Abstract
This study aimed to observe the therapeutic effects and adverse reactions of radiofrequency thermocoagulation combined with adriamycin injection in dorsal root ganglia on lung cancer rib metastasis-related refractory pain which has no response to conventional therapy.
This study contained 27 patients with lung cancer rib metastasis-related moderate or severe pain which had no response to conventional therapy. Under computed tomography (CT)-guidance, radiofrequency puncture need reached the corresponding intervertebral foramens to ensure needle point near dorsal root ganglia (DRG) by sensory and motor stimulation tests, and then radiofrequency thermocoagulation was performed on each corresponding DRG followed by injection of 0.5 to 1 mL of adriamycin (0.5%). The conditions of pain and complications were observed before management and 3 days, 1 month, and 3 months after management, respectively.
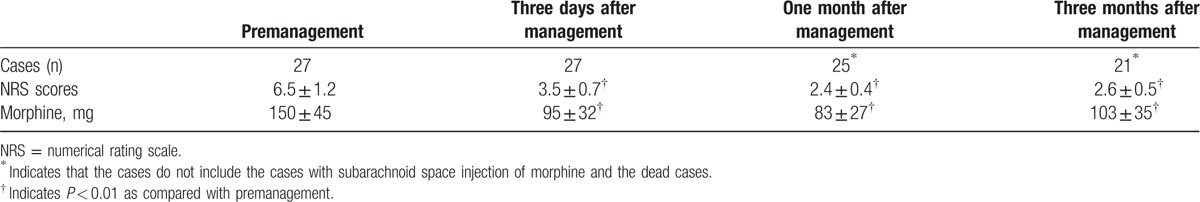
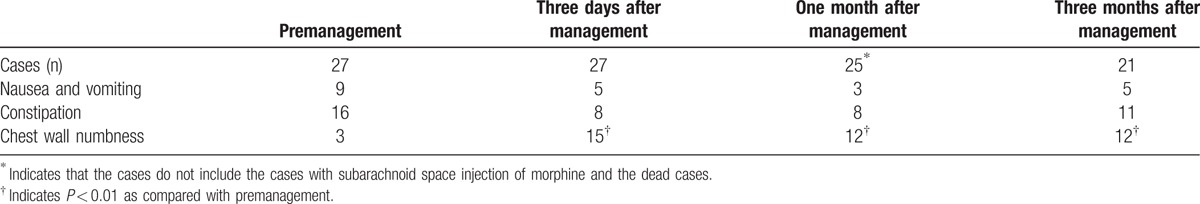
Numerical rating scale (NRS) scores and dosage of morphine were all significantly decreased after management as compared with those before management (all P < 0.01). Although the number of patients with chest wall numbness was significantly increased after management as compared with that before management (all P < 0.01), the degree of chest wall numbness was tolerable. There were no statistical differences between before and after management in nausea and vomiting, and constipation.
CT-guided radiofrequency thermocoagulation combined with adriamycin injection in DRG can effectively control lung cancer rib metastasis-related pain which has no response to conventional therapy. This combinatory treatment regimen is featured by better therapeutic effects and a few complications, so it is worthy of being recommended in clinical application.
Keywords: lung cancer, radiofrequency thermocoagulation, refractory pain, rib metastasis
1. Introduction
Rib is one of the most common sites of bone metastasis in the patients with lung cancer.[1] For some patients, even the application of radiotherapy, local treatment, bisphosphates and tri-ladder analgesia[2] is unable to control the neuropathic pain caused by tumor-induced intercostal nerve compression, the pain associated with tumor invasion-induced pathological fracture and pleural pain stimulated by invasive tumor growth. In recent years, by application of a new treatment regimen, radiofrequency thermocoagulation combined with adriamycin injection in thoracic dorsal root ganglia (DRG), we obtained better effects on controlling lung cancer rib metastasis-related pain in the patients who had no response to conventional managements. This study provides a new treatment option for rib metastasis-related refractory pain.
2. Materials and methods
All study methods were approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University and Henan Provincial Tumor Hospital. All patients gave written informed consent to participate in this study.
