Abstract
Our study sought to review our experience from biportal to uniportal video-assisted thoracoscopic surgery (VATS) major lung resection. Lessons we learned from the evolution regarding technical aspects were also discussed.
We retrospectively reviewed patients who underwent VATS lobectomy or segmentectomies in Ditmanson Medical Foundation Chia-Yi Christian Hospital, Chia-Yi, Taiwan, during January 2012 and December 2014. Patient clinical profiles, surgical indications and procedures, postoperative course, and oncological parameters were analyzed and compared between the biportal and uniportal groups.
A total of 121 patients were enrolled in this study with median follow-up of 19.5 ± 11.6 months for all patients and 22.5 ± 11.5 months for primary lung cancer patients. Operation time (146.1 ± 31.9–158.7 ± 40.5 minutes; P = 0.077), chest drainage time (3.8 ± 3.3–4.4 ± 2.4 days; P = 0.309), conversion to thoracotomy rate (2.2%–2.6%; P = 0.889), and complication rate (15.6%–19.7%; P = 0.564) were equal between the groups, whereas blood loss (96.7 ± 193.2–263.6 ± 367; P = 0.006) was lower in the uniportal group. For lung cancer cases, there were no statistical differences in the histology, cancer staging, mediastinal lymph node dissection stations, numbers of dissected N1, N2, and overall lymph nodes between uniportal and biportal groups.
Our preliminary data showed that uniportal VATS anatomical lung resection is as feasible, equally safe, and of comparative oncological clearance efficacy to biportal VATS.
Keywords: biport, lobectomy, segmentectomy, single-port, uniport, video-assisted thoracoscopic surgery
1. Introduction
For the past 20 years, video-assisted thoracoscopic surgery (VATS) has become the major method for invasive diagnosing or resecting pulmonary and mediastinal diseases, because VATS offers lower postoperative pain, and better cosmetics and recovery for patients.[1–3] The pursuit for ultimate minimal invasiveness keeps driving the evolution of VATS from traditional VATS (1-utility mini-thoracotomy with 2–3 instrument access ports) to biportal VATS (utility mini-thoracotomy with another additional thoracoscopic port), eventually to uniportal (only 1-utility thoracotomy) for all instrumentation, camera position, and specimen retrieval. Yamamoto et al[4] and Rocco et al[5] were the first to introduce uniportal VATS into pleural biopsy or minor lung resections. Gonzalez-Rivas et al utilized the uniportal VATS in series of major lung resection, including lobectomy, segmentectomies, and even complex procedures, like double-sleeve lobectomy.[6,7] Nevertheless, the comparison between biportal and uniportal VATS in anatomical lung resections were barely reported. We herein reviewed our experience of biportal and uniportal VATS anatomic pulmonary resection in this study.
2. Patients and methods
We retrospectively reviewed patients who underwent VATS anatomical lung resection, including lobectomy and segmentectomy, by a single surgeon, during January 2012 and December 2014, at Ditmanson Medical Foundation Chia-Yi Christian Hospital, Chia-Yi, Taiwan. The study was reviewed and approved by the Institutional Ethical Committee of the hospital, and individual patient consent was waived.
In our institute, triportal VATS (one 3–5-cm utility thoracotomy at 4th intercostal space (ICS), anterior axillary line with another two 11–12-mm working ports at 6–7th ICS, anterior and posterior axillary lines) gradually replaced traditional posterolateral thoracotomy approach for major lung resections in 2007. As technique and instruments refined, we shifted to biportal technique in 2009 and it became our standard approach for most VATS procedures. In April 2013, we began our uniportal VATS set-up. So far, we had performed more than 300 biportal and over 100 uniportal VATS lobectomies and segmentectomies. Over 90% VATS major lung resections were performed using uniportal approach for the recent 1 year.
All patients underwent complete preoperative evaluation including chest computed tomographic scan and pulmonary function test. Our uniportal VATS and biportal VATS anatomic resection shared the same indications, and were as follows: tumor diameter no greater than 5 cm; without great vessel or tracheobronchial invasions; without chest wall invasion; and patient tolerable to 1-lung ventilation.
2.2. Anesthesia and operation setting
All operations were performed after double-lumen endotracheal intubation, and patients were placed in lateral decubitus position. The operator always stood in front of the patient.
