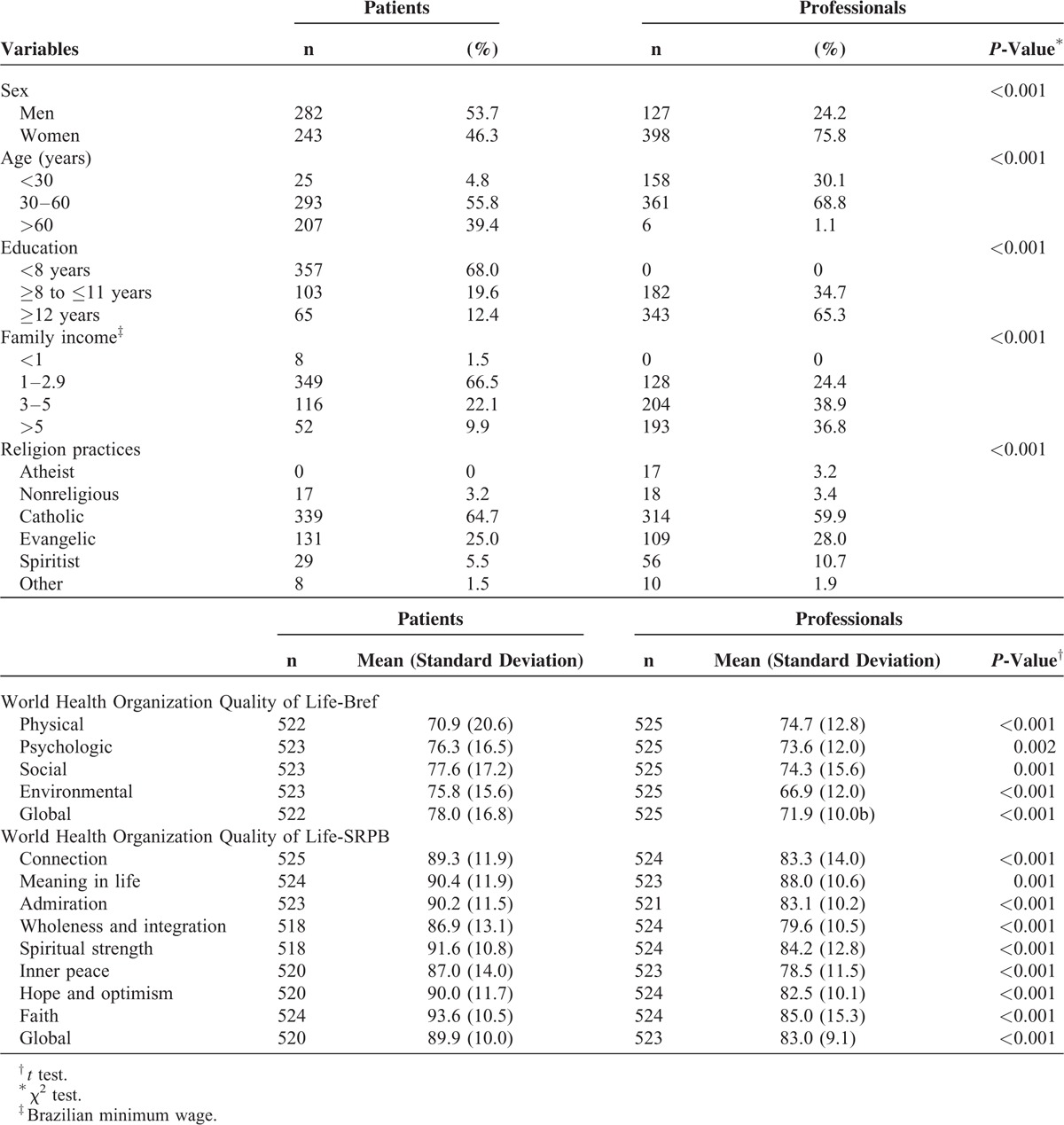
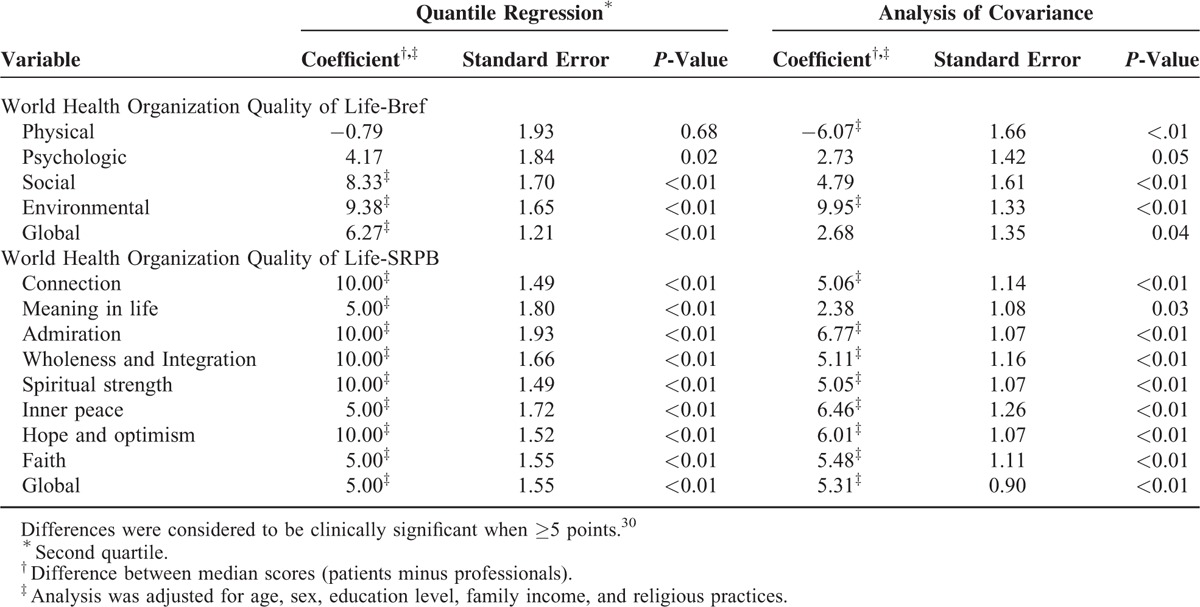
As patients and health professionals exhibited different sociodemographic characteristics, both a quantile regression and an ANCOVA model were applied to compare the WHOQOL-Bref and WHOQOL-SRPB domains after adjustments for age, sex, education level, family income, and religious practices. After these adjustments, health professionals continued to exhibit higher scores in the physical domain according to the ANCOVA analysis. Conversely, patients exhibited clinically significant higher scores for the social (quantile regression), environmental (quantile regression and ANCOVA) and global QOL (quantile regression) domains. Although patients presented higher scores in the psychologic domain, it was of low magnitude. We observed a clinically significant difference between groups when domains of the WHOQOL-SRPB were compared; patients exhibited higher spiritual QOL scores in all domains of the instrument even after adjustments (Table 5). Detailed results of the regression analyses are shown in the Supplementary Table 2.
