Abstract
Reactive gliosis is an early pathological feature common to most neurodegenerative diseases, yet its regulation and impact remain poorly understood. Normally astrocytes maintain a critical homeostatic balance. After stress or injury they undergo rapid parainflammatory activation, characterized by hypertrophy, and increased polymerization of type III intermediate filaments (IFs), particularly glial fibrillary acidic protein and vimentin. However, the consequences of IF dynamics in the adult CNS remains unclear, and no pharmacologic tools have been available to target this mechanism in vivo. The mammalian retina is an accessible model to study the regulation of astrocyte stress responses, and their influence on retinal neuronal homeostasis. In particular, our work and others have implicated p38 mitogen-activated protein kinase (MAPK) signaling as a key regulator of glutamate recycling, antioxidant activity and cytokine secretion by astrocytes and related Müller glia, with potent influences on neighboring neurons. Here we report experiments with the small molecule inhibitor, withaferin A (WFA), to specifically block type III IF dynamics in vivo. WFA was administered in a model of metabolic retinal injury induced by kainic acid, and in combination with a recent model of debridement-induced astrocyte reactivity. We show that WFA specifically targets IFs and reduces astrocyte and Müller glial reactivity in vivo. Inhibition of glial IF polymerization blocked p38 MAPK-dependent secretion of TNF-α, resulting in markedly reduced neuronal apoptosis. To our knowledge this is the first study to demonstrate that pharmacologic inhibition of IF dynamics in reactive glia protects neurons in vivo.
Astrocyte reactivity (reactive gliosis) is an early pathological feature common to most neurodegenerative diseases, yet its regulation and impact remains poorly understood. In the healthy central nervous system (CNS), astrocytes coordinate homeostatic vascular perfusion, free radical detoxification and neurotransmitter recycling.1, 2 Injury or stress induces a phenotypic switch, whose cardinal features are cellular hypertrophy and increased expression and polymerization of type III intermediate filaments (IFs), particularly glial fibrillary acidic protein (GFAP).3, 4, 5 The role of intermediate filaments in reactive gliosis remains unclear.3, 6, 7, 8, 9 Genetic deletion of IFs GFAP and vimentin have been shown to promote axonal outgrowth and regeneration in developing neurons and models of CNS injury,10, 11, 12 yet result in developmental defects to inner retinal function13 and increased damage in models of Alzheimer's disease.14 Genetically, GFAP gain of function mutations associated with Alexander's disease induce a p38 mitogen-activated protein kinase (MAPK)-dependent pathology.15 However, no pharmacologic tools have been available to specifically modulate and explore this reactive switch in the context of pathological CNS injury. Consequently, strategies to therapeutically target the reactive switch have remain challenging to explore.
Withaferin A (WFA) is a small molecule withanolide that is a potent and specific inhibitor of type III intermediate filament dynamics.16, 17, 18 Its activity has been most closely studied with respect to vimentin rearrangement and phosphorylation in the context of angiogenesis, fibrosis and cancer, through downstream effects on inflammatory signaling and cell proliferation.19, 20, 21, 22, 23, 24 Interestingly, WFA has been reported to regulate vimentin-mediated activation of MAPKs in a context dependent manner, as well as NFκB.25, 26 Recently Bargagna-Mohan et al.27 reported that, in addition to vimentin, WFA also binds covalently to GFAP at cysteine 294. In these studies WFA impaired GFAP filament assembly and polymerization in cultured astrocytes, and in vivo in retinal astrocytes and related Müller glia in a model of injury-induced gliosis.27 Therefore, WFA presents a novel tool to test the pharmacologic blockade of intermediate filament remodeling during gliosis. However, the consequences of WFA disruption of IFs on neuronal damage has not been studied.
We have previously used the retina as a uniquely accessible model to study the regulation of astrocyte stress responses, and their influence on retinal neuronal survival.28, 29, 30 In the human and rodent eye retinal ganglion cells (RGCs) and amacrine cells of the inner retina maintain a delicate homeostatic balance and are particularly vulnerable to excitotoxic and metabolic damage, mediated in part through non-cell autonomous interactions with neighboring glia.31, 32, 33, 34 In addition, our work and others has implicated signaling through p38 MAPKs as key regulators of glutamate recycling, antioxidant activity, and cytokine secretion in neighboring stress-activated retinal astrocytes and Müller glia.29, 35, 36, 37 Here we take advantage of a model of induced retinal astrocyte reactivity to establish whether WFA, and the selective p38 MAPK inhibitor SB203580 (SB), affect neuronal apoptosis in a mouse model of excitotoxic injury.
Results
WFA and SB treatment blocks glial reactivity and rescues retinal neurons from apoptosis
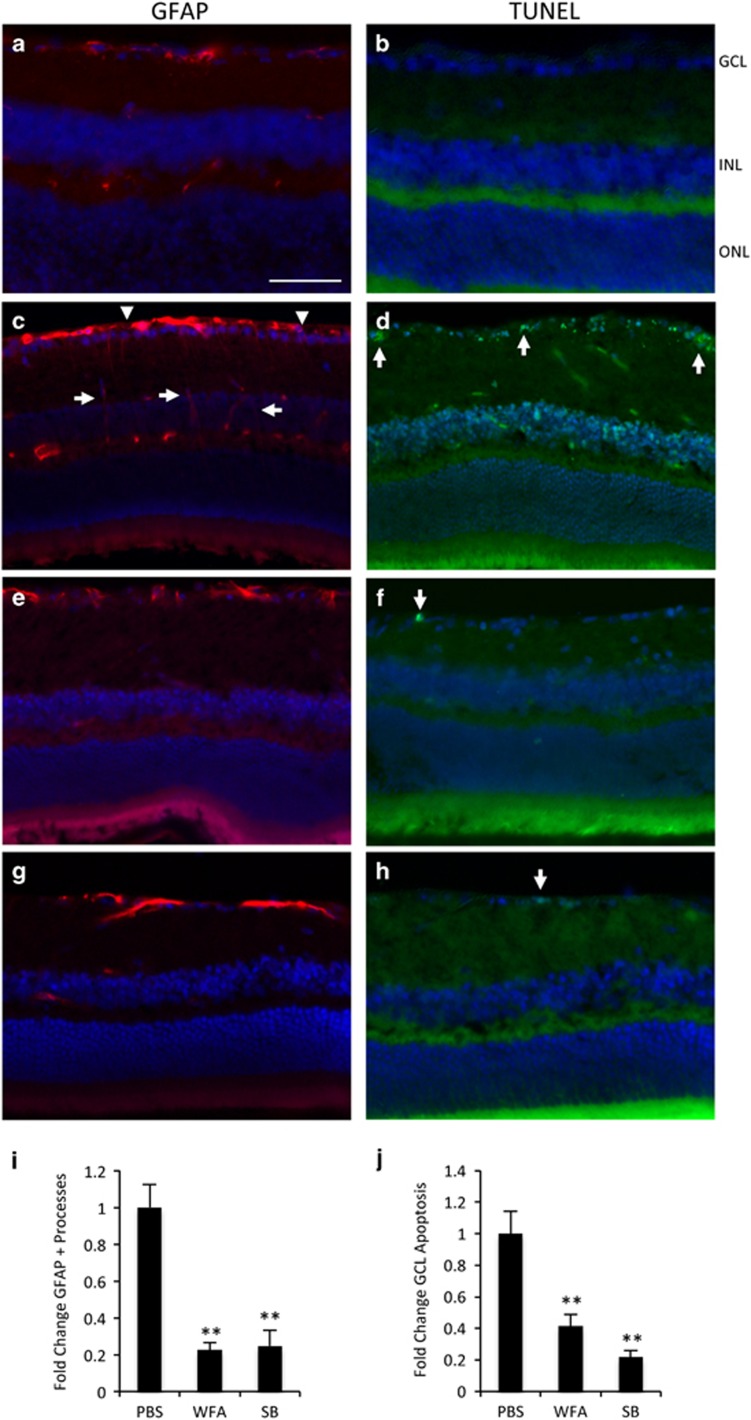
For the present series of experiments we utilized a well-established excitotoxic model of inner retinal injury that is closely associated with reactivity of resident astrocytes and Müller glia.33, 38, 39, 40, 41, 42 Intraocular injection of kainic acid (KA) consistently generated rapid accumulation of GFAP in retinal astrocytes and Müller fibers (Figure 1a and c), and apoptosis of RGCs and amacrine cells in the ganglion cell layer (GCL) and inner nuclear layer (INL) by 18 h (Figure 1b and d). This method facilitates rapid and accurate quantification of markers for the resulting neuronal apoptosis and glial reactivity.28 In order to study the influence of IF dynamics on this model, we first tested the efficacy of WFA and the selective p38α and β-MAPK inhibitor SB203580 (SB).
