Abstract
Background:
In a patient underwent aortic valve replacement (AVR) due to bicuspid aortic valve (BAV) insufficiency without marked dilation of ascending aorta, the development of delayed-typed aneurysmal complication of ascending aorta has been often reported because the dilated aorta tends to grow insidiously with age.
Case summary:
A 58-year-old man who underwent AVR with mechanical valve due to severe aortic regurgitation secondary to BAV 7 years previously presented with exertional chest discomfort for 1 year. An echocardiography showed a well-functioning mechanical aortic valve without any significant abnormal findings. Cardiac multidetector computed tomography (MDCT) revealed a huge saccular aortic root aneurysm (79.7 mm × 72.8 mm in size) compressing the proximal right coronary artery resulting in ∼90% eccentric diffuse luminal narrowing. The patient subsequently underwent open-heart surgery with resection of the ascending aortic aneurysmal sac and consecutive ascending aorta and hemi-arch replacement using a graft.
Conclusion:
After successful AVR in the patient with BAV insufficiency and mildly dilated ascending aorta, a regular aortic imaging such as cardiac MDCT with aortography would be helpful to monitor the morphology and size of ascending aorta and related complications to guide future management.
Keywords: aortic aneurysm, aortic valve replacement, bicuspid aortic valve, computed tomography, coronary artery
1. Introduction
Bicuspid aortic valve (BAV) is the most common congenital cardiac anomaly, occurring in 0.46% to 1.37% of the general population.[1] Aortic valve stenosis and regurgitation are the most common complications of BAV. Abnormalities of the aorta such as dilatation, bicuspid aortopathy, coarctation, cystic medial necrosis, and dissection are also often present in affected persons and can be potentially life threatening.[2–4] The prevalence of dilatation of the ascending aorta among persons with a bicuspid aortic valve is reported in anywhere from 20% to 84% of patients.[3] After successful aortic valve replacement (AVR) due to BAV insufficiency, the dilated aorta tends to grow insidiously with age compared to a normal tricuspid aortic valve.[5] Development of large, delayed-typed aneurysmal change following AVR has been previously reported.[6]
Hereby, we report a rare complicated case with an unusual type of aortic dilatation 7 years post-AVR that was performed in the setting of BAV insufficiency.
2. Case report
A 58-year-old man came to our outpatient department complaining of exertional dyspnea (NYHA class I or II/IV) and intermittent chest discomfort. The symptoms had developed insidiously over the past year. His chest pain and dyspnea had been getting progressively worse during the last 6 months. On physical examination, irregular heartbeats without significant murmur were noted.
Seven years ago, the patient had initially presented to our clinic complaining of exertional dyspnea (NYHA class II/IV). An initial transthoracic echocardiography demonstrated a BAV with severe aortic regurgitation but without significant calcification. The echocardiogram also demonstrated normal left ventricular systolic function (ejection fraction: 60%) with eccentric hypertrophy and loss of A wave due to atrial fibrillation. The diameter of the aortic root was measured to be 4.56 cm at that time. Invasive coronary angiography with aortography before surgery revealed no significant coronary luminal narrowing and a mildly dilated ascending aorta (Fig. 1 A and B). He underwent successful AVR using a mechanical prosthetic valve (Saint Jude #25) without additional aortic surgery.
Figure 1.
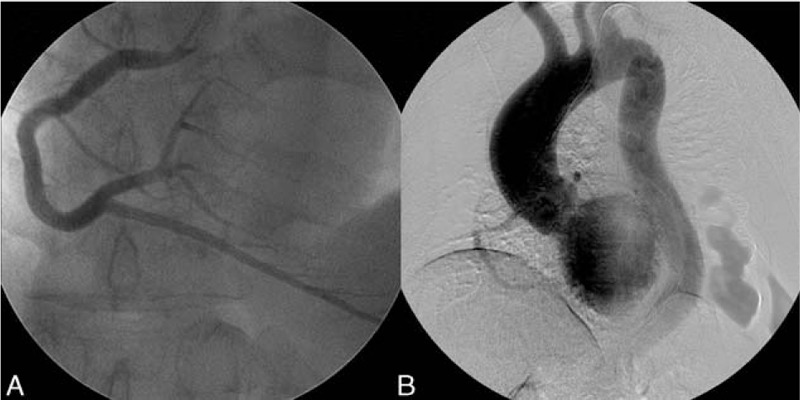
Preoperative coronary and aorta angiography. (A and B) Preoperative (November 2008) coronary artery and aorta angiography demonstrating a normal right coronary artery with a mildly dilated ascending aorta without significant aneurysmal change.
