Abstract
Objective To review trials of the effectiveness of interventions aimed at improving communication between health professionals and women in maternity care.
Search strategy The electronic databases Medline, PsycLit, The Cochrane Library, BIDS Science and Social Science Indexes, Cinahl and Embase were searched. Final searches were carried out in April 2000.
Inclusion criteria Controlled trials of interventions explicitly aimed at improving communication between health professionals and women in maternity care were included. Other trials were included where two reviewers agreed that this was at least part of the aim.
Data extraction and synthesis 95 potentially eligible papers were identified, read by one reviewer and checked against the inclusion criteria. The 11 included trials were read, assessed for quality and summarized in a structured tabular form.
Results The included trials evaluated interventions to improve the presentation of information about antenatal testing, to promote informed choice in maternity care, woman‐held maternity records and computer‐based history taking. Four trials in which women were provided with extra information about antenatal testing in a variety of formats suggested that this was valued by women and may reduce anxiety. Communication skills training for midwives and doctors improved their information giving about antenatal tests. The three trials of woman‐held maternity records suggested that these increase women's involvement in and control over their care.
Conclusions The trials identified by this review addressed limited aspects of communication and focused solely on antenatal care. Further research is required in several areas, including trials of communication skills training for health professionals in maternity care and other interventions to improve communication during labour and in the postnatal period.
Keywords: communication, maternal health services, review
Introduction
Communication in health‐care, particularly between health‐care professionals and patients, has attracted an increasing amount of attention at official and professional levels in recent years. The Department of Health, the royal colleges 1 , 2 and other statutory bodies have all been involved in initiatives to promote good communication and to improve record keeping. Guidance from the General Medical Council on undergraduate medical education places communication skills training at the heart of the curriculum 3 although the extent of compliance with these recommendations is variable. 4 More recently, in the NHS Plan, the Department of Health announced plans for new training in communication skills across all professions in the NHS. 5 These initiatives are in part a response to increasing evidence from researchers that the quality of the interaction between patients and their carers may have a significant effect on a variety of aspects of patient well being. 6 , 7 These include satisfaction, knowledge and understanding, compliance with advice or treatment, quality of life, and psychological and other health outcomes.
Maternity care is an area of health‐care in which the importance of good communication has received particular attention. Changing Childbirth, the report of the Expert Maternity Group, commissioned in 1992 by the Department of Health to review maternity care in England and Wales, highlighted the importance of good communication and recognized that in many cases communication is not as good as it should be. 8 A separate volume outlined the principles of good communication and detailed examples of good communication practice. 9
Studies of women's views of maternity care suggest that good communication is central in determining whether women are satisfied with the care that they receive. 10 , 11 The specific additional challenge for communication in maternity and perinatal care is that, because care is required for both mother and baby, a much wider group of health professionals may be involved than in many other areas of health‐care. Before discussing how to improve communication in maternity care, however, we need to know what we mean by communication.
In Changing Childbirth, the provision of appropriate and accessible information was recognized as an important aspect of communication. 8 Good communication was explored further in the accompanying volume 9 where it was made clear that listening to women's preferences and concerns is also central. Changing Childbirth was explicit in recognizing that `there is no template for effective communication' and good communication will always be difficult to define, but studies of women's views of maternity care support the idea that good communication is essentially a two‐way process. Clear and readily available information is important to women, and is a good first step in communicating, but women also highlight the importance of staff listening to them and responding to their individual needs. 10 , 12 Observational studies of communication between midwives and women during labour have highlighted the misunderstandings that can occur when communication is poor at this time and identified areas where communication could be improved. 13 , 14 In particular, this work has drawn attention to ways in which women's requests for information or expressions of concern may be ignored or diverted, often with false reassurance.
