Abstract
Objectives To explore the sources of patients’ knowledge about the potential side‐effects of oral steroids prescribed to treat asthma.
Methods Seventeen in‐depth interviews were conducted with patients taking prescribed oral steroid medication (prednisolone) for asthma. The interviews were transcribed verbatim and the data organized according to common themes.
Results All the respondents acknowledged they had no choice but to take oral steroids but they wanted to be informed about the potential side‐effects. Respondents reported that they had not received sufficient information about side‐effects from their general practitioner (GP). Information was sought from both medical sources (pharmacists and asthma nurses) and non‐medical sources (friends and family, self‐help groups and the media) to supplement their knowledge. The conclusions drawn about the risks of taking oral steroids were also influenced by respondents’ existing beliefs.
Conclusions Respondents drew upon information about oral steroids from a variety of professional and lay sources. The findings add weight to calls for doctors and patients to share their respective knowledge in consultations. Developing an understanding of the views of GPs about the provision of information about side‐effects would help to identify any perceived barriers to a more open exchange of information in the consultation.
Keywords: asthma, information about drugs, oral steroids, patient beliefs about medicine, side‐effects
Introduction
Increasing knowledge about modern medicine, declining deference to experts, changing attitudes of doctors, and changing patterns of morbidity, may be modifying patients’ expectations about consultations with their general practitioner (GP). 1 Pressure on GPs to make the consultation less of an encounter between the expert professional and the uninformed patient comes from recent legislative changes, 2 , 3 an increasing interest in alternative therapies, 4 a growth in the number of self‐help groups, 5 and the critical analysis of issues around health and illness by the media. 6 Moreover, the recent proliferation of home computers and access to the Internet provides access to a vast amount of information about medicines. In this changing social climate it might be expected that patients are likely to be informed about their medicine from both medical and non‐medical sources and that this may affect their medicine taking.
As recently as 1995, Makoul et al. 7 reported that in over two thirds of the consultations they had studied no mention was made by either the patient or the physician of side‐effects, risks and precautions. This suggests that despite the conclusions of previous studies that people want more information about their medicines, in particular information about side‐effects, 8 , 9 such information may still not be provided in practice. Explanations for the failure to discuss side‐effects in consultations have focused on the behaviour of both practitioners and patients. It has been suggested that practitioners are reluctant to provide information about side‐effects, 10 and that patients are reluctance to ask. 11 , 12, –13 This issue is further complicated by the idea that people may be given more information in the consultation than they report receiving when questioned afterwards. 14
We were interested in how patients acquire and use information about medicines. In order to provide a focus to this broadly based subject, we decided to restrict this study to patients with asthma who had been prescribed oral steroids. Asthma and oral steroids were chosen because information about both is available from a variety of lay sources. Whilst the results reported here relate to patients’ accounts of being prescribed oral steroids, the findings have wider implications concerning patients’ perceptions of the availability of information about medicines and in particular the role of the GP as a provider of information about the effects of prescribed medication.
Methods
The sample
After obtaining ethical approval, respondents were recruited from a convenience sample of four general practice surgeries in Derbyshire. All were group practices and ran asthma clinics. A random sample of 10 patients from each practice was drawn from a list of patients who were over 18, had been diagnosed with asthma and had also been prescribed oral steroids (prednisolone) in the previous month. Ten letters were sent from each practice explaining the study and inviting the selected patients to participate. The reply slip was addressed to the researcher.