Figure 1.
WFA and SB inhibit retinal gliosis and apoptosis. (a and b) Intraocular injection of vehicle alone leads to no increase in GFAP stained glial fibers or TUNEL stained apoptotic cells. (c and d) Injection of KA induces increased GFAP staining of retinal astrocytes (arrowheads), and induced staining in Müller fibers (arrows) and apoptotic death of cells in the GCL (arrows) and INL by 18 h. (e and f) Treatment with WFA blocks the increased GFAP and TUNEL staining. (g and h) Treatment with SB203580 (SB) similarly blocks the increased GFAP and TUNEL staining. (i) Quantification of the GFAP and TUNEL results from multiple animals showing fold change compared with contralateral control eyes (bars indicate S.E., **P<0.01, n⩾4). Scale bar indicates 50 μm. GCL, ganglion cell layer; INL, inner nuclear layer; ONL, outer nuclear layer. All of the following panels and images are oriented in the same way
Mice were administered either WFA (2 mg/kg), or vehicle control. WFA strongly reduced GFAP levels in inner retinal astrocytes and Müller fibers following KA challenge (Figure 1e). WFA treatment also resulted in a corresponding marked reduction in inner retinal apoptosis in the GCL and INL compared with control mice (Figure 1f). As we have previously determined that blocking p38 MAPK reduces activation of retinal astrocytes in vitro,29 we also tested intravitreal administration of SB (2 mM), which similarly strongly reduced GFAP staining (Figure 1g), and markedly decreased neuronal apoptosis compared with vehicle (Figure 1h).
To quantify the extent of retinal gliosis and neuronal apoptosis in these studies, we followed established procedures to count activated Müller glia and GCL death. However, similar patterns were also observed in the INL (Figure 1a–h). For gliosis quantification, the number of GFAP-positive processes crossing the inner plexiform layer were counted across the retina in multiple sections through the level of the optic nerve head, and averaged for multiple animals.43 On adjacent sections TUNEL-positive cells in the GCL were similarly quantified across the retina and averaged by established methods.28, 44, 45, 46 These analyses confirmed a highly significant 80% reduction in GFAP-positive processes for both WFA and SB, and 60% and 80% reductions in GCL apoptosis, respectively (Figure 1i and j). Therefore, administration of WFA or SB effectively blocked KA-induced reactivity and apoptosis in the retina.
WFA treatment compromises intermediate filament polymerization
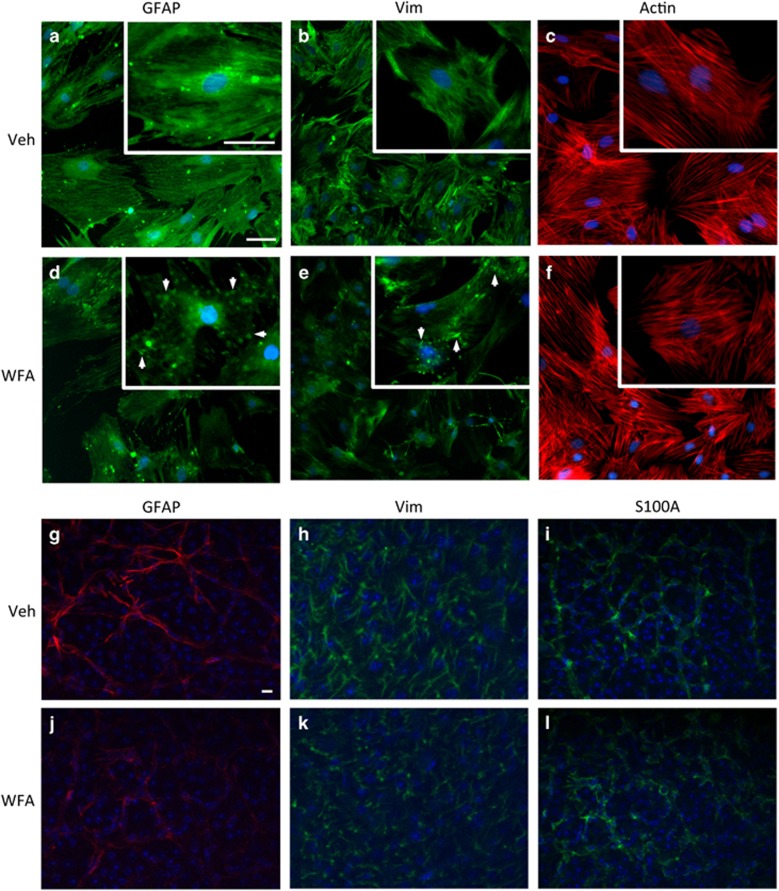
In order to confirm the direct activity of WFA on astrocyte IFs, we treated cultured retinal astrocytes with the drug for subsequent analyses by fluorescent microscopy. Highly enriched retinal astrocyte cultures were established from adult rats according to our published methods.28, 29, 30 We have previously shown that these cells present typical astrocytic morphology, and a variety of specific markers, including GFAP, vimentin, Pax-2, glutamine synthetase (GS) and S100A.29 They also robustly respond to metabolic and oxidative stress with p38 MAPK-dependent changes in activation markers, secreted cytokines and antioxidants.29 In the present study, vimentin and GFAP filaments were assessed in retinal astrocytes by fluorescent microscopy following treatment with 2 μM WFA or vehicle. Both vimentin and GFAP showed reduced filamentous signal and the formation of short aggregates following WFA exposure (Figure 2a–b and d–e). In comparison, staining for actin showed no effect on filament assembly (Figure 2c and f). These specific WFA effects on IF polymerization are consistent with previous reports.16, 27
Figure 2.
WFA treatment inhibits IF dynamics. (a–f) Treatment of cultured retinal astrocytes with 2.0 μm WFA resulted in reduced staining for GFAP (a and d), and vimentin (vim; b and e), compared with control treated cells after 8 h. At higher magnifications (insets), filamentous staining for GFAP and vimentin was disrupted, resulting in formation of IF aggregates (arrows). In comparison, filamentous actin remained unaffected (c and f). (n=3, scale bars indicate 100 μm. Identical exposures were used for all treatments). (g–l) WFA treatment in vivo similarly disrupts GFAP and vimentin in retinal flatmounts, but not S100A. (n=3, scale bars indicate 100 μm. Identical exposures were used for all treatments)
To confirm these effects in vivo, retinas from control and WFA-treated mice were also flatmounted and probed for GFAP and vimentin, followed by imaging with confocal microscopy. The intensity and extent of GFAP and vimentin filaments was reduced in WFA-treated animals compared with vehicle, consistent with our in vitro results (Figure 2g–h and j–k). By comparison, staining for the astrocyte marker S100 was not strongly affected and indicated similar numbers of cells in treated and vehicle samples, but with apparent changes to astrocyte morphology (Figure 2i and l). Likewise, there were no WFA-induced changes in staining for GS in retinal sections (Supplementary Figure 1). In general the treated astrocytes appeared smaller with fewer processes (Figure 2j–l).
A non-invasive injury model of induced retinal glial activation
Demonstrating IF-dependent effects in vivo is challenging due to developmental and compensatory effects of induced gene deletions, and the intimate associations between glial reactivity and neurodegeneration. For this purpose we took advantage of a recently described model of induced retinal glial activation. Bargagna-Mohan et al. reported that mechanical corneal debridement-induced sensitive and robust retinal astrogliosis, but did not cause any apparent changes in retinal morphology or pathology compared with untreated eyes.27, 47 This new model of retinal astrocyte reactivity provides a unique opportunity for investigating the influence of injury-induced glial reactivity on neurovascular tissue. We decided to use this assay to test the reactivity-dependent effects of WFA and SB. In order to adapt the model for this purpose, we first set out to reproduce and expand the previously reported results.