Reviews of doctor‐patient communication confirm that communication involves much more than giving or receiving information. In a review of the effect of doctor‐patient communication on patient outcomes, interventions that encouraged doctors to share decision‐making or that increased patients' information‐seeking skills and involvement in the consultation, resulted in improved psychological and other health outcomes. 7 In another review of research on doctor‐patient communication, information exchange was highlighted as one purpose of medical communication with two further purposes, creating a good interpersonal relationship and medical decision‐making, added. 6 These aspects also find some resonance in research into women's views of maternity care. Women often relate good communication to having a smaller number of caregivers, being able to build relationships over time with their caregivers and being involved in decisions about their care. 10 , 11
Despite the acknowledged importance of communication in maternity care, and the official recognition that communication is not always as good as it should be, 8 there have been few evaluations of strategies to improve communication between women and their carers. Previous reviews of doctor‐patient communication have not included any studies carried out in maternity care. 6 , 7 , 15 , 16
Our objective was to identify and review trials of the effectiveness of interventions aimed at improving communication between health professionals and women in maternity care. The purposes of communication already defined in a review of the subject 6 were used as a framework with which to assess whether improved communication was an implicit aim or aspect of the intervention. For example, while evaluations of information leaflets for women might not include improving communication as an explicit aim, they were generally considered by us to be eligible for inclusion in the review since `information exchange' is one purpose of communication. Using these criteria, trials of other interventions where improved communication was judged by us to be at least part of the aim were also eligible for inclusion.
This review is derived from a larger report which was commissioned by the Confidential Enquiry into Stillbirths and Infant Deaths (CESDI). 17 In it we looked at a number of communication issues within the CESDI framework, including the role of poor communication as a contributory factor in stillbirth and infant death. 18
Methods
Inclusion criteria
The review considered randomized and quasi‐randomized controlled trials where improving communication between health professionals and women in maternity care was a stated aim of the intervention for inclusion. Studies in which there was no explicit statement to this effect, but for which two reviewers agreed that this was at least part of the aim, were also included. We were aware of interventions in maternity care that may have the effect of improving women's perceptions of communication with their careers without improved communication ever having been an explicit or implicit aim of the intervention. Changes in the organisation of midwifery services, such as shared care schemes and one‐to‐one midwifery, are a good example of this. 19 Trials like these were not included in the review, partly because of the difficulty of searching for studies using communication as an outcome measure and partly because we judged that in these trials improved communication was often likely to be incidental to the intervention rather than an aim.
Only interventions evaluated in actual clinical practice were eligible for inclusion. Eligible interventions could be targeted at the health professional or the woman. They included, for example, communication skills training for carers or for women, changes to history taking or consultation style, woman‐held maternity records and information leaflets for pregnant women. We were primarily interested in women's health outcomes, including clinical and psychological outcomes. Other more immediate outcomes such as compliance with advice or treatment; knowledge, recall, or understanding of advice or treatment; satisfaction with aspects of care and measures of the process of care were also included. Studies that measured the effect of an intervention on communication skills alone were excluded.
Search methods
Search strategies were devised and run on the following electronic databases to identify studies relevant to this and two related reviews that made up the main report: 17 Medline (from 1966), PsycLit (from 1967), The Cochrane Library, BIDS Science Citation Index and Social Science Citation Index, Cinahl (from 1982), Embase (from 1980). Final searches for the main report were carried out in May 1999 and were updated for this review in April 2000. The Medline search terms used for this review were the text term communicat* and the Medline MeSH terms communication; hospital‐patient relations; interpersonal relations; medical staff, hospital; patient acceptance of health‐care; patient compliance; patient satisfaction; medical history taking; informed consent; consumer satisfaction; medical records; forms and records control; pregnancy; obstetrics; antenatal care; perinatal care; postnatal care; neonatal nursing and labour. No language limits were used for any of the searches.
National Perinatal Epidemiology Unit (NPEU) databases and collections, reference lists of all studies meeting the inclusion criteria and any relevant reviews identified were also searched for further studies. No systematic attempt to identify unpublished studies was made.
Results of the literature search
Abstracts retrieved from the literature searches were checked by one reviewer (RR) and full copies of the 95 papers that appeared to meet the inclusion criteria were obtained. Eleven of these were review articles. The remaining 84 papers were read by one reviewer (RR), checked against the inclusion criteria and classified as included, excluded or uncertain. Studies classified as uncertain were discussed with a second reviewer (JG). This process identified 9 eligible studies. Seventy‐five studies did not meet the inclusion criteria for the review and were excluded. Most of these were trials of interventions to improve communication in settings other than maternity care, uncontrolled studies and descriptive or discussion papers. Two further eligible studies were identified during the publication peer review process. One of these was a study that we knew to be in progress, which reported after submission for publication. The second was drawn to our attention by one of the peer reviewers.
