Abstract
Objective To determine the health‐care preferences of people with Multiple Sclerosis (MS).
Design Cross‐sectional survey using a postal questionnaire comprising standardized measures of health related quality of life (SF‐36) and of depression (BDI) and original questions about issues linked to health‐care, prioritized by people with MS during an earlier qualitative phase.
Participants A stratified sample of 318 people with MS in Scotland and England.
Results Questionnaires were sent to 471 people with multiple sclerosis. The 318 respondents (68%) reported a wide variation in quality of life, but on average scored significantly lower than normative values in all dimensions of the SF‐36. The most commonly used home treatment during the previous year was evening primrose oil, taken by almost half of the sample (47%). Use of cannabis was acknowledged by 8%. There was evidence that many preferences concerning health services were not satisfied. For instance lack of advice about at least one MS related issue was reported lacking for three‐quarters of the sample and 17% lacked advice in at least five areas. Advice about exercise was the single most requested area. The most frequently consulted health professional was the GP (78%) followed by the hospital consultant (50%). The professional that respondents most commonly said they would like to have seen was a specialist MS nurse (30%). Forty‐three percent of the sample said they had attended a special meeting for people with MS or disabilities. They were equally divided between those who did and who did not find their last attendance helpful.
Conclusions People with MS display a wide variation in their preference for services and unmet needs. Information about management (both conventional and unconventional), relevant tailored advice and access to appropriately skilled professionals should be feasible components of high quality care. This work has highlighted the value of involving people with MS in the identification of their preferences; further research is needed to show how these might be provided most effectively.
Keywords: home treatments, multiple sclerosis, preferences, quality of life
Introduction
In the UK approximately 85 000 people have Multiple Sclerosis (MS) making it the most common demyelinating disease of the nervous system. A characteristic of MS is that its course is both highly variable and equally unpredictable in terms of symptoms, signs and the resulting degree of disability. Each individual who has the disease encounters different challenges to their physical, psychological and social well‐being. Health and social care providers are, thus, faced with the problem of addressing varying needs, frequently over a period of many years.
The importance of caring for individuals within a community setting has been stated Government policy for the last decade 1 , 2, 3, –4 and advances in terms of assistive technology have recently expanded the possibility of managing physical impairment at home. 5 To ensure that appropriate and efficient services are provided to counter the impact of MS, it is important that people with MS are given the opportunity, through detailed research, to define what they perceive their needs to be and to express their preferences in the broadest sense, regarding different forms of health and social care.
An earlier qualitative study used in‐depth interviews to ascertain what a selected sample of 16 people with MS wished for in terms of social and health‐care and also what they perceived as the barriers to achieving satisfactory care. The study reported here, aimed to assess the extent to which the picture that emerged from those interviews was representative of the preferences and experiences of those who have MS in the UK. It comprised a survey based on a stratified sample of people with MS in Scotland and England using a postal questionnaire designed specifically for this task. The purpose of this paper is to present descriptive statistics concerning the health‐related quality of life of the study sample, their preferences, that is their use of self‐treatments, their actual and desired contact with health‐care professionals and their unmet information needs.
Methods
The Questionnaire
The Questions
Twelve broad constructs were identified in the qualitative study as relevant overall to the health‐care preferences of those interviewed. They were: perceptions of personal control, social support, and dependency; contribution of family and friends; contribution of health professionals; individual illness trajectory; MS exacerbations; uncertainty and stress; personal crises; fear for the future; social comparison; and life before MS.
Embedded within each of these constructs was a range of factors that had emerged as important to two or more of the interviewees. For instance, within the construct ‘perceptions of personal control’ were the following factors that might have a bearing on that construct: ‘range of self‐treatments’, ‘sufficiency of access to information’, ‘access to help with MS problems’, ‘ability to ask for help with MS problems’ and ‘perceptions of personal autonomous behaviour’. The questions were designed to enquire about the 12 constructs and the factors within them, using detailed information from the qualitative work to determine the exact wording and to define the response categories. The questions were either entirely original or were from other questionnaires with modification where necessary. Additional questionnaire items comprised socio‐demographic questions and standardized measures of health related quality of life and depression.
The original questions were piloted with the individuals who took part in the qualitative study to ensure that they were accurate representations of the content of the interviews, were easily understood, relevant and unambiguous. Some minor modifications were made and the whole questionnaire was then piloted with a wider sample.
