Abstract
Background:
Acupuncture has been suggested to treat chronic obstructive pulmonary disease (COPD) in China. However, current evidence is insufficient to draw a firm conclusion regarding the effectiveness of acupuncture in COPD. Therefore, this multicenter, randomized, sham-controlled study was designed to evaluate the efficacy of acupuncture for treating patients with COPD.
Methods:
This is a two-arm, parallel group, multicenter, randomized, sham-controlled trial with concealed allocation, and participants, assessor, and analyst blinding. Seventy-two participants with COPD were recruited and randomly divided into 2 groups (real acupuncture group and sham acupuncture group) in a 1:1 ratio. Patients received either real or sham needling at the same acupoints 3 times weekly for 8 weeks. The primary outcome was dyspnea on exertion evaluated using the 6-minute walk test. In addition, health-related quality of life was also evaluated. Measurements were obtained at baseline and after 8 weeks of treatment.
Results:
Six-minute walking distance measurements and health-related quality of life were significantly better in the real acupuncture group than that in the sham acupuncture group.
Conclusion:
The findings suggest that acupuncture can be used as an adjunctive therapy to reduce dyspnea in patients with COPD.
Keywords: acupuncture, chronic obstructive pulmonary disease, dyspnea, randomized controlled trial
1. Introduction
Chronic obstructive pulmonary disease (COPD) is a common, slowly progressing disease characterized by irreversible airflow limitation and the gradual loss of lung function.[1] It is thought that COPD affects 64 million people worldwide, and World Health Organization projections estimate that it will be the third leading cause of death by 2030.[1–2] COPD brings a significant burden not only for patients and their families but also for social healthcare systems in general. The disease is associated with poor health-related quality of life in many patients.[3]
Smoking cessation is considered as number one priority, followed by pharmacological intervention, to help relieve symptoms, reduce acute exacerbations, and improve exercise capacity and quality of life in clinically stable COPD patients. However, more effective and safer therapies are still looked for.[4]
Acupuncture therapy has been widely used to treat a variety of conditions, such as stroke,[5–8] insomnia,[9] migraine,[10,11] knee pain,[12–14] neck pain,[15,16] frozen shoulder,[17] pressure ulcer,[18,19] irritable bowel syndrome,[20] chronic pelvic pain syndrome,[21] cancer care,[22] Alzheimer disease,[23] and COPD.[24–26] Specifically, acupuncture therapy has been suggested and used to treat patients with COPD in China.[24,25]
It is reported that acupuncture may help relieve COPD by reducing bronchial immune-mediated inflammation and by promoting release of vascular and immunomodulatory factors.[27,28] A recent systematic review of randomized controlled trials of acupuncture therapies for treating COPD found that acupuncture therapies may result in clinically important improvements in quality of life and dyspnea.[29] However, research studies have generally provided poor evidence due to methodological limitations, including low-quality study design, inadequate control groups, and variation in acupuncture composition. Therefore, more rigorously designed studies are needed to elucidate the effectiveness of acupuncture therapy for treating patients with COPD. We hypothesized that real acupuncture would be superior at 8 weeks compared with sham needle acupuncture. Thus, this study aimed to conduct a multicenter, randomized, sham-controlled trial to evaluate the efficacy of acupuncture therapy for treating patients with COPD.
2. Methods/design
2.1. Study design
This is a two-arm, parallel group study with participants, assessor, and analyst blinding. The study was conducted at Hangzhou Fuyang Hospital of Traditional Chinese Medicine, The People's Hospital of Fuyang, and the First Affiliated Hospital of Heilongjiang University of Chinese Medicine in accordance with the Declaration of Helsinki and its amendments and each institution's Guidelines for Good Clinical Practice. From April 2014 to July 2015, 72 eligible participants were randomly divided into 2 groups (real acupuncture group and sham acupuncture group) at a 1:1 allocation ratio. The patients received either real or sham acupuncture needling 3 times weekly for 8 weeks. Outcome evaluation and data analysis were performed after 8 weeks of treatment by a team of professionals, who were blinded to group allocation.