2.1. General data
A total of 27 patients aged 38 to 76 years including 15 men and 12 women that were treated in our hospital due to lung cancer rib metastasis between December 2013 and December 2015 were enrolled in this study. Of the 27 patients, 16 only had rib metastasis and the other 11 were also complicated with other organ metastasis. However, the main pain was all located in the affected thoracic ribs in these patients. The 27 patients all had moderate to severe pains of (6.5 ± 1.2) scores assessed by numerical rating scale (NRS). All patients received conventional managements including radiotherapy, local treatment, bisphosphates and tri-ladder analgesia, but they had no response to the conventional managements. The maximal dosage of analgesic drug was equivalent to 600 mg of morphine with a mean dosage of (150 ± 45) mg.
2.2. Methods
After patients were in side-lying position or prone position, computed tomography (CT)-guided localizations of the intervertebral foramens of the affected ribs, the upper and lower intervertebral foramens of the affected ribs, the skin puncture points and the puncture paths from the puncture points to the corresponding intervertebral foramens were performed. For instance, if metastasis occurred in the left T9 rib, the locations of left T8, T9, and T10 intervertebral foramens were required. After routine disinfection, covering sterile towels and local anesthesia with 1% lidocaine, the puncture was carried out using radiofrequency needles. When images confirmed that the needles reached the corresponding intervertebral foramens, radiofrequency electrode was applied for sensory and motor stimulation tests. The sensory stimulation was performed with an intensity of 0.1 to 1.0 mV, a frequency of 50 Hz and a wave width of 0.1 ms, while the parameters of motor stimulation test were 0.1 to 1.0 mV, 2 Hz, and 1 ms. The position and angle of radio-frequency needle point were adjusted to stimulate sensory and motor nerves. Less than 0.6 mV of both sensory and motor stimulus intensity could induce numbness, tingling, and sense of local jumping in the corresponding intercostal innervation areas, suggesting that the needle point had been close to DRG and the puncture was successful. The abnormal sensation could cover all pain regions in the chest after all tests were finished.
If no blood and cerebrospinal occurred after withdrawing plunger of the needle, 0.4 mL contrast agent and 0.1 mL of 2% lidocaine were injected through the corresponding intervertebral foramens. Subsequently, after CT scan confirmed that the radio-frequency needle points were located in the intervertebral foramens and no contrast agent diffused into the subarachnoid space and blood vessels, radiofrequency thermocoagulation was performed on each DRG. The maximum radiofrequency temperature was 75 to 85 °C and the duration was set as 360 to 480 s. After radiofrequency thermocoagulation, 0.5 to 1 mL of 5% adriamycin was slowly injected into each intervertebral foramen and the total dosage of adriamycin was less than 20 mg. Then, radiofrequency needles were slowly pulled out accompanied by the injection of 0.1 to 0.2 mL Diprospan to prevent nerve root inflammation caused by adriamycin reflux. After withdrawal of puncture needles, pressing hemostasis and covering the puncture point with clean dressing, the patients were sent back to the ward and monitored by electrocardiogram for 12 hours. If postoperative NRS was not more than 3 scores, opioid drugs were gradually decreased or even discontinued. If postoperative NRS was not less than 4 scores, the pain was controlled by adjustment of analgesic drugs or other minimally invasive analgesia until the NRS was not more than 3 scores. The treatment regimen for tumor remained unchanged.
2.3. Observation parameters
2.3.1. Pain
Pain was assessed by NRS. The dosages of morphine and the conditions of pain were recorded and observed before management and 3 days, 1 month, and 3 months after management, respectively. It was regarded as effective treatment that postoperative NRS was not more than 3 scores.
2.3.2. Complications
Complications such as hemopneumothorax, nausea and vomiting, constipation, chest wall numbness, and intraspinal injection were closely observed during and after management.
2.4. Statistical analysis
Statistical treatment was performed using SPSS 19.0 (Beijing, China). Measurement data were expressed as
 |
t Test was used for comparison between groups. Statistical significance was established as P < 0.05.
