Abstract
Decision aids for health service users facing decisions about screening have been developed for controversial tests (such as that for prostate specific antigen as a screen for prostate cancer) and tests in which outcomes are value laden (as in some prenatal tests). The potential usefulness of decision aids in established screening programmes (such as those offering mammography to women over 50 in the United Kingdom) remains to be explored. In principle any decision about screening test acceptance may be sensitive to individual preferences and could be supported by an appropriate decision aid. Decision aids might also help reduce some of the problems currently associated with public misconceptions about screening. Objections to the promotion of individual choice regarding screening tests usually take the form of concern that this will lead to unacceptable losses in terms of population health gain and health system efficiency, or of fear that individuals will choose options that are wrong for them. The introduction of decision aids could alleviate both of these objections to some extent. Decision aids could encourage people to consider the social as well as the individual consequences of their choices and they should promote choices consistent with personal values. Although there are strong arguments in principle for introducing decision aids into established screening programmes, their potential needs to be confirmed in empirical evaluations and there may be many contentious decisions and practical challenges to be overcome in order to implement them.
Keywords: decision support, screening, shared decision‐making
Introduction
Decision aids have been variously defined, but broadly speaking they are interventions to help people facing specific decisions between alternative courses of action. Decision aids for health service users aim to help them to consider relevant health‐care options before deciding which (if any) to have. They usually encourage selection of the option most likely to lead to individually preferred outcomes.
Decision aids for health service users have been developed for several situations in which it is thought particularly important that individual preferences influence decisions or that people make their own informed choices. These include situations in which treatment outcomes are uncertain or the outcome profiles of the treatment options are such that individual preferences may vary. 1 , 2 For example, several decision aids have been developed for people facing decisions about the treatment of benign prostate disease 3 , 4 and early‐stage breast cancer. 5 , 6 , 7 , 8 Decision aids have also been developed for people facing decisions about controversial screening tests such as prostate specific antigen (PSA) testing for prostate cancer 9 , 10 , 11 and about prenatal 12 and genetic 13 screening tests that are recognized to raise difficult personal and moral issues. Information materials that aim to persuade people to accept a particular option are excluded from the definition of decision aids. 14
It has been suggested that decision aids are less useful than conventional informed consent approaches for situations in which treatment policies have been set as standard because treatment outcomes are known and patients’ preferences consistently favour a particular option. 15 However, not all ‘standard’ treatments would be consistently favoured by all well‐informed individuals. This raises the question of whether decision aids should be used to enable people to opt for something other than the standard intervention.
This paper considers the potential of decision aids for individual decisions about screening tests, particularly in the context of established screening programmes. After noting the diversity of screening tests, programmes and decision aids, it explores when and why decision aids might be useful and considers some objections to their use. It notes the importance of empirical data about the effectiveness of decision aids and lays down some challenges for the future.
The diversity of screening tests and programmes
Screening tests have been developed to identify various latent diseases or problems that have different implications and can be treated with varying degrees of success. The tests themselves vary in terms of their sensitivity, specificity and predictive values in particular populations and the performance of a test can be significantly affected by the context in which it is used. Screening tests carry different risks of side‐effects, including psychological harm. The nature of the decisions that follow the receipt of positive (abnormal) test results varies because of the diverse properties of the diagnostic and treatment options that are available for different suspected conditions.
The diversity of screening test attributes across a range of variables means that whatever criteria are used to assess them, their desirability varies. The attractiveness of a particular screening test may seem different when viewed from population and individual perspectives. For example, risks of harm which seem acceptable when considered as population averages may not seem so acceptable when considered on an individual basis. 16 Individuals may value screening tests differently for themselves.
Decisions about whether and how health‐care systems will make particular screening tests available can be made in various ways. 17 , 18 This is not the place to review approaches to policy formulation or the merits of particular policies. However, it is important to note that the ways in which screening tests are made available affect both the properties of the test package and the extent to which people are free to make their own choices. For example, state laws and regulations about the screening of newborn babies in the USA vary in terms of: the conditions they cover; what kind of information is provided about screening tests; whether or not parents can refuse the tests; what reasons for refusal are allowed; and whether explicit consent is required. 19 At a local level, the way that screening test provision is organized and the preferences and communication practices of health professionals also affect the extent to which individuals are enabled to make their own informed choices.
