Abstract
Objective
To compare length of stay, functional status, and discharge destination between individuals who fell during in-patient stroke rehabilitation and those who did not fall.
Design
Retrospective cohort study.
Setting
Rehabilitation hospital.
Participants
Individuals who fell during in-patient stroke rehabilitation (n=106; fallers group; mean age=67.8 years, SD=12.9; mean time post-stroke=26.4 days, SD=28.3) were matched to individuals who did not fall (n=106; non-fallers group; mean age=67.3 years, SD=13.6; mean time post-stroke=21.9 days, SD=28.8) on age and functional status (N=212).
Interventions
Not applicable.
Main outcome measures
Total length of stay, Functional Independence Measure (FIM) assessed at discharge, and discharge destination.
Results
The mean length of stay for fallers was 11 days longer than non-fallers (p=0.0017). Non-fallers and fallers did not differ on discharge total FIM scores (p=0.19), and both groups were discharged home after in-patient rehabilitation (non-fallers: 77%; fallers: 74%; p=0.52).
Conclusions
This study suggests that falls experienced during in-patient stroke rehabilitation may have contributed to a longer length of stay; however, falls did not impact discharge functional status or discharge destination.
Keywords: Accidental Falls, Rehabilitation, Stroke
Falls are common post-stroke, with 12–47% of individuals falling at least once during in-patient stroke rehabilitation.1–5 Individual risk factors for falls among stroke survivors are numerous and interrelated,6 and can include impaired performance of activities of daily living,1,3,4 inability to transfer,7 decreased balance control,5,8 and not following instructions.2,9 Falls after stroke can have significant immediate physical and psychological consequences,10 including injuries2–4,11 such as hip fractures,12 fear of falling,13 reduced physical activity,11 and depression.14 In-hospital falls have been identified as one of the most common medical complications after stroke,15,16 which can negatively influence stroke rehabilitation and recovery.2
In-patient rehabilitation is a health care setting where patients are focused on improving function and maximizing their abilities. It is typically delivered during the sub-acute stage of stroke recovery (i.e. less than three months post-stroke) when patients are likely to receive the most benefit from intensive therapy.17,18 Unfortunately, there is limited available evidence for the effectiveness of falls prevention interventions after stroke across acute care, rehabilitation, community, and institutional care settings.19,20 Thus, the incidence of falls will remain of concern, as it may not be possible to prevent every fall.
Little evidence exists on the impact of falls on rehabilitation outcomes; therefore, it is important to understand the effect that falls have on the course of patient recovery and delivery of care during the critical sub-acute phase of stroke. The primary objective of this study was to compare length of stay, functional status, and discharge destination between individuals who fell during in-patient stroke rehabilitation and those who did not fall. It was hypothesized that patients who fell would have poorer recovery compared to those who did not fall. This would be demonstrated by a longer length of stay, worse functional outcomes at discharge, and less likely to be discharged home following the rehabilitation stay among individuals who fell.
METHODS
Study design
A retrospective cohort study involving a chart review was conducted. The chart review involved consecutive admissions to the specialized stroke unit at the Toronto Rehabilitation Institute from October 1, 2009 to September 30, 2012. The Toronto Rehabilitation Institute Research Ethics Board approved this study, and a waiver of patient consent for the purpose of this review was obtained.
