Abstract
Background:
Secondhand smoke (SHS) exposure is deleterious to pregnant women and their unborn children. The prevalence of SHS exposure among pregnant women is particularly high in many Asian countries where approximately half of the male population smokes. We aim to investigate the efficacy of an intervention based on an expanded Health Belief Model (HBM) incorporating self-efficacy to educate and empower pregnant women to reduce their SHS exposure.
Methods:
We conducted a 3-arm randomized controlled trial (N = 50 in each arm) comparing the effectiveness of group-based and individual-based interventions with a treatment-as-usual group. A questionnaire tapping into constructs of the expanded HBM was administered at baseline and 1- and 2-month follow-ups. Exhaled carbon monoxide was used to determine SHS exposure (>=6 ppm). ANOVA was used to compare HBM construct scores, self-efficacy for rejecting SHS exposure, and SHS rejection behavior among the 3 groups at baseline and the 1- and 2-month follow-ups, while logistic regression analysis was used to compare the risk of exposure to SHS at each follow-up.
Results:
The group-based intervention significantly improved health beliefs, self-efficacy, and self-reported rejection behaviors. The individual-based intervention effect was limited to some health belief constructs and SHS rejection behaviors. Both group- and individual-based interventions showed significant reductions in SHS exposure 2 months after the intervention (P < 0.0001).
Conclusion:
Group-based educational interventions based on the HBM are particularly effective in training pregnant women to avoid and refuse exposure to SHS. Policy makers should consider offering group-delivered programs to educate and empower pregnant women to reduce their SHS exposure.
Keywords: global health, harm reduction, human rights, prevention, secondhand smoke
1. Introduction
The health hazards of secondhand smoke (SHS) exposure has been well documented (Centers for Disease Control and Prevention, 2010). In many East Asian countries approximately half of men smoke; the prevalence of smoking in women, however, is generally low (less than 5%).[1] Therefore, while not smoking themselves, the health of many women in Asia still being threatened by SHS.
Pregnant women are particularly vulnerable to SHS, as environmental tobacco smoke exposure has been found to be associated with negative consequences on pregnancy and infant outcomes.[2] Increased risk of low birth weight, stillbirth, preterm delivery, congenital anomalies, and sudden infant death syndrome have all been found to be associated with SHS exposure during pregnancy.[3] In Taiwan, where only 3.3% of women are current smokers,[4] as many as 70% of pregnant women have been estimated to be exposed to SHS.[5,6] This egregious figure calls for proactive action to curb an unwarranted public health hazard.
Educational interventions based on an expanded Health Belief Model (HBM) incorporating self-efficacy to enhance the knowledge and efficacy of women to avoid and refuse SHS exposure is an effective strategy to reduce the level of SHS exposure in western countries.[7,8] The HBM posits that changes in health behaviors can be predicted through 4 sets of individual perceptions: perceived susceptibility to a disease or illness, perceived severity of a particular condition, perceived barriers which may prevent action, and perceived benefits of the recommended behavior.[9] Application of the HBM predicts that a pregnant woman will be more willing to change her behavior, and hence avoid SHS exposure, if she perceives the negative consequences of SHS exposure, understands the severity of the consequences, and recognizes the benefits of reducing her exposure. In other words, the HBM is based on the proposition that a person will take a health-related action if she feels that a negative health condition can be avoided (i.e., health belief). The addition of the “self-efficacy” construct to the HBM accounts for the capability aspect of behavior change, which has further strengthened the model.[9]
One previous study from Taiwan using a randomized controlled design has demonstrated that educational interventions based on this expanded HBM successfully enhance the capability of pregnant women to avoid and refuse SHS.[10] In that study, the intervention group demonstrated higher levels of readiness to refuse SHS and was more motivated to engage in SHS preventative actions than the comparison group. Similar findings were reported by Kazemi et al in Iran.[11] Although the results from these 2 randomized controlled trials are encouraging, case-by-case skill training is labor-intensive and time-consuming. Group interventions thus offer a possible cost-effective alternative. The current study aims to assess the efficacy of group- and individual-based interventions based on an expanded HBM by comparing them with a control group to determine the respective effects of these 2 interventions on the health beliefs, self-efficacy, rejection behaviors, and SHS exposure of pregnant women.
2. Methods
2.1. Study design and sampling
This 3-arm randomized controlled trial was conducted in the obstetric clinic of Taipei City Hospital (TCH) from May 1st, 2013 to September 30th, 2013. Nonsmoking pregnant women 18 years of age and older whose pregnancy had not exceeded 12 weeks of gestation were included. Those who were illiterate, not Taiwanese citizens, terminated their pregnancy during the study period, or had a history of psychiatric or substance use disorders were excluded. Eligible participants were approached when they received routine antenatal checkups in the obstetric clinic of TCH. The randomization procedure and study protocols were introduced upon recruitment. Each participant provided written informed consent.