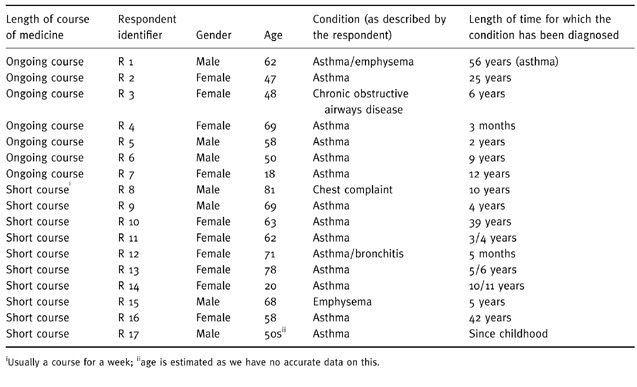
Seventeen patients agreed to participate. The GPs were unaware of which patients took part and patients were assured that their responses would be confidential. The final sample comprised 10 woman and seven men. Respondents ranged in age from 18 to 81. They had been diagnosed with asthma, and in some cases a related condition, for between 3 months and 56 years. Table 1 presents the sample in terms of gender, age and length of diagnosis. Ten of the respondents had been prescribed short courses of oral steroids for an acute exacerbation of their asthma, and seven had been prescribed an ongoing course of low dose oral steroids in order to control their symptoms. The sample included patients prescribed both ongoing and short‐term courses of steroids. This was due to the fact that development of side‐effects differs according to the length and strength of the course prescribed and the length of treatment may also influence patients’ perceptions of both their medical condition, and their medication. The sampling strategy meant it was possible to gain insights from patients with a variety of demographic characteristics, degree of severity of illness and experience with treatment for asthma.
Table 1.
The demographic characteristics of respondents
The interviews
In‐depth interviews were conducted with the 17 patients in their own homes during the summer and autumn of 1994. Each patient completed a consent form and all agreed to the interview being tape recorded. This method has been used in other studies about the experiences of people with chronic conditions, such as asthma. 15
Respondents were informed that the researcher was not medically trained and were encouraged to talk about their medicines and their knowledge of their medicines in their own terms. Although we were interested in knowledge about side‐ effects, this was not asked about directly for fear of worrying respondents. Respondents were asked about any medicine they took and when it had first been prescribed. They were also asked how they felt about the medicine, the information they had about the medicine and the source of that information. Prompts were used to explore whether respondents recalled receiving information from friends and family or the media, and whether they belonged to a support group. Respondents were also asked if they were aware of any particular problems with the medicine and if so at what stage, and how, they had been alerted to these problems. They were also asked about their relationship with their GP and about the experience of being prescribed oral steroids. Throughout the interview, respondents were encouraged to talk about their condition and how the medicines used to control it affected their life.
Analysis
Each respondent’s individual medical career was constructed from verbatim transcripts and fieldnotes. The interview transcripts were analysed using the technique of charting, which involved selecting and reorganizing the responses according to themes. 16 Themes were identified in repeated close scrutiny of the transcripts by the first author (FS) and refined in discussions with the other authors.
Results and discussion
Two main themes emerged. The first concerned patients’ perceptions of the necessity for their treatment, and their experiences of oral steroid medicine. The second theme concerned the variations in the extent to which respondents wanted to take control or be involved in and understand, their treatment. As we were concerned with the sources from which respondents had gained information, rather than their actual knowledge about their medicine, the first theme provided a context that enabled a deeper understanding of the issues raised to be developed within the second theme.
The necessity for treatment and the experience of side‐effects
Unsurprisingly, given that oral steroids are only prescribed in asthma when the symptoms are severe and potentially life threatening, all of the informants noted the efficacy of the prescribed medicine and felt they had no choice but to take it, regardless of any side‐effects. This was summed up by the comment made by a 50‐year‐old man who had suffered with asthma for 9 years. He said:
It’s [taking oral steroids] the best of two evils (R 6).
Our findings supported Britten’s 17 observations of both positive and negative orientations to the taking of medicines. Although all our respondents acknowledged the efficacy of oral steroids, concerns about addiction and the desire not to take any medicine unless it was really necessary were also expressed. One woman compared her attitude with those of ‘other’ people and said:
I just take things when I need them, but otherwise I’ve always been a bit anti drug and pill. You know some people love to tell you how many pills they’re on and shake the bottle and show you, but I’d rather be able to say very proudly no I don’t take anything, because then I would feel one hundred per cent for it (R 13).
Potential side‐effects of oral steroids include: a false sense of well‐being, increased appetite, indigestion, nervousness or restlessness, and trouble in sleeping, filling or rounding out of the face, muscle cramps or pain, nausea or vomiting, pain in the back, hips, ribs, arms, shoulders, or legs, swelling of feet or lower legs, thin, shiny skin, unusual bruising, unusual tiredness or weakness, and unusual weight gain. 18 Each of these symptoms was reported by at least one respondent, although this cannot be taken to mean that these symptoms had necessarily been caused through taking oral steroids. Fears were also expressed about osteoporosis, another potential side‐effect.