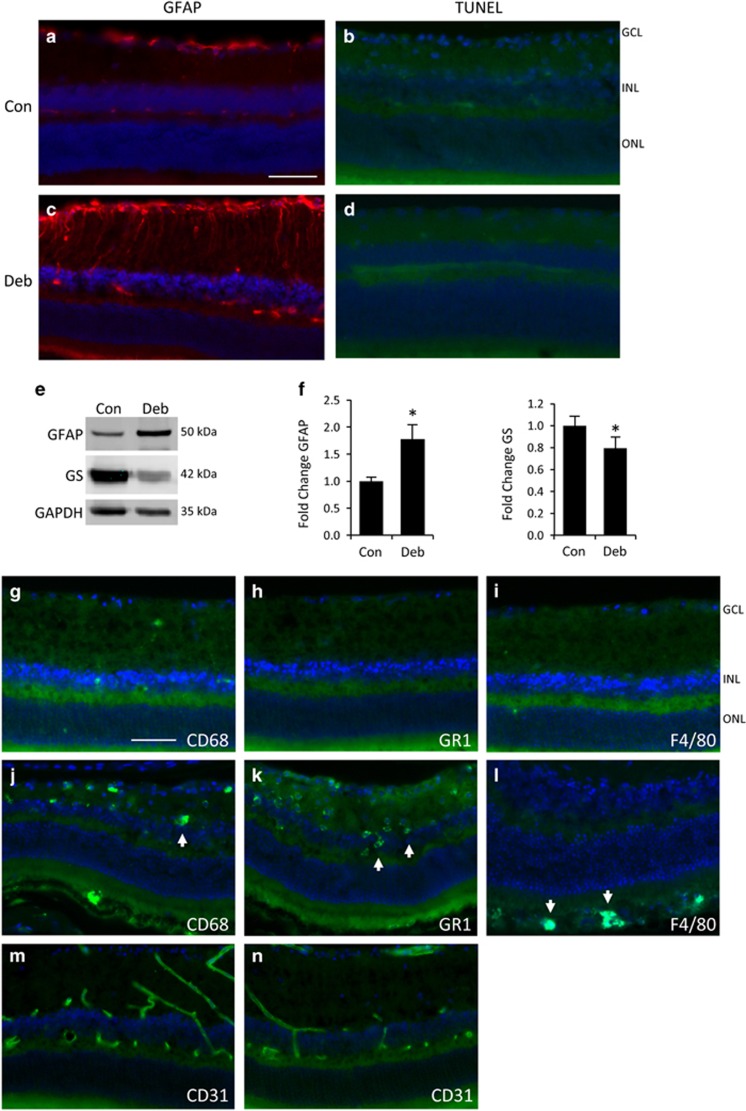
According to well-established methods the corneal epithelium was transiently removed by gentle mechanical debridement, according to our published procedure.48 The epithelium resurfaces within 1–2 days accompanied by transient corneal inflammation and neovascularization. Bargagna-Mohan et al. reported that by 7 days post injury a robust increase in GFAP is induced in astrocytes and Müller fibers.27, 47 Following the same procedure we also observed a strong increase in retinal GFAP staining compared with non-debrided controls (Figure 3a and c). Also consistent with the previous reports, there was no major change to retinal morphology or evidence of apoptosis (Figure 3b and d). As a second confirmation of increased gliosis, we performed western blotting for GFAP, and also for GS; a key glutamate recycling enzyme that is characteristically reduced in activated astrocytes.49, 50 Consistent with the immunofluorescence images, GFAP was significantly increased and GS significantly decreased in retinas isolated from debrided eyes, compared with non-debrided controls (Figure 3e and f).
Figure 3.
Rapid retinal glial reactivity is induced by corneal injury in the absence of cell death or inflammation. (a and b) Non-debrided control eyes show no evidence of gliosis or cell death. (c and d) Mechanical debridement of the corneal epithelium in the contralateral eye results in strongly increased GFAP staining in retinal astrocytes and Müller glia by 7 days (c), but no evidence of cell death or disrupted morphology (d). (e) Western blots from whole retina lysates show increased GFAP and decreased GS. (f) Densitometry and statistical analyses from multiple blots confirming the changes in e (bars represent SE, *P<0.05, n=3 animals). (g–i) Staining of debrided retinas for activated microglia, neutrophils and macrophages, was largely negative with CD68, GR-1 and F4/80 antibodies, respectively. (j–l) Corresponding antibody-positive controls from eyes treated with 150 mM NaOH. (m and n) There was no change in retinal blood vessel staining with the endothelial marker CD31 between control (m) or debrided eyes (n). (Scale bar indicates 50 μm, Con; control, Deb; debrided.)
To control for possible inflammatory effects we probed retinas from debrided eyes for CD68, GR-1 and F4/80, for evidence of activated microglia, neutrophils and macrophages, respectively (Figure 3g–i). Little or no staining was found, compared with positive controls (Figure 3j–l). We also stained retinas from debrided eyes for vascular changes with CD31 and observed no differences from non-debrided controls, as previously reported27 (Figure 3m and n). Therefore, we confirmed that this model does induce robust and consistent astrocyte and Müller glial reactivity in the inner retina with no evidence of accompanying damage or inflammatory response.
Activation of retinal astrocytes increases neuronal vulnerability in an IF and p38 MAPK-dependent manner
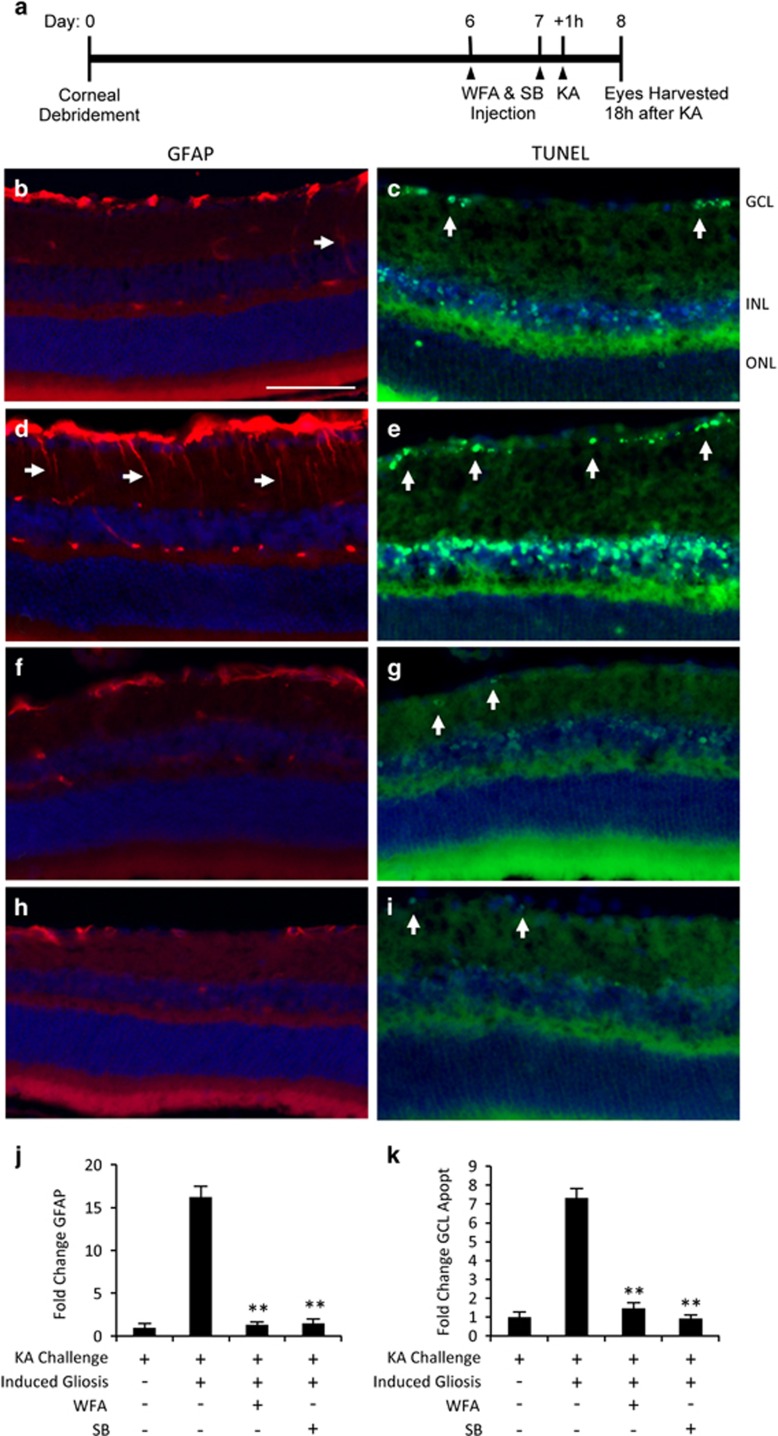
Our initial experiment treatment with WFA or SB potently blocked KA-induced astrocyte activation and neuronal apoptosis, but each inhibitor could also act through additional mechanisms to directly affect neurons. In particular, SB has been proposed to directly inhibit p38-dependent RGC apoptosis.51 Therefore, we designed a combined experiment in which KA challenge was combined with, or without, induced astrocyte activation in order to isolate the influence of the IF-mediated reactivity response.