The 11 included studies were read by two reviewers (RR & JG). One of the reviewers (RR) summarized the characteristics and results of each study in consultation with a second reviewer (JG). Methodological quality was assessed independently by two reviewers (RR & JG) on three dimensions: method of randomization and allocation concealment, masking of outcome assessment and the occurrence and handling of participant attrition. 20 Any differences of opinion were resolved by discussion. Studies were not excluded on the basis of methodological quality at this stage. Given the differences in the interventions, settings and outcomes used by the studies a quantitative analysis was not appropriate. The trials were therefore summarized in a structured tabular form, which included the statistical results reported by the authors.
Results
Characteristics of the studies
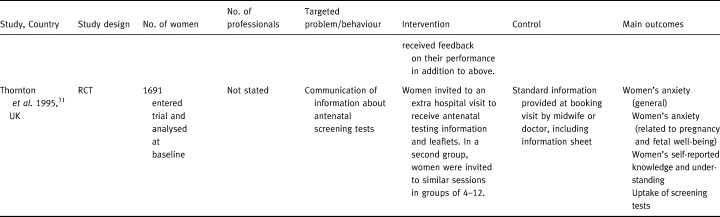
1 2 3 4 5Table 1 summarizes the 11 identified trials of interventions to improve communication in maternity care. 21 , 22, 23, 24, 25, 26, 27, 28, 29, 30, –31 Ten of these were parallel‐group randomized trials focusing on aspects of antenatal care while the 11th 28 was a cluster randomized trial covering information about antenatal and intrapartum care. Five trials were concerned with the presentation of information about antenatal testing. 24 , 27 , 29 , 30, –31 Three trials compared the use of woman‐held maternity records with standard co‐operation cards 22 , 23 , 26 and two compared using a computer‐based questionnaire for history taking at the first antenatal (booking) appointment with different types of manual checklist. 21 , 25 In the remaining trial, staff at maternity units were supplied with evidence‐based leaflets and given training in their use with women. 28 Women's informed choice at these units was compared with women receiving standard care at other units.
Table 1.
Characteristics of studies
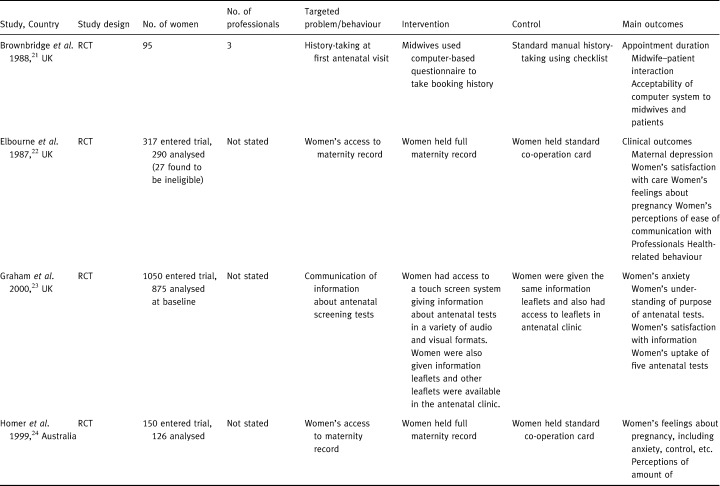
Table 2.