TABLE 5.
Comparison Analysis of the Difference in Scores Between Patients and Health Professionals After Adjustments From the Quantile Regression and Analysis of Covariance Models
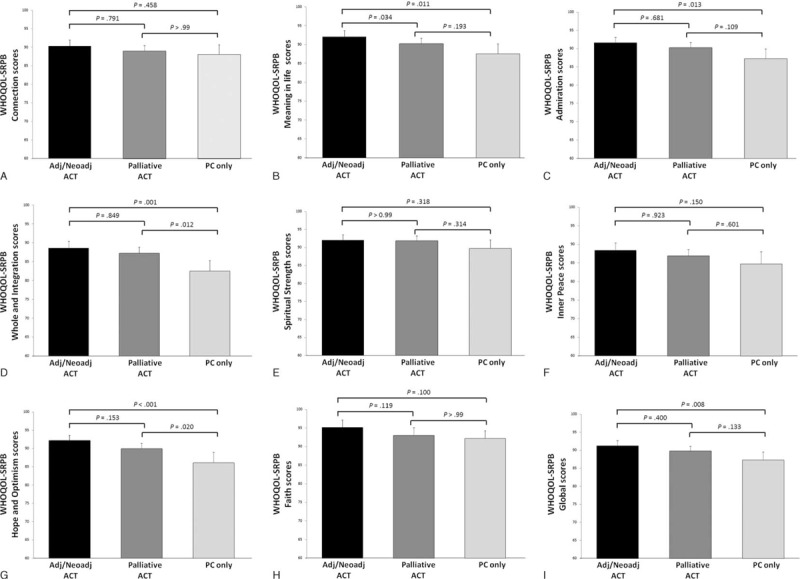
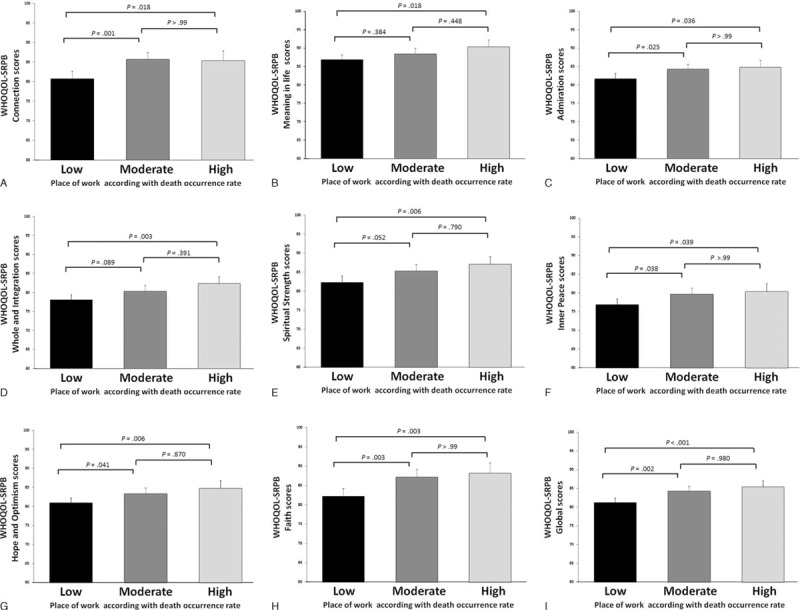
To better understand differences between patients and health professionals, subgroup analyses were performed. The spiritual QOL scores were compared between patients undergoing different treatment modalities. In general, patients undergoing curative treatments (adjuvant and neoadjuvant treatments) reported higher spiritual QOL scores than those receiving palliative care only (Table 6 and Figure 1). Regarding the health professionals, comparisons were made among 3 categories of workplace according to the probability of dealing with a new patient's death. Interestingly, professionals working in Palliative Care and the Intensive Care Unit reported higher scores of spiritual QOL than those working in places where death occurrence is a rare event (Table 7 and Figure 2).