The varied characteristics of screening tests and programmes, the modus operandi of local systems and the beliefs and behaviours of the people who deliver screening tests may all affect the potential impact and value of decision aids for screening tests.
The diversity of decision support
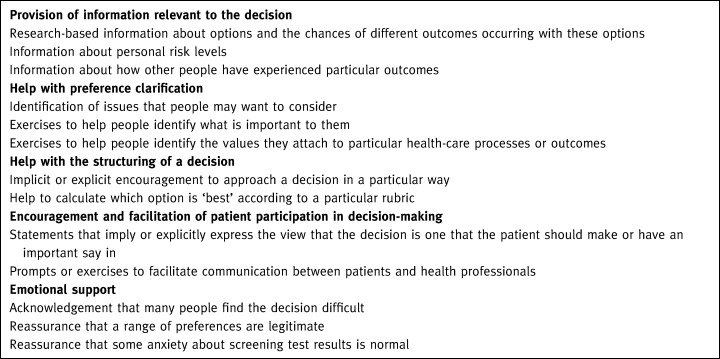
Decision aids can vary enormously in terms of (among other things) the decisions they refer to, the type(s) of decision support they provide (see Box 1), the media they employ, and the way they are intended to be used in relation to discussions between health‐care providers and health service users.
Table Box 1.
Various forms of decision support
The types of decision support that are provided in decision aids developed for health service users probably reflect developers’ beliefs about how decisions should be informed and made, and what is currently poorly done or problematic in the making of the particular decisions that they are interested in. Even ‘evidence‐based’ decision aids require value judgements to be made in their development. 20
Why might decision aids be useful in screening programmes?
All screening tests involve trading‐off acceptance of an intervention that carries some inconvenience and risk to physical, psychological and possibly social well‐being in the present against the possibility of averting some other health state (in oneself or one’s children) in the future. People can vary in their relative valuations of the different health states in question, the way they discount time, and their opinions about when interventions such as screening are appropriate and acceptable. Decisions about the acceptance of any screening test may therefore be sensitive to individual preferences. Thus there is a strong argument, particularly if we draw on the ethical principle of respect for autonomy, that decisions about the acceptance or otherwise of any screening test should be made individually and could be facilitated by decision aids that help people to weigh up the trade‐offs for themselves.
However, decision aids for health service users would seem anomalous in the context of compulsory screening programmes. Similarly, it would seem strange for a health‐care system to actively distribute a decision aid relating to a screening test that it does not offer (although information materials about the test might still be useful in both situations).
Decision support is already considered useful (at least by some) in situations where the importance (and perhaps difficulty) of individual decisions is widely accepted. These include situations in which the performance of screening tests is being tested (i.e. people are being asked to participate in research), medical opinion about the value of the test is divided, or the test is widely recognized to raise personal and moral issues on which individuals may legitimately adopt different standpoints.
However, what about the role of decision aids in the context of established but non‐compulsory screening programmes such as the national screening programmes for breast and cervical cancers in the UK or those offered by health maintenance organizations in the United States of America? The screening tests provided in these contexts have been deemed by a team of policy makers to warrant offering them to a particular population, although their effectiveness in relation to various criteria and their desirability to individuals may vary.
Within established but non‐compulsory screening programmes, decision aids could facilitate the implementation of policies promoting informed individual choice consistent with personal values. They might also, depending on the types of decision support that they offer, help to address several currently perceived problems.
Misconceptions about the purpose and accuracy of screening tests are widespread 21 , 22 and may cause several problems. Many people apparently accept or reject tests on the basis of misunderstandings. For example, in the absence of good quality information, many women assume that prenatal tests are routine procedures that are clearly in their best interests. 23 People who accept tests without being aware of their implications may be ill‐prepared for the decisions they have to face if they receive positive (abnormal) results and may wrongly interpret negative (normal) results as a guaranteed ‘all clear’. When tests do not live up to inappropriately high expectations public confidence in screening programmes can be dented and expensive litigation may ensue. 24
By presenting decisions about screening tests as ones that need to be deliberated and by providing information about their limitations and possible consequences, decision aids might alleviate some of these problems. In particular, they might encourage people to understand that although a policy decision has been taken at a national or service level to offer or promote a screening test, the test is not perfect and may have disadvantages as well as advantages. Decision aids might help people to be clearer and more confident about why they are having screening tests and might also help people to cope with test results and their implications.
