Abstract
Background
As a consequence of a rapid growth of an ageing population, more people with dementia are expected on the roads. Little is known about whether these people are at increased risk of road traffic-related accidents.
Objective
Our study aims to investigate the risk of road traffic-related accidents for people aged 65 years or older with a diagnosis of dementia in Denmark.
Methods
We will conduct a nationwide population-based cohort study consisting of Danish people aged 65 or older living in Denmark as of January 1, 2008. The cohort is followed for 7 years (2008-2014). Individual’s personal data are available in Danish registers and can be linked using a unique personal identification number. A person is identified with dementia if the person meets at least one of the following criteria: (1) a diagnosis of the disease in the Danish National Patient Register or in the Danish Psychiatric Central Research Register, and/or (2) at least one dementia diagnosis-related drug prescription registration in the Danish National Prescription Registry. Police-, hospital-, and emergency room-reported road traffic-related accidents occurred within the study follow-up are defined as the study outcome. Cox proportional hazard regression models are used for the main analysis.
Results
Our study protocol has 3 phases including data collection, data analysis, and reporting. The first phase of register-based data collection of 853,228 individual’s personal information was completed in August, 2016. The next phase is data analysis, which is expected to be finished before December 2016, and thereafter writing publications based on the findings. The study started in January 2016 and will end in December 2018.
Discussion
This study covers the entire elderly population of Denmark, and thereby will avoid selection bias due to nonparticipation and loss to follow-up. Furthermore, this ensures that the study results are reliable and generalizable. However, underreporting of traffic-related accidents may occur, which will limit estimation of absolute risks.
Keywords: dementia, accidents, traffic, comorbidity, epidemiology, public health
Introduction
Background
The elderly population is rapidly increasing globally as a result of extended life expectancy due to the success of social, medical, and economic development [1,2]. Consequently, ageing brings societal challenges due to the increase in the proportion of elderly people with chronic diseases including dementia [3].
Dementia is one of the major causes of functional disabilities and dependency among elderly people [4-6]. It is a symptomatic decline in cognitive ability severe enough to affect daily activities, and is usually irreversible, accumulative, and age-dependent [7]. Alzheimer disease and vascular dementia are the most common causes of dementia, other diseases and injuries to the brain are also contributing factors [8].
The prevalence of dementia is expected to increase substantially in parallel with elderly population growth [9]. By 2050, there will be a projected 135 million people suffering from dementia worldwide [3]. Denmark is facing the brunt of the dementia epidemic, an approximately 150,000 Danes are estimated to be afflicted with dementia by 2040, which is nearly doubled than of 2015 [10].
Elderly people in Denmark tend to choose cycling, walking, and private motor vehicles, as their daily mode of transportation [11]. Hence, leading society to a growing concern regarding road traffic-related accidents risk among those suffering from dementia in the coming years. The Statistics Denmark (DST) reported a total of 3375 road traffic-related accidents, including 182 fatal accidents occurring in 2014. Of those accidents, 15% of total and 32% of fatal accidents occurring among people aged 65 or older [12]. Dementia-related accidents within this group of people have never been well reported in Denmark.
However, older people do not necessarily pose an increased risk of traffic accidents as compared with other age groups, as age itself is a poor indicator of movement competence due to individual practice, experience, and general functioning skills being different [13]. However, dementia as a cognitive impairment disorder may affect vision, balance, judgement, perception, motor skills, and problem-solving, therefore it could increase the risk of traffic accidents [14]. Certain people with mild dementia however may still be capable of conducting themselves safely in traffic, at least for a certain period of time [15]. But, it is worth noting that motor skills are deteriorating, depending on the type and the severity levels of the dementia onset, and therefore the risk of accidents may vary [16,17].
Relatively limited numbers of studies have investigated dementia for the risk of traffic accidents, but with inconsistent results. Among published studies, approximately 2 to 10 times higher risks of crashes for people with dementia have been reported [18-21]. However, some others have reported no significant risk difference between people with dementia and their controls [22,23]. Despite traffic accidents being infrequent among elderly people, heterogeneity, small study population, and the quality of accident reporting, justify further studies into dementia and traffic accidents. Nationwide cohort studies with register-based information including exposures, confounders, and various health-related outcomes may fill these gaps.
A population-based Swedish study from 2013 with a sample size of more than 6.9 million people aged 20 years or older, found that the risk of total accidental deaths, including falls, suicides, transport accidents, and accidental poisoning, was 6- to 7-fold higher among people with dementia compared with the general population during 8 years of follow-up [24]. However, the Swedish study only measured accidental death, and therefore this study was not able to identify risk for nonfatal traffic accidents. Additionally, the Swedish study did not adjust for chronic illnesses and possibly harmful medications (eg, tranquillizers and sleeping medication) that may potentially affect the accidental risk [25].