TABLE 6.
Mean Scores of Spiritual Quality of Life of Cancer Patients According With the Different Types of Cancer Treatments
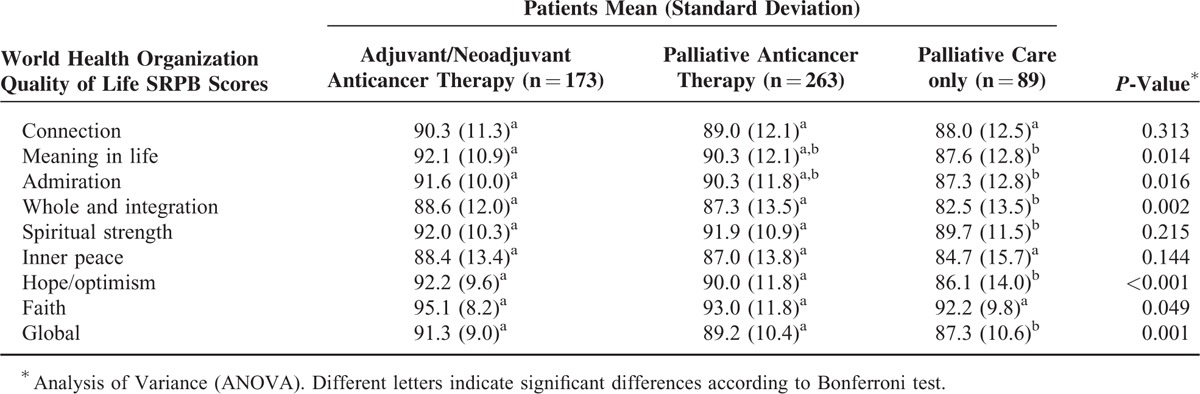
FIGURE 1.
Mean scores of spiritual quality of life of cancer patients according with the different types of cancer treatments. Patients with cancer were categorized into 3 groups of treatments: adjuvant/neoadjuvant anticancer treatment, palliative anticancer treatment, or palliative care only. Mean scores of different domains of WHOQOL-SRPB reported by the cancer patients are shown: (A) connection, (B) meaning in life, (C) admiration, (D) whole and integration, (E) spiritual strength, (F) inner peace, (G) hope and optimism, (H) faith, and (I) global. Errors bars indicate 95% confidence intervals. P-values were obtained using Bonferroni multiple comparison test.
TABLE 7.
Mean Scores of Spiritual Quality of Life of Health Professionals According With the Different Workplaces
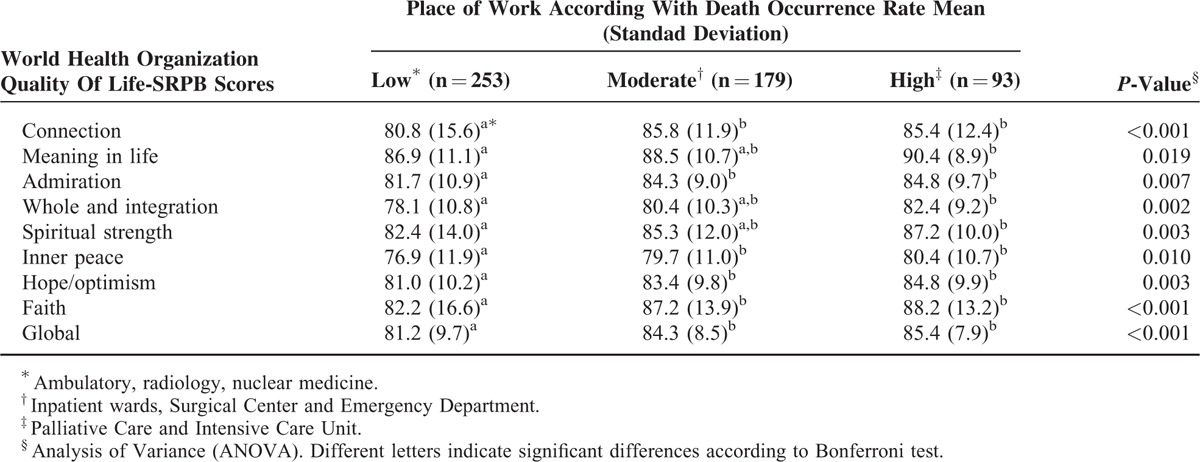
FIGURE 2.
Mean scores of spiritual quality of life of health professionals according to the different workplaces. Health professionals were categorized into 3 groups of different places of work: low (ambulatory, radiology, nuclear medicine), moderate (inpatient wards, Surgical Center and Emergency Department), and high (Palliative Care and Intensive Care Unit) according with death occurrence rate. Mean scores of different domains of WHOQOL-SRPB reported by the health professionals are shown: (A) connection, (B) meaning in life, (C) admiration, (D) whole and integration, (E) spiritual strength, (F) inner peace, (G) hope and optimism, (H) faith, and (I) global. Errors bars indicate 95% confidence intervals. P-values were obtained using Bonferroni multiple comparison test.
Based on our findings, a conceptual framework was developed (Figure 3).
FIGURE 3.
