Abstract
Objectives To determine preference for prognostic information in women with early breast cancer.
Design Cross sectional survey.
Participants 100 women with early stage breast cancer attending six teaching hospitals in Sydney, Australia.
Main outcome measures Women’s preference for prognostic information.
Results This study identifies new elements to consider in the prognostic consultation. Whilst 91% of women wanted to know their prognosis prior to commencing adjuvant treatment, 63% wanted their cancer specialist to check with them first before giving it. Seventy‐seven percent wanted to be asked if they would like a second opinion. Seventy‐five percent wanted to know about complementary therapies. Most wanted their cancer specialist to check their understanding, provide an opportunity to ask questions, and explain medical terms (98%). The majority wanted information summarized (94%), supported by published information (88%) and written down (79%). Ninety‐seven percent wanted their fears and concerns listened to and 79% wanted emotional support. In addition 80% of women wanted their cancer specialist to tell them where they could go to get additional emotional support for themselves and their families. Seventy‐two percent of women wanted their cancer specialist to make sure they had a relative or friend with them.
Conclusions Data from this study suggests that a variety of techniques are needed to communicate prognosis. Whilst acknowledging individual women’s preferences, and not wanting to appear prescriptive, recommendations emerge for effective discussion of prognosis with women with early stage breast cancer.
Keywords: breast cancer, communication, patient preferences, prognosis
Introduction
Over the past 20 years, the incidence of breast cancer has increased in Australia and around the world. There were 3327 new cases of breast cancer in New South Wales in 1994 (21 males and 3306 females). The lifetime risk in New South Wales has increased from one in 17 in 1973–77 to one in 11 in 1994. 1
Many people with cancer today want detailed information about their cancer diagnosis, prognosis, and treatment options, and women with breast cancer are amongst those with the strongest information needs. 2 It is now a generally accepted principle in medicine, 3 , 4 and indeed the law, 5 that people have a right to be involved in decision‐making about their medical treatment. Charters for patient rights – for example, the internationally binding Declaration of Helsinki 6 – exist to formally safeguard patient autonomy, while in several countries doctors are now legally required to provide patients with written information prior to commencing medical interventions.
The National Health & Medical Research Council of Australia recommends that ‘Patients should be encouraged to make their own decisions about medical treatments or procedures’ and that in order to do this they should be given ‘adequate information about all pertinent matters, including even low probability or mild risks in a form which promotes understanding’. 7 Recognizing the inherent difficulties in this position, which did not take into account the patient’s desire to make decisions, their emotional state or level of understanding, more recent guidelines (and many independent authors) encourage doctors to tailor information provision, and include people with cancer in decision‐making at whatever level they choose. 8 , 9, 10, –11
However, such sensitivity in communication is difficult to achieve and a number of studies have revealed disparity between patient preferences and the doctor’s ability to assess these individual preferences. For example, Strull and co‐workers (1984) studied 210 hypertensive outpatients and 50 clinicians in three different medical practices and found that physicians underestimated how much information and discussion patients with hypertension wanted. 12
A notable component of the potential array of information a clinician can disclose, and arguably the most difficult, is prognosis. While most Australian doctors tell their patients their cancer diagnosis, 13 discussion on the likely outcome of their disease, i.e. the prognosis, is less commonly presented. 14 Many doctors are concerned that frank discussion of prognosis can preclude hope and prevent helpful denial. Yet if presented with a question prompt sheet encouraging question asking before their first consultation with a medical oncologist, prognosis is the one area about which patients ask more questions. 15 In this study, it was found that of 142 patients with heterogeneous cancers who were randomized to receive either the question prompt sheet or a general information handout, 35% of those receiving the prompt sheet asked questions about prognosis compared to 16% of those receiving a general information sheet. This suggests that, when given the opportunity, some patients want to discuss their prognosis with their cancer specialist.
Several studies have documented the type of prognostic information women want, e.g. the stage of the disease and the likelihood of cure. 16 , 17 We recently surveyed 100 women with early stage breast cancer, and found that the vast majority wanted specific information about prognosis. 18 For example, 95% wanted to know their probability of cure, 94% wanted staging information and 87% wanted 10 year survival figures. However, it is not known how these preferences for prognostic information are related to preferences for amount and type of general information, or for participation in treatment decision‐making.
