Abstract
Pompe disease is an autosomal recessive lysosomal storage disease characterized in adult patients by slowly progressive limb-girdle muscle weakness and respiratory insufficiency. Data on pregnancy in women with Pompe disease, intrauterine development of the fetus and parturition are rare. Here we describe a twin pregnancy followed by a second pregnancy in a 38-year-old female patient with Pompe disease. We report the impact of pregnancy on muscle and respiratory functions as well as the neurological and endocrine systems and discuss the medical consequences for anaesthetic management at parturition.
Introduction
Pompe disease (OMOM 232300) is an autosomal recessive, lysosomal storage disease characterized by a mutation of the acid α-glucosidase (GAA) gene. In adult patients, the disease manifests with a slowly progressive myopathy of limb-girdle and trunk muscle, with restrictive respiratory insufficiency as a possible complication. Patients may become wheelchair bound and respirator dependent. Enzyme replacement therapy is available, effectively improving or stabilizing muscle function in some and slowing deterioration of the disease in other patients (Teener 2012; Schuller et al. 2013).
Pregnancy induces a host of adaptive changes in the mother which may worsen signs and symptoms of Pompe disease, putting at risk both the mother and the fetus. Data on pregnancy in Pompe disease are rare (Cilliers et al. 2008; de Vries et al. 2011; Zagnoli et al. 2013; Karabul et al. 2014), and no twin pregnancy has been reported so far.
Here we report on a patient with a successful twin pregnancy after assisted reproduction intervention, followed by a second, spontaneous pregnancy 11 months after parturition of the twins.
Case Report
The patient was diagnosed with Pompe disease at the age of 35 years. Genotyping demonstrated a heterozygous mutation of the GAA gene with the well-known mutation IVS 0–45T>G in the promoter region and a second mutation, c2407 C>T (Q803X), in exon 16 that has not been observed in a Pompe patient so far. Thereafter, enzyme replacement therapy (ERT) with alpha-glucosidase and supportive physiotherapy were initiated. Repeated allergic reactions to alpha-glucosidase necessitated intermittent premedication with antihistamines and prednisolone, resulting in partial insufficiency of the ACTH/cortisol axis. Due to restrictive respiratory insufficiency, non-invasive ventilation during the night was introduced.
An unfulfilled desire for parenthood led to consultation at an external fertility centre, assisted reproduction intervention and implantation of two fetuses (15.12.2012). With the pregnancy confirmed, the patient requested termination of ERT. Intrauterine development of the twins was normal. At pregnancy week 32, haemolysis, sevenfold increased transaminases compared to those before the pregnancy and thrombocytopenia developed, indicating HELLP syndrome (haemolysis, elevated liver enzymes and low platelets). Therefore, at week 33, delivery of two healthy male children by caesarean section was performed. Alpha-glucosidase therapy was resumed after 16 months but discontinued by the patient as soon as a new, spontaneous pregnancy was diagnosed. After an uncomplicated pregnancy, a healthy child was born at term by caesarean section (Table 1). So far reintroduction of enzyme replacement therapy and re-evaluation were declined by the patient due to her time restrictions and workload.
Table 1.
Timeline of events
| Event | Week |
|---|---|
| Assisted reproduction intervention, first pregnancy and end of ERT | 0 |
| Parturition first pregnancy (twins) | 31 |
| Re-initiation of ERT | 67 |
| Diagnosis of second pregnancy and end of ERT | 77 |
| Parturition second pregnancy | 113 |
| Last investigation | 152 |
Results
Clinical Course of Pompe Disease During Pregnancy
During pregnancy, functional data [time-related tests, time for (i) climbing four stairs, (ii) walking 10 m, (iii) getting up from supine] as well as the 6-min walk test (distance-related test, distance in metres walked within 6 min)] worsened compared to those before pregnancy (Fig. 1a, b). The 322% increase in the time to get up from supine was mostly due to severe lower back pain related to the twin pregnancy.
Fig. 1.