Table 1 (Continued)
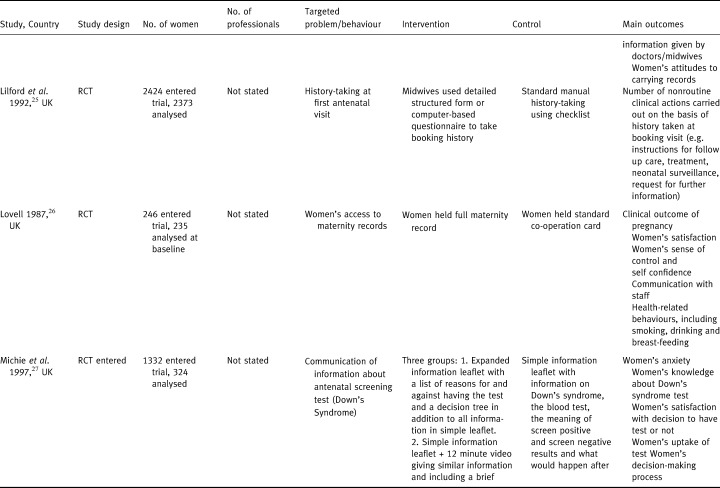
Table 3.
Table 1 (Continued)
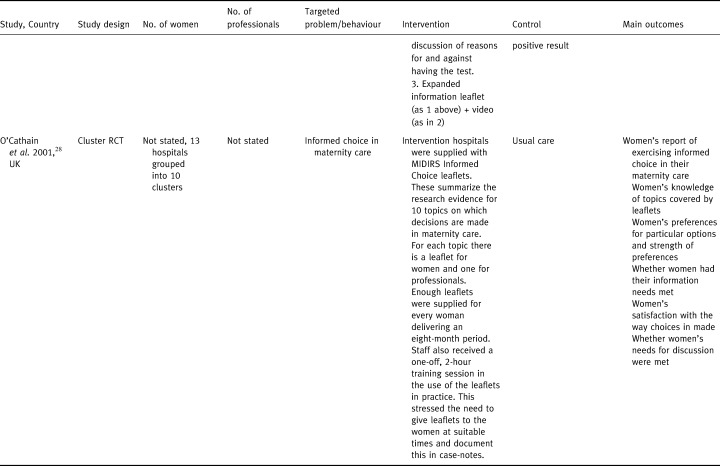
Table 4.
Table 1 (Continued)
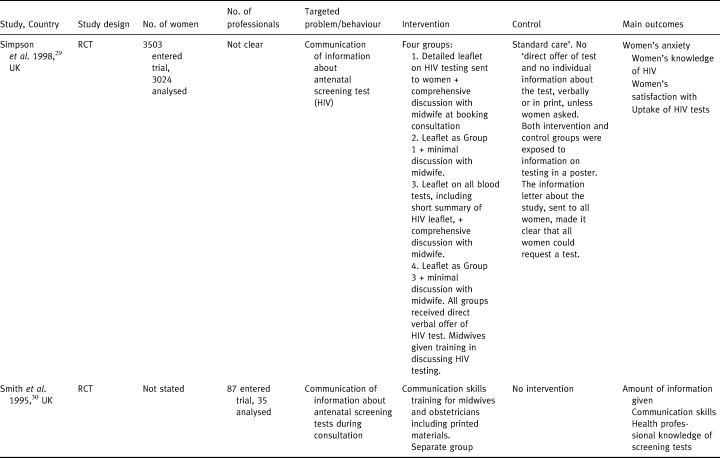
Table 5.