Furthermore, communication of prognosis is also hindered by our lack of data on women’s preferences for the manner in which they wish this information conveyed. Clearly, the actual data conveyed is only one aspect of a doctor–patient interaction, and transactional elements, both non‐verbal and verbal, play a large role in modifying the impact of such news.
This study investigated women’s individual preferences for the manner in which their cancer specialist could explain the risk of their breast cancer returning after surgery. The relationships between preferences for prognostic information, and preferences for general information and involvement in decision‐making are also explored.
Methods
Sampling and recruitment
Women were recruited through their treating physician. All major centres providing care for women with breast cancer in the Sydney Metropolitan Area were identified. In order to ensure input from a range of women, five urban centres attracting referrals from populations varying in socio‐economic status and one rural centre were approached to participate in the study. Thirteen breast surgeons and 13 medical oncologists from these centres, in both private and public practices, were invited to participate in the study and all agreed.
Consecutive women newly diagnosed (i.e. within 2 months of diagnosis) with stage I or II breast cancer between January and December 1997, were recruited. Women from a non‐English speaking background with insufficient English to complete the questionnaire, and women presenting with a second cancer were excluded. Eligible patients were sent a letter and invited to participate in the study. They received the letter within 2–4 weeks of making their own adjuvant treatment decisions. The letter was followed up by a phone call from the Research Co‐ordinator, who obtained verbal consent for participation and then sent out the questionnaire through the mail. One centre opted to send women a letter signed by their oncologist inviting them to participate in the study.
Measures
Preferences for general information and involvement in decision‐making
The amount of information the participants expected and the level of involvement in decision‐making preferred by the participants were measured using an adapted form of the Cassileth Information Styles Questionnaire. 2 Three general items from this questionnaire were included: (1) participants were asked to indicate on a Likert scale the amount of information they preferred ranging from ‘as little as possible’ to ‘as much as possible’; (2) they were asked to indicate their preferences from three response options: ‘only information needed to deal with the immediate issues’, ‘additional information only if it is good news’ and ‘as much information as possible, good or bad’ and (3) participants were also asked to indicate from a range of five options their preferred level of involvement in decision‐making. The five options ranged from ‘doctor only’ to ‘patient only’ making the decision. This scale has good internal reliability with a Cronbach’s alpha of 0.89. 2
Preferences for discussion about prognosis
Women’s preferences for discussing their prognosis with their cancer specialist were assessed by 19 questions that were a mix of both information and emotional aspects of the prognosis consultation. Women were asked to indicate on a Likert scale their agreement on each of the 19 aspects of the consultation (1=disagree completely − 5=agree completely). Items were generated on the basis of a review of the literature, an analysis of 20 audio‐tapes of initial oncology consultations with breast cancer patients (collected during another study undertaken between 1995 and 1997) 9 and expert consultation. The audio‐tapes were transcribed and content analysed to identify ways in which prognosis was described to patients.
In addition, three open‐ended questions were asked to elicit qualitative data, concerning positive and negative experiences of receiving information and emotional support from their cancer specialists, and those aspects of their communication that they found particularly useful.
Demographics
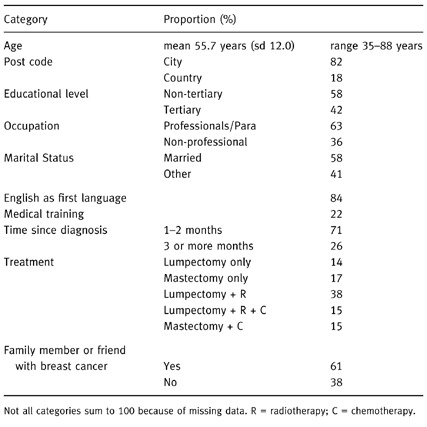
Demographic details on the subject’s age, post code, highest educational qualification achieved, occupation, marital status, quality of spoken English, level of medical training, date of diagnosis, treatment, and family members or close friends with a previous breast cancer diagnosis, were requested from participants. (See Table 1)
Table 1.
