Abstract
Patients with chronic obstructive pulmonary disease (COPD) have a high prevalence of osteoporosis. The clinical sequel of osteoporosis is fracture. Patients with COPD who experience a fracture also have increased morbidity and mortality. Currently, the types of all-cause and site-specific fracture among patients with COPD are unknown. Thus, we elucidated the all-cause and site-specific fractures among patients with COPD.
A retrospective, population-based, cohort study was conducted utilizing the Taiwan Longitudinal Health Insurance Database.
Patients with COPD were defined as those who were hospitalized with an International Classification of Diseases, Ninth Revision, Clinical Modification code of 490 to 492 or 496 between 2001 and 2011. The index date was set as the date of discharge. The study patients were followed from the index date to the date when they sought care for any type of fracture, date of death, date of health insurance policy termination, or the last day of 2013. The types of fracture analyzed in this study included vertebral, rib, humeral, radial and ulnar/wrist, pelvic, femoral, and tibial and fibular fractures.
The cohort consisted of 11,312 patients with COPD. Among these patients, 1944 experienced fractures. The most common site-specific fractures were vertebral, femoral, rib, and forearm fractures (radius, ulna, and wrist) at 32.4%, 31%, 12%, and 11.8%, respectively. The adjusted hazard ratios of fracture were 1.71 [95% confidence interval (95% CI) = 1.56–1.87] for female patient with COPD and 1.50 (95% CI = 1.39–1.52) for patients with osteoporosis after covariate adjustment.
Vertebral and hip fractures are common among patients with COPD, especially among males with COPD. Many comorbidities contribute to the high risk of fracture among patients with COPD.
Keywords: chronic obstructive pulmonary disease, fracture, National Health Insurance Research Database
1. Introduction
Chronic obstructive pulmonary disease (COPD) is an obstructive airway disease that is not fully reversible. Compared with the general population, patients with COPD have a high prevalence of osteoporosis,[1] which results from chronic, systemic inflammation, the use of corticosteroids, low body mass, and a sedentary lifestyle. The clinical sequel of osteoporosis is fracture. Patients with COPD and fracture experience a decreased quality of life, increased medical expenditures, increased hospital stay durations, and increased mortality.[2,3] A previous study evaluated the prevalence and predictors of vertebral fractures among patients with COPD.[4] In a study using Danish health care registries, patients with COPD had a 60% to 70% higher risk of death following hip fracture than patients without COPD. Furthermore, for patients with COPD and hip fracture, the 1-year mortality rate increased 3 to 5 times compared with patients without hip fracture.[5] Thus, this investigation focused on the outcomes following fracture and the effect of medications on osteoporosis or fracture[6] among patients with COPD. None of the aforementioned studies evaluated all-cause and site-specific fractures among patients with COPD, and most studies only focused on hip or vertebral fractures.
Given the relative paucity of studies regarding the incidence of fracture and site-specific fracture among patients with COPD, in the present study, we examined the incidence of site-specific fracture among patients with COPD.
2. Methods
2.1. Database
This population-based, cohort study utilized the Longitudinal Health Insurance Database 2005 (LHID2005), which is a subset of the National Health Insurance Research Database (NHIRD). The LHID2005 includes the medical claims data of two million beneficiaries randomly selected from the Registry of Beneficiaries of the NHIRD in 2005. The LHID2005 database consists of all inpatient and outpatient medical claims from January 2001 to December 2013. The personal identification numbers of all selected individuals in the LHID2005 were de-identified to protect their privacy. This study was approved by the Institutional Review Board of the Chi Mei medical center (IRB: 10402-E03).
2.2. Patient identification
Patients with COPD were defined as those who were hospitalized with an International Classification of Diseases, Ninth Revision, Clinical Modification code (ICD-9-CM) of 490 to 492 or 496 between 2001 and 2011. If the patient was admitted 2 or more times during the study period, then only the first-time hospitalization was included in the analysis. The index date was defined as the date of discharge. Patients with 1 or more medical claims and a diagnosis of cancer or fracture and patients aged 40 years or younger before the index date were excluded from the study. The patients with COPD were then followed from the index date to the date that care was sought for any type of fracture, date of death, date of health insurance policy termination, or the last day of 2013. The types of fracture analyzed in this study included vertebral fracture (ICD-9-CM: 805, 806), rib fracture (ICD-9-CM: 807), humeral fracture (ICD-9-CM: 812), radial or ulnar/wrist fracture (ICD-9-CM: 813, 814), pelvis fracture (ICD-9-CM: 808), femoral fracture (ICD-9-CM: 820, 821), and tibial or fibular fracture (ICD-9-CM: 823).