2.3. Incision and approaches
For biportal approach, one 3 to 4-cm utility thoracotomy was made at the 4th ICS, anterior axillary line, with another 11 to 12-mm working port at the 6 to 7th ICS, middle axillary line. For uniportal VATS, only a 3 to 4-cm incision wound was made at the 5th ICS, anterior axillary line. A wound protector was routinely used. All surgical instruments were exactly the same for both approaches. The operator used harmonic scalpel and curved specialized thoracoscopic instruments (Scanlan) for dissection and traction; the assistant controlled the thoracoscope and curved sucker to offer proper counter-traction and suction. We preferred 10 mm 30∘thoracoscope and high-definition imaging system. Vascular and bronchial divisions were performed using articulated endostapler with sometimes curved-tip ones if difficult angles were encountered, or occasional hand-sewn ligation. When the resection was completed, the specimen was removed in a retrieval bag. We proceeded to mediastinal lymph node dissection (MLND) in cases of primary lung cancer according to current National Comprehensive Cancer Network's (NCCN) guideline of minimum of 3 N2 lymph node (LN) stations.[8] Finally, the wound was closed with a single 20 to 24-Fr. chest tube placed in the middle.
2.4. Postoperative management
Patients would be extubated immediately after the operation in the operation room or later on the same day in the intensive care unit (ICU). The chest drain would be removed 2 to 4 days after air leak was sealed and lung expansion was observed on chest film.
Clinical parameters were recorded, including patient sex, age, comorbidities, and preoperative pulmonary function. Operative data including surgical procedures, operation time, blood loss, and lesion distribution; postoperative course including ICU duration and postoperative hospital stay; and complications such as prolonged air leak (defined as air leak >5 days) and mortality were assessed. Oncological efficacy including tumor histology, staging, pT, pN status, and dissected N1 and N2 LN stations and numbers were also analyzed.
2.5. Statistical analysis
To analyze differences between uniportal and biportal VATS groups, continuous data are presented as means ± SD and analyzed by the 2-tailed Student t test. Categorical variables were presented as counts with percentages, and analyzed using the chi-square or Fisher exact tests. A P value <0.05 was taken to indicate statistical significance. All data analyses were performed using SPSS software (SPSS 22.0 for Windows, SPSS Inc, Chicago, IL).
3. Result
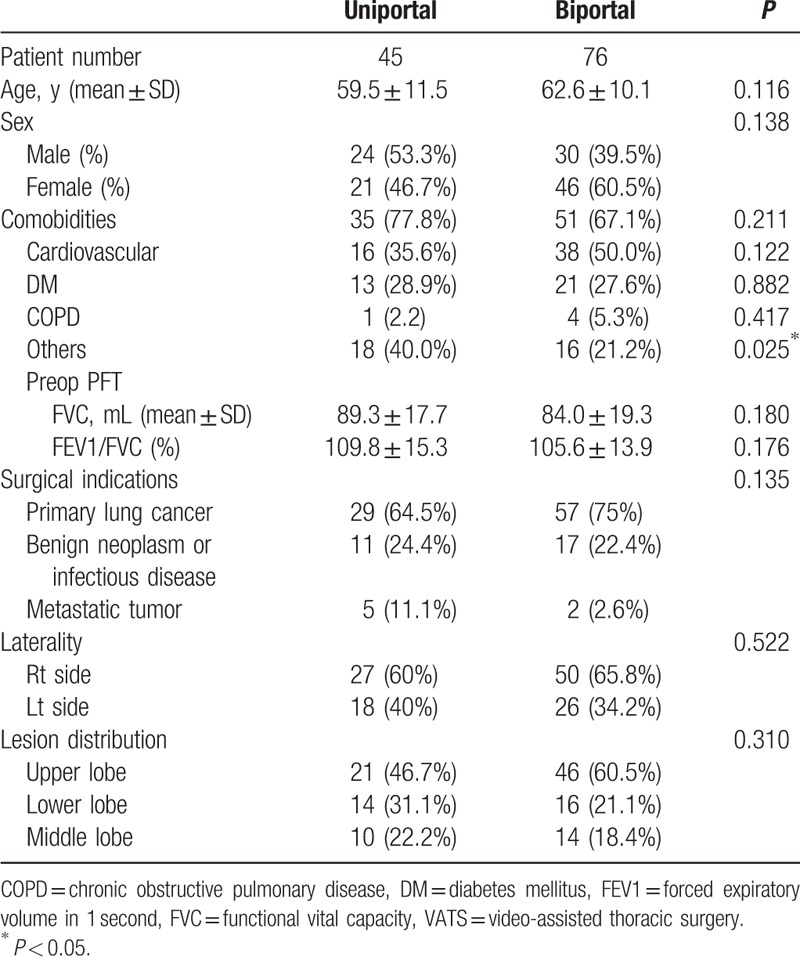
During January 2012 and December 2014, in all, 121 consecutive patients who underwent VATS lobectomy or segmentectomy were enrolled in this study. Of the 121 patients, 76 (62%) were performed with biportal VATS and 45 (38%) with uniportal VATS. The median follow-up period was 19.5 ± 11.6 months for all patients and 22.5 ± 11.5 months for primary lung cancer patients. Comparing the uniportal and biportal VATS, there were no differences in patient sex, age (59.5 ± 11.5–62.6 ± 10.1 years; P = 0.116), comorbidities, and preoperative pulmonary functions. Primary lung cancer was the most common indication (89, 69.9%) for VATS anatomic resection for both groups. There were no statistical differences between the 2 groups regarding surgical indications, operation laterality, lesion distribution, and tumor size, as shown in Table 1.