Standardized measures
The two standardized measures were included in the questionnaire because they explored aspects of life that had emerged as important generally to people with MS, namely health related quality of life and psychological well‐being. In addition, their use provided descriptive information concerning the study population.
The SF‐36 6 is a self‐administered generic measure of health related quality of life that has been used extensively in MS research. 7 , 8, 9, –10 It comprises 36 questions that produce scores for eight dimensions. The dimensions are physical functioning, physical role limitation, bodily pain, general health, vitality, social functioning, emotional role limitation, and mental health. Change in health is a further optional dimension which was used in this study as it was applicable to people with MS. Many of the SF‐36 items specifically reflect some of the constructs that emerged as important during the qualitative phase, for example emotional problems and limitations resulting from physical impairment or social concerns. In addition, the general concept of health related quality of life has overall relevance for people with MS.
Depression is a common feature of the lives of people with MS. 11 , 12, 13, 14, –15 The Beck Depression Inventory (BDI) 16 is designed to assess the existence and severity of depression. 17 It has also been used extensively in MS research. 18 , 19, –20 A number of BDI items emerged independently as important in the qualitative phase (for example, suicidal feelings, interest in sex and disappointment with self). For brevity, the short form BDI was used. 21 A further benefit of using both the SF‐36 and the BDI was that comparison with data collected during other studies would be facilitated. 17 , 18, 19, 20, 21, –22
The Sample
The target population was all people in Scotland and England who have MS. Virtually all people with MS in these countries are registered with a GP and the vast majority of practices have procedures in place that will permit identification of these individuals. Sampling was therefore via general practices and it was planned that a total of 200 general practices would be invited to take part in the study.
It was estimated that if 35% of the selected practices agreed to participate, then, assuming an average practice list size of 8000 and a prevalence of MS of one per 1000, the study population would comprise approximately 560 people with MS. It was further assumed that between 50% and 60% of these patients would return the questionnaire or would be prepared to complete it by telephone. This would yield a sample size of between 280 and 340 people with MS, which was deemed on statistical grounds to have adequate numbers to detect associations between health outcomes and variables representing access to health‐care services. The principal purpose of this paper is to present detailed descriptive statistics from the survey.
The incidence of MS has been found to be higher in northern than in southern latitudes. In the UK, it has been documented that Scotland experiences particularly high rates of incidence and prevalence. 23 The target population was, therefore, divided into four strata: Scotland, Northern England, the Midlands, and Southern England. The health authorities (health boards in Scotland) were then numbered sequentially and random number tables were used to select two from each stratum. The actual number of practices approached within each health authority was in proportion to the number in that particular area/board. Random number tables were used to select the requisite numbers of practices for each health authority.
Recruitment
There were two recruitment stages. First, the randomly selected general practices were asked to participate. Second, people with MS who were registered with the participating practices were invited to complete the questionnaire. Before recruitment began ethics approval was gained from the relevant multicentre and local research ethics committees and the process was piloted with six local general practices.
Stage 1 – recruitment of practices
All practices selected during the sampling process were contacted by telephone to check that the address details and the name of the senior partner were correct. A letter addressed to the senior partner and information about the study were then sent to each practice. A full explanation concerning the role of participating practices was provided. A letter was sent to the non‐responding practices after 3 weeks to remind them about the study and again to invite them to take part.
Stage 2 – recruitment of people with MS
Participating practices were requested to forward an explanatory letter, a questionnaire and a prepaid return envelope, to each person they had identified in their practice as having MS.
Questionnaire completion
In the first instance completion was intended to be by the person with MS. However, there was an option for the recipient to indicate that the researcher might make contact by telephone and assist with completion; alternatively it was suggested that a carer, friend or relative could help complete the questionnaire.
A record was kept of the sex and date of birth of each person to whom a practice agreed to send a questionnaire. Receipt of completed questionnaires was recorded and after 3 weeks reminder cards were sent to the practices with a request that they were forwarded to the non‐respondents (who were identified by their sex and date of birth). To assess the possible impact of bias resulting from the sampling process and from non‐responders, limited information was obtained concerning all the practices and recipients of the questionnaire and where possible any reasons for non‐participation at either practice or individual level, were noted. For practices, the reasons included ‘lack of time’, ‘not aware of any patients with MS’ and ‘perceived patient to be too ill to complete a questionnaire’ or ‘perceived that completion would be too troublesome for patient.’ Reasons for non‐participation at the individual level were more difficult to obtain but two individuals indicated by telephone that they did not perceive the questions to be relevant to them. In one case this was because MS had such a small impact on the individual’s life and in the other it was because the person felt that they had so little mobility that all their responses would be in the lowest category (or worse).