Involvement in, and understanding, treatment
The extent to which people want information
Only four of the 17 respondents said they did not know much about their medicines, or had not bothered to get any information. Interestingly this included the two youngest people in the sample (R 7 and R 14) who were 18 and 20 years of age, respectively. It may have been expected, given their ages, that they would be interested in the long term effects of taking oral steroids.
Information from the medical consultation
Eight out of the 17 respondents reported that they were happy to rely on the judgement and expertise of their doctor, but this cannot be taken to imply that they did not want to be informed about their medicines. In three of these cases respondents discussed how the potential for side‐effects had been referred to in only a general way by their GP. Phrases such as, ‘the good outweighs the side‐effects’ (R 5) and, ‘we don’t want any side‐effects’ (R 15) were recalled as explanations for the dosage and length of treatment. The following example illustrates how generalized references to the possibility of side‐effects may generate concerns. A 69‐year‐old woman who had recently developed asthma following pneumonia reported being told by her GP that she would not be on the medicine long enough to develop any side‐effects. This comment had made her anxious to stop taking oral steroids as soon as possible:
They reckon you’ve got to be on them quite a while before side‐effects really take place, um well I’m trying to get me doctor to wean me off them before it happens (R 4).
Five respondents recounted asking their GP explicitly for information, and were critical about the experience. Their specific complaint was that the information that was provided did not contain sufficient detail. One respondent described his strategy of repeating requests for information until he was satisfied:
Well, every time I go down to the doctors I’m asking questions er if I want to know something I ask, if they want to answer me they’ll answer me if they don’t, they don’t, but I’ll only ask again so they might as well let me know the first time (R 5).
Two of the respondents said they had specifically requested information on side‐effects but both indicated they felt that their GP had not satisfied their requests. In one case the GP concerned had raised the possibility of weight gain, but failed to elaborate any further. However, the respondent’s wife had previously been prescribed oral steroids, so he was aware there were other side‐effects and suspected his GP was withholding important details:
…since I’ve been on them, I don’t know whether it’s just coincidence or, I know I’ve different bones really aching and cracking, and God knows what. I don’t know what to put it down to, whether it’s age or…
Have you thought about asking your doctor?
I’ve asked him and he says could be your age, you know, he kind of brushed it off […] I don’t like asking for too many of these tablets if there is side‐effects, you know. I would like to know what the side‐effects was of them really (R 17).
The respondent who reported experiencing the most side‐effects had been taking oral steroids, on and off, for the past 25 years. She reported hair loss, ulcers, bruising and pains in her limbs. She said she had received no warning about these side‐effects and although she had asked the doctors, they had not answered her queries:
I’ve virtually had to find out about all the side‐effects myself (R 2).
She continued:
Well I’ve asked before but I’ve not a reply and sometimes they don’t answer you or they just sort of pooh pooh you off, why I don’t know (R 2).
This case demonstrates how failure to provide relevant information may affect the doctor‐patient relationship. This patient believed that information about potential side‐effects was being deliberately withheld and she did not understand why:
Unless they think you’re going to jump out the window or something, or what… But I mean I’ve put up with it for 25 years so…(R 2).
Another respondent said that although she felt she had no choice but to trust the doctor, she was teased in the practice about the number of questions she asked:
I’d rather know than not know. Doctor down the road calls me Dr C. (laughter) (R 3).
This example suggests questions may not always be welcome.
These cases all concern people who were not satisfied with the information they got when they asked questions. Of even more concern was a respondent who said that she did not even feel she had the opportunity to ask:
Sometimes you don’t have time to ask, you know. They’ve written the prescription before you’ve had time really (R 10).
She also described her experience when last prescribed oral steroids. She said she had indicated that she was not happy about the prescribing decision, yet her concerns were not explored. This illustrates how patients who are open about their concerns may have their questions or doubts ignored:
I went down the other week and he said, ‘oh now I’m going to put you on a course of steroids’ and I said ‘oh’, and he said ‘what for you mean oh’ and I said ‘I wasn’t too happy’ but he said ‘you’ll be a new woman in a few days’, which I was. (R 10).
When asked by the researcher to say more about her concerns she stressed that she had taken the medicine as prescribed and her symptoms had been relieved. GPs may rely on the therapeutic effects of oral steroids to outweigh their patients’ misgivings. However, such a strategy relies on patients overcoming their misgivings in order to try the medicine. In addition, failure to take account of patients’ concerns may damage the therapeutic relationship.