Demographic characteristics of sample (N = 100)
Procedure
The questionnaire was posted to the woman, with a stamped, addressed return envelope, as closely as possible to the woman’s initial consultation with her medical oncologist, or at her post‐surgery consultation (2–4 weeks). This timing gave women an opportunity to discuss their own prognosis with their doctor, and make decisions about their own treatment before completing the questionnaire, whilst eliciting preferences at a highly salient time. Patients who did not return their questionnaire within 3 weeks were followed up with a telephone call, or sent another questionnaire with a letter if telephone contact was not possible.
Data analytic plan
Data were analysed using the Statistical Package for Social Scientists (SPSS). 19 Descriptive statistics were used to summarize demographic data and data relating to the aspects of prognostic discussion considered important by women. Analysis of variance (anova), student t‐tests and chi‐square tests of association were used to examine the relationship between demographic variables and patient preferences for general information and involvement in decision‐making, and between general preferences and preferences for specific aspects of prognostic discussion. Test results were considered statistically significant if the P‐values were less than 0.05.
Sample sizes were calculated using the SAM sample size software package. 20 A sample size of 100 allowed detection of a difference between subgroups of 30% or more in the proportion of women preferring different levels of information and/or involvement, with a power of 0.8 and a significance level of 0.05. This sample size was also realistic, given the number of women with newly diagnosed early breast cancer seen by participating physicians within the study period.
The open‐ended responses in the questionnaire were analysed using a constant‐comparative method proposed by Glasser and Strauss (1967). 21 This involved coding each unit of meaning (i.e. specific response), and comparing and contrasting these to identify recurring regularities and discrete categories.
Results
One hundred and forty‐three women seen consecutively at six treatment centres were contacted by letter and telephone. One hundred and eighteen agreed to participate (83%) and 100 questionnaires were returned. Demographic characteristics are presented in Table 1. Mean age was 56 years (sd 12.0); and most were city dwellers. Just over half had completed University entrance, university or some form of tertiary training. The percentage of women with tertiary qualifications was 42% (compared with 37% in the general Australian population). 22 Nearly two thirds worked (or had worked) in professional or paraprofessional occupations, and 22% were working in occupations related to medicine (e.g. doctor, nurse, medical receptionist, technician).
Women’s preferences for prognosis discussion
The way in which prognostic information is communicated was important to the women in this study. (See Table 2). Sixty‐three percent of women wanted their cancer specialist to check with them first to ascertain whether they wanted to know their prognosis. Ninety‐nine percent of women wanted their cancer specialist to check understanding, give them an opportunity to ask questions (99%) and explain medical terms (98%). Seventy‐seven percent wanted to be asked if they would like a second opinion. Seventy‐five percent of women also wanted their specialist to talk to them about complementary therapies, e.g. relaxation.
Table 2.
Aspects of prognostic discussion women considered important
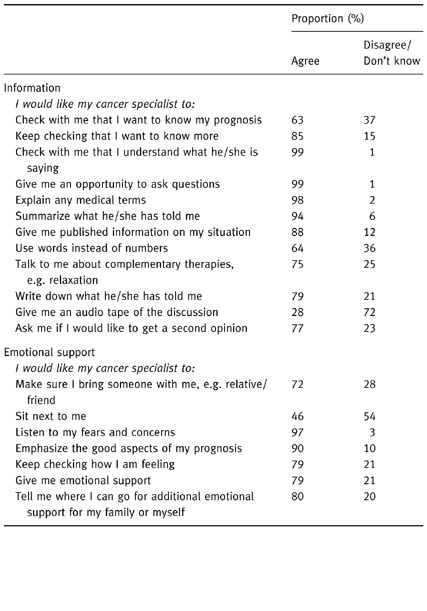
Emotional sensitivity and the provision of emotional support (e.g. listen to my fears and concerns, keep checking how I am feeling) was also important for women in this study. Ninety‐seven percent of women wanted their cancer specialist to listen to their fears and concerns when discussing prognosis and 79% wanted emotional support. However, whilst they rated both information and emotional support highly, suggesting that they want their doctor to meet many of their needs, 80% of women wanted their cancer specialist to tell them where they could go to get additional emotional support for themselves and their families.