Analysis
The characteristics of the study population and the study sample were described using frequency distributions. Comparisons were made between responders and non‐responders in respect of area, sex and age using the χ2 test. Items from the questionnaire were initially investigated using frequency distributions and summary statistics such as proportions, means and standard deviations. Self‐reported types of MS were compared in terms of mean SF‐36 scores using one way analyses of variance and in terms of depression categories using the χ2 test. Use of self‐treatments and topics about which advice was required were analysed using proportions and χ2 tests for comparisons between sexes. All analyses were conducted in Stata version 6.0 and a 5% level of statistical significance was used throughout.
Results
Characteristics of study population and study sample
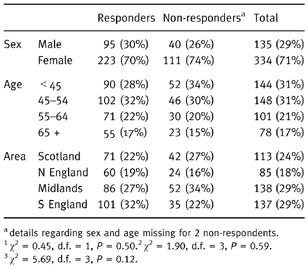
A total of 67 (34%) practices out of the 200 approached agreed to participate. The participation rates were similar across the geographical areas, apart from a lower rate (26%) in Northern England. The participating practices indicated that the total number of people with MS on their combined lists was 537 (as expected, an average of 8 per practice). However, in 66 cases, the person with MS was regarded by their GP, as unsuitable to receive a questionnaire because of their ill health (see limitations below). Consequently only 471 questionnaires were sent to the practices to be forwarded to people with MS. Although the number of questionnaires distributed was smaller than anticipated, the proportion returned was higher. A total of 318 people (68%) returned questionnaires, 95 (30%) from male and 223 (70%) from female respondents (Table 1). This sex distribution was similar to that of the non‐responders. The age distribution was also similar for responders and non‐responders. There was a slightly higher proportion of responders from southern England than the other areas but this was not statistically significant. The questionnaires were completed independently by 227 (73%) participants and with assistance by the remainder.
Table 1.
Characteristics of responders and non‐responders
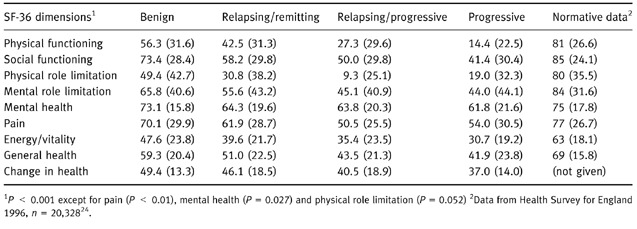
A total of 265 (83%) participants in the study sample were able to categorise their MS as either benign, relapsing/remitting, relapsing/progressive or progressive. The mean SF‐36 scores (higher score indicates better health status) for each of these categories is given in Table 2. Normative values from a national postal questionnaire that includes a similar age range 24 are also presented. In general SF‐36 scores are highest for the group categorizing their MS type as benign and decrease progressively across the groups. For a few SF‐36 dimensions, however, there is little difference between the two progressive groups. The means for all groups are lower than normative values (Table 2), and overall are similar to those found in other studies of people with MS. 8 , 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, –25
Table 2.
Mean SF‐36 (SD) scores, according to stated MS type (n = 219–262)
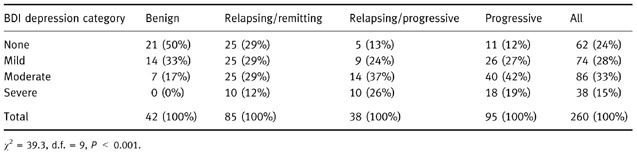
Self reported MS type according to the BDI categories of ‘no depression’, ‘mild’, ‘moderate’ or ‘severe depression’ reveal a similar trend (Table 3). Of those with ‘benign’ MS, 83% had BDI scores falling within ‘no’ or ‘mild’ depression groups and none fell into the severely depressed group. Amongst those with ‘progressive’ MS, 61% had scores that placed them in the ‘moderate’ or ‘severely depressed group’ 28% were categorized as having ‘mild depression’ and 24% as having ‘no depression’. These differences are highly statistically significant (Table 3).
Table 3.