Participants
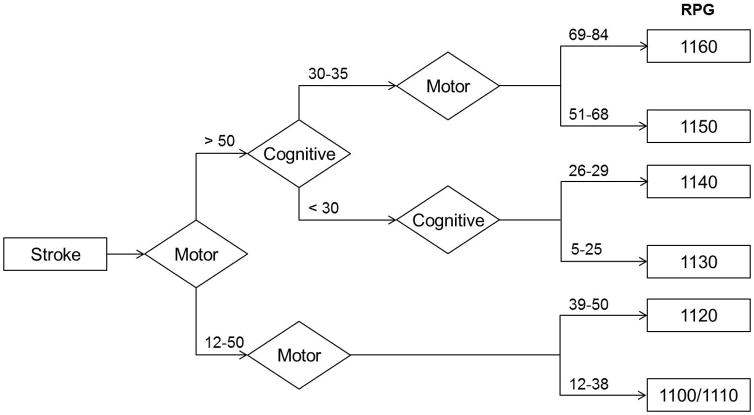
The in-patient stroke rehabilitation unit housed 20 to 23 beds during the time of data collection, and admitted patients who were medically stable and had the endurance to participate in the program. Patients received multidisciplinary care including individualized physiotherapy, occupational therapy, and speech-language therapy for one hour per discipline per day, five days per week over a typical length of stay of four to six weeks. Excluding duplicate admissions for another stroke and individuals without imaging (n=20), 504 patients with confirmed stroke were admitted to the stroke unit during the three year period. Patients were excluded from the analysis if they were not living at home before their acute stroke hospitalization (n=18), and/or if their Functional Independence Measure (FIM)21 scores on admission were missing (n=17). The study sample was created by matching all individuals who fell at least once during in-patient rehabilitation (i.e., “fallers”) with a randomly-selected sample of individuals who did not fall (i.e., “non-fallers”). A fall was defined as any time an individual came to rest unintentionally on the ground, floor, or other lower level.22 Matching was necessary because, on average, fallers and non-fallers tend to differ on measures of function and impairment on admission that are predictive of the current study’s primary outcomes.5,23 The sample of non-fallers was matched to fallers by stratified random sampling according to the Rehabilitation Patient Group and age. The Rehabilitation Patient Group algorithm was developed to provide a case-mix classification system to estimate in-patient rehabilitation costs, and is often used to determine length of stay (LOS) (i.e., one of the primary outcomes).24 Admission FIM scores and age (i.e. <40, 40–59, 60–79 and >80 years) were used to stratify all individuals. Due to the distribution of the study sample, the two lowest Rehabilitation Patient Group categories from the original algorithm were combined, representing patients with a motor score of 12 to 38, leaving six possible Rehabilitation Patient Group categories (Figure 1).
Figure 1.
Data extraction
All data were recorded in patients’ clinical charts during their rehabilitation stay by clinical staff (medical and allied health professionals), and extracted by trained research staff using a chart review form. Data were checked for inconsistencies and logical errors that may have arisen due to errors in extraction and were corrected, as necessary. The following variables were extracted to describe the cohort: age, sex, Berg Balance Scale (BBS)25 score on admission, and the date and type of stroke. Falls experienced during in-patient rehabilitation were captured from hospital incident reports, nursing notes, and patient interviews that were part of routine care at discharge from rehabilitation.26 Where available, information on each fall was recorded, which included details of the activity undertaken at the time of fall, where and when the fall occurred, and if any injury resulted. During the in-patient rehabilitation length of stay, patients may have had the opportunity to go home on a weekend pass; therefore, any falls that took place in the home of the patient were also included. Details of falls experienced on a weekend pass were collected through patient interviews, as these events were not recorded by the hospital incident reporting system. The three primary outcomes of this study are described below.
Length of stay (LOS) was determined by the total number of days spent on the in-patient stroke rehabilitation service (i.e. the number of days between admission and discharge date). Occasionally, patients were placed on alternate level of care (ALC; i.e. when patients no longer required the level of care provided in the given hospital setting) while waiting for a discharge plan to be finalized (e.g. if the patient was on a waiting list for long-term care). Thus, a patient’s discharge date was the date that the patient left the rehabilitation hospital permanently. If a patient was temporarily transferred to another location for at least one overnight stay (e.g. to an acute care facility for treatment), LOS was adjusted by subtracting the number of days spent off the stroke unit.
Functional status was measured at admission and discharge from rehabilitation using the Functional Independence Measure (FIM).21 The FIM instrument is a standardized measure of motor and cognitive disability, and rates an individual’s level of independence in 18 tasks on a scale from 1 to 7, with 1 corresponding to full dependence, and 7 corresponding to complete independence. Total FIM scores can range from 18 to 126; the motor domain ranges from 13 to 91 and the cognitive domain ranges from 5 to 35. The FIM has been studied extensively and has been found to have acceptable inter-rater and test-retest reliability in rehabilitation populations.27 The minimal clinically important difference for the FIM is a 22-point change, which reflects a significant improvement in functional independence among patients with stroke.28
Discharge destination after in-patient rehabilitation was defined dichotomously, home or not home. If an individual was not discharged home, other possible discharge destinations included a retirement home, acute care hospital (transferred and did not return to the rehabilitation facility), convalescent care (for additional therapy), long-term care, and another rehabilitation facility (to be closer to home).