Dementia is often comorbid with other chronic diseases, and the risk of having multiple morbidity increases with age [2,26]. In primary care in America, there is an average of 2.4 additional chronic diseases and above 5 prescribed medications associated with dementia patients aged 65 or older [27]. In Scotland, only 5.5% people with dementia had no other chronic diseases [28]. Sharing some common risk factors and pathophysiological mechanisms such as inflammation and endothelial dysfunction may be one of the reasons for coexistence of multiple chronic diseases, other factors may also play a role [29].
National prevalence of dementia-related comorbidity in the elderly population in Denmark is unclear. However, depression, Type 2 diabetes (T2D), ischemic heart disease (IHD), and chronic obstructive pulmonary disease (COPD), are among the 10 most common chronic diseases among Danish patients, and have been found as independent risk factors for the development of dementia, and can even exacerbate dementia [30-37]. For instance, a systematic review with 17 cohort studies reported that depression, especially late-life depression, was associated with a significant risk of dementia (pooled risk=1.59, 95% confidence interval (CI)=1.41-1.80) [32]. Another meta-analysis with 19 population-based longitudinal studies found a 2- to 3-fold higher risk of developing dementia with diabetes [38].
Moreover, these chronic diseases have also been reported as independent risk factors for traffic accidents [24,39-41]. A structure review with 7 studies found increased odds, or risk ratios of crashes ranging from 1.9 to 7.7 for people with post stroke [42]. Given that the combined effects of those chronic diseases are higher than single or additive effects [43,44], it is possible that dementia accompanied with other chronic disorders can pose an even higher risk of traffic accidents, and chronic disease-related medications may modify the risk estimations. However, to date, those issues have not been studied in much detail elsewhere, or in Denmark.
Aims of the Study
This study protocol overall aim is to investigate the risk of road traffic-related accidents for people aged 65 years or older with diagnosis of dementia in Denmark. The following will be investigated: (1) the risk of road traffic-related accidents among older people with and without dementia, (2) the effect modification of dementia and association with the risk of road traffic accidents by comorbidities, and (3) the effect modification of dementia and association with the risk of road traffic accidents by sedative prescription medications.
Methods
Study Design and Population
The study is designed as a register- and population-based cohort study consisting of all residents in Denmark aged 65 years or older as of January 1, 2008 (n=853,228). These people are followed for 7 years from baseline until December 31, 2014 to assess the incidence of road traffic-related accidents attributable to a dementia diagnosis. The follow-up period of 7 years is chosen because (1) the median survival time for people with dementia in Denmark is 6.6 years; this is slightly longer than other countries (median ranged 3.2-6.6 years) [45,46], and (2) the validity of the dementia diagnosis in recent years has increased and therefore is more accurate from 2008 compared with earlier registration [47-50].
Data Sources
Personal-level data are available in the Danish Civil Registration System (CRS) [51]. This registry electronically records the name, address, migration, marital status, date of birth, place of birth, date of death, and other basic information on all residents in Denmark since 1968. Using a unique 10-digit Civil Personal Register (CPR) number assigned to each individual at birth, or to a person who holds a Danish residence upon immigration, one can access an individual’s information in all national registers, hospitals, general practitioners, police offices, and other authorities in Denmark.
Assessment of Dementia and Comorbidity
Dementia and subtype of dementia including Alzheimer’s disease [52], vascular dementia [53], frontotemporal dementia [54], dementia with Lewy bodies [55], mixed dementia [56], Parkinson’s disease [57], and dementia without specification, are identified by any primary and secondary diagnosis in the Danish National Patient Register (NPR) (Table 1), or in the Danish Psychiatric Central Research Register (PCRR) [58,59].
Table 1.
International Classification of Diseases, Tenth Revision (ICD-10) codes for dementia and other chronic diseaseadiagnoses in Danish health registers.
| Diseases |
|
ICD-10 codes |
| Dementia | ||
|
|
Alzheimer’s disease | F00.0, F00.1, F00.2, F00.9, G30.0, G30.1, G30.8, G30.9 |
|
|
Vascular dementia | F01.0, F01.1, F01.2, F01.3, F01.8, F01.9 |
|
|
Frontotemporal dementia | F02.0 |
|
|
Dementia with Lewy bodies | G31.83 |
|
|
Mixed dementia |
|
|
|
Parkinson’s disease | F02.08 |
|
|
Dementia without specification | F03.9 |
|
Other chronic diseases | ||
|
|
Type 2 diabetes | E11 |
|
|
Chronic obstructive pulmonary disease | J44 |
|
|
Ischemic heart disease | I20–I25 |
|
|
Depression | F32-F33 |
|
|
Hypertension | I10, I15 |
|
|
Stroke | I60-I69 |
|
|
Atrial fibrillation | I48 |
|
|
Asthma | J45 |
International Classification of Diseases versions 10 codes (ICD-10) are used for disease classification in the registers. Additionally, the prescription of antidementia drugs and the corresponding Anatomical Therapeutic Chemical (ATC) codes (Multimedia Appendix 1) from the Danish National Prescription Registry (DNPR) are also used to identify people with dementia disorders [60].