Decisions about screening can be complex and decision aids might reduce the cognitive burdens of thinking through the various ‘what if’ scenarios associated with the receipt of different possible test results and diagnostic and management options. Decision aids that show how different people have experienced these scenarios might be helpful to those who find them hard to imagine.
People who undergo screening tend to be anxious about the results and their anxiety doesn’t always resolve on provision of negative results. 25 Decision aids might reduce anxiety that is due to misunderstandings by providing relevant information and may also help by addressing emotional issues.
Objections to the use of decision aids in established screening programmes
The two main objections to the promotion of individual choice about screening tests arise when population considerations are given precedence over individual ones and when paternalistic beneficence is given precedence over autonomy.
Screening programmes are usually established with the aim of improving population health (improvement being defined by the policy makers), and doing this in a resource efficient way. These aims can come into tension with policies that encourage people to make decisions about their health‐care on an individual basis. If individuals choose not to have the screening test in question (and the extent to which they would do this with or without decision aids is an empirical question), the hoped‐for population health gains will be less than theoretically possible and the costs of the test per person accepting it and in relation to benefits obtained will rise. Some people think that, at least in some circumstances, resource efficient population health gain should be the primary goal and should take precedence over individual choice. They therefore advocate compulsory screening and/or think that interventions such as decision aids which support individual choice would be inappropriate.
Some health professionals, particularly those with narrow views of what constitutes health gain, fear that ordinary people will not make ‘good’ decisions about their health‐care. They worry that people may make choices that are ‘wrong’ and harmful for them as individuals.
The question of when it is appropriate for health systems or their representatives to prevent people from making their own choices cannot be discussed here. However, the objections to individual choice that are outlined above might be alleviated rather than exacerbated by decision aids. Autonomous individual choices need not be selfish individualistic ones 26 and decision aids need not deny the importance of population perspectives. They could explore the implications of a screening test from a population as well as an individual perspective and could explicitly encourage people to consider the social implications of their individual decisions. Also, decision aids are more likely to reduce than increase the likelihood of individuals choosing options that are detrimental to their interests because they should help people to make informed decisions consistent with their personal values.
The effects of decision aids in practice
Although there are strong arguments in principle for introducing decision aids into established screening programmes, decisions about this should be informed not just by arguments about their potential, but by empirical evidence of their effects in practice. Reviews of such evidence (covering decision aids about treatment as well as screening options) show that decision aids can improve people’s understanding of relevant health‐care options and their outcomes, reduce decisional conflict, increase the extent to which choices are congruent with personal values and stimulate people to be more active in decision‐making about their care without increasing their anxiety. Decision aids have had a variable impact on the patterns of decisions made (the variable impact on screening test uptake rates may reflect variations in baseline uptake rates and differences in the dominant influences on uptake before the decision aids were introduced). Their impact on health‐care outcomes is unclear. 14 , 15 , 27
However, the generalizability of findings from evaluations of specific decision aids may be limited. Most of the decision aids studied to date have been developed with and evaluated among health professionals who recognize that individuals have varying but legitimate preferences and who want to help people to make the choice that is right for them. Decision aids may have different effects if health professionals do not share or prioritize their aims. 28 , 29 The effects of decision aids are also likely to be influenced by the nature of the decisions addressed, the types of decision support provided, the health‐care contexts in which they are used and the population groups using them.
Challenges for policy makers and decision aid developers and evaluators
There are good reasons to think that decision support may be useful to people facing decisions about specific screening tests in the context of established screening programmes. However, there is no clear consensus about where and how the balance should be struck between supporting informed individual choice and promoting widespread uptake of at least some tests.
Before they decide what type of support to provide for people eligible for specific screening programmes, policy makers need to clarify the objectives, facts and values that underpin those programmes. If they want to improve the extent to which the uptake of screening tests is informed and/or to ensure respect for individual choice, then the potential contribution of decision aids certainly warrants further exploration.
If decision aids are to be used, consideration must be given to issues such as who will produce them and how, what forms of decision support they will include, and how they will be made available. 30 Questions about whether and how to present some types of information may be particularly contentious and arguments may rage about the elusive boundary between information that facilitates individual choice and information that is inappropriately persuasive. For example, in the past the benefits and harms of screening have usually been discussed solely in terms of physical health outcomes as experienced by those who screen positive. However, the importance of the psychological, behavioural and social implications of screening, particularly for those who do not benefit in the sense of having a physical health problem detected early, is increasingly recognized and may be important to individual decisions. 31 Opinions will vary about the appropriateness of including this information in decision aids.