In this combined design retinal astrogliosis was induced by debridement injury one week before KA challenge, along with each drug treatment or vehicle (Figure 4a). In naive, non-debrided eyes, KA treatment-induced moderate glial activation and GCL apoptosis as previously described (Figure 4b and c). In comparison, corneal debridement-induced massive reactivity in combination with KA challenge (Figure 4d). This combination also produced a marked increase in GCL apoptosis compared with KA alone (Figure 4e). Quantification of these results demonstrated a highly significant 16-fold increase in glial reactivity in debrided eyes compared with KA alone, and a 7-fold increase in apoptosis (Figure 4j and k). However, these increases were completely rescued by administration of either WFA or SB (Figure 4f–k). This experiment therefore provides evidence that induced glial reactivity increases the vulnerability of retinal neurons to excitotoxic injury, and that WFA and SB mediate their protective effects through blocking this switch.
Figure 4.
Induced glial reactivity promotes inner retinal apoptosis and is rescued by IF and p38 MAPK inhibition. (a) Schematic for induction of retinal gliosis by corneal debridement, followed by drug or vehicle treatments and KA challenge. (b and c) KA challenge induced rapid gliosis and GCL death as previously. (d and e) Prior corneal debridement-induced increased GFAP accumulation and increased GCL apoptosis following KA insult (arrows). Treatment with WFA (f and g) or SB (h and i) rescued the debridement-induced gliosis and cell death. (j and k) Quantification of the results showing that gliosis induced GCL death in WFA and SB-treated animals is significantly reduced (bars are S.E., **P<0.01, n⩾6 animals). Scale bar indicates 50 μm
WFA inhibits p38 MAPK-dependent TNF-α secretion
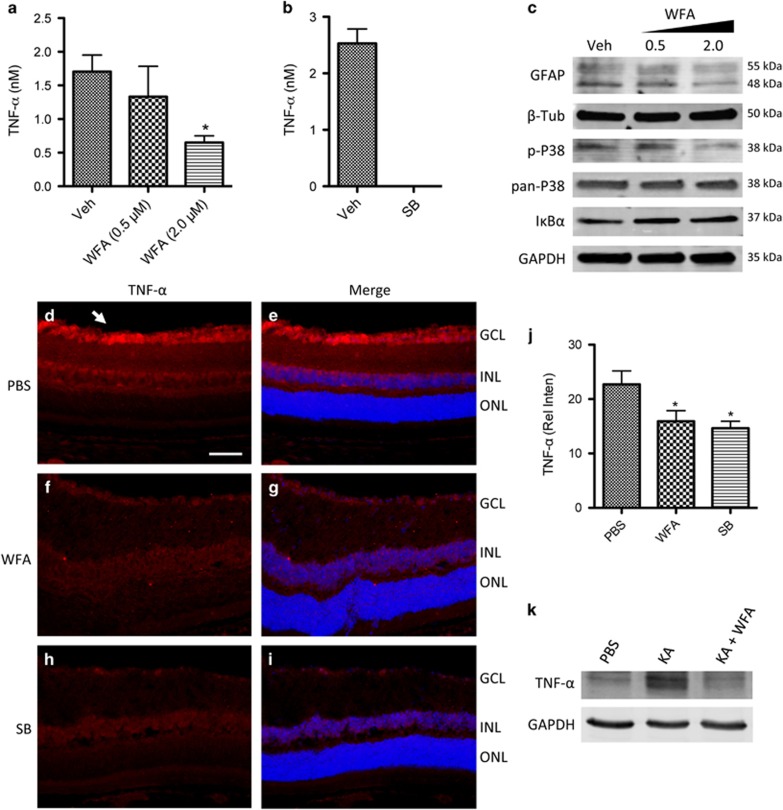
Neuronal apoptosis in the inner retina following disease and excitotoxic injury has been previously shown to be dependent on cytokine signals secreted by adjacent astrocytes.33, 34, 50, 52 Therefore we investigated WFA- and SB-regulated cytokines that might explain the IF-dependent effects in our models. Starting with cultured astrocytes, conditioned media was collected from treated cells and subjected to multiplex cytokine analyses. In this case the cells were stressed by serum deprivation to facilitate collection and analyses of conditioned media. Surprisingly, out of a panel of 27 cytokines and growth factors assessed, only TNF-α levels were significantly altered by WFA, although, negative trends were also identified for IL-1α and β, and EGF, and a positive trend for IL-10 (Table 1). TNF-α concentrations were strongly reduced by WFA treatment, in a dose-dependent manner to 2 μM (Figure 5a). To test whether this TNF-α signal was also dependent on downstream p38 MAPK signaling, cells were alternatively treated with SB, which we have previously reported to effectively block reactivity markers.29 SB treatment reduced TNF-α levels to below detection (Figure 5b). Western blotting demonstrated that increasing concentrations of WFA reduced GFAP in cultured retinal astrocytes, but not the intermediate filament β-tubulin (β-tub) (Figure 5c). Furthermore, phospho-p38 MAPK signal (p-p38) was reduced compared with total p38 (Figure 5c), consistent with previous reports.25, 26 In comparison, levels of IκBα were unaffected up to 2 μM (Figure 5c). Therefore, the WFA-induced effect on TNF-α may be mediated through p38 MAPK in retinal astrocytes.
Table 1. Media cytokines after WFA treatment.
| Analyte |
Normalized concentrations |
|
|---|---|---|
| Vehicle | 2 μM WFA | |
| TNF-αa | 1.00 | 0.38 |
| IL-1α | 1.00 | 0.50 |
| EGF | 1.00 | 0.55 |
| IL-1β | 1.00 | 0.62 |
| LIX | 1.00 | 0.90 |
| IL-6 | 1.00 | 0.91 |
| RANTES | 1.00 | 0.95 |
| MIP-2 | 1.00 | 0.98 |
| VEGF | 1.00 | 1.01 |
| IP-10 | 1.00 | 1.08 |
| Leptin | 1.00 | 1.16 |
| IL-13 | 1.00 | 1.18 |
| GRO/KC | 1.00 | 1.20 |
| IL-2 | 1.00 | 1.21 |
| IL-12(p70) | 1.00 | 1.22 |
| IL-5 | 1.00 | 1.28 |
| MCP-1 | 1.00 | 1.29 |
| Fractalkine | 1.00 | 1.45 |
| IL-4 | 1.00 | 1.52 |
| IFNy | 1.00 | 1.59 |
| IL-18 | 1.00 | 1.70 |
| MIP-1α | 1.00 | 1.74 |
| GM-CSF | 1.00 | 1.86 |
| Eotaxin | 1.00 | 2.24 |
| IL-17A | 1.00 | 2.39 |
| IL-10 | 1.00 | 4.36 |
| G-CSF | — | — |
Abbreviation: WFA, withaferin A.
P<0.05, n=3 isolates from eight animals each
Figure 5.
WFA treatment inhibits p38 MAPK-dependent TNF-α secretion in the inner retina. (a) Conditioned media from astrocytes treated with WFA showed a dose-dependent decrease in TNF-α concentrations (*P<0.05, n=3 cultures). (b) Conditioned media from astrocytes treated with 15 μm SB showed a complete loss of detectable TNF-α (n=3 cultures). (c) Western blot showing increasing concentrations of WFA resulted in reduced GFAP protein and phospho-p38 MAPK (p-p38), compared with pan-p38 MAPK. In comparison there was no change in β-tub, IκBα, or a GAPDH loading control. (d and e) Staining for TNF-α (red) appears strongly in the inner retina in KA challenged eyes (arrow). (f and g) Treatment with WFA, or (h and i) SB, reduced TNF-α staining. Cell nuclei are indicated by Dapi staining in all images (blue). (j) Quantification of TNF-α intensity across the GCL confirms a reduced signal in WFA- or SB-treated eyes following KA challenge (*P<0.05, n=3 animals per group). Scale bar represents 50 μm. (k) Western blot of retinal lysates similarly shows increased TNF-α signal following KA challenge that is blocked by WFA treatment, compared with GAPDH loading control (n=4 animals per lane)
Glial derived TNF-α has been closely linked to the induction of neuronal apoptosis in a variety of acute and degenerative models, including following excitotoxic injury,33, 53, 54, 55 and during progression of glaucoma.34, 56, 57 To confirm the effects of WFA on secretion of TNF-α, we probed retinal sections from KA challenged and control eyes with antibodies to TNF-α to observe the effect of IF inhibition in vivo.