Statistical analysis
Characteristics of non-fallers and fallers were compared on admission to in-patient rehabilitation using the Mann-Whitney U test for continuous or ordinal data, and the chi-square or Fisher’s exact test for nominal data. The alpha level for comparing baseline characteristics of the two groups was set at 0.05. To test the outcomes of interest, non-fallers and fallers were compared on LOS, discharge FIM scores using the Mann-Whitney U test, and discharge destination (i.e. home or not home) was compared using the chi-square test. Non-parametric testing (i.e. Mann-Whitney U test) was necessary for LOS and FIM scores after assumptions of normality were violated (i.e. Shapiro-Wilk test, quantile-quantile plot). To examine the three primary outcome measures, a one-tailed test was used and an alpha was set at 0.017 (i.e., Bonferonni-corrected for multiple comparisons; 0.05 divided by three primary outcome measures). Statistical analyses were carried out using SAS version 9.2.
RESULTS
Of the 469 patients attending in-patient stroke rehabilitation, 113 patients (24%) were classified as fallers; therefore, a pool of 356 patients was available to select a matched sample of non-fallers. A final sample of 212 participants (106 non-fallers and 106 fallers) was included in the analysis; seven fallers were excluded because no non-faller match was found. Over half (51%) of the participants were in the lowest Rehabilitation Patient Group category, representing severe disability. There were no significant differences on demographic and stroke characteristics between non-fallers and fallers on admission to rehabilitation (Table 1).
Table 1.
Participant characteristics on admission to rehabilitation.
| Characteristic | Patients not included (n=257) | Study sample | p value | |
|---|---|---|---|---|
| Non-fallers (n=106) | Fallers (n=106) | |||
| Age (years) | 69.4 (13.6) | 67.3 (13.6) | 67.8 (12.9) | 0.90 |
| Number of women | 117 (46) | 48 (45) | 47 (44) | 0.89 |
| Time post-stroke (days) | 20.2 (28.9) | 21.9 (28.8) | 26.4 (28.3) | 0.078 |
| Type of stroke | ||||
| Ischemic | 205 (80) | 81 (76) | 81 (76) | 0.44 |
| Hemorrhagic | 36 (14) | 19 (18) | 14 (13) | |
| Ischemic & hemorrhagic | 3 (1) | 1 (1) | 1 (1) | |
| Transforming to hemorrhagic | 13 (5) | 5 (5) | 10 (9) | |
| Total FIM (points) | 88.4 (18.5) | 65 (21) | 61.9 (18.1) | 0.34 |
| Motor | 64 (16.5) | 43.1 (18.3) | 61.9 (18.1) | 0.21 |
| Cognitive | 24.4 (5.9) | 21.9 (6.5) | 21.6 (5.9) | 0.38 |
| Berg Balance Scale (0–56 points) | 35.7 (16.4)* | 19.1 (15.5) | 14.6 (13.9) | 0.059 |
NOTE: Values are means (standard deviation) for continuous or ordinal variables, and counts (% rounded to the nearest integer) for categorical variables. The p value is for the Mann-Whitney U test, chi-square or Fisher’s exact test comparing non-fallers to fallers on admission.
Berg Balance Scale scores missing for two patients.
A total of 157 falls were recorded, and 31/106 fallers (29%) fell more than once. The average time from admission to an individual’s first fall was 20.5 days (SD=18.3 days), and 30/157 falls (19%) took place within the first week of rehabilitation (Figure 2). Circumstances of in-patient falls are presented in Table 2. Fifty-four falls of the 157 falls (34%) occurred during transfers (e.g. from bed to wheelchair), 78/157 falls (50%) took place in the patient’s room in the hospital, and no injury was observed in 106/157 falls (68%).
Figure 2.