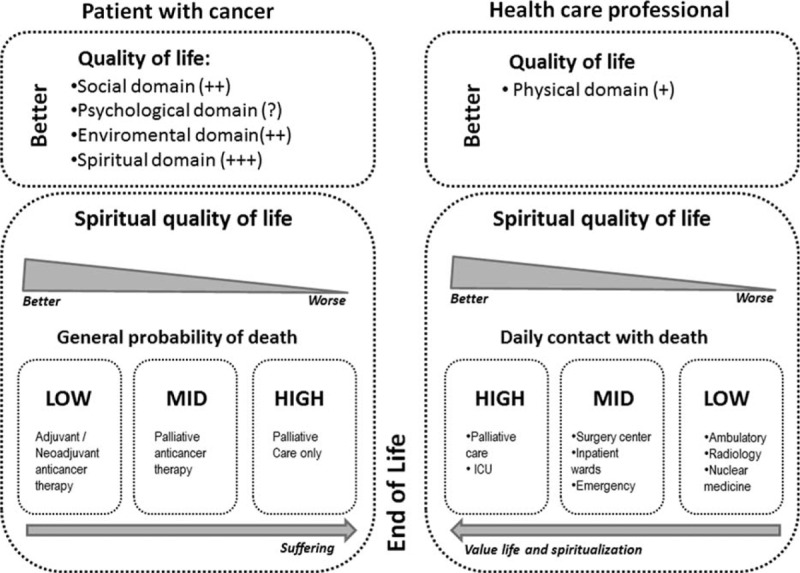
Conceptual framework of the study findings. Better quality of life scores observed in the group of (A) cancer patients and (B) health professionals. C, Relationship between spiritual quality of life in patients with cancer in view of the treatment received. The higher the possibility of death (end of life), the lower the spiritual quality of life scores. D, Relationship between spiritual quality of life in the health care professional group in view of the workplace. The higher the daily contact with death (patients at the end of life), the higher the quality of spiritual life scores. Supplemental Figure. Flowchart of study recruitment.
DISCUSSION
In this study, we evaluated the QOL of cancer patients and health professionals and observed a positive correlation between spiritual QOL and the other domains of QOL. As expected, patients exhibited lower physical QOL. Conversely, contrary to our initial predictions, patients reported clinically significantly better social, environmental, and global QOL, and a trend toward better psychologic QOL. More importantly, patients reported consistently higher spiritual QOL scores in comparison with health professionals.
In the current study, all patients and 96.8% of health professionals believed in God. All questions that investigated the importance of S/R in oncology practice received over 90% positive replies for both patients and health professionals. Both groups reported that S/R helped them in their personal and professional lives, and the participants ascribed importance to having religious affiliations, to participating in religious activities, and to praying individually or in a group. The religion and spirituality in Cancer Care Study evaluated 75 patients with advanced cancer and 339 health professionals (doctors and nurses) in multiple centers. Most patients (77.9%), doctors (71.6%), and nurses (85.1%) believed that spiritual care could be beneficial to patients. Only 25% of the patients, however, had received this type of care previously.37 In another study, 91% of hospitalized patients reported some spiritual need.38 Typically, spiritual care is offered by skilled health professionals, by the religious community to which the patient belongs, and by hospital chaplains. Among patients with advanced cancer, receiving spiritual care through religious organizations was associated with more aggressive care at the final stage of life, with decreased hospice use and more Intensive Care Unit admissions. Conversely, among patients with good spiritual support offered by religious communities, additional spiritual care by the medical team was associated with fewer invasive and unnecessary procedures during the final stage of life.39 In agreement with the findings of the current study, patients considered it important that the spiritual and religious dimensions be addressed by health professionals.10,21–23 The best strategy to address these dimensions and benefit patients, however, remains to be defined.
Previous studies demonstrated that patients and professionals seek spiritual and religious resources to improve their QOL.9,11,16,27 A Danish study investigated 1043 oncology patients to assess the extent to which faith and spiritual well being were associated with psychologic distress. Higher spiritual well being was associated with less distress and greater adaptation to the disease.14 A North American multicenter study evaluated S/R and religious coping in 69 patients with advanced cancer and found that 84% of individuals used religious and spiritual beliefs to cope with the disease; in the multivariate analysis, religious coping was associated with better QOL.16 Spirituality/religiosity has been observed as a source of support, adaptation, coping, comfort, strength, and well being during the course of disease and treatment.11,17,19
Several studies identified a positive impact of S/R on individuals’ health, especially in the physical and mental domains.20,40,41 Measures of S/R have been found to be negatively associated with cardiac diseases, hypertension, hypercholesterolemia, depression, suicidal ideation, substance abuse, risky sexual behaviors, and mortality within large population studies.40,42 Furthermore, patients with advanced cancer who reported praying more often exhibited higher overall survival and lower levels of inflammatory serum markers.43 Among the possible explanations, it is believed that participation in religious activities may push the individual to healthier behavioral practices40 and may promote better social support.13 Spirituality/religiosity also appears to influence physiologic processes related to cardiovascular, neuroendocrine, and immunologic systems, promoting health benefits for individuals.20,40,42 Paiva et al44 reported a negative association between religiosity and QOL in their study of women with breast cancer who started adjuvant chemotherapy. They suggested that patients with worse QOL use religiosity more often as a way of coping with cancer. Another explanation could be that highly religious persons may have distinct spiritual needs and concerns contributing to a worse QOL. The most accepted hypothesis, however, is that S/R is associated with a better QOL,45 where one of the likely mediating mechanisms is the stimulus of a feeling of greater autonomy in life.46
Our results differed from our initial hypothesis, as we believed that patients would exhibit significantly lower QOL scores compared with professionals (considered in our study to be representative controls of the healthy population). Although patients reported lower physical QOL scores than professionals, the former unexpectedly reported higher scores on social relationships and environmental domains in comparison with the professionals. One question from the social domain of WHOQOL-Bref addresses social relationships, and the other investigates satisfaction with the support they received from their friends. The diagnosis and/or treatment of a potentially serious disease, such as cancer, may produce significant changes in the patient's life.47,48 Usually, there is an approximation of patients and their families/friends, which may induce more effective coping strategies and better satisfaction in relation to their social life and environment.49,50 After the diagnosis of a potentially life-threatening disease, such as cancer, patients with advanced cancer seek meaning in life, and we postulate that they may be less likely to be bothered by everyday minor situations that used to affect their environmental QOL in the past. In addition, most evaluated patients were work inactive, probably living closer to their families, and spending more time at home. A previous Brazilian study showed that nurse technicians (half of the investigated professionals in our sample) excessively dedicate themselves to professional activities, which negatively interferes with the time available for rest, leisure, and time spent with their own families.51