A total of 283 pregnant women were approached. Forty three refused to participate and 68 were excluded because they did not have adequate literacy skills to understand the content of the educational material. The women who refused to participate did not differ from those who did participate in terms of age and educational attainment. The 172 participants admitted into the study were randomly assigned to 3 arms: group-based educational intervention (N = 55), individual-based educational intervention (N = 57), and treatment-as-usual group (N = 60). Several cases from each group dropped out during the intervention period leaving exactly 50 participants in each arm. The dropout rate did not differ significantly between the 3 groups. We set the effect size as 0.8,[12] at the 5% level of statistical significance, 50 women in each arm would yield 85% of power to detect the group differences. The study was approved by the Institutional Review Board of the TCH (IRB No. TCHIRB-1010213). Figure 1 presents a flow chart of participants’ allocation process.
Figure 1.
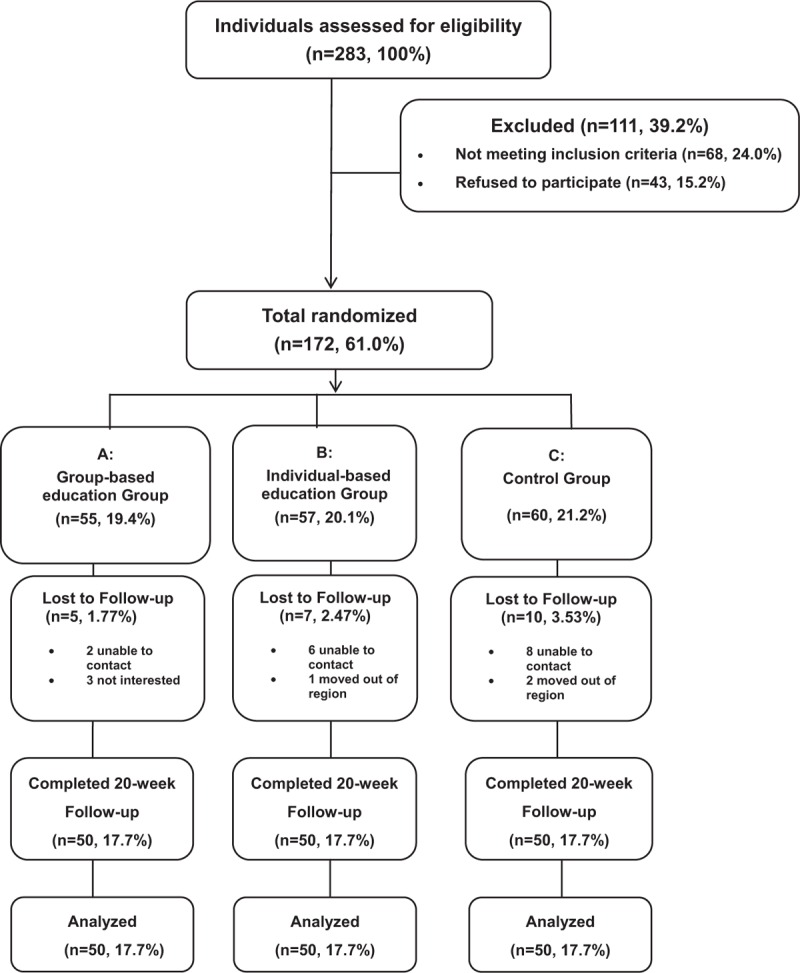
Flowchart of the participants recruitment and allocation.
2.2. Study procedure
Participants were blind to group allocation. Each participant filled out a self-report questionnaire at the time of recruitment. Both intervention groups filled out the same questionnaire again at the 1st and 2nd month following the completion of the intervention. The control group filled out the self-report questionnaire at the time of recruitment and at the 1st and 2nd month following recruitment. The questionnaire taps into constructs of self-efficacy, the 5 main aspects of the HBM (i.e., knowledge, perceived susceptibility and severity of exposure to SHS, perceived barriers to refusing SHS exposure, and perceived benefits of avoiding SHS), and self-reported behaviors in response to SHS.
Participants in the group-based intervention received a 50-minute educational group intervention while the participants in the individual-based intervention received the same education through a one-on-one training session. Both individual- and group-based interventions were conducted during participants’ 1st trimester. The treatment-as-usual group received standard government-mandated antenatal care and served as a nonintervened control group for comparison.
Exhaled carbon monoxide (CO) concentration was also assessed and documented along with questionnaire data at baseline and at each successive follow-up. Exhaled CO provided an objective biological measure of SHS.