2.3. Covariate definitions
The comorbidities were diagnosed by either 1 outpatient visit or 1 hospitalization within 1 year before the index date. These comorbidities included cardiovascular disease, cerebrovascular disease, chronic kidney disease, liver disease, and diabetes. The oral corticosteroid used within 3 months before the index date was also recorded.
2.4. Statistical analyses
The comparisons of baseline covariates between the patients with/without fracture was performed with an independent Student t test for continuous variables or Pearson χ2 test for categorical variables, as appropriate. The distributions of various types of fractures according to the baseline covariates were described with numbers and percentages. The incidence of all-cause fractures and the cumulative survival of all-cause fractures were estimated using the life-table method[7] every 2 years (i.e., 0–2, 2–4, 4–6, 6–8, and 8–10) after the index date. The number of person-years observed during follow-up was calculated from the index date to the date of inpatient/outpatient care for fracture, loss of follow-up, death, or the end of the study (i.e., December 31, 2013). Finally, Cox's proportional hazard regression model was utilized to identify any baseline covariates that may significantly predict the incidence of all-cause fracture.
All statistical analyses were performed using Statistical Analysis Software (SAS) System, version 9.3 (SAS Institute Inc., Cary, NC). Statistical significance was defined with a 2-sided P value <0.05.
3. Results
In total, 35,146 patients were diagnosed with COPD upon discharge between January 2001 and December 2011. Among these patients, we excluded patients younger than 40 years (n = 2803), patients with malignant diseases (n = 13,311), and patients with a fracture history (n = 9801). The final cohort consisted of 11,312 patients. The study population was male dominated (68.05%). More than 74% of the patients were older than 65 years. Table 1 presents the distributions of patient characteristics and selected comorbidities among the 11,312 patients with COPD. Notably, 9368 patients with COPD did not have a fracture, and 48.6% of them were more than 75 years of age. In total, 1944 patients with COPD also had a fracture, and 49.1% of them were more than 75 years of age.
Table 1.
Characteristics of patients with COPD with and without fractures.
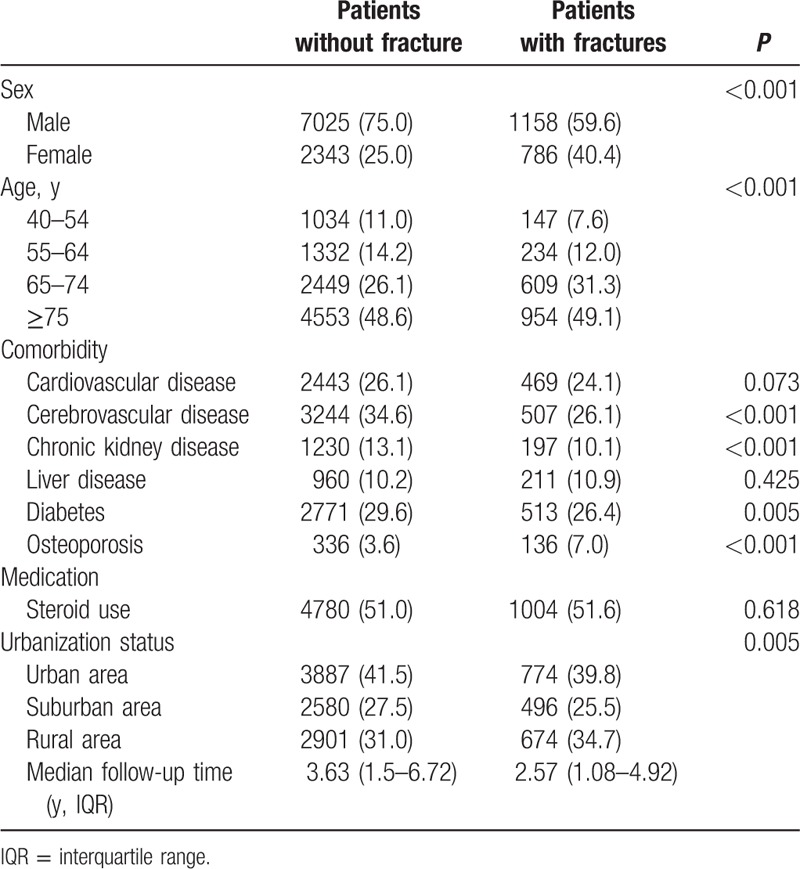
The prevalence of a history of cerebrovascular disease, diabetes, and cardiovascular disease was 34.6%, 29.6%, and 26.1%, respectively, among the patients with COPD and no fractures. The prevalence of a history of cerebrovascular disease, chronic kidney disease, and diabetes was higher among patients with COPD and no fractures than patients with fractures. The median follow-up time was 3.63 years among patients with COPD and no fractures and 2.57 years among patients with COPD and fracture. The percentage of patients treated with an oral corticosteroid within 1 year before the index date was 51% (similar in both groups).