To more accurately define the earliest date of a dementia diagnosis, the diagnosis is dated back to either the first inpatient or outpatient record ever mentioning dementia or the first prescription of antidementia medication since the inception of the DNPR, whichever comes first. A person is identified with dementia if this person meets at least one of the following criteria: (1) a diagnosis of disease in NPR or in PCRR, and/or (2) at least one antidementia drug registration in DNPR.
In this study, comorbidity is defined as a person with at least 2 chronic diseases as listed in Table 1. For chronic disease ascertainment, we apply a similar assessment procedure as with dementia. A person is identified with a specific chronic disorder if this person had a diagnosis of disease in NPR or in disease-specified register if available (Multimedia Appendix 2). Because there is no such registration regarding the exact time when the chronic disease symptoms began, we use the date of registration and/or drug prescription as the initial time point for dementia onset and the comorbidity. Therefore, if the date of registration for any of the comorbidities has been recorded prior to the date of dementia registration, we consider the comorbidity has occurred before onset of dementia, and vice versa.
Study Outcomes Ascertainment
The primary outcome (time to first road traffic-related accident event) is Danish police-reported road traffic accidents including minor injuries, serious injuries, and fatal accidents caused by road traffic during the study follow-up interval. The information such as the date, location, and type of traffic accident is recorded in DST. Because some traffic injuries may only be registered by the hospital or emergency room without being reported to the police, any hospital or emergency room diagnosis representing road traffic accident (ICD-10 codes V00-V89, V98-V99) within the study follow-up period in NPR is supplementary being assessed.
Other Covariates
Age, sex, education, marital status, geographic location, and living in a nursing home are examined as predictors and adjustment variables based on prior knowledge in the present study. Those data are available in CRS and in DST. Driving experience (eg, the years of holding a valid driver license) as one of the potential confounders will also be included in the sensitivity analysis if possible. The chronic disease-related medications that impair ability to drive are addressed as covariates in our study and ascertained by the information of side effects from the drug labelling (Multimedia Appendix 3). If medication involvement in the analysis gets too complicated, we will begin with the most common drugs for the listed chronic diseases.
Statistical Analyses
For aims 1, 2, and 3, the relation between a diagnosis of dementia, or of selected comorbid chronic diseases, as well as antidementia medication, and the incidence of traffic accidents, will be analysed in Cox proportional hazard (Cox) regression models. The total period at risk for a person is the time from January 1st, 2008 until the first occurrence of a traffic accident, death, emigration or end-of-follow-up at December 31st, 2014, whichever comes first; the latter 3 occurrences are censoring events. Dementia, and the other selected comorbid conditions, will be modelled as time-varying covariates in that persons contribute to “nondiagnosed” person-years before and “diagnosed” person-years after the first occurrence of the corresponding diagnosis.
The magnitude of the associations will be reported as hazard ratios (HRs) with 95% CIs. The associations of dementia and other selected comorbid conditions with a traffic accident incidence will be adjusted for several potential confounders in multivariable Cox regression models: age, sex, education, marital status, geographic location, living in a nursing home, medication, and Charlson comorbidity index (CCI) [69]. The proportional hazard assumption will be evaluated by adding interaction terms between the logarithm of time and the independent variables to the model; a joint test for these interaction terms evaluates the proportional hazard assumption.
By the addition to the model of interactions between the selected chronic disorders and the dementia diagnosis, we will investigate a possible differential effect of dementia on the incidence of traffic accidents depending on the aforementioned factors. The different impacts of dementia for the different levels of the corresponding interacting variable will be recorded, and the differences will be evaluated for statistical significance.
Study Power Calculation
There were 6323 road traffic accidents (including injuries and fatalities) in 2008 in Denmark, which represented 1.16‰ (6323/5,475,791) of the total population (DST 2008). If we assume that there is a 1% prevalence of dementia in the Danish population (which is lower than the 1.53% that Alzheimer Europe has estimated for 2012) [70], we can, with nationwide data, detect a traffic accident incidence increase from 1.16‰ for those without dementia to 1.60‰ for those with dementia with 80% power and 5% significant level.
There were 661 road traffic accidents in 2008 among people aged 65 years and over in Denmark, which represented 0.78‰ (661/853,041) of people aged 65 and over in Denmark (DST 2008). If we assume that there is a 7% prevalence of dementia in this age group [10,71,72], we can, with these data, detect a traffic accident incidence increase from 0.78‰ for those without dementia to 1.13‰ for those with dementia with 80% power and 5% significant level.
All statistical tests will be two-sided and use a significance alpha level of 5%. STATA 14.0 will be used for all statistical analysis.
Ethical Consideration and Dissemination
The study protocol was approved by the Danish Data Protection Agency for data permission as well as for ethical considerations (J.no. 2016-41-4674).
Results
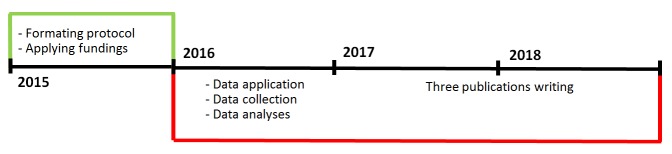
This 3-year PhD study is planned from January 1, 2016 to December 31, 2018. The study timeline is illustrated in the Figure 1. At the current stage, we have finished the data collection, and are beginning the data analysis.