Women’s preferences for general information
Eighty‐three percent of women wanted as much information as possible and 16% wanted limited information. Women’s preference for the amount of information they wanted about their illness was unrelated to age, education, occupation, time since diagnosis or type of surgery or adjuvant treatment received.
Relationship between preferences for general information and specific prognostic preferences
Two prognostic features preferred by women were related to general information preferences. The preferences for each prognostic feature were collapsed into 2 categories (disagree/don’t know or agree). Fifty‐four percent of women who wanted limited information vs. 83% of women who wanted as much information as possible, wanted the doctor to keep checking on how they were feeling (χ2 1=5.9, P=0.02). Sixty‐two percent of women who wanted limited information vs. 92% of women who wanted as much information as possible wanted to be given published information (χ2 1=9.1, P=0.003).
Women’s preferences for decision‐making
Fifty‐four women wanted collaborative decision‐making (i.e. involving both themselves and their doctor). Twenty‐three preferred the doctor make the treatment decision, and 23% preferred to make the decision themselves. Women preferring collaborative decision‐making were significantly younger than women who preferred that their doctor make the decision (F2,95=5.7, P=0.005). The mean age of women wanting collaborative decision‐making was 52.6 years in comparison to women preferring that the doctor make the decision (mean 62.2 years). The age of women wanting to make their own decision spanned a wider range (mean 57.1 years). Involvement in decision‐making was unrelated to any other demographic variables.
Relationship between preferences for involvement in decision making and specific prognostic preferences
Only one prognostic feature was related to preferences for involvement in decision‐making. Fifty‐five percent of women who wanted their doctor to make the decision for them, wanted a second opinion vs. 86% and 82%, respectively, of women who wanted to make the decision themselves or to make the decision collaboratively (χ2 2=7.1, P=0.03).
Qualitative data
Sixty‐seven women completing the questionnaire gave additional comments on how they were given information on their own cancer.
Women reported on positive and negative experiences related to receiving information and emotional support from their cancer specialists. The positive aspects (n=17) of information giving included the doctor giving a full explanation, using plain language, drawing diagrams, providing written information (booklets), repeating information, allowing time to ask questions, using positive language, e.g. ‘small’, ‘early’. Several women commented on the value of having access to the doctor after the initial consultation to ask further questions for clarification, e.g. ‘I appreciated the fact that I was able to ring my specialist and ask more questions a few days after the initial information was given’.
The benefits of written information were also emphasized: ‘Written information that can be read and absorbed in your own time, this is essential as the initial shock of diagnosis drives rational thought from your mind’; ‘As English is my second language, I would have preferred that all information be given up front so I could discuss it with my family’; ‘I did understand, but when one gets home and you try to remember, you only take in certain amounts. I feel it is very important that facts and figures are written down for each patient on the first visit’.
The interpersonal elements which women found useful (n=17) were the doctor ‘giving hope; assisting in making decisions, showing compassion; being honest, sensitive, positive, sympathetic, empathetic; and the provision of support outside of the consultation, e.g. volunteer support services, access to the internet; NH & MRC Consumer Guidelines to Early Breast Cancer 8 ; and being able to telephone the doctor for clarification after the consultation’.
The negative aspects (n=23) included the doctor inadequately preparing women for surgery; rushing women to make a decision about treatment; using inappropriate language, e.g. ‘bunt, unfeeling; harsh, fear arousing, patronising, abrupt’ not asking how much information and detail women wanted; giving insufficient information on staging; or giving prognostic information before pathology results were confirmed; not explaining medical information and not writing down information.
Receiving prognostic information at the same time as having to make decisions about treatment was problematic for some women. ‘I had to immediately decide on the date and detail of my operation – it was too soon. I was still digesting the fact that I had cancer and was not capable of making good decisions about follow‐up events.’‘On the first visit to the surgeon I thought I was being booked in for 1 day surgery and lumpectomy. I was alone and he very bluntly said he would have to take the whole breast and lymph nodes. Three months later and on chemotherapy I am still in shock’. ‘I was told the very first day that if you don’t have the lump removed you will die. Already in shock I thought it was very harsh’.