2.2. Eligibility
2.2.1. Inclusion criteria
The inclusion criteria were as follows:
A confirmed diagnosis of COPD (stage II, III or IV) in accordance with the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines[1]
A clinically stable condition without history of infections or exacerbation of respiratory symptoms
No changes in medication within the 3 months preceding the study outset
No signs of edema
The ability to walk without assistance
No pulmonary rehabilitation in the previous 6 months
The provision of written informed consent prior to enrollment into the study
2.2.2. Exclusion criteria
Patients with the following conditions were excluded: cardiovascular disease, collagen disease, renal failure, thyroid dysfunction, hepatic function disorder, cancer, and severe mental disorder.
2.3. Randomization and allocation concealment
Participants who met all the inclusion and exclusion criteria were randomly assigned to the real acupuncture group or sham acupuncture group in a 1:1 ratio at the second visit through central randomization. A professional statistician, who was blinded to this study, generated the random numbers using a computerized number generator with SAS package (Version 9.1; SAS Institute Inc., Cary, NC). Allocation was concealed in sequentially numbered, opaque, and sealed envelopes containing the randomization assignments. Acupuncturists were not blinded. However, the participants, outcome assessors, and data analysts were masked to the treatment allocation.
2.4. Intervention
In addition to the daily medication, the participants in the real acupuncture group received 30-minute sessions of acupuncture treatment, 3 times weekly for 8 weeks. Acupoints were selected according to the previous studies on acupuncture for COPD and the literature describing the traditional prescription of acupuncture points for bronchial asthma and chronic bronchitis pulmonary dysfunction.[30,31] The following bilateral acupoints were used: LU1, LU9, LI18, ST36, GB12, BL13, BL20, and BL23. Both groups used the same acupoints.
Sham acupuncture treatment was operated by a Park sham device.[32] The tips of the sham needles were blunt and appeared to be penetrating the skin but actually telescoped back into place in the sham acupuncture group. The needles were not inserted into the skin.
Both real and sham needles were the same size (sterile disposable acupuncture needles, 40 mm in length and 0.30 mm in diameter; Andy brand, Guizhou Andy Medical Instrument Co., Guizhou, China). De qi (tingling, numbness, and heaviness) was achieved during the manipulation of needles at every point in the real acupuncture group.
2.5. Outcome measurements
All outcomes were measured at baseline and after 8 weeks of treatment.
2.5.1. Primary outcomes
The primary outcome was the severity of dyspnea on exertion (DOE), which was assessed using the 6-minute walk test (6MWT). A modified 10-point Borg category ratio scale was used to measure the breathlessness before and immediately after the 6MWT, where 0 signified “breathing very well, barely breathless” and 10 signified “severely breathless.”[33]
2.5.2. Secondary outcomes
Secondary outcome measures included the 6-minute walk distance (6MWD)[34]; the lowest oxygen saturation during the 6MWT; and forced expiratory volume in 1 second (FEV1).[35] In addition, quality of life of the patients was measured with the St. George Respiratory Questionnaire (SGRQ).[36] Measurements were obtained at baseline and after 8 weeks of treatment.
2.6. Statistical analysis
Statistical analysis was conducted by an analyst. Statistical Package for the Social Sciences (SPSS) software 17.0 (SPSS Inc., Chicago, IL) was used to conduct the data analysis. The sample size was calculated based on the primary outcome, that is, the change in the Borg scale score at the end of the 6MWT. The minimal clinically important difference in the Borg scale score in COPD patients is 2 units.[37] Therefore, the required sample size of this study was estimated to be 72 subjects (36 per group) in order to detect a minimal difference between means in the Borg scale score of 2.0 with α = 0.5 and β = 0.8. We also assumed a 20% dropout rate. All data are presented as the mean (standard deviation [SD]) or the mean (95% confidence interval [CI]). Analysis was by intention-to-treat. Statistical significance is reported as P values from independent t-tests, because all outcome data were normal distribution. The statistical significance level was set at P < 0.05.