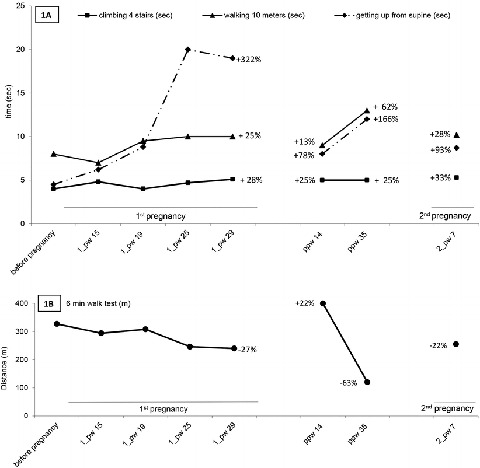
(a) Functional parameters: time-related tests (climbing four stairs, walking 10 m, getting-up from supine) and (b) distance-related test (6-min walk test). 1_pw15 first pregnancy week 15, 2_pw 7 second pregnancy week 7, ppw 14 postpartum week 14. The curves indicate absolute values, i.e. time needed (a) or metres walked (b); the numbers indicate the percent change compared to that before the first pregnancy. For the time-related tests, the percent increase indicates deterioration, i.e. more time needed than before pregnancy. For the distance-related test, deterioration is indicated by the percent decline (−percent), i.e. less metres walked within 6 min
Postpartum time-related tests improved but were still worse compared to those before pregnancy (plus 38%). The improvement was mostly due to less time needed in getting up from supine (basal vs. during pregnancy +322% and postpartum +166%, respectively). The distance covered during the 6-min walk test increased by 22% compared to basal. However, during further follow-up, all functional parameters worsened (mean time-related tests +85%, distance-related test −63%) compared to basal. Subsequently, ERT was resumed at week 67 but terminated again when 10 weeks later a second pregnancy was diagnosed. Functional tests were repeated on the last day of ERT. Performance in both, the time-related tests (+51%) and the 6-min walk test (−22%), was still less than basal indicating that despite 10 weeks of ERT, the basal activity performance had not been achieved.
In conclusion, all functional parameters deteriorated significantly during pregnancy by about 25%, with the exception of getting up from supine that was clearly more restricted, possibly due to the twin pregnancy. After parturition, without ERT, a further decline of the time-related tests was observed, while the 6-min walk test noticeably improved. During the second pregnancy, with functional tests available only during the first trimester, after 10 weeks on ERT, the results were similar to those obtained at the end of the first pregnancy.
The Patient’s Complaints During Pregnancy
The patient was mostly affected by the weight gain related to the twin pregnancy. The compensating pregnancy lordosis added to the lordosis of Pompe disease resulting in lower back pain and, during the last trimester, increasing difficulties in getting up from the supine position (see Fig. 1).
Neurological Status
Results of the Walton and Gardner-Medwin scale did not change during pregnancies, while the arm function test deteriorated by one grade. There were slight changes in the overall muscle strength, yet after both pregnancies, muscle strength was identical to the basal evaluation (Fig. 2).
Fig. 2.
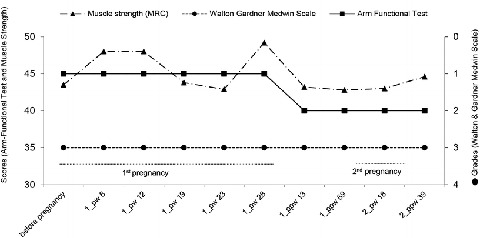
Neurological scores: muscle strength, Walton and Gardner-Medwin scale and arm function test. 1_PW 8 first pregnancy_pregnancy week 8, 1_ppw 13 first pregnancy_postpartum week 13, 2_pw 18 second pregnancy_pregnancy week 18, 2_ppw 39 second pregnancy_postpartum week 39
Lung Function Tests
One-second forced expiratory volume (FEV1) and vital capacity (VC) were 80% of normal values before the first pregnancy and were unchanged during the first and slightly declined during the second pregnancy, only to return to basal after parturition (Fig. 3). Before pregnancy, the difference between sitting and supine was 21% and 18% for FEV1 and VC, respectively. The difference became slightly more pronounced during the course of the twin pregnancy and was maximal during the second pregnancy with 30% and 28% for FEV1 and VC at week 29, respectively. After the second parturition, all parameters returned to basal, despite an almost continuous interruption of ERT for 3 years and 2 months. In conclusion, pregnancy-related effects on respiratory functions were most pronounced for the difference between sitting and supine for both FEV1 and VC. No persistent pregnancy-related negative effects on respiratory functions were observed.
Fig. 3.