In KA challenged eyes TNF-α staining was prominently localized in the inner retina, matching the observed pattern of apoptosis in the GCL and INL, but was not present in the outer retinal layers (Figure 5d and e; Supplementary Figure 2). Correspondingly, TNF receptor 1 (TNFR1) staining primarily localized to GCL neurons (Supplementary Figure 2), consistent with previous reports.33, 34 In comparison, sections from KA challenged eyes treated with WFA or SB showed strongly reduced TNF-α signal (Figure 5f–i). This TNF-α signal was quantified by measuring the average staining intensity across the GCL from multiple sections per animal, for multiple animals in each treatment group. Results indicated a significant reduction of TNF-α in WFA- and SB-treated animals compared with control (Figure 5j). Reduced TNF-α signal in retinal lysates was further confirmed by western blot (Figure 5k). Thus, treatment with WFA or SB reduced TNF-α signal in the inner retina following injury in vivo.
Discussion
Astrocyte reactivity is associated with many neurodegenerative and neurotoxic processes, including Alzheimer's disease, Parkinson's disease, stroke, diabetic retinopathy and glaucoma.3, 32, 58, 59, 60 This parainflammatory switch contributes to progression of non-cell autonomous disease mechanisms.4, 61 However, the pathogenic cascades underlying reactivity have proven difficult to study in vivo due to a lack of pharmacologic tools to modulate this process. Genetic deletion of vimentin or GFAP results in compensatory changes in remaining IF's. Although double knockouts of GFAP and vimentin promote axonal outgrowth and regeneration in developing neurons and after CNS injury,10, 11, 12 and use of glial toxins is similarly protective.42 Yet, these deletions also result in developmental and pathologic defects in CNS patterning and function that can alter baseline tissue homeostasis.13, 14, 15 In order to fully test the role of IF dynamics during glial reactivity and disease, pharmacological tools are necessary to block increased activity on a normal background. Here we have presented data demonstrating that pharmacologic inhibition of glial IF dynamics blocks p38 MAPK-dependent secretion of TNF-α, and dramatically reduces apoptosis in a non-cell autonomous model of excitotoxic neuronal death.
WFA is the cardinal member of a family of bioactive steroidal lactones termed ‘withanolides', derived from the Withania somnifera plant.62 It is a potent inhibitor of vimentin polymerization, and has been primarily investigated for anti-angiogenic, cytostatic, and anti-inflammatory effects, particularly through modulation of NFκB and MAPK signaling. Recent studies have clarified the mechanism of WFA to specifically target type III intermediate filaments, including vimentin and GFAP.16, 27 Additionally, multiple labs have demonstrated that its downstream kinase and transcriptional effects, as well cytostatic effect at high concentration, are dependent on IF blocking activity.16, 20, 25, 27, 63, 64 Therefore, WFA provides a potent tool for probing the efficacy of IF disruption in the context of neuronal injury. Interestingly, Swarup et al.65 reported improved CNS outcomes following WFA administration in a model of amyotrophic lateral sclerosis, but did not explore these results in the context of IF inhibition.
In our experiments pharmacologic blockade of IF dynamics in reactive glia with WFA-protected retinal neurons from excitotoxic metabolic stress. In the inner retina astrocyte processes and Müller glia endfeet interact closely with RGC bodies and axons to regulate inner retinal homeostasis.8, 31, 58 Reactive gliosis is rapidly induced following insult to the inner retina,7, 66 and is associated with cytokine secretion, remodeling of the optic nerve head, loss of glutamate buffering and increased production of detoxifying enzymes.8, 58, 67, 68, 69 Our results suggest that the anti-apoptotic activity of WFA is mediated by inhibiting a p38 MAPK-dependent production of TNF-α by reactive astrocytes and Müller glia. Inhibition of IFs or p38 MAPK-reduced glial reactivity, and inhibited neuronal cell death. In contrast, a new model of induced glial reactivity markedly increased susceptibility to excitotoxic death. WFA or SB might act through additional mechanisms to directly affect neurons, as previously reported for SB.51 Therefore, we performed a combined experiment of KA challenge with induced glial activation to demonstrate a rescue of the reactivity-mediated injury by treatment with WFA or SB.
To explain these results we show that IF inhibition blocked p38 MAPK phosphorylation, and p38-dependent secretion of TNF-α. In comparison, IκBα levels were unchanged, suggesting that NFκB signaling was not strongly affected. Increased p38 phosphorylation and signaling has been closely associated with astrocyte and microglia reactivity in the context of oxidative and metabolic stress through regulation of antioxidant defense, mitochondrial function and cytokine secretion, particularly TNF-α.29, 70, 71 In addition, gain of function accumulations of mutant GFAP protein causes Alexander's disease via a p38 MAPK-dependent pathology.15 Accordingly, inhibition of p38 signaling is protective in models of metabolic and oxidative neuronal injury.51, 72, 73
A cytokine screen identified that WFA significantly reduced TNF-α release, although a trend for negative regulation was also identified for IL-1α and β, and EGF, and a positive trend for IL-10. IL-10 has been reported to play a role in astrocyte mediated neuroprotection, through direct and indirect mechanisms.74, 75, 76, 77 Therefore, these additional factors may also contribute to the observed efficacy. TNF-α is a key proinflammatory cytokine that binds to two major death receptors (TNFR1 and TNFR2) to induce the extrinsic apoptosis cascade.55 Non-cell autonomous neuronal cell death due to glial derived TNF-α signaling has been implicated in a diverse range of neurodegenerative and neurotoxic conditions,55 including excitotoxicity.33, 53 In the eye, TNF-α secretion by reactive astrocytes and Müller glia has been well established to induce RGC apoptosis in experimental models,52, 54 and during degenerative disease.34, 56 Subsequently, pharmacologic inhibition or genetic deletion of TNF-α signaling is protective to RGCs.33, 54 The present results suggest that type III IF dynamics initiate a p38—TNF-α signaling cascade in reactive glia that exacerbates inner retinal injury. In addition, the inhibition of p38 MAPK conversely decreased IF accumulation. As both p38 and TNF-α have roles in the induction of astrocyte reactivity,29, 71, 78 it seems likely that an autocrine loop is at play that may include additional mediators, such as IL-10. Future experiments will be required to fully elucidate this signaling cascade.
Excitotoxic damage due to elevated glutamate has been associated with many acute and chronic neurodegenerative diseases of the retina and brain, including stroke, Alzheimer's disease and glaucoma.31, 32, 79 The inner retina is particularly vulnerable to excitotoxic and metabolic stress, which is exacerbated through the release of TNF-α by neighboring astrocytes and Müller glia.28, 33 However, the astrocyte reactivity cascade is a complex process that has both positive and negative aspects. For example, ischemic preconditioning has been reported to have protective effects that are partially attributed to activated glia.80, 81, 82 The mechanism underlying this protection remains unclear, and is likely influenced by signaling through additional metabolic response pathways that may differ from the p38 driven mechanism we have described here. A key goal for the present work is the targeted inhibition of IFs, rather than complete ablation of the reactive cascade. Here we have demonstrated that pharmacologic targeting of IF dynamics modulates cytokine release and dramatically reduces neuronal cell death following acute retinal injury. It will be important for future studies to expand these findings by using WFA as a probe to further investigate the roles and mechanisms of glial IF dynamics in other neurotoxic and neurodegenerative processes.
Materials and Methods
Retinal injury model
All animal experiments were approved by the UHN Animal Care Committee in accordance with applicable regulations. Male C57BL/6 mice were anesthetized by i.p. injection of ketamine/xylazine. Intravitreal injections with 10 mM kainic acid (KA) were performed as previously described.28 Briefly, a 30 g needle was inserted tangentially into the vitreous and replaced with a Hamilton syringe to inject a volume of 2 μl, followed by application of ophthalmic antibiotic ointment (BNP, Vetoquinol). For drug experiments, mice received two injections of either vehicle, 2 mg/kg WFA i.p., or 2 mM SB203580 (Selleckchem, Burlington, ON, Canada) intravitreally, the day before, and 1 h before KA challenge. Eighteen hours after KA challenge mice were euthanized by CO2 asphyxiation and eyes processed for histopathology. In all experiments n refers to the number of animals tested.
Induced glial reactivity model
Corneal epithelial debridement was performed to induce retinal glial reactivity as previously described.27, 48 Briefly, anesthetized mice received topical proparacaine to the eyes (Bausch and Lomb, Vaughan, ON, Canada). Eyes were proptosed with forceps, and the corneal epithelium was gently removed with a sterile disposable scalpel, followed by application of antibiotic ointment. For some experiments, at 6 and 7 days post debridement, mice received injection of either vehicle, 2 mg/kg WFA i.p., or 2 mM SB203580 intravitreally, followed by KA challenge, as described above. The retinas were processed on day eight as described above. In all experiments n refers to the number of animals tested.