Figure 1.
The study timeline.
Three publications are planned within the protocol. The publication titles at the current stage can potentially be: (1) The risk of road traffic-related accidents among people with dementia, (2) The modification of the dementia and association with the risk of road traffic accidents by comorbidities, or (3) The modification of the dementia and association with the risk of road traffic accidents by sedative prescription medications.
Discussion
Strengths and Limitations
This is the first study to evaluate elderly people with dementia and the link to transport safety injuries in Denmark. With our objectives, we are expecting to find an association between the onset of dementia and the risk of traffic-related accidents among people aged 65 or older.
Denmark is internationally recognized for having rigorous registrations of data regarding many activities. Using nationwide register data to examine the association between dementia and the risk of traffic-related accidents with an entire national elderly population is a major strength of our study, as selection bias due to nonparticipation or loss to follow-up is negligible [47]. The health care system is free of charge and all citizens have equal access to it. Hence, our study results are more reliable and generalizable than those of previous studies with limited sample sizes or case-control designs.
However, underreported traffic-related accidents might occur, and this may limit our risk estimation. It seems a common social norm is that, with very minor traffic accidents such as scratches, the drivers tend to negotiate between each other rather than to rush to report to the police. Nevertheless, using police and hospital, as well as emergency room-registered road traffic accidents, the present study has much more complete data than previous studies on a similar topic.
Implications
Transportation in an ageing society is a general challenge, and it is considered appropriate to actively engage people with dementia and their families in social chores. But the traffic risk has not been well assessed. Therefore, this study may identify the magnitude of traffic accident risk among people with dementia in order to provide initiatives for reducing this potential risk.
Acknowledgments
This 3-year PhD study (2016-2018) is funded by Denmark Health Foundation (15-B-0130), Denmark Psychiatry Research Foundation (R24-A1155-B604), and University of Southern Denmark Faculty Scholarship. The sponsors have no other involvement in this study except for the financing supports.
Abbreviations
- ATC
anatomical therapeutic chemical
- CCI
Charlson comorbidity index
- CI
confidence interval
- COPD
chronic obstructive pulmonary disease
- Cox
Cox proportional hazard
- CPR
Civil Personal Register
- CRS
Danish Civil Registration System
- DNPR
Danish National Prescription Registry
- DST
Statistics Denmark
- HRs
hazard ratios
- ICD-10
International Classification of Diseases, Tenth Revision
- IHD
ischemic heart disease
- NPR
Danish National Patient Register
- PCRR
Danish Psychiatric Central Research Register
- T2D
type 2 diabetes
ATC-codes for drugs in the Danish National Prescription Registry.
Overview of databases and indicators for data assessment.
Medicines labelled with side-effects as impaired driving ability.
Footnotes
Authors' Contributions: Frans Boch Waldorff initiated the project and guided throughout the protocol writing process. Jindong Ding Petersen wrote the protocol. Volkert Siersma advised and drafted the statistical analysis including a power calculation. Connie Thurøe Nielsen and Mikkel Vass gave academic suggestions for the project. All the authors have approved the protocol for publishing.
Conflicts of Interest: None declared.
References
- 1.World Health Organization . Ageing and Life-Course. Facts About Ageing. World Health Organization; 2014. [2016-09-15]. http://www.who.int/ageing/about/facts/en/ [Google Scholar]
- 2.Banerjee S. Multimorbidity--older adults need health care that can count past one. Lancet. 2015;385:587–589. doi: 10.1016/S0140-6736(14)61596-8.S0140-6736(14)61596-8 [DOI] [PubMed] [Google Scholar]