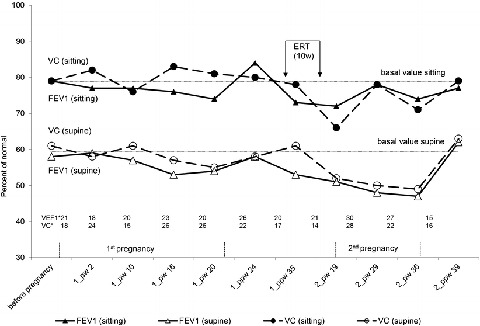
Lung function tests. FEV1 one-second forced expiration volume, VC vital capacity, 1_PW 2 first pregnancy_pregnancy week 2, 1_ppw 24 first pregnancy_postpartum week 24, 2_pw 19 second pregnancy_pregnancy week 19, 2_ppw 39 second pregnancy_postpartum week 39, ERT (10w) enzyme replacement therapy for 10 weeks. The dotted line indicates basal, i.e. before pregnancy. * The numbers give the difference between FEV1 and VC during sitting and supine, respectively, at the indicated time points
Echocardiography
Before pregnancy, echocardiography demonstrated a normal left ventricular ejection fraction of 60% and a first-grade insufficiency of the mitral and tricuspid valves. Echocardiographic results did not change during or after the pregnancies.
Pituitary: Adrenal Axis
Allergic reactions to ERT with subsequent repeated glucocorticoid premedication resulted in partial insufficiency of the ACTH/cortisol axis, defined as normal basal cortisol concentration yet failure to increase cortisol secretion in response to insulin-induced hypoglycaemia. As no signs and symptoms of hypocortisolism were detected, hydrocortisone was only substituted during stressful events, i.e. during the assisted reproduction intervention, as well as during parturition.
Pregnancy
Assisted reproduction intervention resulted in a dichorial twin pregnancy. Both fetuses grew well without growth discrepancy. An ultrasound examination, performed due to bruising and persistent lower left abdominal pain at 32 weeks and 2 days of pregnancy, showed no evidence of an early placental abruption, and all fetal parameters were normal. Newly diagnosed systolic hypertension, an increased concentration of transaminases and thrombocytopenia were consistent with HELLP syndrome. Subsequently, at week 33, a caesarean section was performed. After delivery the number of platelets normalized, no maternal postpartum complications were observed. APGAR scores (8/9/9 for both) and umbilical cord pH levels were normal for both babies. Birth weight was 1,885 and 2,170 g, respectively. Pathologic investigation of the uterus was normal. The myometrium was free of glycogen deposits by morphological and electron microscopic criteria (Fig. 4).
Fig. 4.
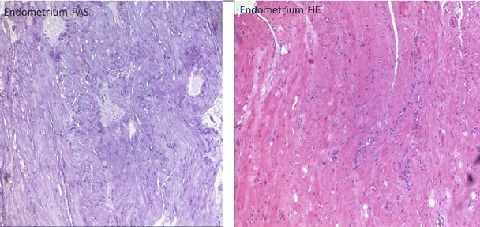
Histology of the placenta. PAS and HE haematoxylin staining of the myometrium. Normal histology of the placenta without glycogen deposits
The course of the subsequent pregnancy in 2014 was uncomplicated. An elective caesarean section was performed at week 38 of gestation, and a healthy male infant (3,190 g, APGAR 9/10/10) was born.
Anaesthetic Management During Parturition
Due to muscular weakness and restrictive respiratory insufficiency, general anaesthesia and perioperative systemic administration of opioids were to be avoided. Therefore, spinal and epidural anaesthesia were administered for the delivery of the twins. The total anaesthesia time was 75 min with stable vital signs and no hypoventilation. Due to the uncomplicated perioperative course of the first delivery, a less invasive protocol, i.e. only spinal anaesthesia, was decided upon for the second caesarean section.