Grouped BDI scores, according to stated MS type (n = 260)
Responses to selected individual items
Self‐treatment
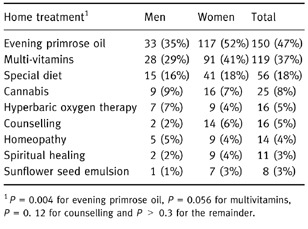
Respondents were asked about self‐treatment during the previous year. A range of alternatives that had been suggested during the qualitative phase were offered with a space for the respondent to add any medication or therapy not listed. All the listed items were used by some of the sample, but usage varied widely (Table 4). However, nearly half (47%) of the sample had taken oil of evening primrose, making this the most commonly used self‐treatment with multivitamins (37%) being the next most popular. Use of cannabis was acknowledged by 8% of respondents. Use of self‐treatments was very similar for both men and women apart from evening primrose oil and multivitamins, although only the former reached statistical significance (Table 4).
Table 4.
Use of self‐treatments by men and by women during previous 12 months
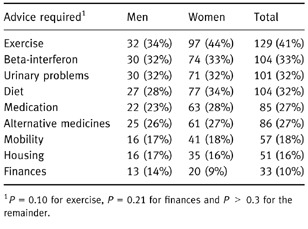
Advice required
The questionnaire attempted to establish in which areas respondents desired further advice (Table 5). Exercise was the area about which advice was most commonly desired, with 41% of the sample highlighting this need. Diet and beta interferon were next, with 33% indicating both of these areas. The need for further advice about urinary problems, other medications and alternative therapies was highlighted by about a quarter of all respondents. Overall, three‐quarters of the sample required advice in at least one area and 17% stated they would like advice about five or more areas. The advice required was very similar for both men and women – apart possibly from exercise, although this did not reach statistical significance (Table 5).
Table 5.
Advice required by men and by women
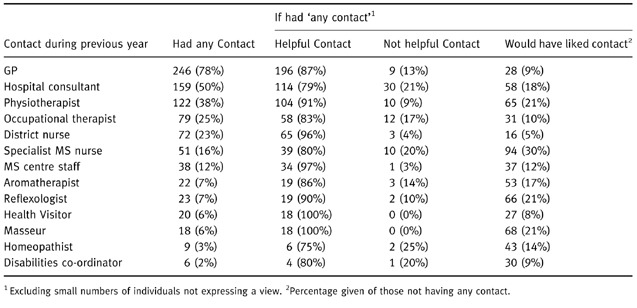
Health professionals
Contact with health professionals was common (Table 6) with only 12% of the sample having had no contact whatsoever in the previous year. The most frequently consulted professional was a GP, 78% of the sample having consulted their GP at least once in the previous year. Hospital consultants had been seen by 50% of the sample. The proportions regarding these consultations as unhelpful were 21% and 13%, respectively. A physiotherapist had been consulted by 39% and a specialist nurse by 16% of respondents. The professional whom most respondents said they would like to have seen was a specialist MS nurse (30%). The next most common response of those having any contact to this question was a masseur and a reflexologist (both 21%).
Table 6.
Contacts, usefulness of contacts and desired contacts
Special meetings
During the qualitative phase, the impact of meeting and comparing oneself with others emerged as an important dimension of life for people with MS. Of the 136 people (43%), who had ever attended a meeting either specifically for people with MS or for others with disabilities, respondents were equally divided into those who did and those who did not find their last attendance to be helpful.
Discussion
Following previous work involving a series of in‐depth interviews with people who have MS, this study has explored their use of self‐treatments, actual and desired contact with health‐care professionals and unmet information needs further by employing a postal questionnaire in a large, population based study.
The study also investigated health status and revealed poor self‐reported health related quality of life amongst people with MS compared to the general population. 24 Overall, the study population scored poorly in every SF‐36 dimension but the physical functioning and the physical role limitation dimensions were at greatest variance with normative scores. The standard deviations for many SF‐36 dimensions were large, reflecting wide variation in the health status of people with MS.
In addition, almost half the sample reported BDI scores that suggest either moderate or severe depression. This figure is in accordance with the proposal by Scott and co‐workers that between 40% and 60% of people with MS will experience moderate or severe depression at some time. 26 In most cases respondents’ self‐reported MS type seemed to be a reasonable indicator of their health status, revealing a sharp decline from benign to progressive illness.
There was considerable evidence of diversity in the range of requirements for services – for example, relating to information sought, self‐treatments used and desired contacts with health professionals. Some needs and preferences appear to be unmet to a greater extent than others. For instance, three‐quarters of the sample state that they lack MS‐related advice in at least one area. An example of this need is advice relating to urinary problems, which was required by almost a third of people in the study sample. A similar number would like to know more about diet and about beta‐interferon treatment. It is particularly striking that 41% of all respondents would like information about appropriate exercise.