Empirical evaluations of the effects of decision aids in practice will continue to be important. However, the selection of criteria against which to evaluate decision aids is value laden. 32 While it may be important to understand the effects of introducing the decision aid on many variables, including screening uptake rates and health service users’ satisfaction with the decision aid and their decision, the question of which criteria should be used to define success is more contentious. It requires reference to the underlying philosophy and values of the screening programmes, decision aids and evaluators and hence is likely to be debated for a while to come.
Acknowledgements
The Health Services Research Unit receives core funding from the Chief Scientist Office of the Scottish Executive Health Department. The views expressed in this paper are those of the author and not necessarily those of the Department.
This paper has been adapted from a paper prepared for discussion at the National Screening Programme workshop on Informed Choice in Screening and Preventive Care, 19–20 June 2000. I am grateful for helpful comments from two reviewers.
References
- 1. Kassirer JP. Incorporating patients’ preferences into medical decisions. New England Journal of Medicine, 1994; 330 : 1895–1896. [DOI] [PubMed] [Google Scholar]
- 2. Pauker SG & Kassirer JP. Contentious screening decisions: does the choice matter? New England Journal of Medicine, 1997; 336 : 1243–1244. [DOI] [PubMed] [Google Scholar]
- 3. Barry MJ, Cherkin DC, Chang YC, Fowler FJ, Skates S. A randomized trial of a multimedia shared decision‐making program for men facing a treatment decision for benign prostatic hyperplasia. Disease Management and Clinical Outcomes, 1997; 1 : 5–14.DOI: 10.1016/s1088-3371(96)00004-6 [Google Scholar]
- 4. Deber R, Kraetschmer N, Trachtenberg J. Shared decision‐making: how does one measure success? (Abstract) Medical Decision-making, 1994; 14 : 429–429. [Google Scholar]
- 5. Street RLJ, Voigt B, Geyer CJ, Manning T, Swanson GP. Increasing patient involvement in choosing treatment for early breast cancer. Cancer, 1995; 76 : 2275–2285. [DOI] [PubMed] [Google Scholar]
- 6. Sawka CA, Goel V, Mahut CA et al Development of a patient decision aid for choice of surgical treatment for breast cancer. Health Expectations, 1998; 1 : 23–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Owens RG, Ashcroft JJ, Leinster SJ, Slade PD. Informal decision analysis with breast cancer patients: an aid to psychological preparation for surgery. Journal of Psychosocial Oncology, 1987; 5 : 23–33. [Google Scholar]
- 8. Chapman GB, Elstein AS, Hughes KK. Effects of patient education on decisions about breast cancer treatments: a preliminary report. Medical Decision-making, 1995; 15 : 231–239. [DOI] [PubMed] [Google Scholar]
- 9. Flood AB, Wennberg JE, Nease RFJ, Fowler FJJ, Ding J, Hynes LM. The importance of patient preference in the decision to screen for prostate cancer. Journal of General Internal Medicine, 1996; 11 : 342–349. [DOI] [PubMed] [Google Scholar]
- 10. Davison BJ, Kirk P, Degner LF, Hassard TH. Information and patient participation in screening for prostate cancer. Patient Education and Counselling, 1999; 37 : 255–263.DOI: 10.1016/s0738-3991(98)00123-2 [DOI] [PubMed] [Google Scholar]
- 11. Wolf AM, Nasser JF, Schorling JB. The impact of informed consent on patient interest in prostate specific antigen screening. Archives of Internal Medicine, 1996; 156 : 1333–1336. [PubMed] [Google Scholar]
- 12. Michie S, Smith D, McClennan A, Marteau TM. Patient decision‐making: an evaluation of two different methods of presenting information about a screening test. British Journal of Health Psychology, 1997; 2 : 317–326. [Google Scholar]
- 13. Lerman C, Biesecker B, Benkendorf JL et al Controlled trial of pre‐test education approaches to enhance informed decision‐making for BRCA1 gene testing. Journal of the National Cancer Institute, 1997; 89 : 148–157.DOI: 10.1093/jnci/89.2.148 [DOI] [PubMed] [Google Scholar]