- 3.Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O'Donnell M, Sullivan R, Yusuf S. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385:549–562. doi: 10.1016/S0140-6736(14)61347-7.S0140-6736(14)61347-7 [DOI] [PubMed] [Google Scholar]
- 4.Agüero-Torres H, Fratiglioni L, Guo Z, Viitanen M, von SE, Winblad B. Dementia is the major cause of functional dependence in the elderly: 3-year follow-up data from a population-based study. Am J Public Health. 1998;88:1452–1456. doi: 10.2105/ajph.88.10.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindbergh CA, Dishman RK, Miller LS. Functional disability in mild cognitive impairment: a systematic review and meta-analysis. Neuropsychol Rev. 2016;26:129–159. doi: 10.1007/s11065-016-9321-5.10.1007/s11065-016-9321-5 [DOI] [PubMed] [Google Scholar]
- 6.Park M, Sung M, Kim SK, Kim S, Lee DY. Multidimensional determinants of family caregiver burden in Alzheimer's disease. Int Psychogeriatr. 2015;27:1355–1364. doi: 10.1017/S1041610215000460.S1041610215000460 [DOI] [PubMed] [Google Scholar]
- 7.Caixeta L, Costa JN, Vilela AC, Nóbrega M. The development of the dementia concept in 19th century. Arq Neuropsiquiatr. 2014;72:564–567. doi: 10.1590/0004-282x20140069. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-282X2014000700564&lng=en&nrm=iso&tlng=en .S0004-282X2014000700564 [DOI] [PubMed] [Google Scholar]
- 8.Fleminger S, Oliver DL, Lovestone S, Rabe-Hesketh S, Giora A. Head injury as a risk factor for Alzheimer's disease: the evidence 10 years on; a partial replication. J Neurol Neurosurg Psychiatry. 2003;74:857–862. doi: 10.1136/jnnp.74.7.857. http://jnnp.bmj.com/cgi/pmidlookup?view=long&pmid=12810767 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quaglio G, Brand H, Dario C. Fighting dementia in Europe: the time to act is now. Lancet Neurol. 2016;15:452–454. doi: 10.1016/S1474-4422(16)00079-X.S1474-4422(16)00079-X [DOI] [PubMed] [Google Scholar]
- 10.Danish Dementia Research Centre. [2016-08-25]. Prevalence of Dementia in Denmark http://uk.videnscenterfordemens.dk/dementia-in-denmark/prevalence-of-dementia-in-denmark/
- 11.Siren A, Haustein S. Department of Transport, Bygningstorvet. Lyngby: Technical University of Denmark; 2012. [2016-09-15]. Cohort Analysis of Older Adults' Travel Patterns in Denmark http://orbit.dtu.dk/en/publications/cohort-analysis-of-older-adults-travel-patterns-in-denmark(844f0037-f42f-441a-8b9a-dfbf23ffe134).html . [Google Scholar]
- 12.Statistics Denmark. 2014. [2016-09-15]. Traffic accidents http://www.dst.dk/en/Statistik/emner/trafikulykker .
- 13.Mathias JL, Lucas LK. Cognitive predictors of unsafe driving in older drivers: a meta-analysis. IPG. 2009;21:637–653. doi: 10.1017/S1041610209009119.S1041610209009119 [DOI] [PubMed] [Google Scholar]
- 14.Wagner JT, Müri RM, Nef T, Mosimann UP. Cognition and driving in older persons. Swiss Med Wkly. 2011;140:w13136. doi: 10.4414/smw.2011.13136. http://www.smw.ch/dfe/set_archiv.asp?target=10.4414/smw.2011.13136 .smw-13136 [DOI] [PubMed] [Google Scholar]
- 15.Gilley DW, Wilson RS, Bennett DA, Stebbins GT, Bernard BA, Whalen ME, Fox JH. Cessation of driving and unsafe motor vehicle operation by dementia patients. Arch Intern Med. 1991;151:941–946. [PubMed] [Google Scholar]
- 16.Tolea MI, Morris JC, Galvin JE. Trajectory of mobility decline by type of dementia. Alzheimer Dis Assoc Disord. 2016;30:60–66. doi: 10.1097/WAD.0000000000000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meuleners Lynn B, Ng Jonathon, Chow Kyle, Stevenson Mark. Motor vehicle crashes and dementia: a population-based study. J Am Geriatr Soc. 2016;64:1039–1045. doi: 10.1111/jgs.14109. [DOI] [PubMed] [Google Scholar]
- 18.Zuin D, Ortiz H, Boromei D, Lopez OL. Motor vehicle crashes and abnormal driving behaviours in patients with dementia in Mendoza, Argentina. Eur J Neurol. 2002;9:29–34. doi: 10.1046/j.1468-1331.2002.00296.x.296 [DOI] [PubMed] [Google Scholar]
- 19.Joseph PG, O'Donnell MJ, Teo KK, Gao P, Anderson C, Probstfield JL, Bosch J, Khatib R, Yusuf S. The mini-mental state examination, clinical factors, and motor vehicle crash risk. J Am Geriatr Soc. 2014;62:1419–1426. doi: 10.1111/jgs.12936. [DOI] [PubMed] [Google Scholar]