2.3. Intervention components
The components of the intervention included direct teaching to enhance knowledge regarding the harms, susceptibility, and severity of exposure to SHS as well as the benefits of avoiding it. Skills related to SHS refusal were taught in the interventions and booklets containing explanations of these skills were distributed. We used role-playing to simulate common difficulties women face when negotiating with their household members about their smoking behavior. The “Values clarification methods” developed by Raths et al[13] were adopted to strengthen self-efficacy and to reinforce decision-making capability. Provocative questions were raised during the intervention to stimulate active thinking and help internalize the knowledge and skills taught in the intervention. The details of the development process and content of the teaching materials can be found elsewhere.[10]
2.4. Measurements
2.4.1. Outcome measures
Self-reported questionnaires measuring health beliefs, self-efficacy, and behavior: this questionnaire contains 86 items – knowledge of SHS (16 items), perceived SHS-related disease susceptibility (13 items), perceived severity of SHS (13 items), perceived barriers (9 items) or benefits related to SHS avoidance (9 items), self-efficacy (8 items), and behavioral responses when facing people who smoke (18 items). Except for the dichotomous items comprising the “knowledge of SHS” construct, the questionnaire contains 5-point Likert items (strongly disagree, disagree, neutral, agree, and strongly agree). The reliability and validity for each construct has been demonstrated in previous research.[10] In our sample, the Cronbach alpha for each construct ranged between 0.80 and 0.95, indicating satisfactory reliability.
Exhaled CO: exhaled CO concentration was used as an objective indicator to measure SHS exposure. Based on estimations from previous studies[14] the cut-off point for SHS exposure was set at 6 ppm. Hence, a CO level of 6 ppm or higher was defined as SHS exposed.
2.4.2. Independent variables
The independent variables in this study included age (<=29, 30–34, and >=35 years), educational attainment (below college, college, and post-graduate), husband's educational attainment (below college, college, and post-graduate), monthly household income (<US $1600, US $1600–US $2200, and >=US $2200), and if the household included any current smokers (yes or no).
2.5. Analytic strategies
We first compared the distribution of baseline sociodemographic characteristics of the 3 study groups using Chi-squared tests. Analysis of variance was used to compare differences in health-beliefs, self-efficacy for rejecting SHS exposure, and behaviors taken to reject SHS among the 3 groups at baseline, 1 month, and 2 months following the conclusion of the intervention. Tukey Honestly Significant Difference test[15] was used as a post hoc test (after performing analysis of variance) to identify specific group differences.
We also assessed the prevalence of exposure to SHS (exhaled CO >= 6 ppm) in our participants at baseline, 1 month, and 2 months after the intervention. The baseline comparison of SHS exposure showed significant differences among the 3 groups (36.0%, 92.0%, and 48.0% in the group-based intervention, individual-based intervention, and treatment-as-usual group, respectively, Chi-squared P < 0.0001). Hence, logistic regression analyses were used to compare SHS exposure status after the intervention while controlling for baseline characteristics (i.e., SHS exposure at baseline, smoking in the household, age, educational attainment, husband's educational attainment, and household income). The Cochran–Armitage χ2 test for trend was used to determine if the intervention effect persisted throughout the follow-up period.
3. Results
Baseline socio-demographic characteristics did not differ significantly in the 3 study groups (Table 1). However, there seemed to be some indication for differences in the prevalence of smoking among household members in the 3 groups (Chi-squared P value = 0.09) with the highest prevalence (78.0%) observed in the individual-based intervention group, the lowest in the group-based intervention group (58.0%), and the treatment-as-usual group falling in the middle (64.0%). This may explain the observed baseline differences in the proportion of SHS exposure measured by the exhaled CO concentration in the 3 groups.
Table 1.
Baseline characteristics of study participants.