Only one respondent (R 1) reported that all the information he wanted had been volunteered to his satisfaction. Yet we need to be aware that people whose queries are resolved without question may not recall the experience as readily as those who have experienced problems and as Stimson and Webb 19 noted, it also might be the case that stories of criticism make more interesting telling than those of praise.
Other health care professionals as information providers
The development of specialist nurses for asthma, and increasing emphasis on pharmacists as a source of information about medicines, means that health care professionals, other than doctors, may play a part in the medical care of patients with asthma. Five out of the 17 respondents reported discussing their medicines with practice nurses and pharmacists. One reported asking both the pharmacist and the asthma nurse for information. Three other respondents discussed asking the pharmacist about their medicines, and another said they contacted the asthma nurse if they had any problems. The extent to which people use pharmacists and nurses as sources of information is likely to vary according to, for example, whether they generally use the same pharmacy and thus are able to build up a relationship with a local pharmacist, and their attendance at nurse‐run asthma clinics.
The influence of friends and family in the provision of information
The influence of friends and family in help‐seeking behaviour has been noted elsewhere, 20 , 21 as has the influence of such networks in making decisions about treatment. 19 In our study two respondents reported that their daughters, who were nurses, provided them with information. Interestingly they reacted differently to this information. One respondent said her daughter had asked the doctor with whom she worked about the effects of prednisolone (oral steroids):
She was very interested as well and she found out a lot of information about that sort of thing, leaflets and stuff (R 3).
However, another respondent did not seem very interested in the information his daughter could supply, although his wife was interested. The following exchange demonstrates his wife’s interest and his lack of interest:
Wife: It can cause all kinds of things. J [daughter who is a nurse] understands it, I mean she does know different things don’t she about this but er.
Researcher: Has she told you a bit about it then?
Respondent: No, not really, never asked (R 15).
Contact with other patients in hospital was also a prime source of information, yet once again people had different views about this. Respondent 1 said he thought he had learnt about the risk of damage to his bones from a fellow patient whilst he was in hospital, however he was not particularly worried about this and tried to be philosophical about the possible side‐effects. In contrast, one respondent (R 2), was upset to have found out about side‐effects from other patients rather than her doctor. She said:
Well, I mean, I’ve been taking it all these years, no‐one said to me initially, this was the bit that really gets me, no‐one when I first took it said to me it’s got side‐effects, I mean I’ve virtually had to find all the side‐effects out myself, just through talking to people when I’ve been in hospital, whenever (R 2).
Self‐help groups
Self‐help groups offer both information, and mutual support, much of it through the opportunity to meet other sufferers and sometimes carers. Only one respondent in this sample reported attending meetings of the Campaign for Asthma. He thought this was a very good resource. He said:
I believe a lot in asthma society [Campaign for Asthma], it gives you full information and we have regular meetings at [name] hospital with speakers who demonstrate um nebulisers, who talk about various medications so you get the full facts, and you’re able then, a lot of them are from the manufactures you see and you are able to ask the manufactures what the side‐effects are if any and that (R 1).
One respondent (R 3) reported requesting information, but had not joined a group. Another (R 2) said she was considering writing to an address she had seen in the newspaper for a support group for people who had taken, or were taking, oral steroids. She had recently visited a stall set up in the shopping centre to give information about asthma but had been disappointed because she felt she knew more about asthma than the woman staffing it:
I got talking to the woman but she didn’t seem to know, you know I think I knew more about it than she did, the woman that was there. She couldn’t give me any sort of more information (R 2).
Groups such as the Campaign for Asthma offer both information and support. The respondents in our study were interested in the information such organizations offer, but did not seek formal membership, suggesting they had less interest in the ‘support’ component.
The media
The mass media is commonly acknowledged as a major vehicle for communicating health risks. 22 Moreover, they may focus on specific conditions, such as asthma, particularly when a new treatment is announced or there is a related tragedy.
All our respondents were asked whether they had gained any information about their medicines or their condition from the media. We found that people were aware of information from newspapers, the radio and television, however, the media was not seen as important a source of information as personal and professional contacts.