Individuals with cancer, as well as those with any other life-threatening disease, frequently use some form of S/R to meet increased needs for meaning and purpose. This becomes more evident when considering those patients approaching the end of life.16,52,53 In the current study, both investigated groups reported high spiritual QOL scores; however, patients had significantly higher scores than professionals in all the spiritual QOL evaluated domains. Positive correlations between spiritual QOL domain scores and the other domains of QOL were observed, which was most evident in relation to the psychologic domain. After excluding the effects of the other spiritual domains, significant correlations however, were observed, mainly regarding whole and integration, inner peace and hope and optimism. In general, the relationship between global spiritual QOLs and the other domains of QOL were stronger in patients than in health professionals. Along the illness process, cancer patients become closer to God, acquire more faith, and then start to feel spiritually stronger. The diagnosis of cancer may promote posttraumatic growth in some patients and they describe spirituality as one of these positive changes.47 To the best of our knowledge, no study has compared spiritual QOL scores between patients and health professionals.
Religious coping can be an important factor influencing the QOL of patients with cancer.16,53 Thus, atheists are expected to report lower spiritual QOL than religious people. Indeed, they presented significantly lower levels of spiritual QOL than the religious participants in the regression analyses. Our findings are in accordance with previous studies that found a low prevalence of religious nonbelievers among patients with cancer 54,55 and also among health care professionals.26,56,57 This low rate of atheists and other nonbelievers has hindered the conduction of detailed studies focusing on this uncommon population.
Several studies have shown that individuals who are confronted with death situations change their personal values.58,59 In a previous study,60 health professionals working in palliative care were compared with a group of health professionals working in maternity wards to investigate how daily experiences of the transience of life influence professionals’ values, meaning in life, and religiousness. Among other findings, palliative care health professionals were significantly more religious than other health professionals. The authors suggested that it could be more a question of choice of working environment than a real secondary modification. However, in our study, it is not possible to exclude the possibility of an effect of changing life values on care for patients with terminal diseases. Regardless, we believe that health professionals’ attitudes toward death can influence their life views, personal values, and priorities. Our research adds new data that support the findings of the aforementioned study.60 Considering that all health professionals work at the same hospital and are dedicated solely to patients with cancer, the observed differences in S/R are probably related to the daily contact with death (the most obvious difference between the groups of health professionals). With regards to the patients with cancer, we observed that they reported worse spiritual QOL in advanced clinical stages than those patients with early clinical stages, probably because they were undergoing a period with a high burden of emotional and physical symptoms. It is important to note that patients receiving palliative anticancer treatment reported intermediate values of spiritual QOL, suggesting a decrease in spiritual QOL scores over time, as the patient becomes aware about his/her incurable disease. It is well known that approximately 90% of patients with advanced cancers refer distressing spiritual struggles and seeking spirituality;38,61 unfortunately, these spiritual needs are often supported minimally or not at all by the medical system,62 potentially influencing the spiritual QOL in a negative way.
Strengths and Improvements Over Previous Studies
Previous studies have assessed the S/R of cancer patients 14,16,54,38 and health professionals 26,63,64 separately. Very few studies, 22,37,65 however, have made direct comparisons between patients with cancer and oncology health care professionals with regards to different aspects of S/R. Thus, we believe that our detailed assessment of the differences between patients and professionals concerning S/R provides new clinical information that might be potentially useful for the design of effective spiritual care protocols in daily practice. A large cross-sectional Danish study 14 has measured the S/R of cancer patients who had completed treatment and had an expected survival of at least 6 months, thus excluding patients undergoing palliative care were excluded. Several other studies evaluated S/R reported by patients with advanced cancers under palliative care.16,38,52 Therefore, one of the strengths of our study is that we have evaluated patients at different phases of cancer care within the cancer continuum, which enabled us to compare S/R scores reported by patients according to their perceived risks of death because of cancer. Of note, a previous prospective study 66 has evaluated physical–psychologic–social–spiritual/existential dimensions and overall QOL scores of 313 cancer patients in their last year of life. They could characterize trajectories of the multidimensional dying experience. Among other findings, posttraumatic growth declined gradually at 1 and 4 months before death, and perceived sense of burden to others increased steadily during the last year of life. Our findings that spiritual QOL scores are lower in patients with higher risk of imminent death (under palliative care only) in comparison with patients who might probably be cured, are in agreement with those reported by Tang et al.66 Unlike our study, they, however, did not measure S/R using standard instruments; they considered posttraumatic growth and burden to others as dimensions of S/R.