During the study period, 1944 patients with COPD experienced fractures. Table 2 presents the types of fracture among the patients according to selected baseline covariates. The most common types of fracture (in a descending order) included vertebral, femoral, rib, and forearm fractures (radius, ulna, and wrist) occurring in 32.4%, 31%, 12%, and 11.8% of patients, respectively. Among men, the most common sites for bone fractures occurred at the vertebra, rib, femur, tibia, and fibula. Forearm fractures (radius, ulna, and wrist) occurred mostly among women. Aging-associated fractures were most frequently observed at the vertebra, rib, humerus, forearm, and femur. Figure 1 presents Kaplan–Meier survival curve for the unadjusted cumulative fracture-free survival by age group. Figure 2 represents Kaplan–Meier survival curve for the unadjusted cumulative fracture-free survival by sex.
Table 2.
Site-specific fractures among patients with COPD.
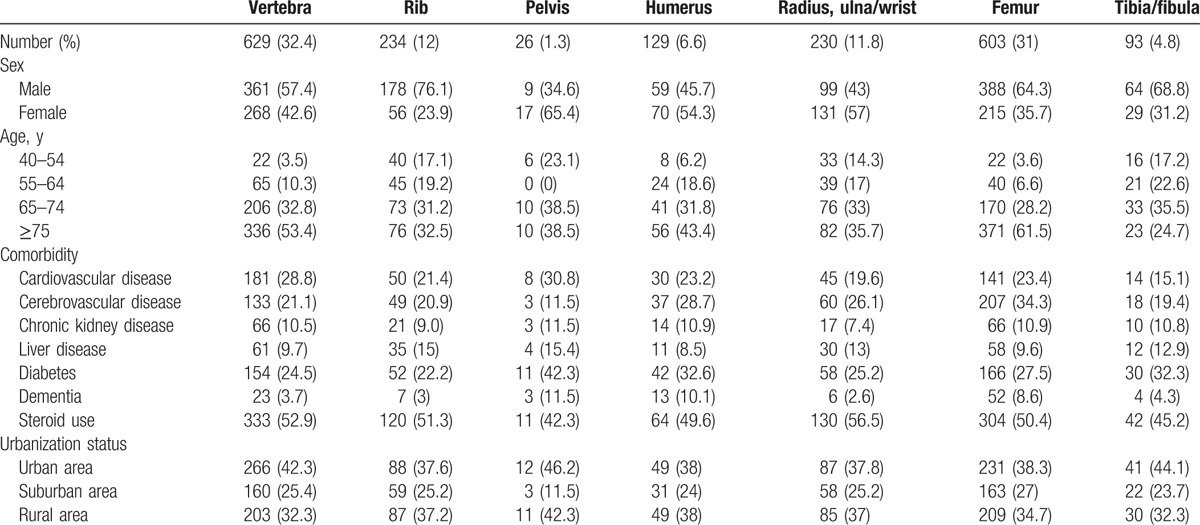
Figure 1.
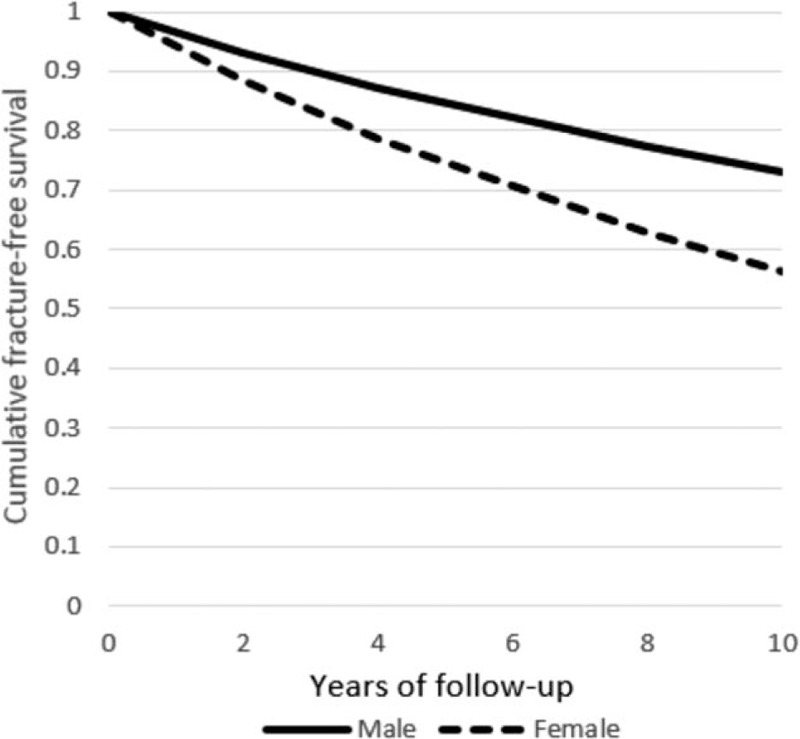
Kaplan–Meier plot showing unadjusted cumulative fracture-free survival by age group.