- 20.Friedland RP, Koss E, Kumar A, Gaine S, Metzler D, Haxby JV, Moore A. Motor vehicle crashes in dementia of the Alzheimer type. Ann Neurol. 1988;24:782–786. doi: 10.1002/ana.410240613. [DOI] [PubMed] [Google Scholar]
- 21.Tuokko H, Tallman K, Beattie BL, Cooper P, Weir J. An examination of driving records in a dementia clinic. J Gerontol B Psychol Sci Soc Sci. 1995;50:S173–S181. doi: 10.1093/geronb/50b.3.s173. [DOI] [PubMed] [Google Scholar]
- 22.Man-Son-Hing M, Marshall SC, Molnar FJ, Wilson KG. Systematic review of driving risk and the efficacy of compensatory strategies in persons with dementia. J Am Geriatr Soc. 2007;55:878–884. doi: 10.1111/j.1532-5415.2007.01177.x.JGS1177 [DOI] [PubMed] [Google Scholar]
- 23.Orriols L, Avalos-Fernandez M, Moore N, Philip P, Delorme B, Laumon B, Gadegbeku B, Salmi L, Lagarde E. Long-term chronic diseases and crash responsibility: a record linkage study. Accid Anal Prev. 2014;71:137–143. doi: 10.1016/j.aap.2014.05.001.S0001-4575(14)00133-X [DOI] [PubMed] [Google Scholar]
- 24.Crump C, Sundquist K, Winkleby MA, Sundquist J. Mental disorders and risk of accidental death. Br J Psychiatry. 2013;203:297–302. doi: 10.1192/bjp.bp.112.123992. http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=23969485 .bjp.bp.112.123992 [DOI] [PubMed] [Google Scholar]
- 25.Orriols L, Queinec R, Philip P, Gadegbeku B, Delorme B, Moore N, Suissa S, Lagarde E. Risk of injurious road traffic crash after prescription of antidepressants. J Clin Psychiatry. 2012;73:1088–1094. doi: 10.4088/JCP.11m07624. http://www.psychiatrist.com/jcp/article/pages/2012/v73n08/v73n0807.aspx . [DOI] [PubMed] [Google Scholar]
- 26.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(12)60240-2 .S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 27.Schubert CC, Boustani M, Callahan CM, Perkins AJ, Carney CP, Fox C, Unverzagt F, Hui S, Hendrie HC. Comorbidity profile of dementia patients in primary care: are they sicker? J Am Geriatr Soc. 2006;54:104–109. doi: 10.1111/j.1532-5415.2005.00543.x.JGS543 [DOI] [PubMed] [Google Scholar]
- 28.Banerjee S. Multimorbidity--older adults need health care that can count past one. Lancet. 2015;385:587–589. doi: 10.1016/S0140-6736(14)61596-8.S0140-6736(14)61596-8 [DOI] [PubMed] [Google Scholar]
- 29.Muqtadar H, Testai FD, Gorelick PB. The dementia of cardiac disease. Curr Cardiol Rep. 2012;14:732–740. doi: 10.1007/s11886-012-0304-8. [DOI] [PubMed] [Google Scholar]
- 30.Peila R, Rodriguez BL, Launer LJ, Honolulu-Asia AS. Type 2 diabetes, APOE gene, and the risk for dementia and related pathologies: The Honolulu-Asia Aging Study. Diabetes. 2002;51:1256–1262. doi: 10.2337/diabetes.51.4.1256. http://diabetes.diabetesjournals.org/cgi/pmidlookup?view=long&pmid=11916953 . [DOI] [PubMed] [Google Scholar]
- 31.Pellegrino LD, Peters ME, Lyketsos CG, Marano CM. Depression in cognitive impairment. Curr Psychiatry Rep. 2013;15:384. doi: 10.1007/s11920-013-0384-1. http://europepmc.org/abstract/MED/23933974 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diniz BS, Butters MA, Albert SM, Dew MA, Reynolds CF. Late-life depression and risk of vascular dementia and Alzheimer's disease: systematic review and meta-analysis of community-based cohort studies. Br J Psychiatry. 2013;202(5):329–335. doi: 10.1192/bjp.bp.112.118307. http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=23637108 .202/5/329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.da Silva J, Gonçalves-Pereira Manuel, Xavier M, Mukaetova-Ladinska EB. Affective disorders and risk of developing dementia: systematic review. Br J Psychiatry. 2013;202:177–186. doi: 10.1192/bjp.bp.111.101931. http://bjp.rcpsych.org/cgi/pmidlookup?view=long&pmid=23457181 .202/3/177 [DOI] [PubMed] [Google Scholar]
- 34.Liao W, Lin C, Chang S, Tu C, Kao C. The association between chronic obstructive pulmonary disease and dementia: a population-based retrospective cohort study. Eur J Neurol. 2015;22:334–340. doi: 10.1111/ene.12573. [DOI] [PubMed] [Google Scholar]
- 35.Abete P, Della-Morte D, Gargiulo G, Basile C, Langellotto A, Galizia G, Testa G, Canonico V, Bonaduce D, Cacciatore F. Cognitive impairment and cardiovascular diseases in the elderly. A heart-brain continuum hypothesis. Ageing Res Rev. 2014;18:41–52. doi: 10.1016/j.arr.2014.07.003.S1568-1637(14)00068-3 [DOI] [PubMed] [Google Scholar]