People demonstrated a desire for self‐reliance in a number of ways, including a range of self‐treatments. Three‐quarters of the sample used at least one treatment at home – evening primrose oil was the most popular, with multivitamins and a special diet also commonly reported. As with most self‐treatments, all of these were more widespread amongst women than amongst men. The rank order of self‐treatments, however, was very similar for women and men.
The contribution of health professionals seems to be regarded as important to most, but not all people. General practitioners were the most frequently consulted health professionals, followed by hospital consultants and physiotherapists. In addition to conventional sources, for example the primary care team, contact is also sought and appreciated from less conventional practitioners such as aromatherapists and masseurs. Amongst those not having contact with each type of practitioner, the practitioner that people with MS most commonly indicated they would like to see was a specialist MS nurse. Amongst those who had contact, however, there was little difference between practitioners in terms of the extent to which contact was helpful.
Limitations
Although the sampling strategy aimed to achieve a representative sample of people with MS, there were practices that declined to participate, patients who did not return the questionnaire and also 66 people in participating practices who were excluded by their GP as it was considered inappropriate to invite them to complete a questionnaire. Previous research has shown that some GPs believe that it is in their patients’ interest to remain oblivious to a diagnosis of MS. 27 An explanation for the possibly paternalistic decision to exclude some individuals from the survey may be either because the GP perceived they would find completion stressful or alternatively that the impact of MS was minimal and the questionnaire would serve as a reminder of an illness of which they were barely aware.
In short, while these exclusions may result in bias, it is just as possible that practices which were aware of the specific needs of people with MS declined to take part as frequently as practices which were unaware. Similarly, participating GPs may have excluded people who were minimally affected by MS as frequently as they excluded people who were severely affected. In addition, although there was a lower participation rate for practices in Northern England, participating practices were representative in terms of number of partners and the response rate amongst patients sent the questionnaire was high. Overall, the similarity of the SF‐36 scores in the present study with those for MS patients observed previously 25 , 26, 27, –28 suggests that the various exclusions have not systematically affected the findings. In any case, the study sample included people across eight geographical areas, a wide age range, both sexes and those who lived alone, with family or in accommodation for people with disabilities.
Inevitably there are limitations to the depth of the information available from questionnaire responses; more information is available from the extensive comments written by patients in response to an open question and these will be reported in a separate paper.
Conclusion
In summary, people with MS seem to be considerably worse off than the general population in all dimensions of health related quality of life. Needs and preferences that are currently unmet relate to the desire for specific information and for the services of particular health professionals. The extent and variety of choices concerning self‐treatment and desired contact underline the need to tailor the services provided to people with MS in accordance with each individual’s preferences.
Acknowledgements
We thank all those who took part in this study. Funding for this research was provided by the Multiple Sclerosis (Research) Trust. The Division of Primary Care and the Department of Social Medicine at the University of Bristol, are part of the Medical Research Council Health Services Research Collaboration.
Bibliography
- 1. Department of Health . Working for Patients London: HMSO, 1989.
- 2. Department of Health . Caring for People: Community care in the next decade and beyond London: HMSO, 1989.
- 3. Department of Health . Caring for People: Implementation Document‐ Assessment and Case Management London: HMSO, 1990.
- 4. Secretary of State for Health and others . The Health of the Nation London: HMSO, 1991.
- 5. Agree E. The influence of personal care and assistive devices on the measurement of disability. Social Science and Medicine, 1999; 48 : 427–443. [DOI] [PubMed] [Google Scholar]
- 6. Brazier JE, Harper R & Jones NMB. Validating the SF‐36 health survey questionnaire: new outcome measure for primary care. British Medical Journal, 1992; 306 : 1440–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vickrey B, Hays RD, Harooni R, Myers LW & Ellison GW. A health‐related quality of life measure for multiple sclerosis. Quality of Life Research, 1995; 4 : 187–206. [DOI] [PubMed] [Google Scholar]
- 8. Brunet DG, Hopman WM, Singer MA, Catherine M & MacKenzie TA. Measurement of Health‐Related Quality of Life in Multiple Sclerosis Patients. Canadian Journal of Neurological Science, 1996; 23 (2): 99–103. [DOI] [PubMed] [Google Scholar]
- 9. Miller D, La Rocca L, Andrews H, Fischer J & Paty D. Illness‐related factors that affect mental health in patients with multiple sclerosis. Quality of Life Research, 1997; 6 : 418–418. [Google Scholar]
- 10. Fabio R, Choi T, Soderberg J & Hansen C. Health‐related quality of life for patients with progressive multiple sclerosis: influence of rehabilitation. Physical Therapy, 1997; 77 (12): 1704–1716. [DOI] [PubMed] [Google Scholar]
- 11. Barak Y, Kimhi R, Bodner E & Achiron A. A treatment of depression in patients with multiple sclerosis. Neurologist, 1998; 14 (2): 99–104. [Google Scholar]
- 12. Bates D. Multiple Sclerosis: A review of management in general practice Surrey: Synergy Medical Education, 1997.