3. Results
A total of 153 Chinese participants were initially screened and entered the study (Fig. 1). Of these 153 patients, 52 did not meet the study criteria and 29 declined to participate. Therefore, 72 participants were randomized into the real acupuncture and sham acupuncture groups. All 72 subjects were evaluated using the 6MWT, but only 65 patients completed the treatment. Seven patients withdrew from the study. The major reasons for withdrawal were withdrawal of consent and change of medication (Fig. 1).
Figure 1.
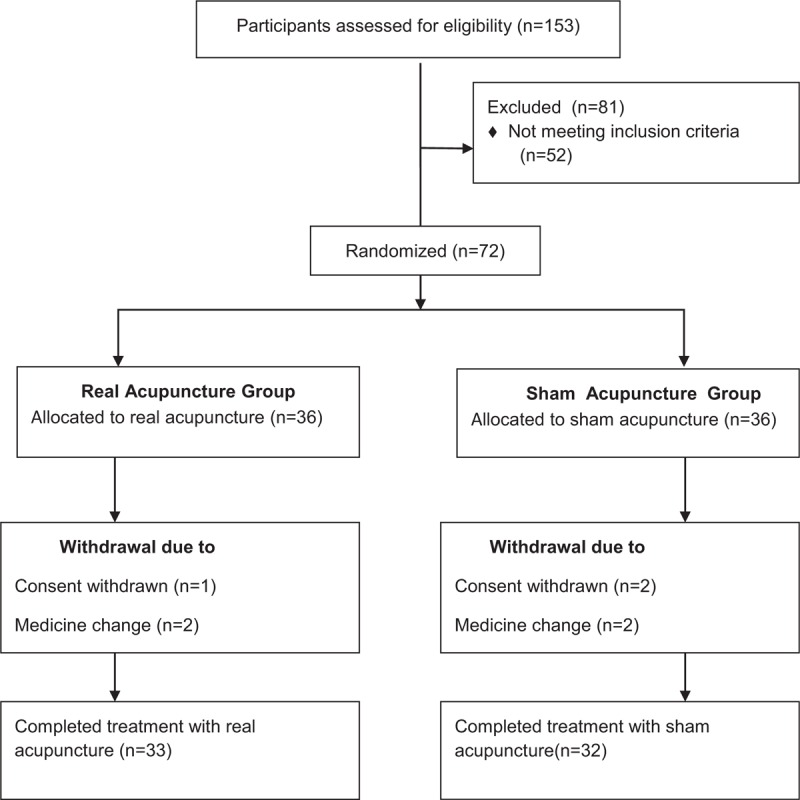
Flow of participants through the trial.
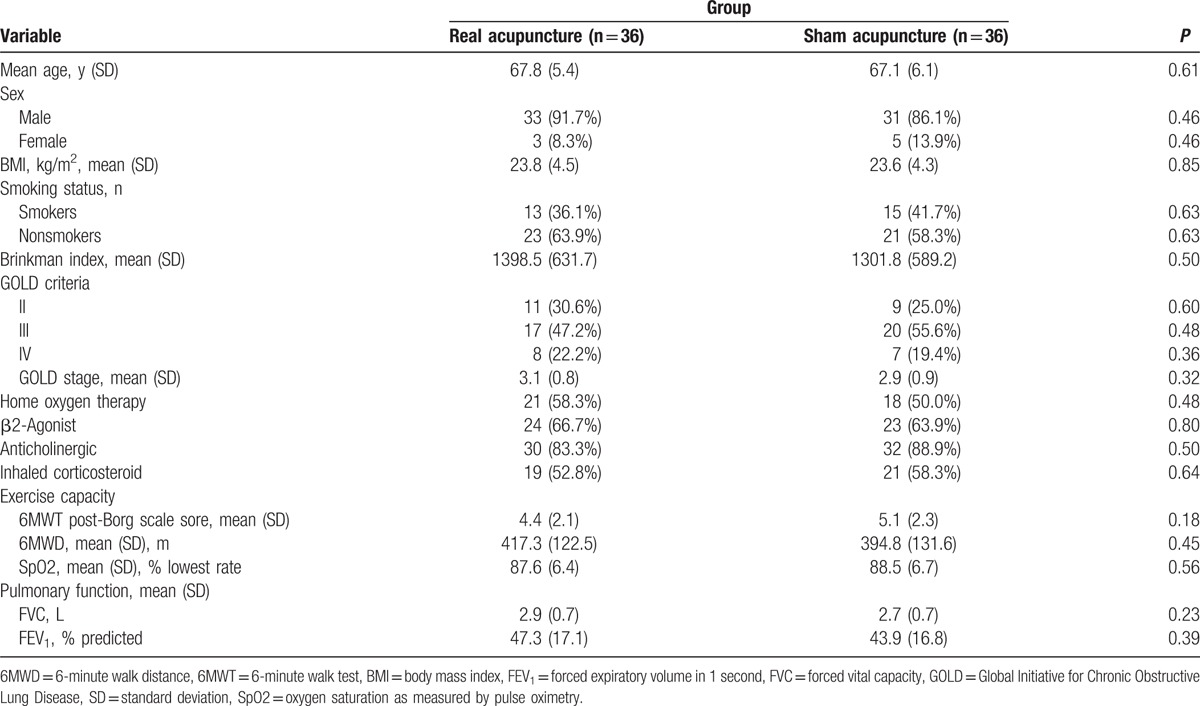
The patient characteristics and the baseline symptom severity of the study population are summarized in Table 1. The 2 groups did not differ significantly in all the characteristics and clinical variables at the baseline visit. At baseline, the mean age (SD) was 67.8 (5.4) years in the real acupuncture group and 67.1 (6.1) years in the sham acupuncture group. The body mass index (BMI) was 23.8 (4.5) in the real acupuncture group and 23.6 (4.3) in the sham acupuncture group. The baseline 6MWT