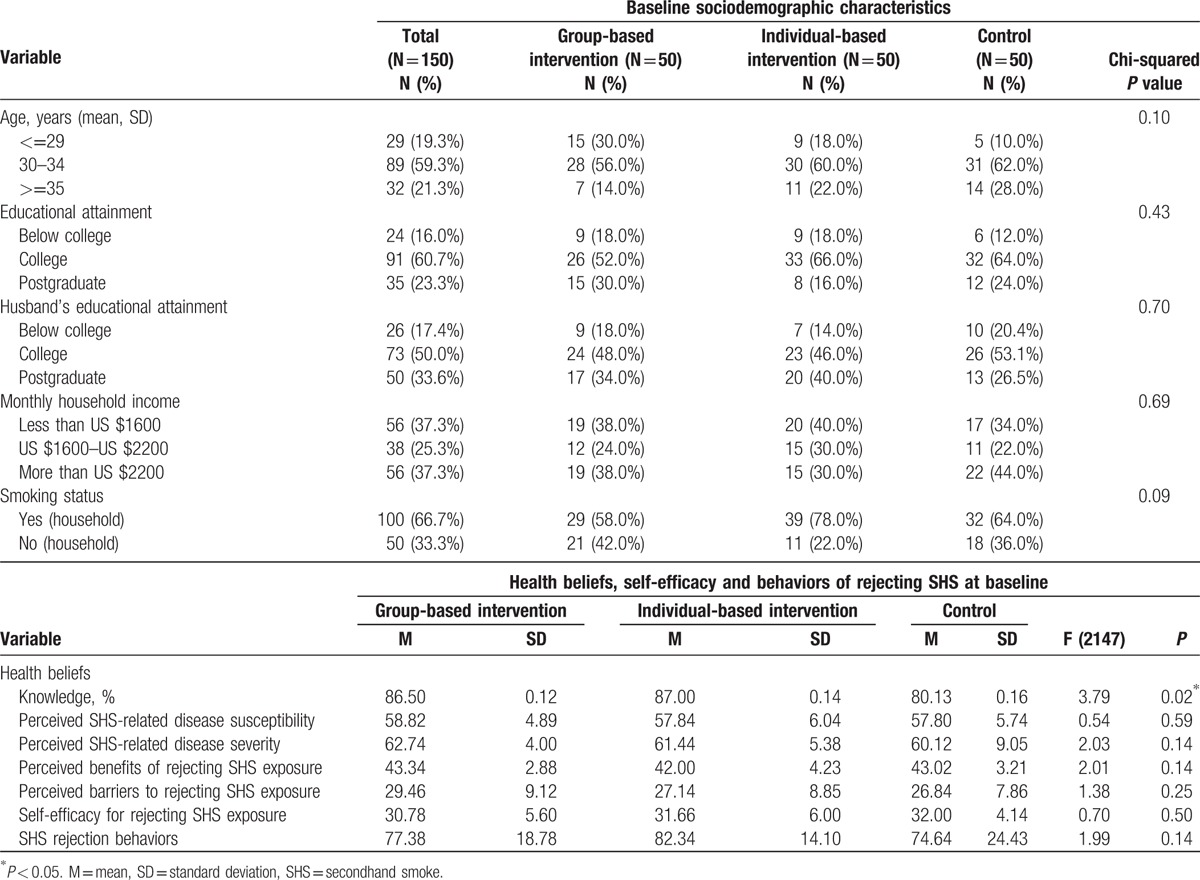
There were no significant differences in baseline health belief constructs, self-efficacy, or SHS rejection behaviors among the 3 groups, except for the “knowledge” construct (Table 1). The treatment-as-usual group had a lower proportion (80%) of correct answers for knowledge regarding SHS than the group-based (86.5%) and individual-based (87.0%) intervention groups (P = 0.02).
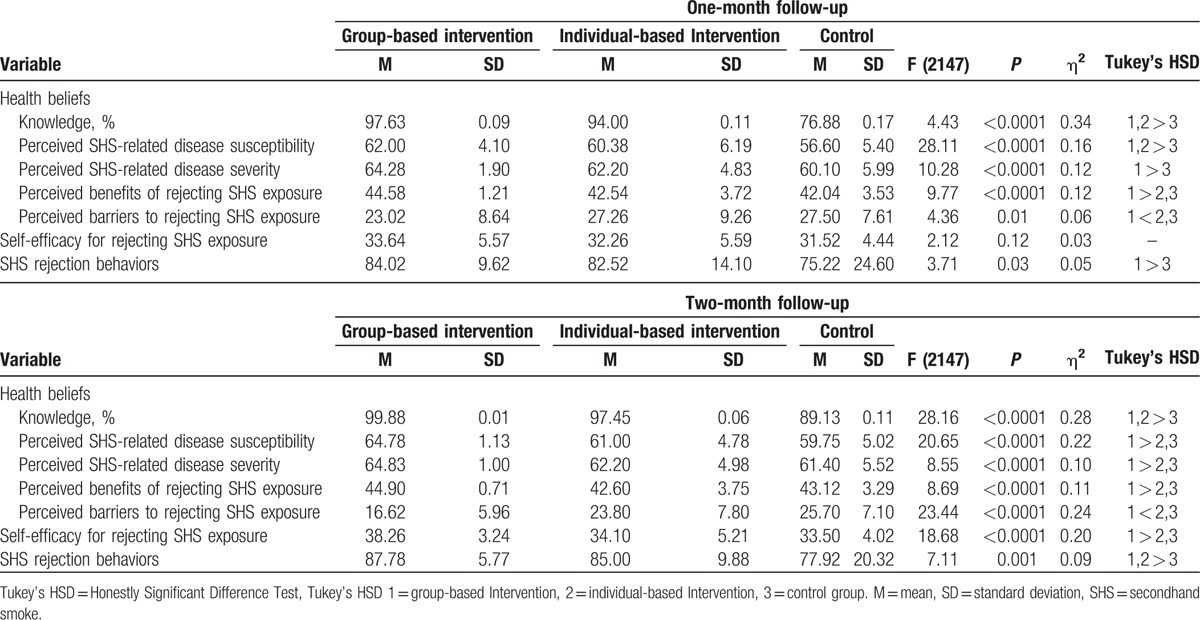
Table 2 shows differences in health beliefs constructs, self-efficacy, and SHS rejection behaviors between the 3 groups 1 and 2 months after the intervention. Overall, both interventions were associated with favorable improvements in all health-belief constructs regarding SHS at the 1- and 2-month follow-ups. However, formal test of statistical significance showed that except for “knowledge” construct, participants in individual-based intervention did not outperform treatment-as-usual group on all other health-belief constructs at 2-month follow-up; group-based participants maintained significantly better in all health-belief constructs 2 months after the intervention (Table 2). The group-intervention performed better than the individual-intervention in terms of self-efficacy for rejecting SHS exposure and SHS behavior. The group-based participants’ self-efficacy for rejecting SHS exposure was statistically greater than that of the treatment-as-usual group at the 2-month follow-up while the individual-based group was not. Furthermore, while both the group- and individual-based intervention groups performed significantly better than the treatment-as-usual group in terms of SHS rejection behaviors at the 2-month follow-up assessment, the group-based participants were already performing significantly better than the treatment-as-usual group by the 1-month follow-up.