Table 1 (Continued)
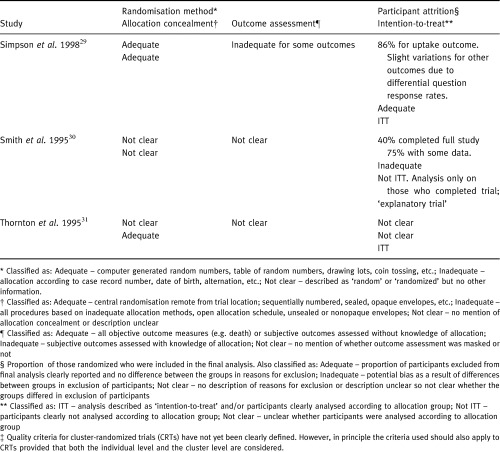
Methodological quality
The quality of the included trials was assessed using three criteria and the results are summarized in 2, 7Table 2. With one or two notable exceptions the reports of these trials were not sufficiently detailed to permit assessment on all our criteria. Most reports gave no information at all about how a random allocation sequence was generated. Based on the information available, only two trials used an acceptable randomization method. 25 , 29 Perhaps surprisingly, more information was provided about the methods used to conceal the allocation sequence from the people enrolling participants. Six trials used an adequate method 22 , 23, –24 , 28 , 29 , 31 ; one was clearly inadequate. 27 Very few trials gave enough information to assess whether outcomes were assessed without knowledge of allocation. In one trial, assessed as adequate on this criterion, outcome assessment was masked for a proportion of cases and compared with cases for which assessment was unmasked and no difference was found. 25 Of the remaining trials, nine did not give sufficient information and one appeared to use unmasked assessment for at least some outcomes. 29 The remaining quality criterion assessed the extent of participant attrition, often referred to as `loss to follow‐up', and how well dropouts and exclusions were handled in the reporting and analysis of the trial. Six trials handled participant attrition in an appropriate way and used intention‐to‐treat analysis. 21 , 23 , 24, –25 , 28 , 29 Two trials were particularly poor in this respect, with a high proportion of participants dropping out or being excluded from the trial and not using intention‐to‐treat analysis. 27 , 30 The remaining trials did not describe the flow of participants through the trial in sufficient detail to assess them using this criterion.
Table 2.
Quality of studies
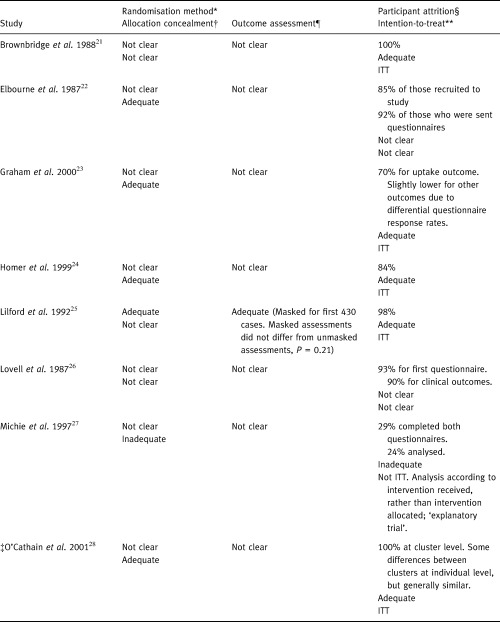
Table 7.
Table 2 (Continued)
Findings
Giving information about antenatal testing
Five trials compared different ways of improving the presentation of information about antenatal screening tests. 24 , 27 , 29 , 30, –31 Their results are summarized in 3, 9Table 3. Three trials looked at many types of antenatal testing, 24 , 30 , 31 one looked at screening for Down's syndrome 27 while the fifth focused on antenatal HIV screening. 29 Four trials evaluated interventions targeted at women, using different strategies for presenting the information given to them, 24 , 27 , 29 , 31 while the fifth focused on improving the presentation skills of the health professionals. 30 The outcomes measured included women's anxiety, knowledge or understanding of screening tests, satisfaction with information provision, and uptake of tests.
Table 3.
Antenatal testing information: results*
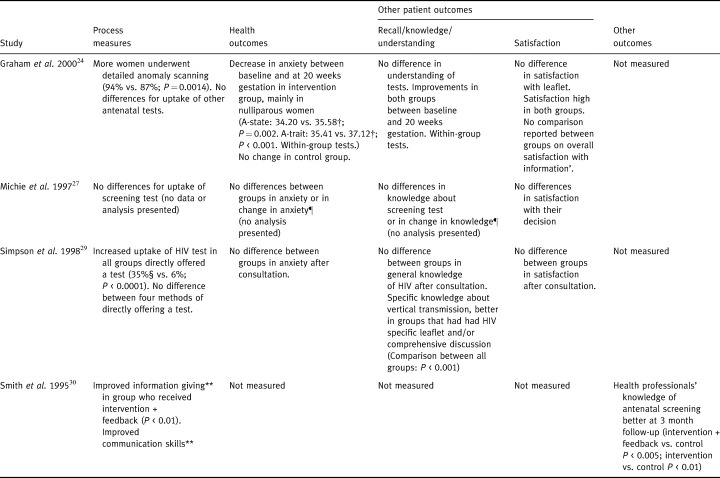
Table 9.