post-Borg scale score, 6MWD, and oxygen saturation as measured by pulse oximetry (SpO2) were 4.4 (2.1), 417.3 (122.5), and 87.6 (6.4), respectively, in the real acupuncture group and 5.1 (2.3), 394.8 (131.6), and 88.5 (6.7), respectively, in the sham acupuncture group. In addition, the baseline forced vital capacity (FVC) and FEV1 were 2.9 (0.7) and 47.3 (17.1) in the real acupuncture group and 2.7 (0.7) and 43.9 (16.8) in the sham acupuncture group.
Table 1.
Baseline characteristics of participants at trial entry.
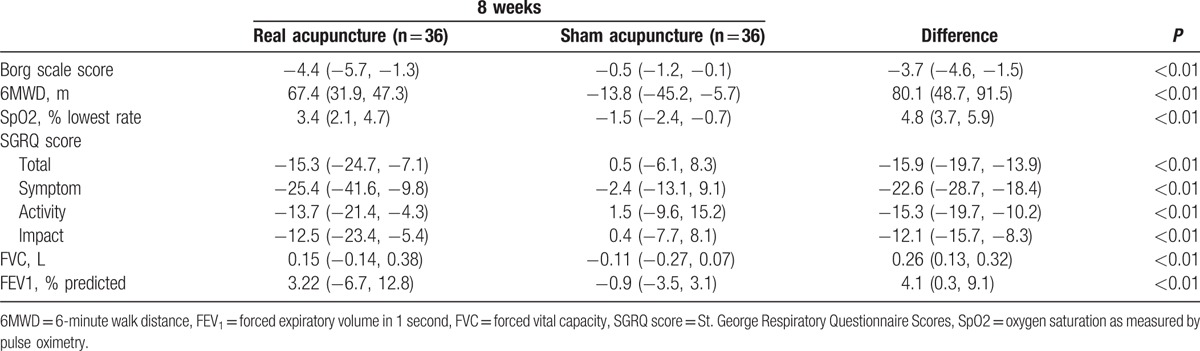
We examined the mean change from baseline (95% CI) by treatment and the difference (95% CI) between real acupuncture and sham acupuncture to evaluate the efficacy of real acupuncture for treating COPD. The results for the efficacy endpoints after 8 weeks of treatment are summarized in Table 2. Real acupuncture improved the severity of DOE evaluated by the 6MWT as well as the lung function compared with sham acupuncture at 8 weeks. After 8 weeks, the real acupuncture group exhibited significant improvements in health-related life quality compared with the sham acupuncture group (Table 2).