Limitations of the Study
The current study has some limitations. First, we were unable to match each patient to their own health professional. Therefore, we were unable to identify whether the spiritual needs of the patients were properly addressed and whether they were effectively included in the provided care. This study design, however, would not have been feasible considering the sample size and the technical difficulties in interviewing participants in a paired manner. Another limitation of the research was that the vast majority of both populations comprised practitioners and individuals affiliated with a religion, with rare cases of atheist participants; thus, it is difficult to generalize our results to populations with different characteristics and cultures.
CONCLUSIONS
Spirituality/religiosity is an important construct in the minds of cancer patients and of health professionals who are involved in the care of cancer patients. Both groups claimed that S/R should be included in a holistic approach to the patient. Furthermore, the participants reported that S/R helped them face problems. A positive correlation between spiritual QOL levels and other QOL domains was observed. Patients exhibited higher spiritual QOL scores compared with health professionals. Considering the importance of S/R in the patient-health professional binomial, further studies are needed to determine how health professionals may effectively address S/R in oncology practice.
Acknowledgments
The authors would like to thank the statistician Cleyton Zanardo de Oliveira for assistance with the sample size estimation and also American Journal of Experts and Ms. Cláudia Serrano for English editing.
Footnotes
Abbreviations: ECOG-PS = Eastern Cooperative Oncology Group performance status, QOL = quality of life, S/R = spirituality/religiosity, WHO = World Health Organization.
This project was supported by the Barretos Cancer Hospital internal research funds (PAIP).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med 1995; 41:1403 L-1409.http://www.ncbi.nlm.nih.gov/pubmed/8560308http://www.ncbi.nlm.nih.gov/pubmed/8560308. Accessed February 11, 2015. [DOI] [PubMed] [Google Scholar]
- 2.Kuyken W, Orley J. Development of the WHOQOL: rationale and current status. Int J Ment Health 1994; 23:24–56. [Google Scholar]
- 3.Minayo MC, Hartz ZM, Buss PM. Quality of life and health: a necessary debate. Ciên Saúde Colet 2000; 5:7–18. [Google Scholar]
- 4.Fallowfield L. Quality of life: a new perspective for cancer patients. Nat Rev Cancer 2002; 2:873–879. [DOI] [PubMed] [Google Scholar]
- 5.Lee RT, Seo B, Hladkyj S, et al. Correlates of physician burnout across regions and specialties: a meta-analysis. Hum Resour Health 2013; 11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suñer-Soler R, Grau-Martín A, Font-Mayolas S, et al. Burnout and quality of life among Spanish healthcare personnel. J Psychiatr Ment Health Nurs 2013; 20:305–313. [DOI] [PubMed] [Google Scholar]
- 7.Tanriverdi O. A medical oncologist's perspective on communication skills and burnout syndrome with psycho-oncological approach (to die with each patient one more time: the fate of the oncologists). Med Oncol 2013; 30:530. [DOI] [PubMed] [Google Scholar]
- 8.O’Connell KA, Skevington SM. To measure or not to measure? Reviewing the assessment of spirituality and religion in health-related quality of life. Chronic Illn 2007; 3:77–87. http://www.ncbi.nlm.nih.gov/pubmed/18072699http://www.ncbi.nlm.nih.gov/pubmed/18072699. Accessed April 20,2015. [DOI] [PubMed] [Google Scholar]
- 9.O’Connell KA, Skevington SM. The relevance of spirituality, religion and personal beliefs to health-related quality of life: themes from focus groups in Britain. Br J Health Psychol 2005; 10:379–398. [DOI] [PubMed] [Google Scholar]
- 10.Surbone A, Baider L. The spiritual dimension of cancer care. Crit Rev Oncol Hematol 2010; 73:228–235. [DOI] [PubMed] [Google Scholar]
- 11.Peteet JR, Balboni MJ. Spirituality and religion in oncology. CA Cancer J Clin 2013; 63:280–289. [DOI] [PubMed] [Google Scholar]
- 12.El Nawawi NM, Balboni MJ, Balboni TA. Palliative care and spiritual care: the crucial role of spiritual care in the care of patients with advanced illness. Curr Opin Support Palliat Care 2012; 6:269–274. [DOI] [PubMed] [Google Scholar]
- 13.Rocha N, Fleck M. Evaluation of quality of life and importance given to spirituality/religiousness/personal beliefs (SRPB) in adults with and without chronic health conditions. Rev Psiquiatr Clín 2011; 38:19–23. [Google Scholar]
- 14.Johannessen-Henry CT, Deltour I, Bidstrup PE, et al. Associations between faith, distress and mental adjustment: a Danish survivorship study. Acta Oncol 2013; 52:364–371. [DOI] [PubMed] [Google Scholar]
- 15.Koenig HG, Larson DB, Larson SS. Religion and coping with serious medical illness. Ann Pharmacother 2001; 35:352–359. http://wwwncbinlmnihgov/pubmed/11261534http://wwwncbinlmnihgov/pubmed/11261534 Accessed April 1 2015. [DOI] [PubMed] [Google Scholar]