Only one respondent appeared to use newspapers as a main source of information and she had collected a wide range of newspaper and magazine articles. However, she was sceptical of some of the information provided:
Well, if you take it half and half, I mean don’t believe newspapers, it’s just out to sell your paper, that’s all it is. But there must be some sort of an inkling of truth else they’re liable aren’t they (R 3).
Comments by respondents such as, ‘the truth isn’t always interesting’ (R 10), and, ‘a little knowledge can be a dangerous thing’ (R 1), suggested a more general scepticism. The following comments from respondents suggested that the information provided by newspapers might be of limited relevance for long‐term asthma sufferers:
Well, you do see things on newspapers, but I mean in newspapers they only tell you things you already know. If you’ve had asthma 11 years and you only see in newspaper what you already know, nine times out of 10 anyway (R 6).
and
Very often you get an article about it [asthma], yes I do read it a bit, but I don’t think I gain any further information than I’ve already received (R 13).
Yet there was general agreement that information presented in newspapers, especially publicity about campaigns such as National Asthma Week, was worthwhile. Particularly as this was seen to increase knowledge about asthma within the general population.
Radio or television programmes often analyse specific health conditions and question the way they are treated. A few days before the penultimate respondent was interviewed a programme outlining the possible side‐effects of oral steroids was broadcast on television. 23 The respondent reported asking her GP about the side‐effects presented on the programme. Since taking oral steroids she had gained weight and had learned from the programme that this was a possible side‐effect. Her GP said that she should already have been told about the risk of weight gain. She was pleased that she now had established an explanation for her weight gain and in the absence of any dietary advice from her doctor, developed her own solution and reported reducing the number of biscuits she ate. She had also learned from the programme that taking oral steroids might damage her bones. She was more concerned about this than she was about the weight gain. She reported that her GP had told her she did not have any bone damage.
In the interview she appeared satisfied with her GP’s response, but we would note that in her account her GP appeared not to have discussed the possibility of problems with her bones in the future if she continued to take oral steroids. She repeated his reassurance that her recent X‐ray, for a different problem, had not indicated any problem. She appeared unaware of any future prognosis. She accounted for her own lack of serious side‐effects by developing a belief that the people featured on the television programme had something other than just asthma wrong with them:
She was in a wheel chair [the person appearing in the television programme] and I thought, ‘ooh’, you know, [...] I thought ‘well is there something else wrong with her as well’, and there was another lady she’d got her neck in a collar and she said, ‘well look at me I’m dying through taking them’, I thought, ‘ooh crikey’ but as I say if it had gone into more detail, the programme, probably there was something else wrong with them people besides they had asthma and they were on this medicine [oral steroids] (R 16).
Whilst this case illustrates the way in which people interpret the information they receive to fit with their own experiences and beliefs, it also provides an example of a GP appearing to avoid addressing a patient’s specific concerns. The patient was left to develop her own explanation as to why she had not developed the more serious side‐effects outlined in the programme.
Making sense of experience: patients’ construction of beliefs
In the conclusion to their edited volume about lay perspectives, Williams & Calnan 24 emphasized the complexity and diversity of people’s beliefs and attitudes towards medicine and medical care. In our study we identified a range of beliefs about medicine which were based on people’s own experiences and their observations of the experiences of other people.
Two respondents reported similar negative experiences with tranquillisers, yet they differed in their interpretation. One blamed the doctor who had prescribed them but did not generalize the experience beyond the event. He remained positive about his current use of medicines, including prednisiolone, because he trusted the health care professionals he currently consulted:
I have enough confidence in the people I’m working with now to know that if there is going to be anything untoward I’ll be told about it (R 1).
The other respondent said her experience of tranquillisers had made her more likely to question the GP, and to avoid taking medicines if possible:
But when I was taking these tranquillisers and such like I had all sorts of side‐effects and [he] just gave me one to counter the other all the time. I was just taking far too much I think. But I did used to think well the doctor knows best and take everything, but now I tend to question a bit (R 10).
Adams et al. 1997 25 illustrated how people with asthma judge their own symptoms with reference to other people so diagnosed. This was true in our study both for respondents’ perceptions of their condition and for potential side‐effects of oral steroids. Concerns about weight gain were specifically expressed. Four respondents, with no weight gain themselves, expressed a fear of it based on their observation of other people, and a concern that it might still happen to them. One woman said:
A friend of mines was on them, she lives in the village. I’ll admit they have put weight on her, she’s blown up like a balloon, you know she’s got ever so fat (R 4).