- 36.Li J, Shao Y, Gong Y, Lu Y, Liu Y, Li C. Diabetes mellitus and dementia - a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2014;18:1778–1789. http://www.europeanreview.org/article/7530 . [PubMed] [Google Scholar]
- 37.Singh B, Parsaik AK, Mielke MM, Roberts RO, Scanlon PD, Geda YE, Pankratz VS, Christianson T, Yawn BP, Petersen RC. Chronic obstructive pulmonary disease and association with mild cognitive impairment: the Mayo Clinic Study of Aging. Mayo Clin Proc. 2013;88:1222–1230. doi: 10.1016/j.mayocp.2013.08.012. http://europepmc.org/abstract/MED/24182702 .S0025-6196(13)00731-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern Med J. 2012;42:484–491. doi: 10.1111/j.1445-5994.2012.02758.x. [DOI] [PubMed] [Google Scholar]
- 39.Cox DJ, Singh H, Lorber D. Diabetes and driving safety: science, ethics, legality and practice. Am J Med Sci. 2013;345:263–265. doi: 10.1097/MAJ.0b013e31828bf8d7. http://europepmc.org/abstract/MED/23531955 .S0002-9629(15)30685-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Inkster B, Frier BM. Diabetes and driving. Diabetes Obes Metab. 2013;15:775–783. doi: 10.1111/dom.12071. [DOI] [PubMed] [Google Scholar]
- 41.Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. 2011;343:d4551. doi: 10.1136/bmj.d4551. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=21810886 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Perrier M, Korner-Bitensky N, Petzold A, Mayo N. The risk of motor vehicle crashes and traffic citations post stroke: a structured review. Top Stroke Rehabil. 2010;17:191–196. doi: 10.1310/tsr1703-191.KM33612617241266 [DOI] [PubMed] [Google Scholar]
- 43.Katon WJ, Lin E, Williams LH, Ciechanowski P, Heckbert SR, Ludman E, Rutter C, Crane PK, Oliver M, Von KM. Comorbid depression is associated with an increased risk of dementia diagnosis in patients with diabetes: a prospective cohort study. J Gen Intern Med. 2010;25:423–429. doi: 10.1007/s11606-009-1248-6. http://europepmc.org/abstract/MED/20108126 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sullivan MD, Katon WJ, Lovato LC, Miller ME, Murray AM, Horowitz KR, Bryan RN, Gerstein HC, Marcovina S, Akpunonu BE, Johnson J, Yale JF, Williamson J, Launer LJ. Association of depression with accelerated cognitive decline among patients with type 2 diabetes in the ACCORD-MIND trial. JAMA Psychiatry. 2013;70:1041–1047. doi: 10.1001/jamapsychiatry.2013.1965. http://europepmc.org/abstract/MED/23945905 .1727436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Andersen K, Lolk A, Martinussen T, Kragh-Sørensen P. Very mild to severe dementia and mortality: A 14-year follow-up - The Odense study. Dement Geriatr Cogn Disord. 2010;29:61–67. doi: 10.1159/000265553.000265553 [DOI] [PubMed] [Google Scholar]
- 46.Todd S, Barr S, Roberts M, Passmore AP. Survival in dementia and predictors of mortality: a review. Int J Geriatr Psychiatry. 2013;28:1109–1124. doi: 10.1002/gps.3946. [DOI] [PubMed] [Google Scholar]
- 47.Phung TK, Andersen BB, Høgh P, Kessing LV, Mortensen PB, Waldemar G. Validity of dementia diagnoses in the Danish hospital registers. Dement Geriatr Cogn Disord. 2007;24:220–228. doi: 10.1159/000107084. http://www.karger.com?DOI=10.1159/000107084 .000107084 [DOI] [PubMed] [Google Scholar]
- 48.Phung K, Waltoft B, Kessing L, Mortensen P, Waldemar G. P4-124: Is dementia underdiagnosed? A nationwide population-based study using national registers. Alzheimer's & Dementia. 2008;4:T706. doi: 10.1016/j.jalz.2008.05.2190. http://www.alzheimersanddementia.com/article/S1552-5260(08)02350-9/abstract . [DOI] [Google Scholar]
- 49.Phung TK, Waltoft BL, Kessing LV, Mortensen PB, Waldemar G. Time trend in diagnosing dementia in secondary care. Dement Geriatr Cogn Disord. 2010;29:146–153. doi: 10.1159/000269933.000269933 [DOI] [PubMed] [Google Scholar]
- 50.Alzheimer Europe alzheimer-europe.org. 2013. May 14, [2016-09-15]. National Dementia Strategies (Diagnosis, Treatment and Research)-Denmark http://www.alzheimer-europe.org/Policy-in-Practice2/Country-comparisons/National-Dementia-Strategies-diagnosis-treatment-and-research/Denmark .