Discussion
Reports on pregnancies in Pompe disease are rare. Recently, a retrospective, questionnaire-based evaluation of pregnancies in Pompe disease reported 17 pregnancies (15 deliveries and 2 miscarriages) in ten women with clinically manifest Pompe disease (Karabul et al. 2014). Muscular symptoms either became manifest (N = 3) or worsened (N = 3) during pregnancy or deteriorated (N = 2) after parturition. Median duration of pregnancies was 40 weeks, and delivery was by caesarean section in 33% and forceps in 5.7%. Only one preterm birth was reported, median birth weight was normal (3,100 g), while fetal distress was observed in 20% (p = 0.04 vs. the general population). In two women on ERT, ERT was interrupted with the diagnosis of pregnancy and restarted immediately after parturition. Overall, the authors concluded that while Pompe disease poses no increased risk of pregnancy or delivery-related complications, Pompe-specific symptoms, i.e. muscle weakness and respiratory complications, might become manifest or worsen during pregnancy. Two single case reports on pregnancy with ERT demonstrated similar results with increased muscle weakness and respiratory problems starting around the 26th week of pregnancy (de Vries et al. 2011; Zagnoli et al. 2013).
In our patient, we observed a twin pregnancy complicated by HELLP syndrome, followed by an uneventful singleton pregnancy. Maternal risk factors supposed to be associated with HELLP syndrome, a special form of preeclampsia, are infertility treatment and several genetic variants (FAS, VEGF and factor V Leiden mutation). However, no relation to Pompe disease has been described so far (Abildgaard and Heimdal 2013).
The deterioration of the functional tests was probably due to the normal burden of pregnancy, exacerbated by a twin pregnancy and superimposed on signs and symptoms of Pompe disease, as may have been the case with symptoms reported in the literature (Karabul et al. 2014). This is supported by the fact that the functional tests almost recurred to the basal status after parturition. Interestingly, caring for the twins proved to be strenuous such as having a negative impact on the functional tests. The loss in muscle strength observed early in the course of the second pregnancy is thus better explained by the long-time interval off therapy and the increased workload than as a consequence of the second pregnancy.
Weight gain in normal pregnancy is on average 12–13 k. To compensate for the additional abdominal weight, the pregnant women develop lower back lordosis (Heidemann 2003). As lordosis is an important characteristic of Pompe disease (ACMG Work Group on Management of Pompe Disease 2006; Schuller et al. 2013), this may be aggravated during pregnancy resulting in lower back pain and increased instability. Lower back pain and the problems in getting up from supine were the leading complaints in our patient, yet resolved after parturition.
The Walton and Gardner-Medwin score did not indicate a severe decline in muscle strength. This may be due to the wide scales allowing grading only between 1 and 4 thus possibly missing subtle changes.
During normal pregnancy, the lung minute volume increases due to expansion of the chest circumference by 5–7 cm and progesterone-induced hyperventilation. The reduced abdominal muscle tonus renders them less active in respiration. Thus, breathing is rather more than less diaphragmatic (Heidemann 2003). On the other hand, diaphragmatic mobility is reduced in the supine position, and this may coincide with the drop of FEV1 and VC that occurs in a supine Pompe patient, as could be observed in our patient (ACMG Work Group on Management of Pompe Disease 2006; Ambrosino et al. 2013). Again, these deteriorations are best explained by the physiological changes induced by the pregnancies and superimposed on the manifestation of Pompe disease.
In conclusion, during the pregnancies, only subtle deteriorations of the lung function tests occurred, posing no risk to the mother and the fetus. No persistent negative effects on respiratory functions were observed after the pregnancies, despite 3 years off ERT.
In adult Pompe disease, cardiovascular function is normal and remained so during both pregnancies and follow-up in our patient.
Each of the many endocrine systems adapts to pregnancy, and whether these changes interfere with Pompe disease is not known. During pregnancy, the CRH/ACTH/cortisol axis is physiologically up-regulated. Secondary adrenal insufficiency may put the patient and the fetus at a significant risk (Donnelly et al. 2003; Lindsay and Nieman 2005; Fux Otta et al. 2008; Halperin Rabinovich et al. 2008; Bjornsdottir et al. 2010). Outside pregnancies, no substitution therapy is required in partial secondary pituitary insufficiency as diagnosed in our patient. The situation is less clear during pregnancy. As a single, procedure-oriented cortisol substitution poses no risk of myopathic adverse effects, we offered hydrocortisone substitution during the assisted reproduction intervention and parturition procedures.
At the end of pregnancy, the physiological, restrictive respiratory insufficiency poses a risk for airway management problems and intubation (Kuczkowski et al. 2003). A reduction of the venous outflow occurs in the supine position, which is compensated for by activation of the sympathetic nervous system leading to vasoconstriction and an increase in heart rate. General anaesthesia or neuroaxial blockade may interfere with these compensatory mechanisms by blocking the increase of heart frequency and cardiac output, respectively (Geburtshilfe 2004). Therefore, regional anaesthesia is thought to be safer for the mother and the unborn child (Geburtshilfe 2004).