Table 3 (Continued)
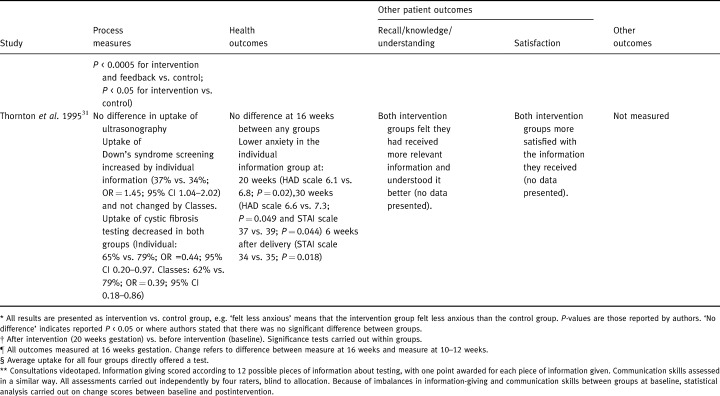
One of these trials involved offering pregnant women extra information on antenatal screening, either in individual sessions or in groups of 4–12 women, compared with a control group who received the standard information provided at the booking appointment. 31 The extra information given included more detail on population risks and specific risks for Down's syndrome, the procedure related risks of amniocentesis and the possibilities of false positive and false negative results. Compared with the other two groups, women who were offered individual information were less anxious. Both groups of women who were offered extra information felt that they had received more relevant information, had better understanding and were more satisfied with the information they received. The uptake of screening was, on the whole, little changed by extra information. The exceptions were Down's syndrome screening, for which uptake was slightly increased by the offer of individual information, and screening for cystic fibrosis, which had lower uptake rates in both the groups that were offered more information.
Another trial compared different methods of offering antenatal HIV testing to women. 29 Direct offers of the test using detailed or summary leaflets and full or brief discussions, were compared with the standard practice where tests were not offered routinely and extra information was not given. All methods of directly offering the test resulted in higher uptake than in the control group, with neither the style of the leaflet nor the length of discussion having any effect on uptake. Anxiety and satisfaction were not affected by differences in the methods used to offer the test.
In two further trials, changes were made to the format as well as to the amount of information given to women. In the first of these, women were offered extra information on antenatal testing by means of a touch screen system available in the antenatal clinic waiting area. 24 The results indicated reduced anxiety in the women who received the more detailed information and novel format of the touch screen system, compared to no change in anxiety in the control group who received standard information leaflets. There were no differences between the two groups in their understanding of antenatal tests or their satisfaction with the information they were given.
In the second trial of this type, women received either a simple information leaflet on Down's syndrome, the screening test and the implications of positive or negative results, or an expanded leaflet which also listed the pros and cons of having the test and a decision‐tree to facilitate the decision‐making process. 27 Two other groups of women also received a video in addition to the leaflets. This was a poor quality trial with a very high dropout rate and no significant differences were found between the four groups on any of the outcomes measured.
In the final trial in this group, doctors and midwives were given training in presenting antenatal screening tests. 30 Consultations were videotaped and the amount of information given about screening was assessed and scored according to 12 possible pieces of information. These items included, for example, that screening is optional, what the screening test involves, the likelihood of the condition(s) occurring, the meaning of possible results and action taken on a positive result. Doctors' and midwives' knowledge of screening tests was also assessed 3 months after training. The numbers in this trial were small, partly due to a high proportion of dropouts, and the outcomes tested were limited, but the results indicated improved information giving about antenatal tests and improved knowledge compared with a group who had no training.