- 14. O'Connor AM, Rostom A, Fiset V et al Decision aids for patients facing health treatment or screening decisions: systematic review. British Medical Journal, 1999; 319 : 731–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. O'Connor AM, Fiset V, DeGrasse C et al Decision aids for patients considering options affecting cancer outcomes: evidence of efficacy and policy implications. Journal of the National Cancer Institute Monographs, 1999; 25 : 67–80. [DOI] [PubMed] [Google Scholar]
- 16. Asch DA & Hershey JC. Why some health policies don’t make sense at the bedside. Annals of Internal Medicine, 1995; 122 : 846–850. [DOI] [PubMed] [Google Scholar]
- 17. Woolf SH, Di Guiseppi CG, Atkins D, Kamerow DB. Developing evidence‐based clinical practice guidelines: lessons learned by the US Preventive Services Task Force. Annual Review of Public Health, 1996; 17 : 511–538. [DOI] [PubMed] [Google Scholar]
- 18. Irwig L & Glasziou P. Implementing honesty about screening using community informed consent (letter). British Medical Journal, 2000; 321 : 450–450. [PMC free article] [PubMed] [Google Scholar]
- 19. Hiller EH, Landenburger G, Natowicz MR. Public participation in medical policy‐making and the status of consumer autonomy: the example of newborn‐screening programs in the United States. American Journal of Public Health, 1997; 87 : 1280–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Entwistle V. Developing research‐based information: creativity or compromise? Health Expectations, 2000; 3 : 87–89.DOI: 10.1046/j.1369-6513.2000.00094.x 11281915 [Google Scholar]
- 21. Austoker J. Gaining informed consent for screening is difficult but many misconceptions need to be undone. British Medical Journal, 1999; 319 : 722–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith DK, Shaw RW, Marteau TM. Informed consent to undergo serum screening for Down syndrome: the gap between policy and practice. British Medical Journal, 1994; 309 : 776–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Al‐Jader LN, Parry Langdon N, Smith RJ. Survey of attitudes of pregnant women towards Down syndrome screening. Prenatal Diagnosis, 2000; 20 : 23–29.DOI: 10.1002/(sici)1097-0223(200001)20:1<23::aid-pd746>3.3.co;2-k [DOI] [PubMed] [Google Scholar]
- 24. Petticrew MP, Sowden AJ, Lister‐Sharp D, Wright K. False‐negative results in screening programmes: systematic review of impact and implications. Health Technology Assessment, 2000; 4. [PubMed] [Google Scholar]
- 25. Cockburn J, Staples M, Hurley S, De Juise T. Psychological costs of screening mamography. Journal of Medical Screening, 1994; 1 : 7–12. [DOI] [PubMed] [Google Scholar]
- 26. Parker M. The ethics of evidence‐based patient choice. Health Expectations, 2001; 4 : 87–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Molenaar S, Sprangers MAG, Postma‐Schuit FCE et al Feasibility and effects of decision aids. Medical Decision-making, 2000; 20 : 112–127. [DOI] [PubMed] [Google Scholar]
- 28. Oliver S, Rajan L, Turner H et al Informed choice for users of health services: views on ultrasonography leaflets of women in early pregnancy, midwives and ultrasonographers. British Medical Journal, 1996; 313 : 1251–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Holmes‐Rovner M, Valade D, Orlowski C, Draus C, Nabozny‐Valerio B, Keiser S. Implementing shared decision‐making in routine practice: barriers and opportunities. Health Expectations, 2000; 3 : 182–191.DOI: 10.1046/j.1369-6513.2000.00093.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Entwistle VA, Watt IS, Davis H, Dickson R, Pickard D, Rosser J. Developing information materials to present the findings of technology assessments to consumers: the experience of the NHS Centre for Reviews and Dissemination. International Journal of Technology Assessment in Health-care, 1998; 14 : 47–70. [DOI] [PubMed] [Google Scholar]
- 31. Stewart‐Brown S & Farmer A. Screening could seriously damage your health. British Medical Journal, 1997; 314 : 533–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Entwistle V, Sowden A, Watt I. Evaluating interventions to promote patient involvement in decision‐making: by what criteria should effectiveness be judged? Journal of Health Services Research and Policy, 1998; 3 : 100–107. [DOI] [PubMed] [Google Scholar]