His current medications include warfarin 4 mg for stroke prevention from atrial fibrillation. His antihypertensive regimen included fimasartan 30 mg daily, nebivolol 2.5 mg daily, and indapamide 1.5 mg daily. He has been compliant with his medication regimen.
The patient's most recent ECG demonstrated atrial fibrillation with controlled ventricular response. A chest x-ray showed no cardiomegaly. A follow-up echocardiography demonstrated a well-functioning prosthetic aortic valve and normal left ventricular systolic and diastolic function.
In order to evaluate the cause of dyspnea with chest pain, a cardiac multidetector computed tomography (MDCT) was performed. Two-dimensional coronary cross-section images revealed a large saccular-typed ascending aortic aneurysm (79.7 mm × 72.8 mm in size) just distal to the prosthetic aortic valve annulus (Fig. 2 A and B). Curved multiplanar reformatted images also demonstrate diffuse, eccentric 90% luminal narrowing of the proximal right coronary artery (RCA) resulting from external compression by the aneuysmal sac. Also noted within the aneurysm was a low-density signal suggestive of mural hematoma or thrombi (Fig. 2C). Three-dimensional volume rendering images with coronary endoluminal and thrombotic settings confirmed compression of the proximal right coronary artery lumen by the aortic root aneurysm (Fig. 3A–F). The patient subsequently underwent open-heart surgery with resection of the ascending aortic aneurysmal sac and consecutive ascending aorta and hemi-arch replacement using a graft (Hemashield #28). The pathology of the resected aneurysmal sac demonstrated a vascular wall with myxoid degeneration and dystrophic calcification with organized thrombi. The patient's post-operative course was uncomplicated, and he has been doing well in outpatient follow-up. Informed consent was given by the patient.
Figure 2.
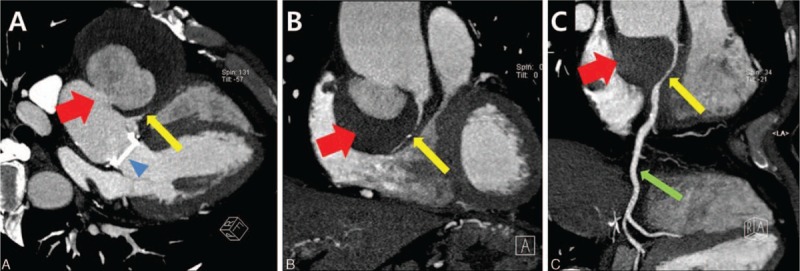
Cardiac MDCT 7 years after aortic valve replacement. (A and B) 2-dimensional coronal cross-section images demonstrate a large saccular aneurysm of the ascending aorta just distal to the previously replaced prosthetic valve (79.7 × 72.8 mm in size). It appears to contain mural thrombi or hematoma and is seen here compressing the proximal RCA. (C) Curved MPR image demonstrates the compressed proximal RCA by the large aneuysmal sac with mural low-density opacities suggesting thrombi or hematoma. ∗ aortic aneurysm with mural thrombi or intramural hematoma (red arrows); eccentrically compressed proximal RCA (yellow arrows); normal mid-RCA (green arrow); prosthetic aortic valve (blue arrow head). MDCT = multidetector computed tomography, MPR = muliplanar reformatting, RCA = right coronary artery.
Figure 3.