Figure 2.
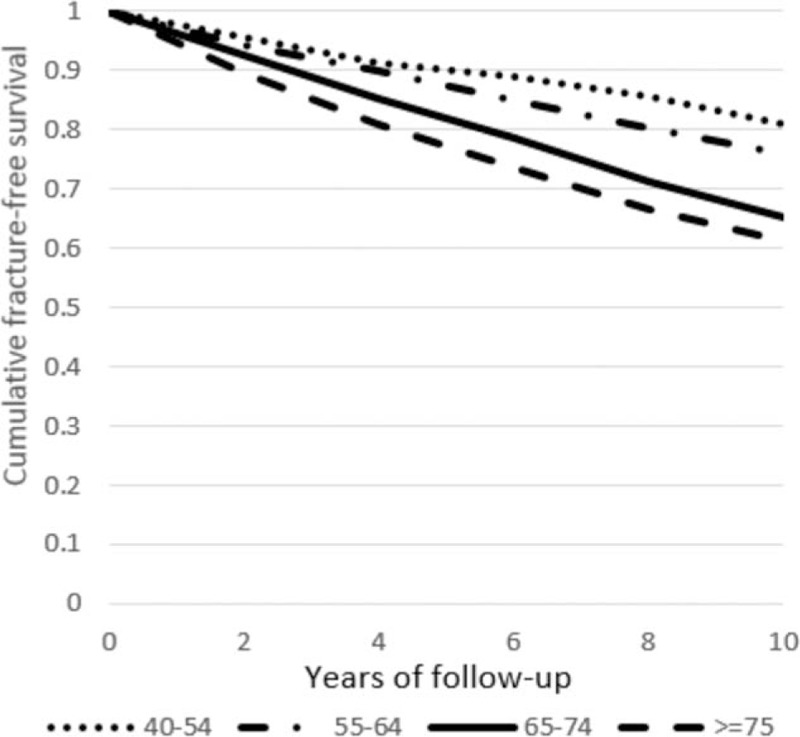
Kaplan–Meier plot showing unadjusted cumulative fracture-free survival by sex.
Table 3 presents the follow-up period-specific cumulative incidence rates for all-cause fractures among patients with COPD. The incidence rate of all-cause fractures remained stable throughout the 10-year follow-up.
Table 3.
Follow-up period-specific incidence rates of all-cause fractures among patients with COPD.
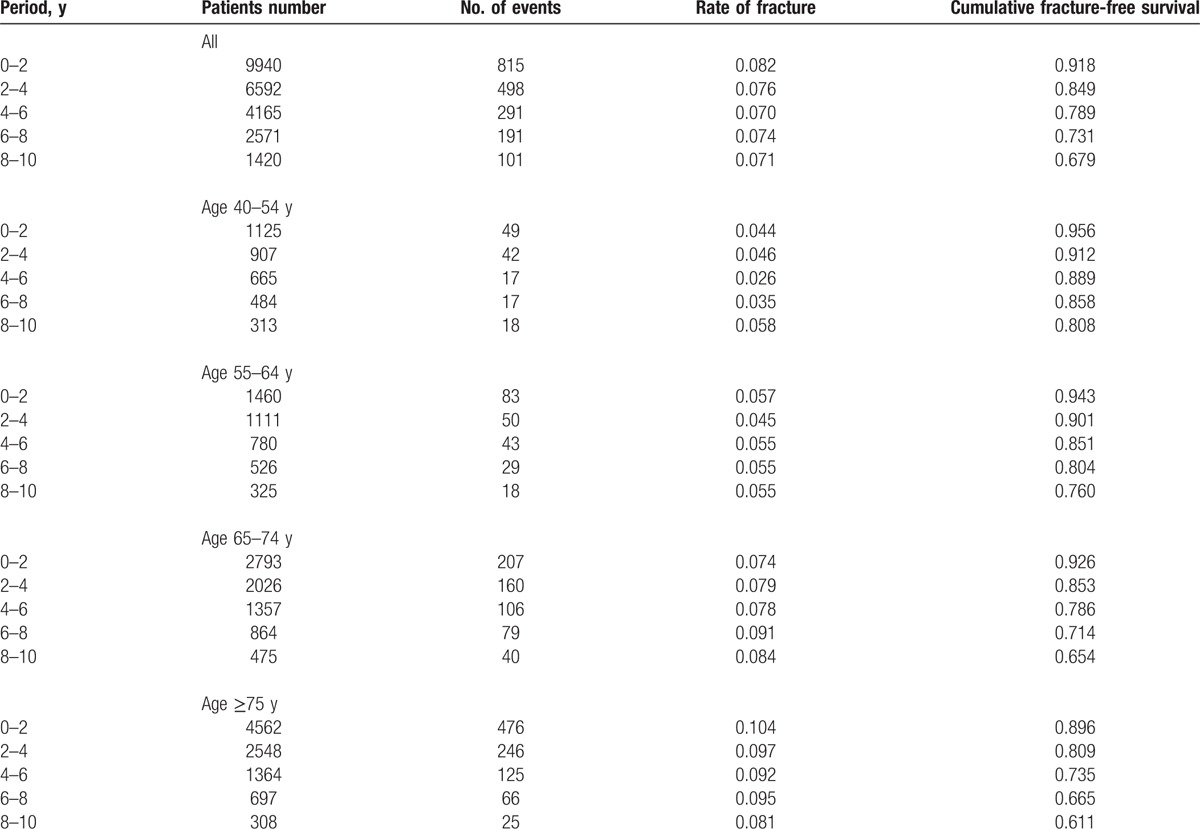
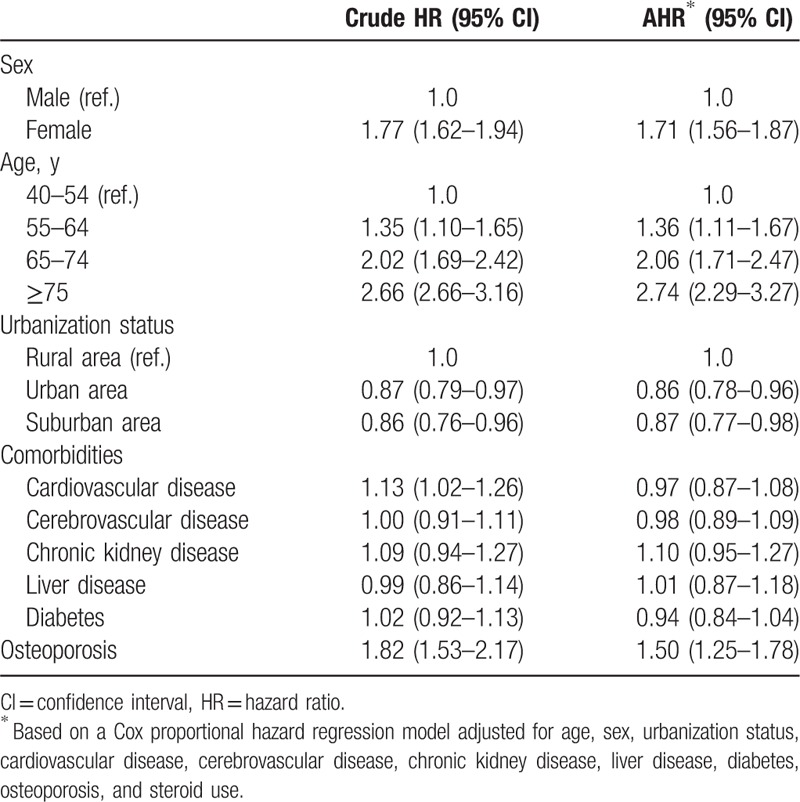
Table 4 presents the hazard ratios (HRs) for fractures according to the baseline characteristics of the study. A significantly increased HR was observed for females, patients in the old age group (≥65 years old), patient living in urban or suburban area, and patients with comorbidity of osteoporosis. The adjusted HR for fractures was highest among patients aged ≥75 years [adjusted hazard ratio (AHR) = 2.74, 95% confidence interval (CI) = 2.29–3.27]. We observed no significant differences regarding the comorbidities of cardiovascular disease, cerebrovascular disease, chronic kidney disease, liver disease, and diabetes. The adjusted HRs for fractures were 1.50 (95% CI = 1.25–1.78) for patients with osteoporosis.
Table 4.