Table 2.
Health beliefs, self-efficacy and behaviors of rejecting Second Hand Smoking (SHS) after the intervention.
Using logistic regression analysis, we controlled for potential confounders and baseline differences between the 3 groups to assess the effect of the intervention on SHS exposure based on the exhaled CO concentration (Table 3). At the 1-month follow-up the group-based intervention group was significantly less likely than the control group to be exposed to SHS (odds ratio [OR] = 0.06, 95% confidence interval [95% CI] [0.02–0.21]). Both the group- and individual-based intervention groups were significantly less likely than the control group to be exposed to SHS at the 2-month follow-up (group-based OR [95% CI] = 0.01 [0.001–0.07]; individual-based OR [95% CI] = 0.10 [0.03–0.38]) (Table 3).
Table 3.
Comparative risk of secondhand smoke exposure measured by exhaled CO concentration at the 1- and 2-month follow-ups.
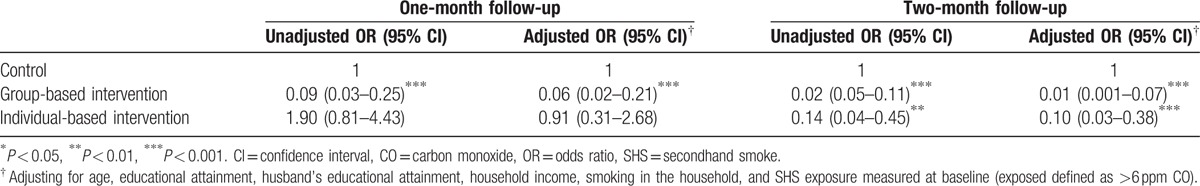
Figure 2 illustrates SHS exposure in the 3 groups at baseline, 1 month, and 2 months following the intervention. The Cochran–Armitage χ2 trend test indicates decreasing trends in SHS exposure in both intervention groups, whereas there was no marked change in SHS exposure in the treatment-as-usual group. A cross-over between the proportion of SHS exposure in the individual-based intervention and the treatment-as-usual group was observed. Participants in the individual-based intervention group began with the highest SHS exposure (92.0% vs 48.0%); however, by the 2-month follow-up, the prevalence of SHS exposure in the individual-based intervention group was lower than the treatment-as-usual group (40.0% vs 56.0%).
Figure 2.