Table 2.
Primary and secondary outcome measurements at 8 weeks after treatment (change from baseline).
4. Discussion
The results of this study met our hypothesis that real acupuncture was superior at 8 weeks compared with sham needle acupuncture for treating COPD. Previous studies have assessed the efficacy of acupuncture for treating COPD. However, 2 studies were conducted in the United Kingdom, and the included patients had various diseases, including bronchial asthma, interstitial pneumonia, cystic fibrosis, and COPD.[38,39] It is therefore inconclusive whether acupuncture is really effective for treating COPD alone. One study was conducted in Japan. It found that acupuncture was effective for treating Japanese patients with COPD.[31] In addition, although 4 studies were also conducted to evaluate the efficacy of acupuncture for treating COPD in China, all these studies suffered from methodological design limitations.[24,25,40,41]
To our best knowledge, this study is the first multicenter, randomized, sham-controlled trial with concealed allocation, and participant, assessor, and analyst blinding conducted in China. Our findings demonstrated the efficacy of acupuncture therapy for patients with COPD.
In this study, the mean decrease of the Borg scale score after the 6MWT, and the increase in the 6MWD with acupuncture treatment were significantly greater in the real acupuncture group than in the sham acupuncture group. In addition, the increase in lowest oxygen saturation during the 6MWT after acupuncture treatment was also greater in the real acupuncture group than in the sham acupuncture group. These results indicate the efficacy of acupuncture for treating the symptoms of COPD patients, especially DOE. Furthermore, the total score on the SGRQ was significantly decreased in COPD patients in the real acupuncture group, when compared with the patients in the sham acupuncture group. Thus, acupuncture treatment appears to be promising for improving the health-related quality of life of COPD patients.
This study had several limitations. First, it was impossible to interrupt the standard medication for the patients with COPD, so most patients kept taking their daily medication. Although the baseline medication was similar between the 2 groups, the achieved efficacy may have been the result of the synergistic effect of acupuncture plus medication, and not of acupuncture alone. Second, this study did not include a follow-up evaluation owing to its short duration. Thus, the long-term effect of acupuncture on COPD still needs to be addressed in the future. Finally, this study did not blind the acupuncturists, because it is impossible and hard to blind them. Therefore, their attitude might have also influenced the results of this study.
In conclusion, the results of this study found that acupuncture can improve DOE and health-related quality of life of COPD patients. Long-term randomized, controlled trials with follow-up assessments are needed to confirm our results.
Footnotes
Abbreviations: 6MWD = 6-minute walk distance, 6MWT = 6-minute walk test, CI = confidence interval, COPD = chronic obstructive pulmonary disease, DOE = dyspnea on exertion, FEV1 = forced expiratory volume in 1 second, GOLD = Global Initiative for Chronic Obstructive Lung Disease, SD = standard deviation, SGRQ = St. George Respiratory Questionnaire, SPSS = Statistical Package for the Social Sciences.
Authors’ contribution: JF and XW contributed equally to this work. JFF conceived and designed the study. JFF and XHW drafted the manuscript. XHW sought funding and ethical approval. All authors read and approved the final manuscript.
Funding/support: This work was supported in part by Youth Fund of National Natural Science Foundation of China (81403234); Heilongjiang Province Natural Science Fund (H201481); Heilongjiang Province Undergraduate College Young Innovative Talent Training Plan (UNPYSCT-2015120); and Doctor Innovation Fund of Heilongjiang University of Chinese Medicine Research Fund (2012bs06).
The authors have no conflicts of interest to disclose.