- 16.Vallurupalli M, Lauderdale K, Balboni MJ, et al. The role of spirituality and religious coping in the quality of life of patients with advanced cancer receiving palliative radiation therapy. J Support Oncol 2012; 10:81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wildes KA, Miller AR, de Majors SS, et al. The religiosity/spirituality of Latina breast cancer survivors and influence on health-related quality of life. Psychooncology 2009; 18:831–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramondetta L, Brown A, Richardson G, et al. Religious and spiritual beliefs of gynecologic oncologists may influence medical decision making. Int J Gynecol Cancer 2011; 21:573–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atef-Vahid M-K, Nasr-Esfahani M, Esfeedvajani MS, et al. Quality of life, religious attitude and cancer coping in a sample of Iranian patients with cancer. J Res Med Sci 2011; 16:928–937. http://wwwpubmedcentralnihgov/articlerenderfcgi?artid=3263107&tool=pmcentrez&rendertype=abstract Accessed April 20 2015. [PMC free article] [PubMed] [Google Scholar]
- 20.Koenig HG. Religion, spirituality and health: the research and clinical implications. ISRN Psychiatry 2012; 2012:1–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor EJ. Nurses caring for the spirit: patients with cancer and family caregiver expectations. Oncol Nurs Forum 2003; 30:585–590. [DOI] [PubMed] [Google Scholar]
- 22.Balboni MJ, Sullivan A, Amobi A, et al. Why is spiritual care infrequent at the end of life? Spiritual care perceptions among patients, nurses, and physicians and the role of training. J Clin Oncol 2013; 31:461–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berg GM, Whitney MP, Wentling CJ, et al. Physician assistant program education on spirituality and religion in patient encounters. J Physician Assist Educ 2013; 24:24–27.Accessed April 20, 2015. [DOI] [PubMed] [Google Scholar]
- 24.Banin LB, Suzart NB, Banin VB, et al. Spirituality: do teachers and students hold the same opinion? Clin Teach 2013; 10:3–8. [DOI] [PubMed] [Google Scholar]
- 25.Nixon AV, Narayanasamy A, Penny V. An investigation into the spiritual needs of neuro-oncology patients from a nurse perspective. BMC Nurs 2013; 12:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodin D, Balboni M, Mitchell C, et al. Whose role? Oncology practitioners’ perceptions of their role in providing spiritual care to advanced cancer patients. Support Care Cancer 2015; 23:2543–2550. [DOI] [PubMed] [Google Scholar]
- 27.Khorami Markani A, Yaghmaei F, Khodayari Fard M. Spirituality as experienced by Muslim oncology nurses in Iran. Br J Nurs 2013; 22:S26–S28. http://www.ncbi.nlm.nih.gov/pubmed/23448951http://www.ncbi.nlm.nih.gov/pubmed/23448951. Accessed April 20, 2015. [DOI] [PubMed] [Google Scholar]
- 28.Panzini RG, Maganha C, Rocha NS. Brazilian validation of the Quality of Life Instrument/spirituality, religion and personal beliefs. Rev Saude Publica 2011; 45:153–165. http://www.ncbi.nlm.nih.gov/pubmed/21181054http://www.ncbi.nlm.nih.gov/pubmed/21181054. Accessed April 20, 2015. [DOI] [PubMed] [Google Scholar]
- 29.Den Oudsten BL, Zijlstra WP, De Vries J. The minimal clinical important difference in the World Health Organization Quality of Life instrument: 100. Support Care Cancer 2013; 21:1295–1301. [DOI] [PubMed] [Google Scholar]
- 30.Whitley E, Ball J. Statistics review 4: sample size calculations. Crit Care 2002; 6:335–341. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=137461&tool=pmcentrez&rendertype=abstracthttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=137461&tool=pmcentrez&rendertype=abstract. Accessed June 16, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc Sci Med 1998; 46:1569–1585. http://www.ncbi.nlm.nih.gov/pubmed/9672396http://www.ncbi.nlm.nih.gov/pubmed/9672396. Accessed April 20, 2015. [DOI] [PubMed] [Google Scholar]
- 32.WHOQOL SRPB Group. A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Soc Sci Med 2006; 62:1486–1497. [DOI] [PubMed] [Google Scholar]
- 33.WHO. WHOQOL User Manual. 1998; Geneva, Switzerland: World Health Organization, Program on Mental Health. [Google Scholar]
- 34.WHO. WHOQOL-SRPB User Manual. Scoring and Coding for the WHOQOL SRPB Field-Test Instrument. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 35.Koenker R, Bassett G., Jr Regression quantiles. Econometrica 1978; 46:33–50. [Google Scholar]
- 36.Fayers P, Machin D. Quality of life: the assessment, analysis and interpretation of patient-reported outcomes. Second edChinchester Uinted Kingdom: John Wiley and Sons; 2007. [Google Scholar]
- 37.Phelps AC, Lauderdale KE, Alcorn S, et al. Addressing spirituality within the care of patients at the end of life: perspectives of patients with advanced cancer, oncologists, and oncology nurses. J Clin Oncol 2012; 30:2538–2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pearce MJ, Coan AD, Herndon JE, et al. Unmet spiritual care needs impact emotional and spiritual well-being in advanced cancer patients. Support Care Cancer 2012; 20:2269–2276. [DOI] [PubMed] [Google Scholar]
- 39.Balboni TA, Balboni M, Enzinger AC, et al. Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Intern Med 2013; 173:1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seybold KS. Physiological mechanisms involved in religiosity/spirituality and health. J Behav Med 2007; 30:303–309. [DOI] [PubMed] [Google Scholar]
- 41.Konopack JF, McAuley E. Efficacy-mediated effects of spirituality and physical activity on quality of life: a path analysis. Health Qual Life Outcomes 2012; 10:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seeman TE, Dubin LF, Seeman M. Religiosity/spirituality and health. A critical review of the evidence for biological pathways. Am Psychol 20035; 58:53–63. http://www.ncbi.nlm.nih.gov/pubmed/12674818http://www.ncbi.nlm.nih.gov/pubmed/12674818. Accessed March 26, 2015. [DOI] [PubMed] [Google Scholar]