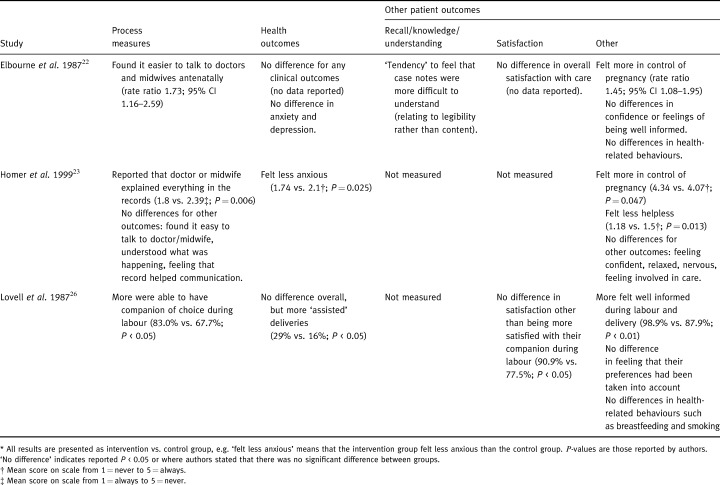
Woman‐held maternity records
These three trials used similar methods and produced similar conclusions. 22 , 23 , 26 Women holding their own maternity records were compared with those holding standard co‐operation cards, which contain an abbreviated version of the full record, updated at each visit. A variety of outcomes was compared including clinical outcomes, perceptions about control over and involvement in their care and quality of communication and satisfaction with their care. The results are summarized in Table 4. No striking differences were found in clinical outcomes. The results of these trials in terms of outcomes directly related to communication were mixed, but suggest that some aspects of communication were improved by women carrying their own records. In one trial, women who carried their own records found it easier to talk to their carers. 22 In the second trial, women carrying their own records did not find it easier to talk to their carers and did not feel that the record helped communication, but were more likely to report that their carers explained everything in their records. 23 In the third trial women who carried their own records were more likely to report feeling well informed during labour and delivery. 26 In both the trials that measured women's perceived control over their pregnancy, women who carried their own records felt more in control. 22 , 23 None of the trials found any differences in satisfaction with care, which was generally high, or in health‐ related behaviours such as smoking, alcohol consumption and breast‐feeding.
Table 4.
Woman‐held maternity records: results*
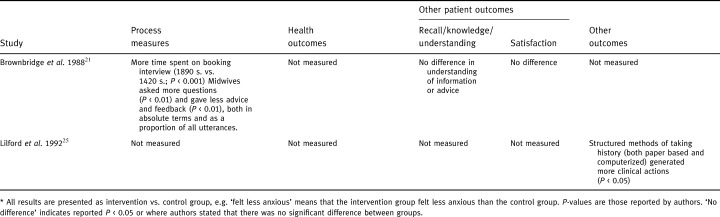
Computer‐based history taking
Two trials examined different aspects of using the same computer system for taking histories at the first antenatal (booking) appointment in one hospital in the UK. 21 , 25 These trials are summarized in Table 5. Using this computer system, midwives and women both faced the computer screen and midwives asked questions prompted by the structured checklist on the screen. In the first trial the computer system was compared with the standard manual checklist used in that hospital. 21 The second trial included these two groups and added a third comparison group, using a longer structured manual checklist. 25 The primary outcomes of these trials related to the process of the booking appointment, such as the time taken for each appointment, and the degree to which the computer system successfully highlighted risk factors requiring action. The first trial also measured aspects of communication between the women and their midwives. 21 In the first trial the booking appointment took more time to complete when the computer system was used and midwives asked more questions and gave less advice and feedback to women. 21 In the second trial, more nonroutine `clinical actions' were generated on the basis of the history taken at the booking appointment when the computer system was used. 25
Table 5.
Computer‐assisted history taking: results*
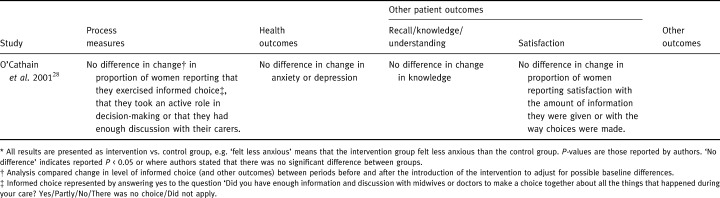
Informed Choice leaflets
The one remaining trial included in this review was different in many respects from the others. 28 It is summarized in Table 6. In this cluster randomized trial, five intervention group maternity units received sets of Midwives Information and Resource Service (MIDIRS) Informed Choice leaflets, aimed at both women and their carers, designed to promote decision‐making based on evidence informed choice in 10 specific topic areas. Staff also received a one‐off training session in using the leaflets in clinical practice. Women's informed choice was assessed using questionnaires before and after the introduction of the leaflets and change in the level of informed choice compared with change over the same period in control hospitals where women received standard care. On the primary outcome measure of informed choice and on other relevant outcomes such as satisfaction and feeling in control the results indicated no significant differences between the two groups.