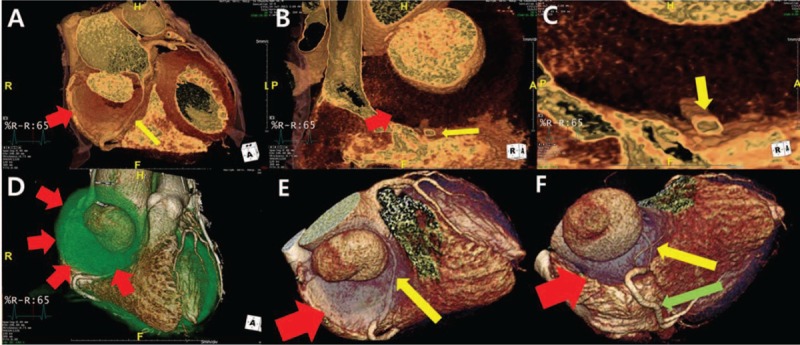
Cardiac MDCT 7 years after aortic valve replacement, (A–D) 3-dimensional volume rendering images demonstrate the saccular type of aneurysm with a narrow neck. The proximal RCA is externally compressed by theaneurysmal sac with mural thrombi or hematoma on endoluminal or thrombotic setting. (E and F) Normal mid-to-distal RCA. MDCT = multidetector computed tomography, RCA = right coronary artery. ∗aortic aneurysm with mural thrombi or intramural hematoma (red arrows); eccentrically compressed proximal RCA (yellow arrows); normal mid-RCA (green arrow); prosthetic aortic valve (blue arrow head).
3. Discussion
In a patient with BAV insufficiency including severe stenosis or regurgitation, AVR is usually recommended instead of valve repair according to the current valvular heart disease guidelines.[7]
Three different types of ascending aorta dilatation in the patient with BAV are known as follows; Type 1 is most common type and characterized by dilatation of tubular ascending aorta (primarily along convexity of aorta) with mild-to-moderate root enlargement. The patients with type 1 have an older age at diagnosis, higher incidence of aortic stenosis, and the right-left cusps fusion pattern. Type 2 is associated with arch dilatation and involvement of tubular ascending aorta, with relative sparing of root. It is usually accompanied by the right-noncoronary cusps fusion pattern. Type 3 involves aortic enlargement confined to aortic root with normal tubular ascending aorta and arch sizes.[3,8–9] This case demonstrates a saccular aneurysm which does not fall within the classic classification system based on the current literature. Furthermore, a large aneurysmal sac compressing the RCA appears to be a very rare and complicated presentation.
In patients with BAV and dilation of the aortic root or ascending aorta, surgical intervention to replace the aortic root and/or ascending aorta is determined by the aortic size according to current surgery guidelines. If the diameter of the aortic root or ascending aorta is >5.5 cm, prophylactic replacement of the ascending aorta is strongly recommended regardless of symptoms to avoid life-threatening aortic dissection. If the diameter of the aortic root or ascending aorta is >5.0 cm and the patient has risk factors for aortic dissection including rapid aortic growth rate (≥0.5 cm/y) and familial history of aortic dissection or if a skillful surgical team performs the procedures to the patient at low operative risk, surgical correction of the ascending aorta is also reasonable even in asymptomatic patients. Furthermore, for patients with BAV undergoing AVR because of severe aortic insufficiency, replacement of the ascending aorta is recommended if the diameter of the ascending aorta is >4.5 cm based on expert opinion of current guidelines. In these cases, close evaluation of the morphology and size of ascending aorta should be performed before operation.[7,10–13]
After successful AVR without replacement of the ascending aorta due to any cause in patients with BAV, aortic magnetic resonance angiography or computed tomography such as chest or cardiac MDCT with aortography is recommended to monitor the size and morphology of the ascending aorta. These evaluation should be performed annually especially in patients with an aortic diameter >4.5 cm after successful AVR according to expert recommendations,.[12]
This case suggests that the use of aortic and coronary imaging using cardiac MDCT may be helpful in elucidating less common causes of vague or unexplained chest discomfort and dyspnea in the absence of significant abnormalities on echocardiography after aortic valve surgery. This imaging modality may also help predict or prevent lethal aortic complications.
4. Conclusion
We present a rare case of huge saccular aneurysm compressing the RCA 7 years after AVR in a patient with BAV insufficiency. In a case of AVR without surgical repair or replacement of the ascending aorta due to any cause, cardiac MDCT with aorta and coronary angiography would be helpful to monitor the morphology and size of ascending aorta and to guide future management.