Table 1.
Clinical demographics of all 121 patients who underwent VATS major pulmonary resection.
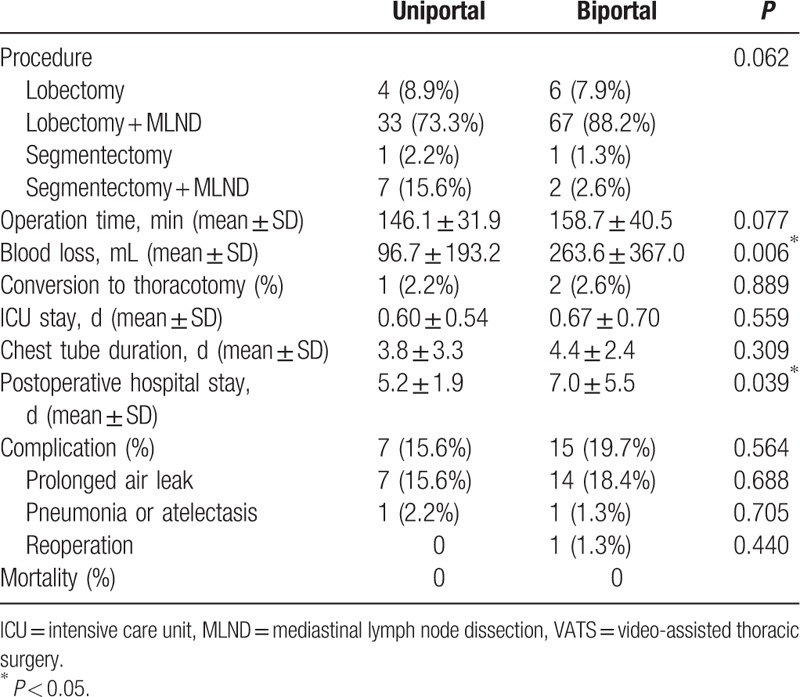
Comparison of perioperative parameters between the 2 groups is shown in Table 2. For surgical procedures, procedure distribution including lobectomies or segmentectomies with and without MLND was similar between uniportal and biportal groups, and also the mean operative time (146.1 ± 31.9–158.7 ± 40.5 minutes; P = 0.077). Blood loss (96.7 ± 193.2–263.6 ± 367 mL; P = 0.006) was lower in uniportal than in biportal group. There was 1 conversion to mini-thoracotomy in the uniportal group (2.2%) and 2 cases (2.6%) in the biportal group (P = 0.889). No differences in postoperative ICU duration (0.60 ± 0.54–0.67 ± 0.70 days; P = 0.559) and chest drainage indwelling time (3.8 ± 3.3–4.4 ± 2.4 days; P = 0.309), but shorter hospital stay with uniportal VATS (5.2 ± 1.9–7.0 ± 5.5 days; P = 0.039) were observed. Overall complication rate was equal (15.6%–19.7%; P = 0.564), and there were no differences regarding prolonged air leak (15.6%–18.4%; P = 0.688) and lung atelectasis or pneumonia (2.2%–1.3%; P = 0.705) between the 2 groups. There was only 1 complication of bronchopleural fistula requiring reoperation due to cavitary tuberculosis and uncontrolled diabetes for fistula repair with thoracoplasty in the biportal group. There was no mortality in this study.