Hazard ratios for fractures according to the baseline characteristics of the study subjects.
4. Discussion
To our knowledge, this report represents the first nationwide study to investigate all-cause and site-specific fractures among patients with COPD. In our study, the most common sites of fracture among patients with COPD were the vertebra and femur (32.5% and 31%, respectively). Female patients with COPD had a higher risk of fracture than male patients with COPD (AHR = 1.71, 95% CI = 1.56–1.87). Age significantly affected the incidence of fracture. The incidences of fracture were more than 2-fold among patients aged 65 to 74 and 75 years and older.
4.1. Fractures among patients with COPD
Female patients had a 71% higher incidence of fracture than male patients (AHR = 1.71, 95% CI = 1.56–1.87). Regarding the age distribution of patients with COPD and fracture, nearly 50% of fractures occurred in the group aged 75 years and older. Our results are similar to those of Majumdar et al.[4] Among 22 COPD patients with moderate-to-severe vertebral fractures, 55% were >75 years old. According to our previous work,[8] the mean age at the time of total hip arthroplasty for a femur fracture in the COPD group was approximately 75 years of age. Age is an important risk factor for fracture, and it is not surprising that the incidence of fracture increased with age. Among patients aged less than 64 years, we observed no significant difference in the risk of fracture between patients with and without COPD.
4.2. COPD and vertebral fracture
McEvoy et al[9] surveyed lateral lumbar and thoracic radiographs to evaluate the presence of vertebral fractures in male COPD patients >50 years of age. The percentage of COPD patients with at least 1 lumbar or thoracic spine fracture ranged from 48.7% among patients who never used a steroid to 63.3% among systemic steroid users. In our study, we enrolled patients with COPD >40 years of age (although we could not assess smoking history or pulmonary function tests). Vertebral fractures accounted for 32.4% of the fractures among COPD patients, and males accounted for 57.4% of vertebral fractures. The low proportion rate of vertebral fractures in our study was because our cohort consisted of patients with less severe fractures and a younger population. In our study, we included patients with COPD who were older than 40 years, regardless of their disease severity. Our results are similar to those from the study by Papaioannou et al[10] who evaluated 127 COPD patients with ICD-9 codes and compared those patients with 127 gender- and age-matched controls. The authors recorded a vertebral fracture prevalence of 26.8%.
The authors performed the study with a small group of COPD patients from an acute care hospital in 1999, and a large proportion of the patients were treated with oral (74.7%) corticosteroids. In our study, a smaller proportion (53%) of the COPD population was treated with an oral corticosteroid.
4.3. COPD and femur fracture
COPD was observed in 47% of the patients with hip fractures and was associated with an increased risk for morbidity and mortality.[11] To our knowledge, the exact prevalence of hip fracture among patients with COPD has not been studied. The prevalence of femoral fracture among patients with COPD was 31%, and femoral fracture was the second most common type of fracture (following vertebral fractures). Femoral fracture was common among patients with COPD, especially among males who accounted for 64.3%. Huang et al[12] also used the NHIRD to survey 16,239 patients with COPD; the hip fracture incidences were 649 per 100,000 person-years among patients with COPD and 369 per 100,000 person-years among patients without COPD. The adjusted HR was 1.57. The authors reported the incidence of hip fracture. We extended their findings and focused on the prevalence of all types of fractures among patients with COPD.
4.4. Cardiovascular disease and fracture
There are many risk factors for fracture.[13–15] Sennerby et al[16] used the registry data from 31,936 enrolled Swedish twins and found that cardiovascular disease was significantly associated with risk of subsequent hip fracture. Genetic factors may play a role in the development of cardiovascular disease and osteoporotic fractures. In addition, Sennerby et al[17] performed a population-based case–control study among women and demonstrated that cardiovascular disease increased the risk of hip fracture among women. Cardiovascular disease and osteoporotic fractures may have common pathological pathways.
4.5. Cerebrovascular disease and fracture
The musculoskeletal system and central nervous system interact with each other. Both bone and brain diseases can result in osteoporotic fractures.[18] Patients with cerebrovascular disease may have decreased bone mineral density resulting from immobilization-induced increased bone resorption.[19,20] Patients who had a stroke had a 10% risk of fracture after 5 years.[21] Early recognition and treatment of poststroke fractures is important for patients with COPD and the general population.