Discussion
This study identified some new elements to consider in the prognostic consultation. The majority of women wanted their cancer specialist to check with them first if they wanted to know their prognosis, and to keep checking if they wanted to know more. This suggests that women want to control the flow of information they receive, and that doctors need to tell women what sort of prognostic information they can give them and then ask what level of detail women want.
The questionnaire did not identify those women who actually sought a second opinion, however, three quarters of the women wanted to be asked if they wanted one. Interestingly, even amongst the women who wanted their doctor to make the treatment decision, over half (55%) wanted this opportunity, although significantly more women who favour a collaborative or dominant role in decision‐making wanted to be asked if they wanted a second opinion. As one woman said, ‘being offered a second opinion from another specialist for my adjuvant therapy was reassuring and very helpful in my care’.
Overwhelmingly, the women wanted their understanding to be checked, an opportunity to ask questions, and explanations of medical terms, reflecting the difficulty of taking in complex new information in a state of heightened emotional arousal, and a desire for opportunities to review the information. These strong preferences also suggest that women regard prognosis as essential information and want to be given the time to understand it. Women also wanted information summarized, supported by published information and to be written down. Women who indicated a general preference for maximum information were significantly more likely to want published information, suggesting that they particularly valued the written word. These results follow recommendations by Ley (1982), 23 who found that understanding can be increased by doctors supporting oral information with written information, using illustrations such as graphs and diagrams, repeating information and allowing an opportunity for questions.
Women could also be followed‐up by specialist breast care nurses who can check understanding and refer women to sources such as Cancer Information Services, or Breast Cancer Support Services for support, information, booklets and other published data. The usefulness of an audio‐tape of the consultation to assist understanding has been identified in previous literature. 24 However, only 28% of women in this study wanted an audio‐tape of their consultation. Finally, videos and interactive programmes have also been demonstrated to aid understanding. 25
Three quarters of the women also wanted their specialist to talk to them about complementary therapies, e.g. relaxation. This figure mirrors the high use of complementary therapies within the cancer community, and perhaps reflects their desire to have some control over their prognosis and outcome.
In Australia, guidelines for doctors on how to break bad news emphasize that the way information is given is as important as the type of information provided. 26 Women in this study wanted both information and emotional support. Ninety‐seven percent of women wanted their cancer specialist to listen to their fears and concerns when discussing prognosis and 89% wanted emotional support. In particular, women who wanted as much information as possible also wanted emotional support suggesting high overall needs in both areas. In addition most women wanted their cancer specialist to tell them where they could go to get additional emotional support for themselves and their families. Whilst the high ratings women gave for information and emotional support may suggest that they want their doctor to meet all their needs, women were willing to access cancer support services for themselves and their family. Cancer specialists can meet this request by directing women to the hospital social work or psychology department or outside sources such as the Cancer Information Services. Breast nurses who may provide support in some clinical settings are not generally available in Australia.
Butow et al. (1996) 14 found that patient preferences for communication during the diagnostic consultation were not always consistent with published guidelines. For example, Australian guidelines 26 recommend the presence of a friend or relative in the bad news consultation. In their study, 38% of patients preferred to be alone when given their diagnosis, whereas others wanted a spouse (50%) or a friend (3%) present. 14 Twenty‐eight percent of women in the current study did not want their cancer specialist to make sure they had a relative or friend with them. This study supports Butow’s conclusion, that a consensus‐based list for how to disclose information is too simplistic and that guidelines concerning communication need to be derived from patient‐based data. 14
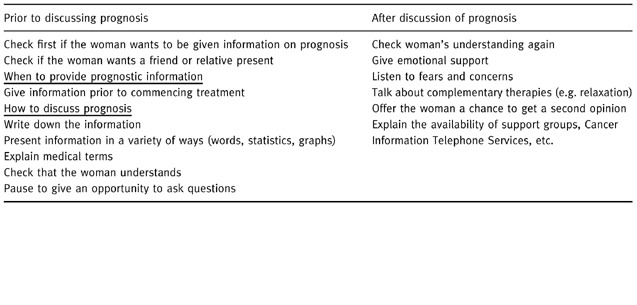
We conclude that women should be given information in a staged manner that gives them the opportunity to confirm their diagnosis and prognosis and formulate questions, and that emotional support is a vital accompaniment to a discussion of prognosis. Whilst acknowledging individual women’s preferences, and not wanting to appear prescriptive, recommendations have emerged for effective discussion of prognosis with women with early stage breast cancer (see Table 3).