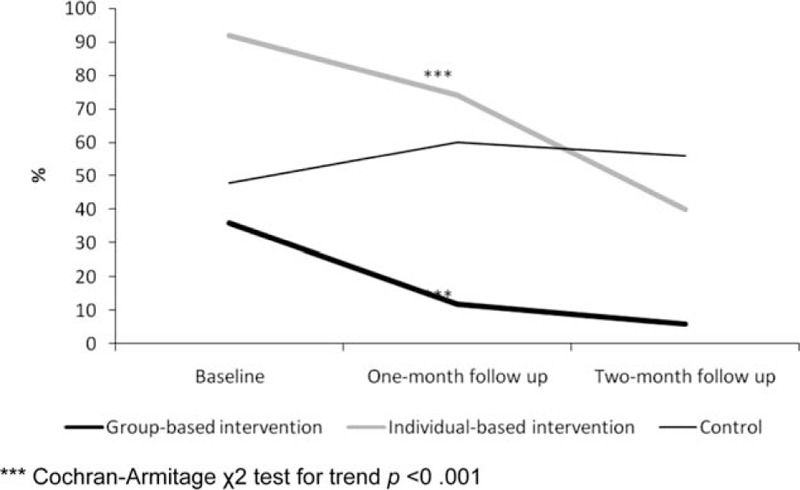
Proportion of Secondhand smoke exposure measured by exhaled carbon monoxide concentration at baseline, 1 month, and 2 months after the intervention.
4. Discussion
4.1. Main findings
In this randomized controlled study, we demonstrated that group- and individual-based educational interventions based on the HBM and self-efficacy theory significantly reduced SHS exposure in pregnant women. The intervention effect remained and even improved at the 2-month follow-up, indicating that the educational programs did not only exert immediate effects, but that the intervention was successful at sustaining behavioral change for at least 2 months following completion of the program. However, the effectiveness of group-based intervention was better than the individual-based intervention; each construct measure was better performed in women allocated to group-based intervention arm. Our study suggests that educational programs based on the expanded HBM can successfully reduce SHS exposure in pregnant women in a country with a very high prevalence of male smoking.
4.2. Strengths and limitations
One important contribution of our study is the provision of valuable information on utilizing a group-based approach to coach pregnant women to help themselves reduce their SHS exposure. Nonetheless, several limitations must be considered in interpreting our results. First, although the allocation to each of the intervention arms was random, simply by chance, group members in the individual-based intervention arm happened to have the highest level of SHS exposure at baseline (Fig. 2). Even though there were no significant differences in socio-demographic characteristics between the 3 groups, the higher prevalence of SHS exposure in the individual-based intervention group may indicate that these 3 groups have intrinsic differences. In our final models assessing the intervention effect on SHS exposure, we adjusted for baseline SHS and socio-demographic variables to take potential intrinsic differences into account. Second, the research focused on the short-term effects of a behavioral change during a 2-month period. Monitoring periods of 12 months or longer would provide more information on the long-term effects of the intervention. Third, the sample is not representative of the general population of pregnant women in Taiwan, and thus caution should be exercised in the generalization of our results.
4.3. Interpretation and comparison with previous studies
Pregnancy is an important life period during which mothers-to-be may be motivated to adopt risk reducing health behaviors to protect the wellbeing of their child.[16] Studies have shown high cessation rates ranging from 30% to 40% in pregnant smokers.[16–20] In many Asian countries, however, the challenges faced by pregnant women are not simply about their own smoking, but their frequent exposure to SHS. For example, in Vietnam, smoking among men is socially acceptable; SHS exposure among pregnant women is widespread.[21] Similarly, in Bangladesh,[22] 46.7% of reproductive-aged women reported exposure to SHS at home. One study applying HBM to help nonsmoking pregnant women to avoid SHS in China; the results were not very encouraging as most pregnant women felt powerless and lacked self-efficacy to stop smokers around them from smoking.[7] Hence, instead of applying the HBM to smoking cession as conducted in many Western countries,[16–19] our current study utilized the theory to help pregnant women refuse exposure to SHS. This innovative approach has rarely been addressed previously.
Existing literature generally focused on individual-based case-by-case interventions.[10,11] The present work provides evidence for the effectiveness of using individual-based, as well as group-delivered health educational interventions to empower and educate pregnant women to refuse SHS. Furthermore, we found the group intervention to perform better than individual-based intervention. The applicability of these findings is immediately apparent given the labor-saving and cost-effectiveness of group interventions.
Potential explanations for the better efficacy of the group-based intervention approach may involve the emotional support received and self-esteem cultivated in the group setting. Previous studies indicate that group interventions promote learning through peer contribution and interaction, a process that provides emotional support to participants through a “togetherness” which strengthens the motivation to take action.[23,24]
Group discussion also conveys ideas and thoughts shared by other group members. This reaffirms and reassures individuals imbuing them with a sense of value in the group.[25,26] Nevertheless, as mentioned in our limitations section, by chance, the participants in the group-intervention arm seemed to have a lower overall exposure to SHS before the intervention, indicating that there may be some intrinsic differences in the 3 groups. We are not able to completely rule out the possibility that the group-intervention arm performed better because this group was already predisposed to SHS avoidance behavior, or that they lived in circumstances better suited to avoid SHS exposure than their counterparts, and hence were more responsive to intervention. However, the significant decrease in SHS exposure and the changes in knowledge, attitude, and behaviors toward SHS still strongly suggest the utility of a group-based educational program in enhancing the knowledge and capability of pregnant women to refuse SHS.