References
- 1.Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: updated 2013. London, UK: Global Initiative for Chronic Obstructive Lung Disease; 2013. http://www.goldcopd.org Accessed March 20, 2016. [Google Scholar]
- 2.World Health Organization. World health statistics: 2008. http://www.who.int/gho/publications/world_health_statistics/EN_WHS08_Full.pdf Accessed January 15, 2015. [Google Scholar]
- 3.Menzin J, Boulanger L, Marton J, et al. The economic burden of chronic obstructive pulmonary disease (COPD) in a US Medicare population. Respir Med 2008; 102:1248–1256. [DOI] [PubMed] [Google Scholar]
- 4.American Thoracic Society. European Respiratory Society Task Force. Standards for the Diagnosis and Management of Patients with COPD. New York, NY: American Thoracic Society; 2004. [Google Scholar]
- 5.Gosman-Hedström G, Claesson L, Klingenstierna U, et al. Effects of acupuncture treatment on daily life activities and quality of life: a controlled, prospective, and randomized study of acute stroke patients. Stroke 1998; 29:2100–2108. [DOI] [PubMed] [Google Scholar]
- 6.Yue JH, Golianu B, Zeng XX, et al. Acupuncture for urinary retention after stroke: a protocol for systematic review. Eur J Bio Med Res 2015; 1:7–11. [Google Scholar]
- 7.Sun ZR, Yu NN, Yue JH, et al. Acupuncture for urinary incontinence after stroke: a protocol for systematic review. BMJ Open 2016; 6:e008062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shih CC, Liao CC, Sun MF, et al. A Retrospective Cohort Study Comparing Stroke Recurrence Rate in Ischemic Stroke Patients With and Without Acupuncture Treatment. Medicine (Baltimore) 2015; 94:e1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheuk DKL, Yeung WF, Chung KF, et al. Acupuncture for insomnia. Cochrane Database Syst Rev 2007; 18:CD005472. [DOI] [PubMed] [Google Scholar]
- 10.Yang Y, Que QH, Ye XD, et al. Verum versus sham manual acupuncture for migraine: a systematic review of randomised controlled trials. Acupunct Med 2016; 34:76–83. [DOI] [PubMed] [Google Scholar]
- 11.Yue J, Sun Z, Zhang Q. Verum versus sham acupuncture for the treatment of migraine. Acupunct Med 2016; 0:1.doi: 10.1136/acupmed-2016-011076. [DOI] [PubMed] [Google Scholar]
- 12.Hinman RS, McCrory P, Pirotta M, et al. Acupuncture for chronic knee pain: a randomized clinical trial. JAMA 2014; 312:1313–1322. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Q, Yue J, Lu Y. Acupuncture treatment for chronic knee pain: study by Hinman et al underestimates acupuncture efficacy. Acupunct Med 2015; 33:170. [DOI] [PubMed] [Google Scholar]
- 14.Zhang QH, Yue JH, Sun ZR, et al. Acupuncture for chronic knee pain: A protocol for an updated systematic review. BMJ Open 2016; 6:e008027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun ZR, Yue JH, Zhang QH. Electroacupuncture at Jing-jiaji points for neck pain caused by cervical spondylosis: a study protocol for a randomized controlled pilot trial. Trials 2013; 14:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun ZR, Yue JH, Tian HZ, et al. Acupuncture at Houxi (SI 3) acupoint for acute neck pain caused by stiff neck: study protocol for a pilot randomised controlled trial. BMJ Open 2014; 4:e006236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun KO, Chan KC, Lo SL, et al. Acupuncture for frozen shoulder. Hong Kong Med J 2001; 7:381–391. [PubMed] [Google Scholar]
- 18.Yue J, Zhang Q, Sun Z, et al. A case of electroacupuncture therapy for pressure ulcer. Acupunct Med 2013; 31:450–451. [DOI] [PubMed] [Google Scholar]