Table 2.
Operative characteristics of all 121 patients who underwent VATS anatomic pulmonary resection.
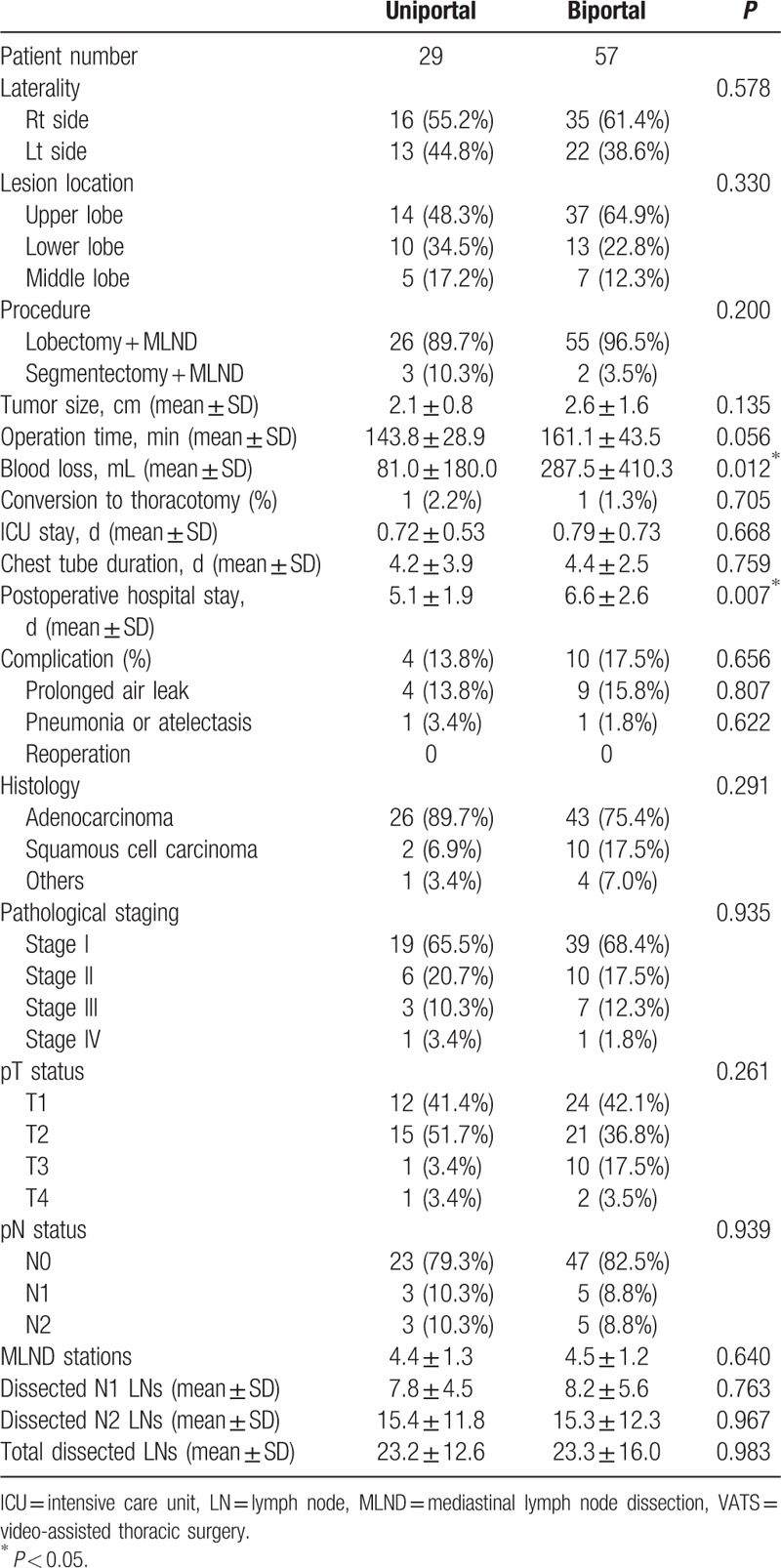
In our series, there were a total of 86 primary lung cancer cases, and analysis between biportal and uniportal approaches among them is detailed in Table 3. We found equal lesion laterality and location distribution. There was no statistical difference regarding surgical procedures of lobectomy + MLND (89.7%–96.5%; P = 0.200) or segmentectomies + MLND (10.3%–3.5%; P = 0.200), nor was the tumor size (2.1 ± 0.8–2.6 ± 1.6 cm; P = 0.135). Further analysis for the tumor histology showed same pattern, with adenocarcinoma being the most common (89.7%–75.4%; P = 0.656), followed by squamous cell carcinoma (6.9%–17.5%). The pathological staging, and pT and pN status distributions were equal between the groups. For oncological clearance efficacy analysis, we compared the numbers of dissected overall LNs and LN stations. Our data revealed no differences in MLND stations, numbers of dissected N1 and N2, and overall LNs between the uniportal and the biportal groups.