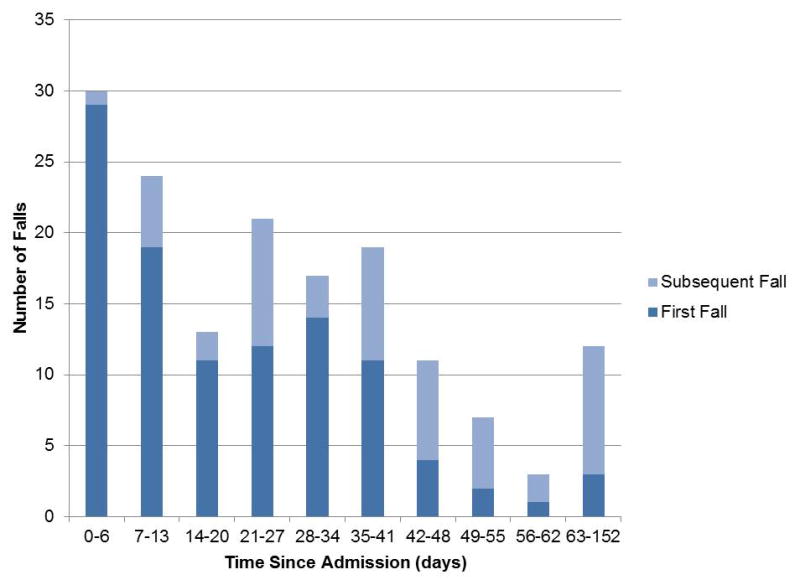
Table 2.
Circumstances of in-patient falls (n=157 falls).
| Frequency (%) | |
|---|---|
| Activity at time of fall | |
| Transferring | 54 (34) |
| Reaching, bending or turning | 30 (19) |
| Walking | 14 (9) |
| Sitting | 9 (6) |
| Standing | 9 (6) |
| Lying | 2 (1) |
| Not available | 39 (25) |
| Location of fall | |
| Hospital | 137 (87) |
| Patient’s room | 78 |
| Bathroom, tub room | 41 |
| Common area | 10 |
| Therapy area | 8 |
| Home of patient | 11 (7) |
| Bedroom | 5 |
| Bathroom | 3 |
| Kitchen | 1 |
| Outdoors | 1 |
| Not specified | 1 |
| Not available | 9 (6) |
| Injury after fall | |
| No injury | 106 (68) |
| Cuts or bruises | 17 (11) |
| Pain (e.g. back, hip, shoulder) | 6 (4) |
| Hit head* | 3 (1) |
| Head injury | 2 (1) |
| Not available | 23 (15) |
NOTE: Values are counts (% rounded to the nearest integer) for categorical variables.
No confirmed head injury; however, the interdisciplinary team initiated a head injury routine as per protocol.
The average LOS for fallers was 11 days longer than non-fallers (W(1)=9963, Z=−2.97, p=0.0017; Table 3). Fourteen patients were placed on ALC and when removing these patients and their matched pairs, differences in LOS remained highly significant between non-fallers and fallers (non-fallers: 42.4 days; fallers: 51.1 days; W(1)=7858, Z=−2.75, p=0.0033). There were no differences in discharge total FIM scores between non-fallers and fallers (W(1)=10981.5, Z=0.87, p=0.19). When analyzed on FIM subscales, the groups did not significantly differ at discharge on the FIM motor subscale (W(1)=11181, Z=1.33, p=0.093) or the FIM cognitive subscale (W(1)=10333, Z=−0.64, p=0.26). Likewise, a similar proportion of non-fallers and fallers were discharged home after in-patient rehabilitation (non-fallers: 77%; fallers: 74%; p=0.52; Table 3). Details of the breakdown of discharge destination are provided in Table 3.
Table 3.
Differences in outcome measures at discharge from in-patient stroke rehabilitation.
| Outcome measure | n | Non-fallers | n | Fallers | p value |
|---|---|---|---|---|---|
| Length of stay (days) | 106 | 43.8 (24.8) | 106 | 54.8 (29.7) | 0.0017* |
| Total FIM (points) | 102 | 97.3 (21) | 105 | 96.4 (18.5) | 0.19 |
| Motor | 69.8 (17.3) | 68.4 (14.8) | 0.093 | ||
| Cognitive | 27.5 (5.6) | 28 (5.5) | 0.26 | ||
| Discharge destination | 106 | 106 | 0.52 | ||
| Home | 82 (77) | 78 (74) | |||
| Not home | 24 (23) | 28 (26) | |||
| Retirement home | 7 (7) | 3 (3) | |||
| Acute care | 6 (6) | 4 (4) | |||
| Convalescent care | 6 (6) | 8 (8) | |||
| Long-term care | 4 (4) | 13 (12) | |||
| Another rehab facility | 1 (1) | 0 (0) |
NOTE: Values are means (standard deviation) for continuous or ordinal variables, and counts (% rounded to the nearest integer) for categorical variables. The p value is for the Mann-Whitney U test and for the chi-square test comparing both groups at discharge.
p value is significant, where p<0.017 (Bonferroni-corrected for multiple comparisons).