Astrocyte cultures
Primary mature retinal astrocytes were isolated and cultured as previously described.30 Briefly, retinas were dissected out of adult Wistar rat eyes and placed in ice-cold MEM-H17 culture medium. Retinas were digested by shaking in MEM-H17 containing trypsin and DNAse, followed by trituration to disperse cell aggregates. When cultures reached confluence, the cells were placed on a rotating shaker for 6–8 h and re-plated. A glial-specific expression profile was confirmed by probing the resulting cells with a marker panel. For staining and biochemistry experiments media was replaced with serum-free media and cultured for an additional 8 h with treatment of 0.5 or 2.0 μM WFA, 15 μM SB or the equivalent DMSO vehicle as a control. Conditioned media was collected after 8 h and immediately frozen for multiplex cytokine analyses.
Western blotting and cytokine profiling
Cells were lysed in RIPA buffer containing Complete Mini EDTA-free protease inhibitor (Roche) and PhosSTOP phosphatase inhibitor (Roche, Mississauga, ON, Canada). Total protein was quantified and equal concentrations were submitted to SDS-PAGE by standard methods. Proteins were transferred to PVDF membrane and probed with antibodies raised against GFAP (Sigma, St. Louis, MO, USA), GS (Abcam, Cambridge, MA, USA), phospho-p38 and pan-p38 MAPK (Cell Signaling, Danvers, MA, USA), IκBα (Santa Cruz, Dallas, TX, USA), TNF-α (R&D Systems, Minneapolis, MN, USA), and GAPDH (Calbiochem, San Diego, CA, USA), and detected with appropriate IRDye secondary antibody (Li-Cor Biosciences, Lincoln, NE, USA). Blots were imaged with an Odyssey infrared imaging system (Li-Cor Biosciences). For TNF-α and multiplex cytokine profiling, conditioned media was snap frozen and submitted for laser bead analyses on a Bioplex 200 to detect sensitive and quantitative target protein concentrations against a standard curve (Eve Technologies).
Immunofluorescence microscopy
Enucleated eyes were fixed in 4% PFA overnight. Eyes were then equilibrated in 30% sucrose for 12 h, embedded in OCT, and cryosectioned at 16 μM. Sections were blocked and probed with primary antibodies to GFAP (Sigma), GS (Sigma), CD68 (Biolegend, San Diego, CA, USA), GR-1 (Biolegend), F4/80 (Biolegend), TNF-α (R&D Systems), RBPMS (Phosphosolutions, Aurora, CO, USA), and CD31 (BD Biosciences, Mississuaga, ON, Canada) according to standard protocols. Following PBS-t washes, sections were incubated with fluorescent-conjugated 2° abs (Molecular Probes, Eugene, OR, USA) and mounted with DAPI. TUNEL staining was performed according to the manufacturer's instructions (DeadEnd; Promega, Fitchburg, WI, USA). Briefly, sections were fixed with 4% PFA for 5 min and washed in PBS. Equilibration buffer was added, and rTdT reaction mix was applied to each slide and incubated at 37 °C for 60 min. Slides were immersed in 2 × SSC and then washed with PBS, followed by blocking with 5% goat serum and incubation with 1° abs at 4 °C. Images were acquired with a Zeiss AxioImager fluorescence microscope. For in vitro staining, cells were washed, fixed in 4% PFA for 15 min, rinsed and permeabilized in 0.2% Triton X-100 for 15 min, and blocked with 5% BSA for 1 h. Cells were probed with 1° abs to: GFAP (Abcam), Vimentin (Sigma), or rhodamine phalloidin (Life Technologies, Burlington, ON, Canada), O/N at 4 °C, followed by washing and the appropriate Alexa Fluor 2° abs antibodies (Life Technologies) for 1 h. Cells were mounted with Vecta-Shield anti-fade medium with DAPI (Vector Labs, Burlingame, CA, USA), and imaged on an inverted Nikon TIE-E fluorescent microscope.
Image analyses
To quantifying glial reactivity, retinal sections were imaged at the level of the optic nerve. The proportion of increased GFAP immunostaining in Müller cell processes was used as an established approach to quantify retinal glial reactivity.43 Briefly, for each animal GFAP-immunopositive processes were counted in the inner plexiform layer for at least five retinal sections at the level of the optic nerve. GFAP-positive processes were counted for each eye and expressed as the average number of positive processes per 100 μm.60 To quantify the extent of apoptosis, we counted the number of TUNEL-positive nuclei in the GCL and expressed it as a fraction of the total GCL nuclei. In treated eyes the TUNEL signal was more difficult to find, so we conservatively counted any suspected labeling in our analyses. For each eye, at least five central retinal sections were analyzed at the level of the optic nerve stretching to each ora serrata, and the results averaged, as previously described.28, 44, 45, 46, 83 For TNF-α staining the mean intensity of antibody signal was measured in the GCL and normalized to the slide background for each section. Intensity readings were averaged for at least three sections at the level of the optic nerve for each eye, and then averaged across each treatment group as indicated. For all experiments eyes from at least three animals were assessed with specific numbers described in each figure legend. Statistical analyses were performed by one-way ANOVA with TUKEY post hoc analyses.
Acknowledgments
Funding was provided by the Canadian Institutes for Health Research (CIHR), the Glaucoma Research Society of Canada (GRSC), and the National Science and Engineering Research Council (NSERC). J Sivak is the Toronto General and Western Hospital Foundation Glaucoma Research Chair. I Livne-Bar was supported by the David and Sandra Smith Postdoctoral Fellowship. This work was supported by CIHR, NSERC, and the Glaucoma Research Society of Canada.
Glossary
- GCL
ganglion cell layer
- GFAP
glial fibrillary acidic protein
- GS
glutamine synthetase
- IF
intermediate filament
- INL
inner nuclear layer
- KA
kainic acid
- MAPK
mitogen-activated protein kinase
- SB
SB203580
- RGC
retinal ganglion cell
- WFA
withaferin A
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Cell Death and Disease website (http://www.nature.com/cddis)
Edited by A Yaron
Supplementary Material
References
- Attwell D, Buchan AM, Charpak S, Lauritzen M, Macvicar BA, Newman EA. Glial and neuronal control of brain blood flow. Nature 2010; 468: 232–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreto GE, Gonzalez J, Torres Y, Morales L. Astrocytic-neuronal crosstalk: implications for neuroprotection from brain injury. Neurosci Res 2011; 71: 107–113. [DOI] [PubMed] [Google Scholar]
- Barres BA. The mystery and magic of glia: a perspective on their roles in health and disease. Neuron 2008; 60: 430–440. [DOI] [PubMed] [Google Scholar]
- Garden GA, La Spada AR. Intercellular (mis)communication in neurodegenerative disease. Neuron 2012; 73: 886–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekny M, Nilsson M. Astrocyte activation and reactive gliosis. Glia 2005; 50: 427–434. [DOI] [PubMed] [Google Scholar]
- Bahr M, Przyrembel C, Bastmeyer M. Astrocytes from adult rat optic nerves are nonpermissive for regenerating retinal ganglion cell axons. Exp Neurol 1995; 131: 211–220. [DOI] [PubMed] [Google Scholar]
- Johnson EC, Morrison JC. Friend or foe? Resolving the impact of glial responses in glaucoma. J Glaucoma 2009; 18: 341–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tezel G. The role of glia, mitochondria, and the immune system in glaucoma. Invest Ophthalmol Vis Sci 2009; 50: 1001–1012. [DOI] [PubMed] [Google Scholar]
- Ullian EM, Sapperstein SK, Christopherson KS, Barres BA. Control of synapse number by glia. Science 2001; 291: 657–661. [DOI] [PubMed] [Google Scholar]
- Menet V, Gimenez y Ribotta M, Chauvet N, Drian MJ, Lannoy J, Colucci-Guyon E et al. Inactivation of the glial fibrillary acidic protein gene, but not that of vimentin, improves neuronal survival and neurite growth by modifying adhesion molecule expression. J Neurosci 2001; 21: 6147–6158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelmsson U, Li L, Pekna M, Berthold CH, Blom S, Eliasson C et al. Absence of glial fibrillary acidic protein and vimentin prevents hypertrophy of astrocytic processes and improves post-traumatic regeneration. J Neurosci 2004; 24: 5016–5021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menet V, Gimenez YRM, Sandillon F, Privat A. GFAP null astrocytes are a favorable substrate for neuronal survival and neurite growth. Glia 2000; 31: 267–272. [DOI] [PubMed] [Google Scholar]