Although she had not gained any weight, she was anxious to stop taking the medicine before it happened. Commonly, those with the option argued for taking as little medicine as possible for as short a time as possible. These findings are reminiscent of Osman’s 26 work that highlighted a distrust of taking long‐term medicine amongst people with asthma.
Conrad 27 argued that people alter their medicine taking as a way of asserting control over their disorder. In our study, all the respondents expressed the view that they had no choice but to take oral steroids, yet even those who suggested they had no concerns about their medicine described strategies they used to exert some control. For example, one respondent who reported taking his medicine as directed believed that his ulcer would cause him ‘problems’ if he took ‘too much’. He saw his ulcer as ‘an early warning system’ that would stop him taking sufficient steroids to develop side‐effects:
It don’t worry me because I know for certain if I have too many I’m going to start ulcer blowing up, so I’m going to keep them down as low as possible (R 15).
The way in which individuals make sense of the information they have and their experiences varies widely, but in each case respondents found their own way of rationalizing what was happening to them. For example, concerns are often expressed by GPs that people may confuse prescribed corticoid steroids with illegal anabolic steroids taken by athletes. In the following case the respondent came to his own conclusions based on the way the medicine worked on his body. This might be perceived by patients as a more accurate indicator than information from any other source:
Athletes take steroids of a sort don’t they? Builds up muscle. Look at me I’m shrinking [...] These, there must be several sorts of steroid. These expand the air passages, makes it better for me [...] I’ve seen people on steroids and their face has been blown up like balloons [...] but it doesn’t do that with me. I don’t know whether it’s a different kind of steroid or not, I don’t know (R 9).
Conclusions
These findings demonstrate a range of responses by patients both in terms of their desire for information and their interpretation of both experiences and information. All the respondents had severe medical problems and acknowledged that they had little choice about whether or not to take oral steroids. They reported receiving information about side‐effects from a range of sources. The findings not only support the conclusions of other studies that patients would like more information about the side‐effects of medicines than they currently receive, 8 , 9 but also suggest that patients prefer information about side‐effects to be provided in advance rather than after side‐effects have developed.
It is possible that GPs are unaware of the availability and influence of sources of information outside of the consultation. These sources proved particularly important when patients did not believe they had received the information they required from their GP. The accounts presented here add weight to the argument that both patients and doctors should share their knowledge in consultations. 28 , 29 Generally GPs do not appear to be addressing patients’ concerns adequately or to be taking account of their beliefs and experiences. The finding of Boreham & Gibson 11 of 20 years ago, that patients have surprisingly little knowledge following consultations despite attaching considerable importance to the acquisition of this knowledge, was also true in our sample.
The findings presented in this paper parallel those from studies that have focused on other conditions and medicines. The issues raised could be further informed by research that focuses on what happens between GPs and patients in the consultation. Moreover, developing an understanding of the views of GPs about the provision of information about side‐effects would help to identify any perceived barriers to a more open exchange of information in the consultation. As only five of the 17 respondents reported consulting their asthma nurse or pharmacist for information, the potential role and possible integration of other health care professionals, could also be explored. Research into strategies for improving communication between health care professionals and patients is important as communication problems may have potentially damaging consequences for patients’ health.
Acknowledgements
This research was conducted whilst the first author was a Research Student at the Medicines Research Unit, School of Health and Community Studies, University of Derby. We wish to acknowledge the help of all the practices and patients involved in the research and Dr Sheila Greenfield for her helpful comments on an earlier draft of this paper. We also wish to acknowledge the constructive comments of two anonymous referees.
References
- 1. Elston MA. The politics of professional power: medicine in a changing health service. In: Gabe J, Calnan M, Bury M (eds). The Sociology of the Health Service. London: Routledge, 1991: 58–88.
- 2. Department of Health . The Patient’s Charter London: HMSO, 1991.