Table 3.
Comparison of total of 86 primary lung cancer cases who underwent VATS anatomical resection.
4. Discussion
Over the past 20 years, from standard thoracotomy to VATS approach, it has been a giant step for thoracic surgeons to explore, practice, and master the new endoscopic surgical techniques due to the major difference in eye-to-hand coordination. By means of well-designed endoscopic instruments and high-definition imaging system, VATS has been applied to virtually all thoracic surgeries including lung, esophagus, and mediastinal operations.[9,10]
Classical VATS was usually performed using one 3 to 5-cm utility thoracotomy with 2 to 3 additional small working ports for thoracoscopy.[11] Among the VATS pioneers, McKenna et al[11] published in 2006 the largest triportal VATS lobectomies of more than 1100 cases with low morbidity and low mortality rate, showing the VATS major lung resection to be not only safe and feasible but also as a standard procedure. Few years later, the procedure was refined to biportal maneuver, with only 1 working port left for thoracoscopy and the operator controlling most of the dissection and traction himself via the utility mini-thoracotomy. D’Amico et al had the largest biportal VATS series of more than 600 cases of lobectomy and segmentectomies, showing not only fewer complication rate but also competitive MLND, compared with thoracotomy.[12–14] However, surgeon's ambition to seek for ultimate invasiveness did not cease here. The uniportal VATS, almost the last piece to the evolution of VATS, matured from initially a modality for diagnostic and minor surgical procedures only, to practical level for routine lobectomy or even complicated vascular and bronchial reconstructions by Dr Gonzalez-Rivas for the recent 5 years.[6,7]
The VATS evolution in our institute matched the worldwide trend. Our preliminary result showed uniportal VATS to be feasible and equally safe to biportal VATS, with no differences in operation time, conversion rate, chest drainage time, ICU period, and slightly favorable postoperative hospital stay, and relative low complication rate, considering similar disease and patient distribution. The slightly improved postoperative recovery might be due to improved wound pain, although some reviews of retrospective studies failed to show explicit advantages of uniportal over multiportal VATS.[15,16] For significantly more blood loss in biportal VATS, reasonable explanation would be due to 6 cases of outliners with 3 patients of unexpected dense extensive pleural adhesion and oozing after pneumolysis; and 3 patients with calcified LNs encasing bronchial branches, causing pulmonary artery injury during dissection, and in 2 of them, conversion to mini-thoracotomy was required for bleeding control.
Regarding the fundamental oncological clearance for lung cancer, although questioned by some authors,[17] it has been shown that VATS lobectomy is comparative with open thoracotomy, not only in MLND stations and overall numbers but also in long-term survival.[14,18,19] Few early studies, including that by Gonzalez-Rivas et al and Liu et al, had shown competitive MLND result with uniportal VATS to multiportal VATS.[20–22] Our preliminary data supported this by showing equal cancer stage distribution and comparative MLND not only in N1, N2, and overall LN numbers but also in station numbers, between uniporal and biportal VATS groups. However, the long-term prognosis of uniportal VATS lobectomy for lung cancer still remained unclear and its efficacy mandates years of follow-up to come. Moreover, whether or not it merits over uniportal VATS regarding patient aesthetics, short-term wound pain, or long-term allodynia or hypaesthesia, and possible socioeconomic effect, also awaits further exploration.