There were 24/106 fallers (23%) who experienced an injury. When the injured fallers and their non-faller matches were analyzed separately, LOS was no longer significantly different between the two groups (non-fallers: 40.9 days; fallers: 53.6 days; W(1)=515, Z=−1.5, p=0.071). For the total FIM scores at discharge, the injured fallers had a higher but not statistically significant mean score than their non-faller matches (non-fallers: 91.9 points; fallers: 99.1 points; W(1)=528, Z=−0.5, p=0.31).
DISCUSSION
In support of the hypothesis, patients who fell had a longer length of stay (LOS) than those who did not fall. The course of rehabilitation may have been extended for fallers due to setbacks in physical recovery that required additional resources or modifications to discharge planning. It is also possible that fallers were fearful of experiencing another fall, which in turn influenced recovery and hospital LOS.29 Waiting periods for patients on alternate level of care (ALC) may have contributed to a prolonged LOS, where active rehabilitation and discharge planning is complete.
Contrary to the hypothesis, both groups had similar functional scores at discharge from rehabilitation, despite the increased LOS for fallers. A potential reason for this result could be that the rehabilitation team kept the patient beyond the targeted discharge date in order for the patient to reach an appropriate functional level before discharge. Since groups were similar on functional status on admission, this finding suggests that fallers required more time to achieve the same level of function as non-fallers. This level of functional improvement was clinically significant, as both groups, on average surpassed the minimal clinically important difference of 22 points on the FIM.28 With a limited number of rehabilitation beds available, information regarding the impact of falls is essential to optimize efficiency of in-patient stroke rehabilitation services. Even though fallers had a longer LOS, and thus greater costs associated with care,24 small improvements in functional status may have significant benefits in quality of life and future health care utilization. Likewise, there were no differences in the proportion of individuals who returned home following their rehabilitation stay between non-fallers and fallers. Participants included in this study lived at home prior to hospitalization for stroke; therefore, it would be expected that individuals would return to their premorbid residence when their medical and functional status improved, and their rehabilitation goals were met.
Both groups of non-fallers and fallers in this study averaged a longer LOS than the median LOS for stroke rehabilitation in Canada (i.e., 35 days).30 This was likely because the sample of individuals included in this analysis represents a lower-functioning subset of the institution’s stroke rehabilitation unit, as measured by the FIM (e.g., see Table 1). Thus, the results of this study apply to lower-functioning individuals receiving in-patient rehabilitation post-stroke. With greater dependence in performing activities of daily living, these stroke survivors are at high risk of falling;1,3,4 however, individuals in the current study were able to achieve benefits from in-patient rehabilitation with a longer LOS.31,32
Similarly, it appears as though fallers were admitted to rehabilitation later post-stroke than non-fallers, which may have been due to a longer LOS in acute care as a result of comorbidities or medical complexities. In addition, fallers averaged lower balance scores than non-fallers as measured by the Berg Balance Scale (BBS) on admission. Data on discharge suggests that fallers continued to have lower BBS scores than non-fallers but this was not statistically significant (p=0.057). Since balance impairment is an important risk factor for falls among individuals with stroke,5,14,33,34 and balance is essential for performing activities of daily living, those who were more affected by stroke (and therefore more prone to falls) required longer in-patient treatment.