- 3. Anony . Patient pack prescribing and the provision of patient information leaflets. Drug and Therapeutics Bulletin, 1995; 33: 86 88. [DOI] [PubMed] [Google Scholar]
- 4. Murray J & Shepherd S. Alternative or additional medicine? An exploratory study in general practice. Social Science and Medicine, 1993; 37: 983 988. [DOI] [PubMed] [Google Scholar]
- 5. Kelleher DJ. Do self‐help groups help? International Disability Studies, 1990; 12: 66 69. [DOI] [PubMed] [Google Scholar]
- 6. Karpf A. Doctoring The Media, The Reporting of Health and Illness. London: Routledge, 1988.
- 7. Makoul G, Arntson P, Schofield T. Health promotion in primary care: physician‐patient communication and decision making about prescription medications. Social Science and Medicine, 1995; 41: 1241 1254. [DOI] [PubMed] [Google Scholar]
- 8. Ridout S, Waters WE, George CF. Knowledge of and attitudes to medicines in the Southampton community. British Journal of Clinical Pharmacy, 1986; 21: 701 712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Keown C, Slovic P, Lichtenstein S. Attitudes of physicians, pharmacists and laypersons towards seriousness and need for disclosures of prescription drug side effects. Health Psychology, 1984; 3: 1 11. [DOI] [PubMed] [Google Scholar]
- 10. Lamb G, Green SS, Heron J. Can physicians warn patients of potential side effects without fear of causing those side effects. Archives of Internal Medicine, 1994; 154: 2753 2756. [DOI] [PubMed] [Google Scholar]
- 11. Boreham P & Gibson D. The informative process in private medical consultations: a preliminary investigation. Social Science and Medicine, 1978; 12: 409 416. [PubMed] [Google Scholar]
- 12. Collier J. The Health Conspiracy. London: Century, 1989.
- 13. Frederickson LG & Bull PE. Evaluation of a patient education leaflet designed to improve communication in medical consultations. Patient Education and Counselling, 1995; 25: 51 57. [DOI] [PubMed] [Google Scholar]
- 14. Ley P. Communicating with Patients. London: Croom Helm, 1988.
- 15. Snadden D & Brown JB. The experience of asthma. Social Science and Medicine, 1992; 34: 1351 1361. [DOI] [PubMed] [Google Scholar]
- 16. Bryman A & Burgess RG. Analysing Qualitative Data. London: Routledge, 1994.
- 17. Britten N. Patients’ ideas about medicines: a qualitative study in a general practice population. British Journal of General Practice, 1994; 44: 465 468. [PMC free article] [PubMed] [Google Scholar]
- 18. British National Formulary 33 . London: BMA and RPSGB, 1997.
- 19. Stimson G & Webb B. Going to See the Doctor London: Routledge, 1975.
- 20. Freidson E. Patients’ View of Medical Practice. New York: Russell Sage Foundation, 1961.
- 21. Pescosolido B, Gardner CB, Lubell KM. How people get into mental health services: stories of choice, coercion and ‘muddling through’ from ‘first timers’. Social Science and Medicine, 1998; 46: 275 286. [DOI] [PubMed] [Google Scholar]
- 22. Nelkin D. Communicating technological risk: the social construction of risk perception. Annual Review of Public Health, 1989; 10: 95 113. [DOI] [PubMed] [Google Scholar]
- 23. BBC . Here and Now (television broadcast). London: BBC, Broadcasting House, 23rd November 1994.
- 24. Williams SJ & Calnan M. Modern Medicine: Lay Perspectives and Experiences London: UCL Press, 1996.
- 25. Adams S, Pill R, Jones A. Medication, chronic illness and identity: the perspective of people with asthma. Social Science and Medicine, 1997; 45: 189 201. [DOI] [PubMed] [Google Scholar]
- 26. Osman LM, Russell IT, Friend JAR et al. Predicting patient attitudes to asthma medication. Thorax, 1993; 48: 827 830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Conrad P. The meaning of medications: another look at compliance. Social Science and Medicine, 1985; 20: 29 37. [DOI] [PubMed] [Google Scholar]
- 28. Charles C, Gafni A, Whelan T. Shared decision‐making in the medical encounter. What does it mean? (or it takes at least two to tango). Social Science and Medicine, 1997; 44: 681 692. [DOI] [PubMed] [Google Scholar]
- 29. Tuckett D, Boulton M, Olson C, Williams A. Meetings Between Experts London: Tavistock, 1985.