Evolution from multiportal to biportal, then to uniportal VATS, it might seem intuitive just to reduce unnecessary working ports in the beginning; however, there are several major differences for technical considerations. The first issue is the operation field perspective. For traditional triportal VATS, the thoracoscope, and the surgeon's left and right-hand instruments formed a triangle, and the 3 aimed to the same vanishing point; therefore the 3 axes were maintained independent without interference. For biportal technique, all instrumentations are usually through the utility thoracotomy, and the surgeon's both-hands axes are turned more perpendicular to the visual axis; the enhanced eye-to-hand inconsistency might compromise delicate hand motions, and yet, could only be compensated by operator's own inner adjustment. However, for uniportal VATS, the axes of thoracoscopic view and instrumentations are parallel. This simulates the direct vision under open thoracotomy maneuver, and the eye-to-hand inconsistency would be the lowest among the 3 approaches; hence, this could facilitate more technically-demanding procedures (illustrated in Fig. 1.) This was proposed to be the major advantage of uniportal VATS.[23] The second is the limited flexibility of instrument circulation. For multiportal and biportal VATS, the camera and instruments could be placed among the utility thoracotomy and ports for ease of dissection and stapling in case of difficult angle, which is contrary to the case of uniportal VATS. In addition, due to single small incision and limited ICS, the inevitably intense jamming and interference among thoracoscope and instruments could be expected; hence, this was claimed the major disadvantage of uniportal VATS.[23] Based on what we learned from our experiences, we herein make a few suggestions: thoracotomy site design would be preferred to be located at fifth ICS, anterior axillary line to avoid difficult angle during stapling of hilum structure, especially superior pulmonary vein; longitudinal instrumentation alignment to avoid mutual collision inside the utility thoracotomy with thoracoscope at upmost posterior tip, often the endo-stapler at the bottom, and other instruments in between; utilization of thin, narrow, and sometimes articulated endoscopic instrument and stapler, especially of variable lengths, together to avoid fencing of the instrument hand pieces and the camera (Fig. 2).
Figure 1.
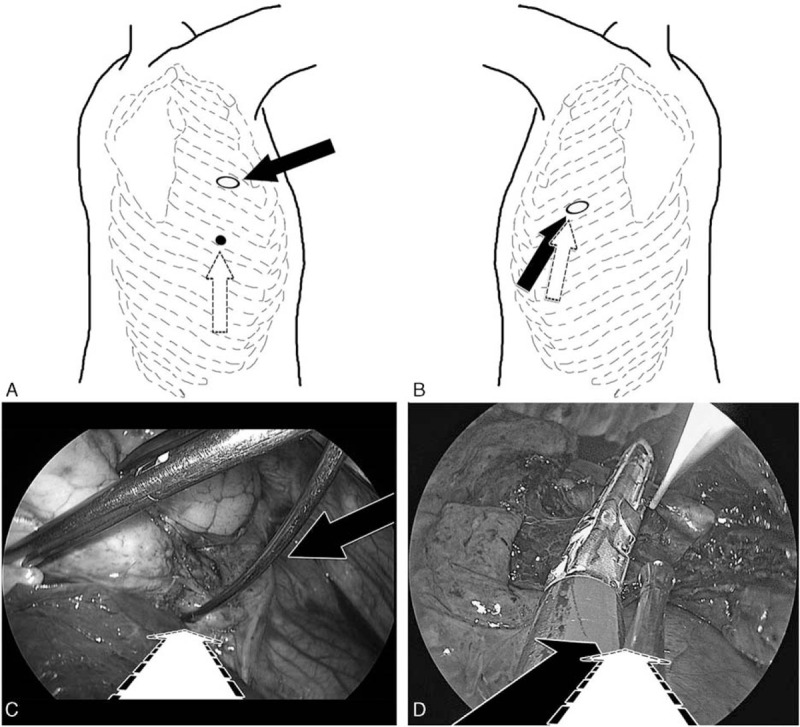
Surgical perspective differences between biportal and uniportal VATS lobectomy. A, Incision location of biportal VATS with one 3 to 4-cm mini-thoracotomy at fourth ICS for instrumentation (black arrow) and thoracoscopy port at sixth ICS (white dashed arrow). B, Actual biportal VATS intraoperative view showing the instrumentation axis (black arrow) is more perpendicular to the thoracoscopic view axis (white dashed arrow), leading to eye-to-hand inconsistency. C, uniportal VATS with one 3 to 4-cm incision at fifth ICS for both instrumentation (black arrow) and thoracoscopy (white dashed arrow). D, Actual uniportal VATS intraoperative view showing the vision axis (black arrow) paralleling instrumentation axis (white dashed arrow). ICS = intercostal space, VATS = video-assisted thoracoscopic surgery.