- 43.Paiva CE, Paiva BSR, Yennurajalingam S, et al. The impact of religiosity and individual prayer activities on advanced cancer patients’ health: is there any difference in function of whether or not receiving palliative anti-neoplastic therapy? Jo Relig Health 2013. 1–11. [DOI] [PubMed] [Google Scholar]
- 44.Paiva CE, Paiva BSR, de Castro RA, et al. A pilot study addressing the impact of religious practice on quality of life of breast cancer patients during chemotherapy. J Relig Health 2013; 52:184–193. [DOI] [PubMed] [Google Scholar]
- 45.Hunter-Hernández M, Costas-Muñíz R, Gany F. Missed opportunity: spirituality as a bridge to resilience in Latinos with cancer. J Relig Health 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Macilvaine WR, Nelson LA, Stewart JA, et al. Association of strength of religious adherence to quality of life measures. Complement Ther Clin Pract 2013; 19:251–255. [DOI] [PubMed] [Google Scholar]
- 47.Connerty TJ, Knott V. Promoting positive change in the face of adversity: experiences of cancer and post-traumatic growth. Eur J Cancer Care (Engl) 2013; 22:334–344. [DOI] [PubMed] [Google Scholar]
- 48.Barskova T, Oesterreich R. Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: a systematic review. Disabil Rehabil 2009; 31:1709–1733. [DOI] [PubMed] [Google Scholar]
- 49.Tan M. Social support and coping in Turkish patients with cancer. Cancer Nurs 2007; 30:498–504. [DOI] [PubMed] [Google Scholar]
- 50.Naseri N, Taleghani F. Social support in cancer patients referring to Sayed Al-Shohada hospital. Iran J Nurs Midwifery Res 2012; 17:279–283. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3702147&tool=pmcentrez&rendertype=abstracthttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3702147&tool=pmcentrez&rendertype=abstract. Accessed April 21, 2015. [PMC free article] [PubMed] [Google Scholar]
- 51.Silva AA, Rotenberg L, Fischer FM. Nursing work hours: individual needs versus working conditions. Rev Saude Publica 2011; 45:1117–1126.Accessed April 21, 2015. [DOI] [PubMed] [Google Scholar]
- 52.King M, Llewellyn H, Leurent B, et al. Spiritual beliefs near the end of life: a prospective cohort study of people with cancer receiving palliative care. Psychooncology 2013; 22:2505–2512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Delgado-Guay MO. Spirituality and religiosity in supportive and palliative care. Curr Opin Support Palliat Care 2014; 8:308–313. [DOI] [PubMed] [Google Scholar]
- 54.Miccinesi G, Proserpio T, Pessi MA, et al. Is the spiritual life of cancer patients a resource to be taken into account by professional caregivers from the time of diagnosis? Tumori 2012; 98:158–161. [DOI] [PubMed] [Google Scholar]
- 55.Tarakeshwar N, Vanderwerker LC, Paulk E, et al. Religious coping is associated with the quality of life of patients with advanced cancer. J Palliat Med 2006; 9:646–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Curlin FA, Lantos JD, Roach CJ, et al. Religious characteristics of U.S. physicians: a national survey. J Gen Intern Med 2005; 20:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lucchetti G, Ramakrishnan P, Karimah A, et al. Spirituality, religiosity, and health: a comparison of physicians’ attitudes in Brazil, India, and Indonesia. Int J Behav Med 2015. [DOI] [PubMed] [Google Scholar]
- 58.Goldenberg JL, Arndt J. The implications of death for health: a terror management health model for behavioral health promotion. Psychol Rev 2008; 115:1032–1053. [DOI] [PubMed] [Google Scholar]
- 59.Niemiec CP, Brown KW, Kashdan TB, et al. Being present in the face of existential threat: the role of trait mindfulness in reducing defensive responses to mortality salience. J Pers Soc Psychol 2010; 99:344–365. [DOI] [PubMed] [Google Scholar]
- 60.Fegg M, L’hoste S, Brandstätter M, et al. Does the working environment influence health care professionals’ values, meaning in life and religiousness? Palliative care units compared with maternity wards. J Pain Symptom Manage 2014; 48:915–923. [DOI] [PubMed] [Google Scholar]
- 61.Winkelman WD, Lauderdale K, Balboni MJ, et al. The relationship of spiritual concerns to the quality of life of advanced cancer patients: preliminary findings. J Palliat Med 2011; 14:1022–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Balboni TA, Vanderwerker LC, Block SD, et al. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol 2007; 25:555–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ramondetta LM, Sun C, Surbone A, et al. Surprising results regarding MASCC members’ beliefs about spiritual care. Support Care Cancer 2013; 21:2991–2998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Balboni MJ, Sullivan A, Enzinger AC, et al. Nurse and physician barriers to spiritual care provision at the end of life. J Pain Symptom Manage 2014; 48:400–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Balboni MJ, Babar A, Dillinger J, et al. It depends”: viewpoints of patients, physicians, and nurses on patient-practitioner prayer in the setting of advanced cancer. J Pain Symptom Manage 2011; 41:836–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tang ST, Liu LN, Lin KC, et al. Trajectories of the multidimensional dying experience for terminally ill cancer patients. J Pain Symptom Manage 2014; 48:863–874. [DOI] [PubMed] [Google Scholar]