3. Results
3.1. Analgesia
Our results showed that in the 27 patients, postoperative NRS was not more than 3 scores in 20 patients 3 days after management with a total effective rate of 74.1%. The other 7 patients had poor pain relief because 5 patients required increased analgesics dosage and 2 patients required continuous subarachnoid space morphine injection to control NRS ≤3 scores.
One-month follow up indicated that in the 20 patients with effective pain control, except 4 patients requiring increased opioid dosage, others still had stable pain control. In the 5 patients with increased analgesics dosage, the pain was relieved and opioid dosage was also decreased in 2 patients, 1 patient had stable pain control and 2 patients required increased opioid dosage to maintain stable pain control. In the 2 patients with continuous subarachnoid space morphine injection, pain control was stable.
Three-month follow up indicated that in the 25 patients with drug-controlling pain, 15 patients had stable pain control, 6 patients required increased opioid dosage, 2 patients required continuous subarachnoid space morphine injection, and 2 patients died.
NRS scores and morphine dosages before and after management are shown in Table 1.
Table 1.
NRS scores and morphine dosages before and after management.
3.2. Complications
No severe complications such as hemopneumothorax and intraspinal injection occurred in all the 27 patients after managements. Three days, 1 month, and 3 months after managements, 15, 12, and 12 patients had tolerable degrees of chest wall numbness, respectively, without the requirement of particular treatment. The conditions of nausea and vomiting, and constipation are shown in Table 2.
Table 2.
Complications in these patients before and after management.
4. Discussion
Rib metastasis is common in patients with advanced lung cancer. Due to tumor invasion of rib and intercostal nerve, pathological fracture and pleural irritation etc., it is difficult for conventional treatment protocols such as radiotherapy, local treatment, bisphosphates and tri-ladder analgesia to control the pain. This seriously affects patients’ life quality.
DRG, ganglia in the dorsal root of spinal nerve, are generally located in the intervertebral foramens.[3] The DRG, acting as primary neurons, transfer and regulate organic sense, and accept and transmit nociception. It has been confirmed that blocking DRG has marked effects on the intractable pain caused by cancer.[4]
Radiofrequency thermocoagulation on DRG has been widely applied for the treatment of various chronic pains.[5,6] The corresponding area of sensory nerve is not able to regenerate after DRG injury, so the therapeutic effects of radiofrequency thermocoagulation are exact and constant. Radiofrequency thermocoagulation has been widely used in the control of pain caused by cancer. The thoracic DRGs have a variety of variations in size and position.[7] Therefore, the therapeutic effects of only radiofrequency thermocoagulation through the intervertebral foramina are not better because radiofrequency needle point may be away from the corresponding DRG. It has been reported that the effective rate of simple DRG radiofrequency is only about 25% to 55% for postherpetic neuralgia.[8,9]
Adriamycin possesses neurotoxicity which can induce DRG neuron necrosis.[10,11] Paravertebral injection of adriamycin can selectively act on DRG by axioplasm counterflow, blocking sensory conduction.[12] In paravertebral injection, needle point is likely to be away from DRG and the dosage and volume of adriamycin are small, these factors allow adriamycin difficultly to enter DRG, affecting therapeutic effects. Therefore, we used CT-guided DRG radiofrequency thermocoagulation through intervertebral foramens, followed by injection of adriacin. Because the sensory and motor tests had been performed previously, the needle point was usually close to the DRG and even a small amount of adriacin could act on DRG by direct dispersion, ensuring exact therapeutic effects. Paravertebral adriamycin injection and radiofrequency thermocoagulation was mutual supplements.