- 13. DeLuca J, Johnson SK, Beldowicz D & Natelson B. Neuropsychological impairments in chronic fatigue syndrome, multiple sclerosis, and depression. Journal of Neurology, 1995; 58 : 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Patten SB & Metz L. Depression in multiple sclerosis. Psychotherapy and Psychosomatics, 1997; 66 : 286–292. [DOI] [PubMed] [Google Scholar]
- 15. Sadovnick AD, Remick MD, Allen J & Swartz E. Depression and multiple sclerosis. American Academy of Neurology, 1996; 46 : 628–632. [DOI] [PubMed] [Google Scholar]
- 16. Beck AT, Steer R & Brown G. BDI‐11 Beck Depression Inventory. Manual 2nd edn. San Antonio: The Psychological Corporation, 1996.
- 17. Wilkin D, Hallam L & Doggett M. Measures of Need and Outcome for Primary Health Care New York: Oxford Medical Publications, 1993.
- 18. Vercoulen JHMM, Hommes OR & Swanink CMA et al The measurement of fatigue in patients with multiple sclerosis. Archives of Neurology, 1996; 53 : 642–649. [DOI] [PubMed] [Google Scholar]
- 19. Aitkens JE, Fischer JS, Namey M & Rudick RA. A replicated prospective investigation of life stress, coping, and depressive symptoms in multiple sclerosis. Journal of Behavioral Medicine, 1997; 20 (5): 433–445. [DOI] [PubMed] [Google Scholar]
- 20. Campbell M, Clark P & Fleming MB. Sleep Disturbance, depression, and lesion site in patients with multiple sclerosis. Archives of Neurology, 1992; 49 : 641–643. [DOI] [PubMed] [Google Scholar]
- 21. Beck A & Beamesderfer A. Assessment of Depression: The depression inventory. Pharmacopsychiatry, 1974; 7 : 151–169. [DOI] [PubMed] [Google Scholar]
- 22. Schwartz C, Vollmer T & Lee H. Reliability and validity of two self‐report measures of impairment and disability for MS. Neurology, 1999; 52 : 63–70. [DOI] [PubMed] [Google Scholar]
- 23. Phadke JG & Downie AW. Epidemiology of Multiple Sclerosis in the north‐east (Grampian Region) of Scotland ‐an update. Journal of Epidemiology and Community Health, 1987; 41 : 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bowling A, Bond M, Jenkinson C & Lang D. Short Form 36 (SF‐36) Health Survey questionnaire: which normative data should be used? Comparisons between the norms provided by the Omnibus Survey in Britain, the Health Survey for England and the Oxford Healthy Life Survey. Journal of Public Health Medicine, 1999; 21 (3): 255–270. [DOI] [PubMed] [Google Scholar]
- 25. Candian BG. Burden of Illness of Multiple Sclerosis: Part II. Quality of Life. Canadian Journal of Neurological Science, 1998; 25 (1): 31–38. [PubMed] [Google Scholar]
- 26. Scott T, Allen D, Price T, McConnell H & Lang D. Characterization of major depression symptoms in multiple sclerosis patients. Journal of Neuropsychiatry, 1996; 8 (3): 318–323. [DOI] [PubMed] [Google Scholar]
- 27. Elian M & Dean G. Doctor and Patient: To tell or not to tell the diagnosis of multiple sclerosis. Lancet, 1985; 7 : 27–28. [DOI] [PubMed] [Google Scholar]
- 28. Brunet DG, Hopman WM, Singer M, Edgar M & Mackenzie T. Measurement of Health‐Related Quality of Life in Multiple Sclerosis. Canadian Journal of Neurological Science, 1996; 23 (2): 99–103. [DOI] [PubMed] [Google Scholar]