- Wunderlich KA, Tanimoto N, Grosche A, Zrenner E, Pekny M, Reichenbach A et al. Retinal functional alterations in mice lacking intermediate filament proteins glial fibrillary acidic protein and vimentin. FASEB J 2015; 29: 4815–4828. [DOI] [PubMed] [Google Scholar]
- Kraft AW, Hu X, Yoon H, Yan P, Xiao Q, Wang Y et al. Attenuating astrocyte activation accelerates plaque pathogenesis in APP/PS1 mice. FASEB J 2013; 27: 187–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang G, Yue Z, Talloczy Z, Hagemann T, Cho W, Messing A et al. Autophagy induced by Alexander disease-mutant GFAP accumulation is regulated by p38/MAPK and mTOR signaling pathways. Hum Mol Genet 2008; 17: 1540–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grin B, Mahammad S, Wedig T, Cleland MM, Tsai L, Herrmann H et al. Withaferin a alters intermediate filament organization, cell shape and behavior. PLoS One 2012; 7: e39065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trendowski M. Exploiting the cytoskeletal filaments of neoplastic cells to potentiate a novel therapeutic approach. Biochim Biophys Acta 2014; 1846: 599–616. [DOI] [PubMed] [Google Scholar]
- Lavie D, Glotter E, Shvo Y. Constituents of Withania somnifera Dun. III. The side hain of Withaferin A. J Org Chem 1965; 30: 1774–1778. [Google Scholar]
- Liu T, Ghamloush MM, Aldawood A, Warburton R, Toksoz D, Hill NS et al. Modulating endothelial barrier function by targeting vimentin phosphorylation. J Cell Physiol 2014; 229: 1484–1493. [DOI] [PubMed] [Google Scholar]
- Stevens C, Henderson P, Nimmo ER, Soares DC, Dogan B, Simpson KW et al. The intermediate filament protein, vimentin, is a regulator of NOD2 activity. Gut 2013; 62: 695–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bargagna-Mohan P, Paranthan RR, Hamza A, Zhan CG, Lee DM, Kim KB et al. Corneal antifibrotic switch identified in genetic and pharmacological deficiency of vimentin. J Biol Chem 2012; 287: 989–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menko AS, Bleaken BM, Libowitz AA, Zhang L, Stepp MA, Walker JL. A central role for vimentin in regulating repair function during healing of the lens epithelium. Mol Biol Cell 2014; 25: 776–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohan R, Hammers HJ, Bargagna-Mohan P, Zhan XH, Herbstritt CJ, Ruiz A et al. Withaferin A is a potent inhibitor of angiogenesis. Angiogenesis 2004; 7: 115–122. [DOI] [PubMed] [Google Scholar]
- Hahm ER, Singh SV. Withaferin A-induced apoptosis in human breast cancer cells is associated with suppression of inhibitor of apoptosis family protein expression. Cancer Lett 2013; 334: 101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bargagna-Mohan P, Lei L, Thompson A, Shaw C, Kasahara K, Inagaki M et al. Vimentin phosphorylation underlies myofibroblast sensitivity to withaferin A in vitro and during corneal fibrosis. PLoS One 2015; 10: e0133399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min KJ, Choi K, Kwon TK. Withaferin A down-regulates lipopolysaccharide-induced cyclooxygenase-2 expression and PGE2 production through the inhibition of STAT1/3 activation in microglial cells. Int Immunopharmacol 2011; 11: 1137–1142. [DOI] [PubMed] [Google Scholar]
- Bargagna-Mohan P, Paranthan RR, Hamza A, Dimova N, Trucchi B, Srinivasan C et al. Withaferin A targets intermediate filaments glial fibrillary acidic protein and vimentin in a model of retinal gliosis. J Biol Chem 2010; 285: 7657–7669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X, Dason ES, Zanon-Moreno V, Jiang Q, Nahirnyj A, Chan D et al. PGC-1alpha signaling coordinates susceptibility to metabolic and oxidative injury in the inner retina. Am J Pathol 2014; 184: 1017–1029. [DOI] [PubMed] [Google Scholar]
- Nahirnyj A, Livne-Bar I, Guo X, Sivak JM. ROS detoxification and proinflammatory cytokines are Linked by p38 MAPK signaling in a model of mature astrocyte activation. PLoS One 2013; 8: e83049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RS, Dharsee M, Ackloo S, Sivak JM, Flanagan JG. Proteomics analyses of human optic nerve head astrocytes following biomechanical strain. Mol Cell Proteomics 2012; 11: M111 012302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almasieh M, Wilson AM, Morquette B, Cueva Vargas JL, Di Polo A. The molecular basis of retinal ganglion cell death in glaucoma. Prog Retin Eye Res 2012; 31: 152–181. [DOI] [PubMed] [Google Scholar]
- Sivak JM. The aging eye: common degenerative mechanisms between the Alzheimer's brain and retinal disease. Invest Ophthalmol Vis Sci 2013; 54: 871–880. [DOI] [PubMed] [Google Scholar]
- Lebrun-Julien F, Duplan L, Pernet V, Osswald I, Sapieha P, Bourgeois P et al. Excitotoxic death of retinal neurons in vivo occurs via a non-cell-autonomous mechanism. J Neurosci 2009; 29: 5536–5545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tezel G, Li LY, Patil RV, Wax MB. TNF-alpha and TNF-alpha receptor-1 in the retina of normal and glaucomatous eyes. Invest Ophthalmol Vis Sci 2001; 42: 1787–1794. [PubMed] [Google Scholar]
- Paintlia MK, Paintlia AS, Singh AK, Singh I. S-nitrosoglutathione induces ciliary neurotrophic factor expression in astrocytes that has implication to protect CNS under pathological conditions. J Biol Chem 2013; 16: 11507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin JH, Jeong JY, Jin Y, Kim ID, Lee JK. p38beta MAPK affords cytoprotection against oxidative stress-induced astrocyte apoptosis via induction of alphaB-crystallin and its anti-apoptotic function. Neurosci Lett 2011; 501: 132–137. [DOI] [PubMed] [Google Scholar]
- Soliman ML, Combs CK, Rosenberger TA. Modulation of inflammatory cytokines and mitogen-activated protein kinases by acetate in primary astrocytes. J Neuroimmune Pharmacol 2012; 8: 287–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mali RS, Cheng M, Chintala SK. Plasminogen activators promote excitotoxicity-induced retinal damage. FASEB J 2005; 19: 1280–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang ML, Wu CH, Jiang-Shieh YF, Shieh JY, Wen CY. Reactive changes of retinal astrocytes and Muller glial cells in kainate-induced neuroexcitotoxicity. J Anat 2007; 210: 54–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Ramos P, Reinoso-Suarez F. Kainic acid prevents peroxidase labeling of retinal ganglion cell bodies in the rat: a possible gate in retrograde axonal transport. Neurosci Lett 1983; 35: 1–6. [DOI] [PubMed] [Google Scholar]
- Wang Q, Yu S, Simonyi A, Sun GY, Sun AY. Kainic acid-mediated excitotoxicity as a model for neurodegeneration. Mol Neurobiol 2005; 31: 3–16. [DOI] [PubMed] [Google Scholar]
- Ganesh BS, Chintala SK. Inhibition of reactive gliosis attenuates excitotoxicity-mediated death of retinal ganglion cells. PLoS One 2011; 6: e18305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickerson PE, McLeod MC, Myers T, Clarke DB. Effects of epidermal growth factor and erythropoietin on Muller glial activation and phenotypic plasticity in the adult mammalian retina. J Neurosci Res 2011; 89: 1018–1030. [DOI] [PubMed] [Google Scholar]
- Chen L, Sham CW, Chan AM, Francisco LM, Wu Y, Mareninov S et al. Role of the immune modulator programmed cell death-1 during development and apoptosis of mouse retinal ganglion cells. Invest Ophthalmol Vis Sci 2009; 50: 4941–4948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada C, Namekata K, Guo X, Yoshida H, Mitamura Y, Matsumoto Y et al. ASK1 deficiency attenuates neural cell death in GLAST-deficient mice, a model of normal tension glaucoma. Cell Death Differ 2010; 17: 1751–1759. [DOI] [PubMed] [Google Scholar]
- Riesenberg AN, Liu Z, Kopan R, Brown NL. Rbpj cell autonomous regulation of retinal ganglion cell and cone photoreceptor fates in the mouse retina. J Neurosci 2009; 29: 12865–12877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paranthan RR, Bargagna-Mohan P, Lau DL, Mohan R. A robust model for simultaneously inducing corneal neovascularization and retinal gliosis in the mouse eye. Mol Vis 2011; 17: 1901–1908. [PMC free article] [PubMed] [Google Scholar]