Figure 2.
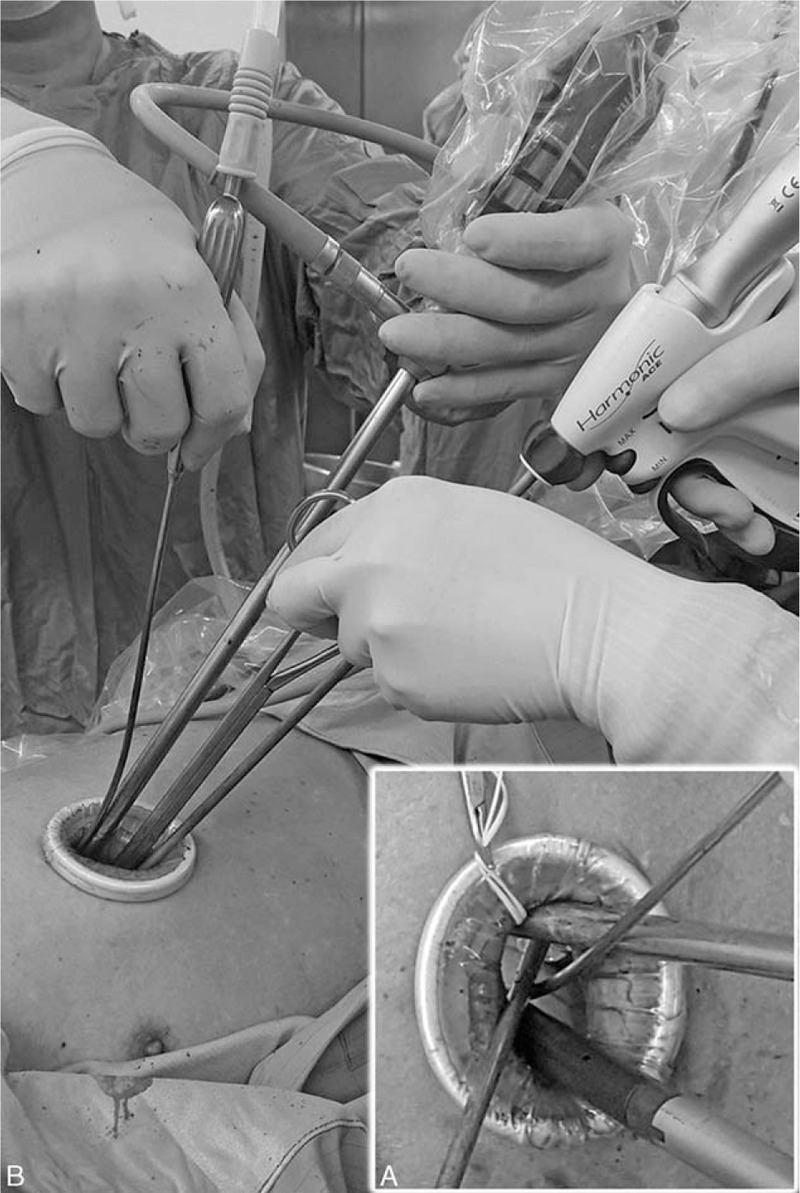
Uniportal VATS instrumentation. A, Longitudinal alignment at utility thoracotomy inlet with thoracoscopy at dorsal tip, endo-stapler at the ventral tip of incision, and the other instruments in between to avoid jamming at wound entry site. B, Sector-shape distribution with instruments of variable lengths to avoid fencing of the hand pieces and the camera. VATS = video-assisted thoracoscopic surgery.
There were several limitations of this study. First, the follow-up time period was limited due to its retrospective review basis. Second, the sample size of the patients was relatively small. Third, subjective surgeon's preference may influence the selection of the procedures.
In conclusion, our results showed that uniportal VATS is as safe, feasible, and effective method as biportal VATS in major lung resection.