Overall, the rate of falls was within the range of other studies reporting falls during in-patient stroke rehabilitation (i.e. 113 out of 469 patients fell; rate: 24%). The proportion of fallers with more than one fall (‘multiple fallers’; rate: 29%) was in line with other studies of patients attending stroke rehabilitation (rates: 5–51%),1,2,4,5 as was the presence of injuries (rates: 8–29%).2–5 Falls while transferring are common in the in-patient rehabilitation setting,2,3 and typically take place in the patient’s room or bathroom,2–4,35 which was the case in the current study. Falls were most prevalent during the first week of admission to rehabilitation, as reported in previous studies,3,36 making this a critical time point. There was also an increase in the frequency of falls in the fourth week of stay (i.e. 21–27 days from admission). Falls may have become more frequent as individuals recovered and may correspond with increased levels of mobility and exposure to risk-taking activities.35
Lastly, the sub-analysis of injured fallers revealed that there was no statistically significant difference in LOS between injured fallers and their non-faller matches. Even though injured fallers stayed an average 12.7 days longer, this result may have been due to a low sample size (n=48). Interestingly, the injured fallers finished with a higher, though not significantly different, mean FIM score; however, this may have been as a result of the additional time on the unit.
This research study is unique because it is the first to our knowledge to examine the link between falls during in-patient stroke rehabilitation and their impact on length of stay and functional status at discharge. Compared to earlier uncontrolled efforts aimed at determining the consequences of falls in the stroke rehabilitation population,1,4,5 the current study matched on admission FIM using the Rehabilitation Patient Group classification and age to ensure that the groups were comparable on admission and, therefore, the main difference between groups was the occurrence of a fall during in-patient rehabilitation.
Study Limitations
This study has several potential limitations. Data were collected from a single hospital and may not be representative of other rehabilitation centres. The retrospective nature of the methodology limited data collection to what was available in the medical chart, and this information extracted from medical charts was written for purposes other than research.37 For instance, there are factors other than falls that may have contributed to an increased LOS, such as comorbidities and psychosocial status that were not measured in the present study. In addition, injuries were classified dichotomously, as there were not enough details available to measure the severity among the types of injury; therefore, all falls were treated equally. Finally, the incidence of falls may have been low as a result of underreporting due to unwitnessed falls or events that staff did not perceive as reportable.
CONCLUSIONS
The results of this study suggest that falls may extend in-patient stroke rehabilitation length of stay. Longer length of stay can influence the overall individual recovery path of the patient, and have large economic consequences to the health care system. However, individuals who fell achieved a similar functional level at discharge and were equally likely to be discharged home compared to those who did not fall. These results shed light on how stroke recovery may be impacted by falls during this critical time for rehabilitation after stroke.
Acknowledgments
The authors acknowledge the support of the Toronto Rehabilitation Institute. Equipment and space have been funded with grants from the Canada Foundation for Innovation, Ontario Innovation Trust and the Ministry of Research and Innovation. The views expressed do not necessarily reflect those of the funders. JSW received funding from the Toronto Rehabilitation Institute Student Scholarship (Ontario Student Opportunity Trust Funds). DB holds a Canada Research Chair. AM holds a New Investigator Award from the Canadian Institutes of Health Research (MSH-141983). Preliminary results were presented at the National Fall Prevention Conference on May 27, 2014 in Toronto, ON, Canada.
List of Abbreviations
- ALC
Alternate level of care
- BBS
Berg Balance Scale
- LOS
Length of stay
Footnotes
Conflict of interest: None.