- 19.Zhang QH, Yue JH, Sun ZR. Electroacupuncture for pressure ulcer: a study protocol for a randomized controlled pilot trial. Trials 2014; 15:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng H, Li Y, Zhang W, et al. Electroacupuncture for patients with diarrhea-predominant irritable bowel syndrome or functional diarrhea: A randomized controlled trial. Medicine (Baltimore) 2016; 95:e3884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Qin Z, Wu J, Zhou J, et al. Systematic Review of Acupuncture for Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Medicine (Baltimore) 2016; 95:e3095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lau CH, Wu X, Chung VC, et al. Acupuncture and Related Therapies for Symptom Management in Palliative Cancer Care: Systematic Review and Meta-Analysis. Medicine (Baltimore) 2016; 95:e2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou J, Peng W, Xu M, et al. The effectiveness and safety of acupuncture for patients with Alzheimer disease: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2015; 94:e933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao J, Ouyang B, Sun G, et al. The effect of warm acupuncture on lung function and quality of life for stable COPD patients (in Chinese). Chin Acupunct Moxibustion 2011; 31:893–897. [PubMed] [Google Scholar]
- 25.Wang H, Zheng L. Acupoint sticking therapy for the treatment of COPD- 60 cases (in Chinese). Chin Med Mod Distance Educ Chin 2010; 8:33–34. [Google Scholar]
- 26.Whale CA, MacLaran SJ, Whale CI, et al. Pilot study to assess the credibility of acupuncture in acute exacerbations of chronic obstructive pulmonary disease. Acupunct Med 2009; 27:13–15. [DOI] [PubMed] [Google Scholar]
- 27.Carneiro ER, Carneiro CR, Castro MA, et al. Effect of electroacupuncture on bronchial asthma induced by ovalbumin in rats. J Altern Complement Med 2005; 11:127–134. [DOI] [PubMed] [Google Scholar]
- 28.Zijlstra FJ, van den Berg-de Lange I, Huygen FJ, et al. Anti-inflammatory actions of acupuncture. Mediators Inflamm 2003; 12:59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coyle ME, Shergis JL, Huang ET, et al. Acupuncture therapies for chronic obstructive pulmonary disease: a systematic review of randomized, controlled trials. Altern Ther Health Med 2014; 20:10–23. [PubMed] [Google Scholar]
- 30.Suzuki M, Namura K, Ohno Y, et al. The effect of acupuncture in the treatment of chronic obstructive pulmonary disease. J Altern Complement Med 2008; 14:1097–1105. [DOI] [PubMed] [Google Scholar]
- 31.Suzuki M, Muro S, Ando Y, et al. A randomized, placebo-controlled trial of acupuncture in patients with chronic obstructive pulmonary disease (COPD): the COPD-acupuncture trial (CAT). Arch Intern Med 2012; 172:878–886. [DOI] [PubMed] [Google Scholar]
- 32.Park J, White A, Stevinson C, et al. Validating a new nonpenetrating sham acupuncture device: two randomised controlled trials. Acupunct Med 2002; 20:168–174. [DOI] [PubMed] [Google Scholar]
- 33.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14:377–381. [PubMed] [Google Scholar]
- 34.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166:111–117. [DOI] [PubMed] [Google Scholar]
- 35.American Thoracic Society. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 1995; 152:1107–1136. [DOI] [PubMed] [Google Scholar]
- 36.Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation: the St George's Respiratory Questionnaire. Am Rev Respir Dis 1992; 145:1321–1327. [DOI] [PubMed] [Google Scholar]
- 37.Calverley PM. Minimal clinically important difference: exacerbations of COPD. COPD 2005; 2:143–148. [DOI] [PubMed] [Google Scholar]
- 38.Jobst K, Chen JH, McPherson K, et al. Controlled trial of acupuncture for disabling breathlessness. Lancet 1986; 2:1416–1419. [DOI] [PubMed] [Google Scholar]
- 39.Lewith GT, Prescott P, Davis CL. Can a standardized acupuncture technique palliate disabling breathlessness? A single-blind, placebo-controlled crossover study. Chest 2004; 125:1783–1790. [DOI] [PubMed] [Google Scholar]
- 40.Li S, Li J, Yu X, et al. Efficacy of Shu Fei Tie for chronic obstructive pulmonary disease (in Chinese). Shaanxi J Tradit Chin Med 2009; 30:391–392. [Google Scholar]
- 41.Ning LQ, Xu YY, Xu F, et al. Clinical observation on treating 44 cases of stable chronic obstructive pulmonary disease by four seasons acupoint external application (in Chinese). J Pract Tradit Chin Intern Med 2011; 25:3–5. [Google Scholar]