Table 3.
Recommended steps for effectively discussing prognosis with women with early breast cancer
Limitations of this study
It is acknowledged that this study is level IV evidence 27 (i.e. uncontrolled trials, e.g. case series or case studies) and could be followed up by research with a stronger design (e.g. randomized controlled trials) to investigate the specific hypotheses raised here. However, for obtaining preference data, a level IV methodology (i.e. a questionnaire) is appropriate.
There are problems associated with conducting a mail survey, e.g. the inability to control the sequence in which the women read questions, the opinions of others distorting responses, and not knowing who has actually completed the questionnaire. However, with seven treatment centres and 23 participating clinicians involved in the research project, it was impractical for the researcher to attend each clinic to interview patients.
It should be noted that women in this study were highly educated (42% to tertiary and above) and that 25% of them had some form of medical training. Overall, the sample size was small (100 women) and sample selection procedures did not ensure that the sample was representative of all women diagnosed with early stage breast cancer in New South Wales, Australia. Therefore, the generalizability of findings to all women in this setting, and to other cultures and countries, is limited.
This study included only women with early breast cancer. However, equally important and more neglected in the time‐course of cancer, are those diagnosed with metastatic disease. Each setting has its own relevant statistics and concerns. A primary concern of patients with early stage disease is their chance of cure. However, for patients with metastatic disease in general, more pertinent information is the likelihood of treatment working and how long they may have to live. Prognostic information is likely to have a much greater emotional impact for this group, and earlier work has shown that as disease progresses, preferences for information decrease. 28 The generalizability of the results reported here to the metastatic setting is unclear. Replication of this study in women with metastatic disease would be desirable.
An examination of the language used by health professionals to communicate risk in areas such as breast cancer screening and in genetic counselling of women from high risk breast cancer families may provide further insight into women’s understanding and preferences for risk communication. It would also be beneficial to examine if the findings of this present study can be generalized to patient understanding and preferences for the communication of prognosis in cancers other than breast cancer.
Finally, further research involving women at any time after a breast cancer diagnosis should allow for comparisons of information needs at difference points in the disease course and a longitudinal study would better enable health professionals to understand patients’ on‐going information needs.
Acknowledgements
We thank Dr Afaf Girgis, Dr Lyn Mann, Ms Kate White, Ms Joan Wilson and Ms Kim Hobbs for their assistance and advice. Acknowledgement is also given to the 23 clinicians who participated in this project, and the women who so willingly filled out the questionnaire. Funding: The NH & MRC National Breast Cancer Centre of Australia funded this research. Conflict of Interest: None.
Bibliography
- 1. Coates M & Armstrong B. Cancer in New South Wales – Incidence and Mortality 1994 Sydney, New South Wales: NSW Central Cancer Registry, Cancer Control Information Centre, NSW Cancer Council, 1997.
- 2. Cassileth BR, Zupkis RV & Sutton‐Smith K V. Information and participation preferences among cancer patients. Annals of Internal Medicine, March; 1980. : 832–836. [DOI] [PubMed]
- 3. Goldberg RJ. Disclosure of issues to adult cancer patients: Issues and update. Journal of Clinical Oncology, 1984; 2 : 948–954. [DOI] [PubMed] [Google Scholar]
- 4. Lantos J. Informed Consent. The whole truth for patients? Cancer, 1993; 72 : 2811–2815. [DOI] [PubMed] [Google Scholar]
- 5. Rogers V. Whittaker High Court of Australia, decision handed down 19, November, 1992 (FC92/045). Canberra: High Court of Australia, 1992.
- 6. World Medical Assembly The Declaration of Helsinki. British Medical Journal, 1964; 1966; 1448–1449.
- 7. National Health & Medical Research Council . Statement on human experimentation and supplementary notes Canberra, Australia, 1988.