- 51.Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29:541–549. doi: 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 52.Scheltens P, Blennow K, Breteler MM, de Strooper SB, Frisoni GB, Salloway S, Van der Flier WM. Alzheimer's disease. Lancet. 2016;388:505–517. doi: 10.1016/S0140-6736(15)01124-1.S0140-6736(15)01124-1 [DOI] [PubMed] [Google Scholar]
- 53.O'Brien JT, Thomas A. Vascular dementia. Lancet. 2015;386:1698–1706. doi: 10.1016/S0140-6736(15)00463-8.S0140-6736(15)00463-8 [DOI] [PubMed] [Google Scholar]
- 54.Bang J, Spina S, Miller BL. Frontotemporal dementia. Lancet. 2015;386:1672–1682. doi: 10.1016/S0140-6736(15)00461-4.S0140-6736(15)00461-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Walker Z, Possin KL, Boeve BF, Aarsland D. Lewy body dementias. Lancet. 2015;386:1683–1697. doi: 10.1016/S0140-6736(15)00462-6.S0140-6736(15)00462-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.De Reuck J, Deramecourt V, Cordonnier C, Pasquier F, Leys D, Maurage C, Bordet R. The incidence of post-mortem neurodegenerative and cerebrovascular pathology in mixed dementia. J Neurol Sci. 2016;366:164–166. doi: 10.1016/j.jns.2016.05.021.S0022-510X(16)30279-9 [DOI] [PubMed] [Google Scholar]
- 57.Barnett R. Parkinson's disease. Lancet. 2016;387:217. doi: 10.1016/S0140-6736(16)00049-0.S0140-6736(16)00049-0 [DOI] [PubMed] [Google Scholar]
- 58.Thomsen RW, Lange P, Hellquist B, Frausing E, Bartels PD, Krog BR, Hansen AS, Buck D, Bunk AE. Validity and underrecording of diagnosis of COPD in the Danish National Patient Registry. Respir Med. 2011;105:1063–1068. doi: 10.1016/j.rmed.2011.01.012. http://linkinghub.elsevier.com/retrieve/pii/S0954-6111(11)00027-8 .S0954-6111(11)00027-8 [DOI] [PubMed] [Google Scholar]
- 59.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(Suppl):54–57. doi: 10.1177/1403494810395825.39/7_suppl/54 [DOI] [PubMed] [Google Scholar]
- 60.Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39(Suppl):38–41. doi: 10.1177/1403494810394717.39/7_suppl/38 [DOI] [PubMed] [Google Scholar]
- 61.Moth G, Vestergaard M, Vedsted P. Chronic care management in Danish general practice--a cross-sectional study of workload and multimorbidity. BMC Fam Pract. 2012;13:52. doi: 10.1186/1471-2296-13-52. http://bmcfampract.biomedcentral.com/articles/10.1186/1471-2296-13-52 .1471-2296-13-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kanmanthareddy A, Vallakati A, Sridhar A, Reddy M, Sanjani HP, Pillarisetti J, Atkins D, Bommana S, Jaeger M, Berenbom L, Lakkireddy D. The impact of atrial fibrillation and its treatment on dementia. Curr Cardiol Rep. 2014;16:519. doi: 10.1007/s11886-014-0519-y. [DOI] [PubMed] [Google Scholar]
- 63.Udompanich S, Lip GY, Apostolakis S, Lane DA. Atrial fibrillation as a risk factor for cognitive impairment: a semi-systematic review. QJM. 2013;106:795–802. doi: 10.1093/qjmed/hct129. http://qjmed.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=23737509 .hct129 [DOI] [PubMed] [Google Scholar]
- 64.Sharp SI, Aarsland D, Day S, Sønnesyn Hogne, Ballard C, Alzheimer's Society Vascular Dementia Systematic Review Group Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2011;26:661–669. doi: 10.1002/gps.2572. [DOI] [PubMed] [Google Scholar]
- 65.Peng Y, Wu B, Su C, Liao W, Muo C, Hsia T, Kao C. Adult asthma increases dementia risk: a nationwide cohort study. J Epidemiol Community Health. 2015;69:123–128. doi: 10.1136/jech-2014-204445.jech-2014-204445 [DOI] [PubMed] [Google Scholar]
- 66.Rozzini L, Riva M, Ghilardi N, Facchinetti P, Forbice E, Semeraro F, Padovani A. Cognitive dysfunction and age-related macular degeneration. Am J Alzheimers Dis Other Demen. 2014;29:256–262. doi: 10.1177/1533317513517032.1533317513517032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Murgatroyd C, Prettyman R. An investigation of visual hallucinosis and visual sensory status in dementia. Int J Geriatr Psychiatry. 2001;16:709–713. doi: 10.1002/gps.426. [DOI] [PubMed] [Google Scholar]
- 68.Kanaan A, Huertas P, Santiago A, Sánchez JA, Martínez P. Incidence of different health factors and their influence on traffic accidents in the province of Madrid, Spain. Leg Med (Tokyo) 2009;Suppl 1:S333–S336. doi: 10.1016/j.legalmed.2009.01.010.S1344-6223(09)00017-0 [DOI] [PubMed] [Google Scholar]
- 69.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 70.Alzheimer Europe alzheimer-europe.org. 2014. [2016-09-15]. The Prevalence of Dementia in Europe http://www.alzheimer-europe.org/Policy-in-Practice2/Country-comparisons/The-prevalence-of-dementia-in-Europe/Denmark .
- 71.Prince Martin, Bryce Renata, Albanese Emiliano, Wimo Anders, Ribeiro Wagner, Ferri Cleusa P. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75, e2. doi: 10.1016/j.jalz.2012.11.007.S1552-5260(12)02531-9 [DOI] [PubMed] [Google Scholar]
- 72.Rosenbaum B, Kristensen M, Schmidt J. [Dementia in elderly Turkish immigrants] Ugeskr Laeger. 2008;170:4109–4113.VP51411 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ATC-codes for drugs in the Danish National Prescription Registry.
Overview of databases and indicators for data assessment.
Medicines labelled with side-effects as impaired driving ability.