The HBM model posits that once an individual is provided with adequate information (e.g., they are susceptible to smoking-related diseases, and these diseases have serious consequences), he or she will adopt health-improving behaviors.[9] Based on the HBM, our current approach assumes that pregnant women bear the responsibility of avoiding and resisting SHS exposure as long as they have adequate knowledge, have an available course of action, and perceive that the benefits of taking action outweigh the costs. However, it should be noted that in many patriarchal societies where male smoking is prevalent, women may have limited capacity to negotiate tobacco use with their husbands and fathers-in-law, as women are located on the lowest rung of the power ladder of the family.[27,28] Women's status has been improving in Taiwan over the past several decades.[29] Based on the composite Gender Inequality Index compiled by the United Nations, Taiwan outperforms all other Asian neighbors.[30] Better gender equity in Taiwan may be an important contributing factor to the success of the intervention program.
5. Conclusion
Our randomized controlled study has demonstrated the efficacy of applying the expanded HBM to design health educational interventions and materials to assist pregnant women refuse being exposed to SHS. The education can be delivered either individually or through a group; both approaches were effective. However, our results indicate that group-based health education confers better efficacy than individual-based intervention. This finding is quite encouraging, as group-based intervention is more cost-effective, less labor-intensive, and can be used to build a smoke-free home and reach a wider audience. Our findings suggest that policy makers should consider including SHS refusal tactics based on the expanded HBM as an integral part of antenatal classes. Our interventions among pregnant women exposed to SHS are viewed as a breakthrough point to achieve the goal of a smoke-free home, could provide the foundation for these programs, and strive to change the culture around pregnant women. This may be particularly useful in many Asian countries where pregnant women and their babies are oftentimes exposed to the hazards of SHS.
Acknowledgements
The authors thank Ministry of Science and Technology, ROC (Grant number: MOST 103-2314-B-532-003-MY2) and the Department of Health, Taipei City Government (Grant number: 10401-62-011 to Y-YC); and Department of Health, Taipei City Government (Grant number: 10102-62-085 to Y-CC) for the support.
Footnotes
Abbreviations: CO = carbon monoxide, HBM = Health Belief Model, OR = odds ratio, SHS = secondhand smoke, TCH = Taipei City Hospital.
Authorship: YCC and YYC were involved in the framing of the research questions, planning and conduct of the analysis, reporting of the research results, and drafting of the first version of the paper; FS, PSFY, and JLC analyzed the research data and drafted tables; they also critically revised the first version of the paper; and YYC, as guarantor of the paper, contributed to proposing the initial research scheme, conducting the initial analysis, monitoring the research process, and revisions of the paper.
What this study adds?
The current randomized controlled study demonstrates the efficacy of applying the expanded HBM (Health Belief Model) to help pregnant women in Taiwan reduce their exposure to SHS (second hand smoking).
The expanded HBM intervention program can be delivered either individually or through group sessions; both approaches were effective. However, our results indicate that group-based health education confers better efficacy than individual-based intervention.
The intervention was successful at sustaining behavioral change for at least 2 months following completion of the program.
Funding/support: This study was funded by Ministry of Science and Technology, ROC (Grant number: MOST 103-2314-B-532-003-MY2) and the Department of Health, Taipei City Government (Grant number:10401-62-011) to Y-YC; and Department of Health, Taipei City Government (Grant number: 10102-62-085) to Y-CC.
The authors have no conflicts of interest to disclose.