4.6. CKD and fracture
In our previous study,[22] COPD increased the risk of chronic kidney disease. COPD patients have a higher risk of developing chronic kidney disease than subjects without COPD. This finding may be due to a systemic inflammation response. The incidence and prevalence of COPD is rapidly increasing worldwide. Due to its association with aging, the prevalence of COPD is expected to increase in the coming years. Because of the high prevalence of both COPD and chronic kidney disease among older adults, it is important to public health to evaluate the fracture risk in this population. Patients with chronic kidney disease are characterized by alterations in bone, mineral metabolism, and abnormal hormones. Kidney dysfunction results in an overproduction of parathyroid hormone, deficiency of activated vitamin D, hyperphosphatemia, hypocalcemia, and premature hypogonadism. These changes affect the balance between bone resorption and bone formation and lead to altered matrix mineralization, increased osteoclastic bone resorption, impaired bone strength, decreased bone mass, deteriorated bone quality, and increased susceptibility to fracture.[23]
4.7. Diabetes and fracture
Previous studies have reviewed the association between type 2 diabetes mellitus and fracture. Patients with diabetes may experience retinopathy and may also have an increased risk of falling and consequent fracture. Nephropathy results in kidney dysfunction and alters the balance between electrolytes and hormones. Furthermore, body mass index, changes in the bone marrow microenvironment, and thiazolidinedione treatment are associated with bone loss and diminished bone formation, which also increases the risk of fracture.
Similar to patients with COPD, patients with diabetes have systemic inflammation, and the formation of advanced glycation end products may change bone remodeling.[24] COPD and diabetes have similar pathophysiological processes that give rise to disease with systemic and local inflammation, oxidative stress, hypoxemia, or hyperglycemia.[25]
4.8. Limitations and strengths
There were some limitations to our study. First, we could not assess the history of smoking, lung function test, or COPD severity from the database. Smokers have an increased likelihood of fracturing their hips and the excess risk increases with age: 17% at age 60 years, 41% at age 70 years, and 71% at age 80 years.[26] Otherwise, people who have smoked can double the risk of vertebral fractures.[27] Reduction of pulmonary function was associated with clinical and radiological measures of severity of spinal fractures.[28] Majumdar et al recruited patients with COPD acute exacerbation presenting at 3 Canadian emergency departments found that pulmonary function tests tended to be worse among patients with vertebral fracture and patients with vertebral fracture tended to have more severe disease according to history or spirometry.[4] Second, we also had no information regarding the severity of osteoporosis. This nationwide, retrospective study represents all-cause and site-specific fractures among patients with COPD, regardless of COPD disease severity and osteoporosis. Third, because the most patients were elderly, and had comorbidities, they were most likely on medication other than steroids (e.g., proton pump inhibitors, thyroid hormone replacement drugs, etc) that may also contribute toward an increased risk of osteoporosis. Finally, because our database lacks information about levels of physical activity, body mass index, or smoking habits, we included no data on levels of physical activity, body mass index, or smoking habits of the cohort of patients, which are all factors that may bias results, independently of COPD. This national study included a large number of participants and is the first study to address the incidence of fracture at all sites among patients with COPD.
5. Conclusion
Vertebral and hip fractures are common among patients with COPD, especially among males with COPD. COPD is a chronic and systemic inflammation disease. Multiple comorbidities often coexist and common among COPD patients and can contribute to the pathogenesis of fracture. It is an important issue to prompt detect and treatment of osteoporosis and comorbid illnesses contributing to fracture in patients with COPD.
Footnotes
Abbreviations: CI = confidence interval, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CVA = cerebrovascular accident, CVD = cardiovascular disease, DM = diabetes mellitus, HR = hazard ration, LHID = Longitudinal Health Insurance Database, NHI = National Health Insurance, NHIRD = National Health Insurance Research Database, SD = standard deviation.
The authors report no conflicts of interest.