These considerations, relevant for other myopathies as well, led to following recommendations: preference of local or regional anaesthesia, avoidance of suxamethonium due to the patient’s myopathy and its associated risk of rhabdomyolysis and hyperkalaemia. Furthermore, regional anaesthesia reduces the risk of aspiration and hypoventilation by evasion of systemic administrated opioids. Moreover, pre-assessment is important to determine the extent of pulmonary and cardiac insufficiency (Kim et al. 2010; Lehberger et al. 2012). Thus, for our patient, spinal and epidural anaesthesia were chosen for the caesarean section.
Two successful pregnancies with ongoing ERT have been described so far (de Vries et al. 2011; Zagnoli et al. 2013). Our patient discontinued ERT during both pregnancies. The slight deterioration of motor function we observed in our patient over the course of the two pregnancies is probably related to the 30 months’ off therapy. As all pregnancy-related changes returned almost to the basal level after parturition of the twins, an interval of 9 months off ERT may have no deleterious effects. However, we strongly recommend resuming ERT as soon as possible. No negative effects on the unborn child have been described in those cases on ERT during pregnancy; thus, ongoing ERT may be an option in severely handicapped patients.
In conclusion, we describe a patient with Pompe disease and a twin pregnancy followed by a singleton pregnancy within 3 years. The patient did not demonstrate any worsening of her Pompe’s symptoms beyond those superimposed by the physiological adaptations of the pregnancies. The slight postpartum decline in her functional tests may be related to the long time interval off ERT, yet the burden of caring for two toddlers while pregnant may as well explain her functional restrictions. Interdisciplinary monitoring of the pregnancy, as well as planning of anaesthesia and parturition, allowed for the delivery of three healthy infants. Thus, with proper interdisciplinary planning, pregnancy in women with Pompe disease poses no risk, neither to the mother nor the child.
Synopsis
During pregnancy, symptoms of Pompe may worsen, due to the burden of the pregnancy. However, with interdisciplinary cooperation, pregnancy and parturition pose no risk for neither the mother nor the child.
Compliance with Ethical Guidelines
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000(5). Informed consent was obtained from the patient for the publication of her data. The institutional ethic committee consented to the publication of the data (EA2/089/15).
Conflict of Interest
Ursula Plöckinger was the recipient of an unrestricted grant by Genzyme, Germany, as well as speaker honorarium from Genzyme, Germany, and BioMarin, Germany, and a research grant from Pfizer, Germany. Nikolaus Tiling has received a speaker honorarium from Shire, Germany, and Genzyme, Germany. Lenka Bosanska, Bettina Temmesfeld-Wollbrück, Kerstin Irlbacher, Viktor Mezger and Gabriele Gossing declare that they have no conflict of interest.
Authorship Contribution
U. Plöckinger wrote the manuscript, Nikolaus Tiling and Lenka Bosanska cared for the patient and provided the data, Bettina Temmesfeld-Wollbrück performed the lung function tests and wrote the part of the manuscript dealing with lung function, Kerstin Irlbacher performed neurologic examinations and wrote the part of the manuscript dealing with neurological functions, Viktor Mezger wrote the part of the manuscript dealing with anaesthesia and Gabriele Gossing cared for the patient during pregnancy and parturition and wrote the part of the manuscript dealing with parturition.