Footnotes
Abbreviations: AVF = aortic valve replacement, BAV = bicuspid aortic valve, MDCT = multidetector computed tomography, MPR = muliplanar reformatting, NYHA = New York Heart Association, RCA = right coronary artery.
The authors have no funding and conflicts of interest to disclose.
References
- 1.Tadros TM, Klein MD, Shapira OM. Ascending aortic dilatation associated with bicuspid aortic valve: pathophysiology, molecular biology, and clinical implications. Circulation 2009; 119:880–890. [DOI] [PubMed] [Google Scholar]
- 2.Yasuda H, Nakatani S, Stugaard M, et al. Failure to prevent progressive dilation of ascending aorta by aortic valve replacement in patients with bicuspid aortic valve: comparison with tricuspid aortic valve. Circulation 2003; 108 suppl 1:II291–II1294. [DOI] [PubMed] [Google Scholar]
- 3.Verma S, Siu SC. Aortic dilatation in patients with bicuspid aortic valve. N Engl J Med 2014; 370:1920–1929. [DOI] [PubMed] [Google Scholar]
- 4.Huang S, Sun JP, Sun Z, et al. Bicuspid aortic valve complicated by pseudo-aneurysm of aortic root abscess. Int J Cardiol 2016; 209:275–277. [DOI] [PubMed] [Google Scholar]
- 5.Nistri S, Sorbo MD, Marin M, et al. Aortic root dilatation in young men with normally functioning bicuspid aortic valves. Heart 1999; 82:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Göncü T, Sezen M, Ari H, et al. Delayed presentation of a giant ascending aortic aneurysm following aortic valve replacement. Case Rep Med 2009; 2009:740247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients with Thoracic Aortic Disease Representative Members, Hiratzka LF, Creager MA, Isselbacher EM, Svensson LG; 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease Representative Members, Nishimura RA, Bonow RO, Guyton RA, Sundt TM 3rd; ACC/AHA Task Force Members, Halperin JL, Levine GN, Anderson JL, Albert NM, Al-Khatib SM, Birtcher KK, Bozkurt B, Brindis RG, Cigarroa JE, Curtis LH, Fleisher LA, Gentile F, Gidding S, Hlatky MA, Ikonomidis J, Joglar J, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Wijeysundera DN. Surgery for Aortic Dilatation in Patients With Bicuspid Aortic Valves: A Statement of Clarification From the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2016;133:680–686. [Google Scholar]
- 8.Ridley CH, Vallabhajosyula P, Bavaria JE, et al. The sievers classification of the bicuspid aortic valve for the perioperative echocardiographer: the importance of valve phenotype for aortic valve repair in the era of the functional aortic annulus. J Cardiothorac Vasc Anesth 2016; S1053-0770: 00072–0. [DOI] [PubMed] [Google Scholar]
- 9.Adamo L, Braverman AC. Surgical threshold for bicuspid aortic valve aneurysm: a case for individual decision-making. Heart 2015; 101:1361–1367. [DOI] [PubMed] [Google Scholar]
- 10.Nishimura RA, Otto CM, Bonow RO, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014; 63:2438–2488. [DOI] [PubMed] [Google Scholar]
- 11.Etz CD, Zoli S, Brenner R, et al. When to operate on the bicuspid valve patient with a modestly dilated ascending aorta. Ann Thorac Surg 2010; 90:1884–1890. [DOI] [PubMed] [Google Scholar]
- 12.Kallenbach K, Sundt TM, Marwick TH. Aortic surgery for ascending aortic aneurysms under 5.0 cm in diameter in the presence of bicuspid aortic valve. JACC Cardiovasc Imaging 2013; 6:1321–1326. [DOI] [PubMed] [Google Scholar]
- 13.Mangini A, Lemma M, Contino M, et al. Bicuspid aortic valve: differences in the phenotypic continuum affect the repair technique. Eur J Cardiothorac Surg 2010; 37:1015–1020. [DOI] [PubMed] [Google Scholar]