References
- 1.Czernuszenko A, Czlonkowska A. Risk factors for falls in stroke patients during inpatient rehabilitation. Clin Rehabil. 2009;23(2):176–88. doi: 10.1177/0269215508098894. [DOI] [PubMed] [Google Scholar]
- 2.Nyberg L, Gustafson Y. Patient falls in stroke rehabilitation. A challenge to rehabilitation strategies. Stroke. 1995;26(5):838–42. doi: 10.1161/01.str.26.5.838. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki T, Sonoda S, Misawa K, Saitoh E, Shimizu Y, Kotake T. Incidence and consequence of falls in inpatient rehabilitation of stroke patients. Exp Aging Res. 2005;31(4):457–69. doi: 10.1080/03610730500206881. [DOI] [PubMed] [Google Scholar]
- 4.Sze KH, Wong E, Leung HY, Woo J. Falls among Chinese stroke patients during rehabilitation. Arch Phys Med Rehabil. 2001;82(9):1219–25. doi: 10.1053/apmr.2001.25094. [DOI] [PubMed] [Google Scholar]
- 5.Teasell R, McRae M, Foley N, Bhardwaj A. The incidence and consequences of falls in stroke patients during inpatient rehabilitation: factors associated with high risk. Arch Phys Med Rehabil. 2002;83(3):329–33. doi: 10.1053/apmr.2002.29623. [DOI] [PubMed] [Google Scholar]
- 6.Weerdesteyn V, de Niet M, van Duijnhoven HJ, Geurts AC. Falls in individuals with stroke. J Rehabil Res Dev. 2008;45(8):1195–213. [PubMed] [Google Scholar]
- 7.Zdobysz JA, Boradia P, Ennis J, Miller J. The relationship between functional independence scores on admission and patient falls after stroke. Top Stroke Rehabil. 2005;12(2):65–71. doi: 10.1310/G89Q-80VR-P5P7-9PTH. [DOI] [PubMed] [Google Scholar]
- 8.Andersson AG, Kamwendo K, Seiger A, Appelros P. How to identify potential fallers in a stroke unit: validity indexes of 4 test methods. J Rehabil Med. 2006;38(3):186–91. doi: 10.1080/16501970500478023. [DOI] [PubMed] [Google Scholar]
- 9.Rapport LJ, Webster JS, Flemming KL, Lindberg JW, Godlewski MC, Brees JE, Abadee PS. Predictors of falls among right-hemisphere stroke patients in the rehabilitation setting. Arch Phys Med Rehabil. 1993;74(6):621–6. doi: 10.1016/0003-9993(93)90160-c. [DOI] [PubMed] [Google Scholar]
- 10.Batchelor FA, Mackintosh SF, Said CM, Hill KD. Falls after stroke. Int J Stroke. 2012;7(6):482–90. doi: 10.1111/j.1747-4949.2012.00796.x. [DOI] [PubMed] [Google Scholar]
- 11.Mackintosh SF, Hill K, Dodd KJ, Goldie P, Culham E. Falls and injury prevention should be part of every stroke rehabilitation plan. Clin Rehabil. 2005;19(4):441–51. doi: 10.1191/0269215505cr796oa. [DOI] [PubMed] [Google Scholar]
- 12.Ramnemark A, Nyberg L, Borssen B, Olsson T, Gustafson Y. Fractures after stroke. Osteoporos Int. 1998;8(1):92–5. doi: 10.1007/s001980050053. [DOI] [PubMed] [Google Scholar]
- 13.Watanabe Y. Fear of falling among stroke survivors after discharge from inpatient rehabilitation. Int J Rehabil Res. 2005;28(2):149–52. doi: 10.1097/00004356-200506000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ. 1995;311(6997):83–6. doi: 10.1136/bmj.311.6997.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Complications after acute stroke. Stroke. 1996;27(3):415–20. doi: 10.1161/01.str.27.3.415. [DOI] [PubMed] [Google Scholar]
- 16.McLean DE. Medical complications experienced by a cohort of stroke survivors during inpatient, tertiary-level stroke rehabilitation. Arch Phys Med Rehabil. 2004;85(3):466–9. doi: 10.1016/s0003-9993(03)00484-2. [DOI] [PubMed] [Google Scholar]
- 17.Kwakkel G, Kollen B, Lindeman E. Understanding the pattern of functional recovery after stroke: facts and theories. Restor Neurol Neurosci. 2004;22(3–5):281–99. [PubMed] [Google Scholar]
- 18.Teasell R, Foley N, Hussein N, Speechley M. Evidence-Based Review of Stroke Rehabilitation. The Elements of Stroke Rehabilitation 2013Chapter 6 [Google Scholar]
- 19.Batchelor F, Hill K, Mackintosh S, Said C. What works in falls prevention after stroke?: a systematic review and meta-analysis. Stroke. 2010;41(8):1715–22. doi: 10.1161/STROKEAHA.109.570390. [DOI] [PubMed] [Google Scholar]