References
- 1.Graat-Verboom L, Wouters EF, Smeenk FW, et al. Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J 2009; 34:209–218. [DOI] [PubMed] [Google Scholar]
- 2.de Luise C, Brimacombe M, Pedersen L, et al. Comorbidity and mortality following hip fracture: a population-based cohort study. Aging Clin Exp Res 2008; 20:412–418. [DOI] [PubMed] [Google Scholar]
- 3.Wehren LE, Magaziner J. Hip fracture: risk factors and outcomes. Curr Osteoporos Rep 2003; 1:78–85. [DOI] [PubMed] [Google Scholar]
- 4.Majumdar SR, Villa-Roel C, Lyons KJ, et al. Prevalence and predictors of vertebral fracture in patients with chronic obstructive pulmonary disease. Respir Med 2010; 104:260–266. [DOI] [PubMed] [Google Scholar]
- 5.de Luise C, Brimacombe M, Pedersen L, et al. Chronic obstructive pulmonary disease and mortality following hip fracture: a population-based cohort study. Eur J Epidemiol 2008; 23:115–122. [DOI] [PubMed] [Google Scholar]
- 6.Loke YK, Cavallazzi R, Singh S. Risk of fractures with inhaled corticosteroids in COPD: systematic review and meta-analysis of randomised controlled trials and observational studies. Thorax 2011; 66:699–708. [DOI] [PubMed] [Google Scholar]
- 7.Culter S, Ederer F. Maximum utilization of the life table method in analyzing survival. J Chronic Dis 1958; 53:457–481. [DOI] [PubMed] [Google Scholar]
- 8.Liao KM, Lu HY. A National analysis of complications following total hip replacement in patients with chronic obstructive pulmonary disease. Medicine 2016; 95:e3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McEvoy CE, Ensrud KE, Bender E, et al. Association between corticosteroid use and vertebral fractures in older men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998; 157:704–709. [DOI] [PubMed] [Google Scholar]
- 10.Papaioannou A, Parkinson W, Ferko N, et al. Prevalence of vertebral fractures among patients with chronic obstructive pulmonary disease in Canada. Osteoporos Int 2003; 14:913–917. [DOI] [PubMed] [Google Scholar]
- 11.Regan EA, Radcliff TA, Henderson WG, et al. Improving hip fractures outcomes for COPD patients. COPD 2013; 10:11–19. [DOI] [PubMed] [Google Scholar]
- 12.Huang SW, Wang WT, Chou LC, et al. Chronic obstructive pulmonary disease increases the risk of Hip fracture: a nationwide population-based cohort study. Sci Rep 2016; 6:23360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sambrook P, Cooper C. Osteoporosis. Lancet 2006; 367:2010–2018. [DOI] [PubMed] [Google Scholar]
- 14.Kanis JA, McCloskey EV, Johansson H, et al. Development and use of FRAX ( in osteoporosis. Osteoporos Int 2010; 21 suppl 2:S407–S413. [DOI] [PubMed] [Google Scholar]
- 15.Kanis JA, Borgstrom F, De Laet C, et al. Assessment of fracture risk. Osteoporos Int 2005; 16:581–589. [DOI] [PubMed] [Google Scholar]
- 16.Sennerby U, Melhus H, Gedeborg R, et al. Cardiovascular diseases and risk of hip fracture. JAMA 2009; 302:1666–1673. [DOI] [PubMed] [Google Scholar]
- 17.Sennerby U, Farahmand B, Ahlbom A, et al. Cardiovascular diseases and future risk of hip fracture in women. Osteoporos Int 2007; 18:1355–1362. [DOI] [PubMed] [Google Scholar]
- 18.Birge SJ. Osteoporotic fractures: a brain or bone disease? Curr Osteoporos Rep 2008; 6:57–61. [DOI] [PubMed] [Google Scholar]
- 19.Sato Y, Maruoka H, Honda Y, et al. Development osteopenia in the hemiplegic finger in patients with stroke. Eur Neurol 1996; 36:278–283. [DOI] [PubMed] [Google Scholar]
- 20.Sato Y, Kuno H, Kaji M, et al. Increased bone resorption during the first year after stroke. Stroke 1998; 29:1373–1377. [DOI] [PubMed] [Google Scholar]
- 21.Lisabeth LD, Morgenstern LB, Wing JJ, et al. Poststroke fractures in a bi-ethnic community. J Stroke Cerebrovasc Dis 2012; 21:471–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen CY, Liao KM. Chronic obstructive pulmonary disease is associated with risk of chronic kidney disease: a nationwide case-cohort study. Sci Rep 2016; 6:25855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nickolas TL, Leonard MB, Shane E. Chronic kidney disease and bone fracture: a growing concern. Kidney Int 2008; 74:721–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moseley KF. Type 2 diabetes and bone fractures. Curr Opin Endocrinol Diabetes Obes 2012; 19:128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rogliani P, Lucà G, Laur D. Chronic obstructive pulmonary disease and diabetes. COPD Res Pract 2015; 1:3. [Google Scholar]
- 26.Seeman E. Marcus R, Feldman D, Kelsey J. The effects of tobacco and alcohol use on bone. Osteoporosis. San Diego, CA: Academic Press Inc; 1996. 577–598. [Google Scholar]
- 27.Aloia J, Cohn SH, Vaswani A, et al. Risk factors for postmenopausal osteoporosis. Am J Med 1985; 78:95–100. [DOI] [PubMed] [Google Scholar]
- 28.Schlaich C, Minne HW, Bruckner T, et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int 1998; 8:261–267. [DOI] [PubMed] [Google Scholar]