- Sivak JM, Ostriker AC, Woolfenden A, Demirs J, Cepeda R, Long D et al. Pharmacologic uncoupling of angiogenesis and inflammation during initiation of pathological corneal neovascularization. J Biol Chem 2011; 286: 44965–44975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krajnc D, Neff NH, Hadjiconstantinou M. Glutamate, glutamine and glutamine synthetase in the neonatal rat brain following hypoxia. Brain Res 1996; 707: 134–137. [DOI] [PubMed] [Google Scholar]
- Reinhardt CA, Schein CH. Glutamine synthetase activity as a marker of toxicity in cultures of embryonic chick brain and retina cells. Toxicol In Vitro 1995; 9: 369–374. [DOI] [PubMed] [Google Scholar]
- Kikuchi M, Tenneti L, Lipton SA. Role of p38 mitogen-activated protein kinase in axotomy-induced apoptosis of rat retinal ganglion cells. J Neurosci 2000; 20: 5037–5044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tezel G, Wax MB. Increased production of tumor necrosis factor-alpha by glial cells exposed to simulated ischemia or elevated hydrostatic pressure induces apoptosis in cocultured retinal ganglion cells. J Neurosci 2000; 20: 8693–8700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bock F, Dornand J, Rondouin G. Release of TNF alpha in the rat hippocampus following epileptic seizures and excitotoxic neuronal damage. Neuroreport 1996; 7: 1125–1129. [DOI] [PubMed] [Google Scholar]
- Lebrun-Julien F, Bertrand MJ, De Backer O, Stellwagen D, Morales CR, Di Polo A et al. ProNGF induces TNFalpha-dependent death of retinal ganglion cells through a p75NTR non-cell-autonomous signaling pathway. Proc Natl Acad Sci USA 2010; 107: 3817–3822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sriram K, O'Callaghan JP. Divergent roles for tumor necrosis factor-alpha in the brain. J Neuroimmune Pharmacol 2007; 2: 140–153. [DOI] [PubMed] [Google Scholar]
- Yuan L, Neufeld AH. Tumor necrosis factor-alpha: a potentially neurodestructive cytokine produced by glia in the human glaucomatous optic nerve head. Glia 2000; 32: 42–50. [PubMed] [Google Scholar]
- Bai Y, Shi Z, Zhuo Y, Liu J, Malakhov A, Ko E et al. In glaucoma the upregulated truncated TrkC.T1 receptor isoform in glia causes increased TNF-alpha production, leading to retinal ganglion cell death. Invest Ophthalmol Vis Sci 2010; 51: 6639–6651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez MR, Miao H, Lukas T. Astrocytes in glaucomatous optic neuropathy. Prog Brain Res 2008; 173: 353–373. [DOI] [PubMed] [Google Scholar]
- Parpura V, Heneka MT, Montana V, Oliet SH, Schousboe A, Haydon PG et al. Glial cells in (patho)physiology. J Neurochem 2012; 121: 4–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis TM, Hamilton R, Yong PH, McVicar CM, Berner A, Pringle R et al. Muller glial dysfunction during diabetic retinopathy in rats is linked to accumulation of advanced glycation end-products and advanced lipoxidation end-products. Diabetologia 2011; 54: 690–698. [DOI] [PubMed] [Google Scholar]
- Ilieva H, Polymenidou M, Cleveland DW. Non-cell autonomous toxicity in neurodegenerative disorders: ALS and beyond. J Cell Biol 2009; 187: 761–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanden Berghe W, Sabbe L, Kaileh M, Haegeman G, Heyninck K. Molecular insight in the multifunctional activities of Withaferin A. Biochem Pharmacol 2012; 84: 1282–1291. [DOI] [PubMed] [Google Scholar]
- Bargagna-Mohan P, Hamza A, Kim YE, Khuan Abby Ho Y, Mor-Vaknin N, Wendschlag N et al. The tumor inhibitor and antiangiogenic agent withaferin A targets the intermediate filament protein vimentin. Chem Biol 2007; 14: 623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahat G, Zhu QS, Huang KL, Wang S, Bolshakov S, Liu J et al. Vimentin is a novel anti-cancer therapeutic target; insights from in vitro and in vivo mice xenograft studies. PLoS One 2010; 5: e10105. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Swarup V, Phaneuf D, Dupre N, Petri S, Strong M, Kriz J et al. Deregulation of TDP-43 in amyotrophic lateral sclerosis triggers nuclear factor kappaB-mediated pathogenic pathways. J Exp Med 2011; 208: 2429–2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann A, Pannicke T, Grosche J, Francke M, Wiedemann P, Skatchkov SN et al. Muller cells in the healthy and diseased retina. Prog Retin Eye Res 2006; 25: 397–424. [DOI] [PubMed] [Google Scholar]
- Tezel G. Oxidative stress in glaucomatous neurodegeneration: mechanisms and consequences. Prog Retin Eye Res 2006; 25: 490–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tezel G, Wax MB. Hypoxia-inducible factor 1alpha in the glaucomatous retina and optic nerve head. Arch Ophthalmol 2004; 122: 1348–1356. [DOI] [PubMed] [Google Scholar]
- Liu B, Neufeld AH. Activation of epidermal growth factor receptors in astrocytes: from development to neural injury. J Neurosci Res 2007; 85: 3523–3529. [DOI] [PubMed] [Google Scholar]
- Bachstetter AD, Van Eldik LJ. The p38 MAP kinase family as regulators of proinflammatory cytokine production in degenerative diseases of the CNS. Aging Dis 2010; 1: 199–211. [PMC free article] [PubMed] [Google Scholar]
- Shrestha R, Millington O, Brewer J, Dev KK, Bushell TJ. Lymphocyte-mediated neuroprotection in in vitro models of excitotoxicity involves astrocytic activation and the inhibition of MAP kinase signalling pathways. Neuropharmacology 2014; 76: 184–193. [DOI] [PubMed] [Google Scholar]
- Irving EA, Bamford M. Role of mitogen- and stress-activated kinases in ischemic injury. J Cereb Blood Flow Metab 2002; 22: 631–647. [DOI] [PubMed] [Google Scholar]
- Rivera-Cervantes MC, Castaneda-Arellano R, Castro-Torres RD, Gudino-Cabrera G, Feria y Velasco AI, Camins A et al. P38 MAPK inhibition protects against glutamate neurotoxicity and modifies NMDA and AMPA receptor subunit expression. J Mol Neurosci 2015; 55: 596–608. [DOI] [PubMed] [Google Scholar]
- Bachis A, Colangelo AM, Vicini S, Doe PP, De Bernardi MA, Brooker G et al. Interleukin-10 prevents glutamate-mediated cerebellar granule cell death by blocking caspase-3-like activity. J Neurosci 2001; 21: 3104–3112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasingam V, Yong VW. Attenuation of astroglial reactivity by interleukin-10. J Neurosci 1996; 16: 2945–2955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwilasz AJ, Grace PM, Serbedzija P, Maier SF, Watkins LR. The therapeutic potential of interleukin-10 in neuroimmune diseases. Neuropharmacology 2015; 96: 55–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S, Yang B, Xi X, Grotta JC, Aronowski J, Savitz SI. IL-10 directly protects cortical neurons by activating PI-3 kinase and STAT-3 pathways. Brain Res 2011; 1373: 189–194. [DOI] [PubMed] [Google Scholar]
- Balasingam V, Tejada-Berges T, Wright E, Bouckova R, Yong VW. Reactive astrogliosis in the neonatal mouse brain and its modulation by cytokines. J Neurosci 1994; 14: 846–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalia LV, Kalia SK, Salter MW. NMDA receptors in clinical neurology: excitatory times ahead. Lancet Neurol 2008; 7: 742–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreixler JC, Poston JN, Shaikh AR, Alexander M, Tupper KY, Marcet MM et al. Delayed post-ischemic conditioning significantly improves the outcome after retinal ischemia. Exp Eye Res 2011; 92: 521–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Sha O, Cho EY. Remote ischemic postconditioning promotes the survival of retinal ganglion cells after optic nerve injury. J Mol Neurosci 2013; 51: 639–646. [DOI] [PubMed] [Google Scholar]
- Lorber B, Guidi A, Fawcett JW, Martin KR. Activated retinal glia mediated axon regeneration in experimental glaucoma. Neurobiol Dis 2012; 45: 243–252. [DOI] [PubMed] [Google Scholar]
- Nishijima K, Ng YS, Zhong L, Bradley J, Schubert W, Jo N et al. Vascular endothelial growth factor-A is a survival factor for retinal neurons and a critical neuroprotectant during the adaptive response to ischemic injury. Am J Pathol 2007; 171: 53–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.