References
- Abildgaard U, Heimdal K. Pathogenesis of the syndrome of hemolysis, elevated liver enzymes, and low platelet count (HELLP): a review. Eur J Obstet Gynecol Reprod Biol. 2013;166:117–123. doi: 10.1016/j.ejogrb.2012.09.026. [DOI] [PubMed] [Google Scholar]
- ACMG Work Group on Management of Pompe Disease Pompe disease diagnosis and management guideline. Genet Med. 2006;8:267–288. doi: 10.1097/01.gim.0000218152.87434.f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrosino N, Confalonieri M, Crescimanno G, Vianello A, Vitacca M. The role of respiratory management of Pompe disease. Respir Med. 2013;107:1124–1132. doi: 10.1016/j.rmed.2013.03.004. [DOI] [PubMed] [Google Scholar]
- Bjornsdottir S, Cnattingius S, Brandt L, et al. Addison’s disease in women is a risk factor for an adverse pregnancy outcome. J Clin Endocrinol Metab. 2010;95:5249–5257. doi: 10.1210/jc.2010-0108. [DOI] [PubMed] [Google Scholar]
- Cilliers HJ, Yeo ST, Salmon NP. Anaesthetic management of an obstetric patient with Pompe disease. Int J Obstet Anesth. 2008;17:170–173. doi: 10.1016/j.ijoa.2007.11.001. [DOI] [PubMed] [Google Scholar]
- de Vries JM, Brugma JD, Ozkan L, et al. First experience with enzyme replacement therapy during pregnancy and lactation in Pompe disease. Mol Genet Metab. 2011;104:552–555. doi: 10.1016/j.ymgme.2011.09.012. [DOI] [PubMed] [Google Scholar]
- Donnelly JC, O’Connell MP, Keane DP. Addison’s disease, with successful pregnancy outcome. J Obstet Gynaecol. 2003;23:199. [PubMed] [Google Scholar]
- Fux Otta C, Szafryk de Mereshian P, Iraci GS, Ojeda de Pruneda MR. Pregnancies associated with primary adrenal insufficiency. Fertil Steril. 2008;90(1199):e1117–e1120. doi: 10.1016/j.fertnstert.2007.08.079. [DOI] [PubMed] [Google Scholar]
- Halperin Rabinovich I, Obiols Alfonso G, Soto Moreno A, et al. Clinical Practice Guideline for Hypothalamic-Pituitary Disturbances in Pregnancy and the Postpartum Period. Endocrinol Nutr. 2008;55:29–43. doi: 10.1016/S1575-0922(08)70633-8. [DOI] [PubMed] [Google Scholar]
- Heidemann B (2003) Changes in maternal physiology during pregnancy. Br J Anaesth 3
- Karabul N, Berndt J, Kornblum C, et al. Pregnancy and delivery in women with Pompe disease. Mol Genet Metab. 2014;112:148–153. doi: 10.1016/j.ymgme.2014.03.010. [DOI] [PubMed] [Google Scholar]
- Kim WS, Cho AR, Hong JM, et al. Combined general and epidural anesthesia for major abdominal surgery in a patient with Pompe disease. J Anesth. 2010;24:768–773. doi: 10.1007/s00540-010-0984-4. [DOI] [PubMed] [Google Scholar]
- Kuczkowski KM, Reisner LS, Benumof JL. Airway problems and new solutions for the obstetric patient. J Clin Anesth. 2003;15:552–563. doi: 10.1016/j.jclinane.2002.12.001. [DOI] [PubMed] [Google Scholar]
- Lehberger J, Roth R, Weingartner K, Heesen M. Pompe disease: anesthesiological special features. Anaesthesist. 2012;61:229–233. doi: 10.1007/s00101-012-1998-0. [DOI] [PubMed] [Google Scholar]
- Lindsay JR, Nieman LK. The hypothalamic-pituitary-adrenal axis in pregnancy: challenges in disease detection and treatment. Endocr Rev. 2005;26:775–799. doi: 10.1210/er.2004-0025. [DOI] [PubMed] [Google Scholar]
- Schuller A, Kornblum C, Deschauer M, et al. Diagnosis and therapy of late onset Pompe disease. Nervenarzt. 2013;84:1467–1472. doi: 10.1007/s00115-013-3947-9. [DOI] [PubMed] [Google Scholar]
- Teener JW. Late-onset Pompe’s disease. Semin Neurol. 2012;32:506–511. doi: 10.1055/s-0033-1334469. [DOI] [PubMed] [Google Scholar]
- überarbeitete Empfehlungen der Deutschen Gesellschaft für Anästhesiologie und Intensivmedizin und des Berufsverbandes Deutscher Anästhesisten in Zusammen arbeit mit der Deutschen Gesellschaft für Gynäkologie und Geburtshilfe Durchführung von Analgesie- und Anästhesieverfahren in der Geburtshilfe. Anästh Intensivmed. 2004;45:151–153. [Google Scholar]
- Zagnoli F, Leblanc A, Blanchard C. Pregnancy during enzyme replacement therapy for late-onset acid maltase deficiency. Neuromuscul Disord. 2013;23:180–181. doi: 10.1016/j.nmd.2012.11.006. [DOI] [PubMed] [Google Scholar]