- 20.Verheyden GS, Weerdesteyn V, Pickering RM, Kunkel D, Lennon S, Geurts AC, Ashburn A. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev. 2013;5:Cd008728. doi: 10.1002/14651858.CD008728.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18. [PubMed] [Google Scholar]
- 22.Ory MG, Schechtman KB, Miller JP, Hadley EC, Fiatarone MA, Province MA, Arfken CL, Morgan D, Weiss S, Kaplan M. Frailty and injuries in later life: the FICSIT trials. J Am Geriatr Soc. 1993;41(3):283–96. doi: 10.1111/j.1532-5415.1993.tb06707.x. [DOI] [PubMed] [Google Scholar]
- 23.Maeda N, Kato J, Shimada T. Predicting the probability for fall incidence in stroke patients using the Berg Balance Scale. J Int Med Res. 2009;37(3):697–704. doi: 10.1177/147323000903700313. [DOI] [PubMed] [Google Scholar]
- 24.Sutherland JM, Walker J. Challenges of rehabilitation case mix measurement in Ontario hospitals. Health Policy. 2008;85(3):336–48. doi: 10.1016/j.healthpol.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 25.Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl 2):S7–11. [PubMed] [Google Scholar]
- 26.Hill AM, Hoffmann T, Hill K, Oliver D, Beer C, McPhail S, Brauer S, Haines TP. Measuring falls events in acute hospitals-a comparison of three reporting methods to identify missing data in the hospital reporting system. J Am Geriatr Soc. 2010;58(7):1347–52. doi: 10.1111/j.1532-5415.2010.02856.x. [DOI] [PubMed] [Google Scholar]
- 27.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: A quantitative review. Archives of Physical Medicine and Rehabilitation. 1996;77(12):1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 28.Beninato M, Gill-Body KM, Salles S, Stark PC, Black-Schaffer RM, Stein J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Arch Phys Med Rehabil. 2006;87(1):32–9. doi: 10.1016/j.apmr.2005.08.130. [DOI] [PubMed] [Google Scholar]
- 29.Gettens S, Fulbrook P. Fear of falling: association between the Modified Falls Efficacy Scale, in-hospital falls and hospital length of stay. Journal of Evaluation in Clinical Practice. 2015;21(1):43–50. doi: 10.1111/jep.12226. [DOI] [PubMed] [Google Scholar]
- 30.Grant C, Goldsmith CH, Anton HA. Inpatient stroke rehabilitation lengths of stay in Canada derived from the National Rehabilitation Reporting System, 2008 and 2009. Arch Phys Med Rehabil. 2014;95(1):74–8. doi: 10.1016/j.apmr.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 31.Pereira S, Graham JR, Shahabaz A, Salter K, Foley N, Meyer M, Teasell R. Rehabilitation of individuals with severe stroke: synthesis of best evidence and challenges in implementation. Top Stroke Rehabil. 2012;19(2):122–31. doi: 10.1310/tsr1902-122. [DOI] [PubMed] [Google Scholar]
- 32.Hayward KS, Kuys SS, Barker RN, Brauer SG. Clinically important improvements in motor function are achievable during inpatient rehabilitation by stroke patients with severe motor disability: a prospective observational study. Neuro Rehabilitation. 2014;34(4):773–9. doi: 10.3233/NRE-141076. [DOI] [PubMed] [Google Scholar]
- 33.Mackintosh SF, Hill KD, Dodd KJ, Goldie PA, Culham EG. Balance score and a history of falls in hospital predict recurrent falls in the 6 months following stroke rehabilitation. Arch Phys Med Rehabil. 2006;87(12):1583–9. doi: 10.1016/j.apmr.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 34.Rabadi MH. Risk factors for falls in stroke patients during inpatient rehabilitation. Clin Rehabil. 2009;23(5):463. doi: 10.1177/0269215509334740. author reply 464. [DOI] [PubMed] [Google Scholar]
- 35.Aizen E, Shugaev I, Lenger R. Risk factors and characteristics of falls during inpatient rehabilitation of elderly patients. Arch Gerontol Geriatr. 2007;44(1):1–12. doi: 10.1016/j.archger.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Vassallo M, Sharma JC, Briggs RS, Allen SC. Characteristics of early fallers on elderly patient rehabilitation wards. Age Ageing. 2003;32(3):338–42. doi: 10.1093/ageing/32.3.338. [DOI] [PubMed] [Google Scholar]
- 37.Hess DR. Retrospective studies and chart reviews. Respir Care. 2004;49(10):1171–4. [PubMed] [Google Scholar]