Footnotes
Abbreviations: COPD = chronic obstructive pulmonary disease, DM = diabetes mellitus, ICS = intercostal space, ICU = intensive care unit, LN = lymph node, MLND = mediastinal lymph node dissection, NCCN = National Comprehensive Cancer Network, VATS = video-assisted thoracic surgery.
J-MC, K-HK, W-WL, and DG-R contributed equally to this work.
The authors declared no conflicts of interest.
References
- 1.Lewis RJ, Caccavale RJ, Sisler GE, et al. Video-assisted thoracic surgical resection of malignant lung tumors. J Thorac Cardiovasc Surg 1992; 104:1679–1685.[discussion 1685–1677]. [PubMed] [Google Scholar]
- 2.Palade E, Guenter J, Kirschbaum A, et al. [Postoperative pain in the acute phase after surgery: VATS lobectomy vs. open lung resection: results of a prospective randomised trial]. Zentralblatt fur Chirurgie 2014; 139 suppl 1:S59–S66. [DOI] [PubMed] [Google Scholar]
- 3.Higuchi M, Yaginuma H, Yonechi A, et al. Long-term outcomes after video-assisted thoracic surgery (VATS) lobectomy versus lobectomy via open thoracotomy for clinical stage IA non-small cell lung cancer. J Cardiothorac Surg 2014; 9:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998; 133:145–147. [DOI] [PubMed] [Google Scholar]
- 5.Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013; 96:434–438. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections dagger. Eur J Cardiothorac Surg 2016; 49 suppl 1:i6–i16. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011; 12:514–515. [DOI] [PubMed] [Google Scholar]
- 8.Ettinger DS, Wood DE, Akerley W, et al. National comprehensive cancer n. Non-Small Cell Lung Cancer, Version 6.2015. J Natl Comprehens Cancer Netw 2015; 13:515–524. [DOI] [PubMed] [Google Scholar]
- 9.Sihag S, Kosinski AS, Gaissert HA, et al. Minimally invasive versus open esophagectomy for esophageal cancer: a comparison of early surgical outcomes from the Society of Thoracic Surgeons National Database. Ann Thorac Surg 2016; 101:1288–1289. [DOI] [PubMed] [Google Scholar]
- 10.Xie A, Tjahjono R, Phan K, et al. Video-assisted thoracoscopic surgery versus open thymectomy for thymoma: a systematic review. Ann Cardiothorac Surg 2015; 4:495–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKenna RJ, Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006; 81:421–425.[discussion 425–426]. [DOI] [PubMed] [Google Scholar]
- 12.Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006; 244:420–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009; 138:419–425. [DOI] [PubMed] [Google Scholar]
- 14.D’Amico TA, Niland J, Mamet R, et al. Efficacy of mediastinal lymph node dissection during lobectomy for lung cancer by thoracoscopy and thoracotomy. Ann Thorac Surg 2011; 92:226–231.[discussion 231–222]. [DOI] [PubMed] [Google Scholar]
- 15.Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg 2015; 20:550–555. [DOI] [PubMed] [Google Scholar]
- 16.Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015; 20:409–414. [DOI] [PubMed] [Google Scholar]
- 17.Denlinger CE, Fernandez F, Meyers BF, et al. Lymph node evaluation in video-assisted thoracoscopic lobectomy versus lobectomy by thoracotomy. Ann Thorac Surg 2010; 89:1730–1735.[discussion 1736]. [DOI] [PubMed] [Google Scholar]
- 18.Sugi K, Kaneda Y, Esato K. Video-assisted thoracoscopic lobectomy achieves a satisfactory long-term prognosis in patients with clinical stage IA lung cancer. World J Surg 2000; 24:27–30.[discussion 30–21]. [DOI] [PubMed] [Google Scholar]
- 19.Berry MF, D’Amico TA, Onaitis MW, et al. Thoracoscopic approach to lobectomy for lung cancer does not compromise oncologic efficacy. Ann Thorac Surg 2014; 98:197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Delgado Roel M, Fieira Costa EM, Gonzalez-Rivas D, et al. Uniportal video-assisted thoracoscopic lymph node dissection. J Thorac Dis 2014; 6 suppl 6:S665–S668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015; 261:793–799. [DOI] [PubMed] [Google Scholar]
- 22.Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique? Eur J Cardiothorac Surg 2016; 49 suppl 1:i64–i72. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013; 95:426–432. [DOI] [PubMed] [Google Scholar]