In this study, the effective rate was 74.1%, suggesting that CT-guided radiofrequency thermocoagulation combined with adriamycin injection in DRG was effective for controlling lung cancer rib metastasis-related pain which has no response to conventional treatment regiments. This combinatory treatment regimen is not only featured by small trauma, ideal pain relief, and long therapeutic effects, but also can greatly reduce the dosage of opioid, thereby reducing opioid adverse reactions. Although the combinatory treatment regimen increased the complication of chest wall numbness, the numbness was tolerable without the requirement of particular treatments. However, we also found that approximately 30% patients had poor therapeutic effects, and even some patients required elevation of opioid dosage to maintain stable pain control 1 month later or longer. These may be associated with the following factors. Firstly, besides the intercostal nerve, tumor invasion can also lead to rib-pathological fractures or pleura stimulation. The pain may caused by exercise factors and pleural stimulation. This may be the main reason for poor therapeutic effects. Secondly, the high variability of thoracic DRG in position and size easily leads to deviation of needle point from the DRG, resulting in incomplete coagulation.[5] Thirdly, the injected adriamycin is not confined to the periphery of intervertebral foramens, it can diffuse into vertebral canal or even the lateral intervertebral foramen. In this study, angiography before radiofrequency thermocoagulation showed that contrast media diffused into vertebral canal and even the lateral intervertebral foramen in some patients although the contrast media was only 0.5 mL. Fourthly, cancer progression is beyond the area that underwent thermocoagulation. Lastly, human bodies are likely to build up a tolerance to opioid as time goes on.
5. Conclusion
In summary, CT-guided radiofrequency thermocoagulation combined with adriamycin injection in DRG can effectively control lung cancer rib metastasis-related pain which has no response to conventional treatment protocols such as radiotherapy, local treatment, bisphosphates and tri-ladder analgesia. This combinatory treatment regimen is not only featured by small trauma, ideal pain relief, and long therapeutic effects, but also can greatly reduce the dosage of opioid, thereby reducing opioid adverse reactions. This combinatory treatment regimen is worthy of being recommended in clinical application.
Footnotes
Abbreviations: DRG = dorsal root ganglia, NRS = numerical rating scale.
The authors have no conflicts of interest to disclose.
References
- 1.Chen YQ, Yang Y, Xing YF, et al. Detection of rib metastases in patients with lung cancer: a comparative study of MRI, CT and bone scintigraphy. PLos One 2012; 7:5806–5819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsuya A, Fukuoka M. Bone metastases in lung cancer. Clin Calcium 2008; 18:455–459. [PubMed] [Google Scholar]
- 3.Li Z-p, Liu S-w. Clinical Anatomy on Central Nerve. 2nd ed.2009; Beijing: Science Press, 29–58. [Google Scholar]
- 4.Jiang Y-g, Xu L-h, Zhang H. The role of dorsal root ganglia in pain mechanism and treatment. Int J Pharma Res 2008; 35:18–22. [Google Scholar]
- 5.Vles GF, Vles JS, van Kleef M, et al. Percutaneous radiofrequency lesions adjacent to the dorsal root ganglion alleviate spasticity and pain in children with cerebral palsy: pilot study in 17 patients. BMC Neurol 2010; 10:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kapural L, Stojanovic M, Sessler DI, et al. Cooled radiofrequency (RF) of L5 dorsal ramus for RF denervation of the sacroiliac joint: technical report. Pain Med 2010; 11:53–57. [DOI] [PubMed] [Google Scholar]
- 7.Chen G-p, Zhang Y, Du Yong, et al. Preliminary study on the anatomy of thoracic spinal ganglion and its MR imaging. J Clin Radiol 2012; 31:1343–1348. [Google Scholar]
- 8.Bennett GJ, Watson CPN. Herpes zoster and postherpetic neuralgia: past, present and future. Pain Res Manag 2009; 14:275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim YH, Lee CJ, Lee SC, et al. Effect of pulsed radiofrequency for postherpetic neuralgia. Acta Anaesthesiol Scand 2008; 52:1140–1143. [DOI] [PubMed] [Google Scholar]
- 10.Han M-f, He Q-y, Ohnishi A. Changes in neurons of dorsal root ganglia and pores of cell nuclei in rats with adriacin poisoning. Chin J Neurol 2000; 33:156–158. [Google Scholar]
- 11.Liu J-z, Bo C-j, Li Q-b, et al. Effects of paravertebral injection of doxorubicin on behavior and ultrastructure of dorsal root ganglion neurons in rates with neuropathic pain. Chin J Anesthesiol 2012; 32:665–669. [Google Scholar]
- 12.Xu J-q, Zheng B-s, Xue Y-l, et al. Selective effect of paravertebral injection of adriacin on dorsal root ganglion in rabbits. Chin J Anesthesiol 2004; 24:714–715. [Google Scholar]