- 8. National Health & Medical Research Council . A consumer’s guide – Early breast cancer 1st edn. Canberra: Australian Government Publishing Service, 1995.
- 9. Brown R, Dunn SM & Butow PN. Meeting patient expectations in the cancer consultation. Annals of Oncology, 1997; 8 : 877–882. [DOI] [PubMed] [Google Scholar]
- 10. Beisecker AE, Helmig I, Graham D & Moore WP. Attitudes of oncologists, oncology nurses and patients from a women’s clinic regarding medical decision making with older and younger breast cancer patients. Gerontologist, 1994; 34 : 505–512. [DOI] [PubMed] [Google Scholar]
- 11. Schain W. Patients’ rights in decision making: the case for personalism versus paternalism in health care. Cancer, 1980; 46 : 1035–1041. [PubMed] [Google Scholar]
- 12. Strull WM, Lo B & Charles G. Do patients want to participate in medical decision making. Journal of the American Medical Association, 1984; 252 : 2990–2994. [PubMed] [Google Scholar]
- 13. Charlton RC. Breaking Bad News. Medical Journal of Australia, 1992; 157 : 615–621. [DOI] [PubMed] [Google Scholar]
- 14. Butow PN, Kazemi J, Beeney LJ, Griffin A, Tattersall MHN & Dunn SM. When the diagnosis is cancer: Patient communication experiences and preferences. Cancer, 1996; 77 : 2630–2637. [DOI] [PubMed] [Google Scholar]
- 15. Butow PN, Dunn SM, Tattersall MHN & Jones QJ. Patient participation in the cancer consultation: Evaluation of a question prompt sheet. Annals of Oncology, 1994; 5 : 199–204. [DOI] [PubMed] [Google Scholar]
- 16. Hughes KK. Decision making by patients with breast cancer: the role of information in treatment decision selection. Oncology Nursing Forum, 1993; 20 : 623–628. [PubMed] [Google Scholar]
- 17. Meredith C, Symonds P, Webster L, Lamont D, Pyper E, Gillis CR & Fallowfield L. Information needs of cancer patients in west Scotland: cross sectional survey of patients’ views. British Medical Journal, 1996; 313 : 724–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lobb EA, Butow PN, Kenny DT & Tattersall MHN Communicating prognosis in early breast cancer: do women understand the language used?. Medical Journal of Australia, 1999; 171 : 290–294. [PubMed] [Google Scholar]
- 19. SPSS . Advanced StatisticsTM, 6.1 Chicago: SPSS Inc., 1994.
- 20. Glaziou P. SAM 2.1: a Sample Size Calculator (Computer Program) Sydney: NHMRC Clinical Trials Centre, 1992.
- 21. Glaser BG & Strauss AL. The discovery of grounded theory. Strategies for Qualitative Research Chicago: Aldine, 1967.
- 22. Australian Bureau of Statistics . Australian Women’s Year Book Canberra: Australian Bureau of Stastics, 1997.
- 23. Ley P. Giving information to patients. Social Psychology & Behavioural Science: 339–372, 1982.
- 24. Dunn SM, Butow PN, Tattersall MHN, Jones QI, Sheldon J, Taylor J & Sumich MD. General information tapes inhibit the recall of the cancer consultation. Journal of Clinical Oncology, 1993; 11 : 2279–2285. [DOI] [PubMed] [Google Scholar]
- 25. Thomas R, Thornton H & Mackay J. Patient information materials in Oncology: Are they needed and do they work. Journal of Clinical Oncology, 1999; 11 : 225–231. [DOI] [PubMed] [Google Scholar]
- 26. Girgis A & Sanson‐Fisher R. How to break bad news – An interactional skills training manual for general practitioners, junior medical officers, nurses, surgeons (Training Manual). Sydney: New South Wales Cancer Council, 1997.
- 27. Oxman AD. Checklists for review articles. British Medical Journal, 1995; 309 : 648–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Butow PN, Maclean M, Dunn SM, Tattersall MHN & Boyer MJ. The dynamics of change: Cancer patients’ preferences for information, involvement and support. Annals of Oncology, 1997; 8 (9): 857–863. [DOI] [PubMed] [Google Scholar]