References
- 1.WHO. WHO Report on the Global Tobacco Epidemic: Warning About the Dangers of Tobacco. 2009. [Google Scholar]
- 2.Leonardi-Bee J, Britton J, Venn A. Secondhand smoke and adverse fetal outcomes in nonsmoking pregnant women: a meta-analysis. Pediatrics 2011; 127:734–741. [DOI] [PubMed] [Google Scholar]
- 3.Hackshaw A, Rodeck C, Boniface S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls. Hum Reprod Update 2011; 17:589–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health Promotion Administration MoHaW. Health Promotion Administration Annual Report 2014, Chapter 3, 36–42. Taipei, 2014. [Google Scholar]
- 5.Lai MC, Chou FS, Yang YJ, et al. Tobacco use and environmental smoke exposure among Taiwanese pregnant smokers and recent quitters: risk perception, attitude, and avoidance behavior. Int J Environ Res Public Health 2013; 10:4104–4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin PL, Huang HL, Lu KY, et al. Second-hand smoke exposure and the factors associated with avoidance behavior among the mothers of pre-school children: a school-based cross-sectional study. BMC Public Health 2010; 10:606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee AH. A pilot intervention for pregnant women in Sichuan, China on passive smoking. Patient Educ Couns 2008; 71:396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schane RE, Prochaska JJ, Glantz SA. Counseling nondaily smokers about secondhand smoke as a cessation message: a pilot randomized trial. Nicotine Tob Res 2013; 15:334–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glanz K, Rimer BK, Viswanath K. Models of Individual Health Behavior. 4th. PublisherJossey-Bass, San Francisco, CA: Health Behavior and Health Education: Theory, Research, and Practice; 2008. [Google Scholar]
- 10.Chi YC, Wu CL, Chen CY, et al. Randomized trial of a secondhand smoke exposure reduction intervention among hospital-based pregnant women. Addict Behav 2015; 41:117–123. [DOI] [PubMed] [Google Scholar]
- 11.Kazemi A, Ehsanpour S, Nekoei-Zahraei NS. A randomized trial to promote health belief and to reduce environmental tobacco smoke exposure in pregnant women. Health Educ Res 2012; 27:151–159. [DOI] [PubMed] [Google Scholar]
- 12.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: L. Erlbaum Associates; 1988. [Google Scholar]
- 13.Raths LE, Harmin M, Simon S. Values and Teaching. 2nd ed.Columbus, OH: Charles E. Merrill; 1978. [Google Scholar]
- 14.Issa JS, Abe TM, Pereira AC, et al. The effect of Sao Paulo's smoke-free legislation on carbon monoxide concentration in hospitality venues and their workers. Tob Control 2011; 20:156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zar J. Biostatistical Analysis. 4th edNew Jersey, Englewood Cliffs: Prentice-Hall; 1999. [Google Scholar]
- 16.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res 2003; 18:156–170. [DOI] [PubMed] [Google Scholar]
- 17.Ussher M, Lewis S, Aveyard P, et al. Physical activity for smoking cessation in pregnancy: randomised controlled trial. BMJ 2015; 350:h2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richmond R. You’ve come a long way baby: women and the tobacco epidemic. Addiction (Abingdon, England) 2003; 98:553–557. [DOI] [PubMed] [Google Scholar]
- 19.Chamberlain C, O’Mara-Eves A, Oliver S, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev 2013; 10:Cd001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Floyd RL, Rimer BK, Giovino GA, et al. A review of smoking in pregnancy: effects on pregnancy outcomes and cessation efforts. Ann Rev Public Health 1993; 14:379–411. [DOI] [PubMed] [Google Scholar]
- 21.Minh HV, Giang KB, Xuan TT. Exposure to second-hand smoke at home and its associated factors: findings from the Global Adult Tobacco Use survey in Vietnam, 2010. Cancer Causes Control 2012; 23 suppl 1:99–107. [DOI] [PubMed] [Google Scholar]
- 22.Fischer F, Minnwegen M, Kaneider U, et al. Prevalence and determinants of secondhand smoke exposure among women in Bangladesh, 2011. Nicotine Tob Res 2015; 17:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riemsma RP, Taal E, Rasker JJ. Group education for patients with rheumatoid arthritis and their partners. Arthritis Rheum 2003; 49:556–566. [DOI] [PubMed] [Google Scholar]
- 24.Wilson SR. Individual versus group education: is one better? Patient Educ Couns 1997; 32 (1 Suppl):S67–S75. [DOI] [PubMed] [Google Scholar]
- 25.Calzone KA, Prindiville SA, Jourkiv O, et al. Randomized comparison of group versus individual genetic education and counseling for familial breast and/or ovarian cancer. J Clin Oncol 2005; 23:3455–3464. [DOI] [PubMed] [Google Scholar]
- 26.Lepore SJ, Helgeson VS, Eton DT, et al. Improving quality of life in men with prostate cancer: a randomized controlled trial of group education interventions. Health Psychol 2003; 22:443–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Balbach ED, Smith EA, Malone RE. How the health belief model helps the tobacco industry: individuals, choice, and “information”. Tob Control 2006; 15 suppl 4:iv37–iv43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Slote WH, Vos GAD. Confucianism and the Family. Albany, NY: State University of the New York, SUNY Press; 1998. [Google Scholar]
- 29.Greaves LJ, Hemsing NJ. Sex, gender, and secondhand smoke policies: implications for disadvantaged women. Am J Prev Med 2009; 37 (2 Suppl):S131–S137. [DOI] [PubMed] [Google Scholar]
- 30.National Statistics RoCT. Based on the UN's definition and methodology, detailed GII data of Taiwan can be obtained on the Internet website. 2015; http://eng.stat.gov.tw/ct.asp?xItem=25280&ctNode=6032&mp=5 [Accessed August 24, 2016]. [Google Scholar]