Table 6.
Informed Choice leaflets: results*
Discussion
The number of trials identified relating to improving communication between health professionals and women in maternity care was very small and they provided information about very few aspects of care. Interventions that aim to change fundamental aspects of communication between patients and their carers, promoting different styles of communication, increasing the involvement of patients in their care and encouraging shared decision‐making, have found some success in other areas of care. 7 With the possible exception of the MIDIRS Informed Choice leaflets trial, 28 which sought in a relatively indirect way to increase the involvement of women in their care and promote shared decision‐making, none of the trials we identified focused on improving communication between women and their carers in any fundamental way.
Of the remaining trials, one trial tested an intervention explicitly designed to improve communication, but used only limited outcome measures. 30 The other four trials in the area of antenatal testing did not explicitly refer to communication, but focused on the provision of information, a central although limited aspect of communication. 24 , 27 , 29 , 31 The primary aim of the three trials of woman‐held maternity records was to assess whether this would increase the woman's involvement in her care, albeit in a relatively indirect way. 22 , 23 , 26 As such, we judged that improved communication was an implicit aim of these interventions. Finally, the trials of computer‐assisted antenatal history taking were included. 21 , 25 This was because improving the transfer of information from the woman to the midwife with the aim of improving decision‐making was judged to be an implicit part of its aim, even though improving communication was not the primary aim of the intervention.
Although this small number of trials explored only limited aspects of the central question of how to improve communication between carers and women in maternity care, some qualified conclusions can be made.
The trial of MIDIRS Informed Choice leaflets was notable in that it explicitly set out to promote informed choice and increase women's involvement in decision‐making about their care. The results of the trial provided no evidence that the leaflets had any effect on informed choice, women's involvement in decision‐making or on components of informed choice such as knowledge or satisfaction, although the vast majority of women found the leaflets helpful. A qualitative study alongside the trial involving observation of clinical practice, interviews with women and professionals, and focus groups with women suggested a number of reasons why the leaflets were not effective. 32 For example, the lack of a strategy for distributing the leaflets and using them to promote informed decision‐ making meant that in most cases simply giving a leaflet to a woman, or just making the leaflets available, was equated with promoting informed choice. The researchers also noted that power differentials between women and their carers often resulted in women's compliance with the `right' choice reflecting normative patterns of care. These and other problems highlight the difficulties involved in intervening to improve a complex process such as communication.
The effects of giving women extra information about antenatal testing appeared to vary according to how this information was presented. 24 , 27 , 29 , 31 These trials also tended to suggest that extra information does not make women more anxious and may even lessen their anxiety. The effects of using different formats such as a video or a multimedia touch‐screen system for conveying information are difficult to assess since these interventions also involved giving more wide‐ranging and more detailed information. Compared with detailed leaflets combined with individual advice and discussion, giving information in a novel format is unlikely to demonstrate additional benefits for women, in terms of anxiety, knowledge and satisfaction.
The other outcome measure used in these trials was the uptake of screening tests. These results are hard to interpret, since the desirable outcome of improved communication is not simply increased or decreased uptake of the clinical tests, but more appropriate uptake. In other words, the aim should be for women to be able to make informed choices as to which tests are most appropriate for their individual circumstances. In some cases, authors speculated that this might have been the underlying cause for changes in uptake of tests. For example, it was suggested that being given extra information about a newly available test for cystic fibrosis empowered more women to decline a test that they might otherwise have accepted. 31 This suggestion is supported by qualitative research looking at women's motivations for antenatal testing, which indicates that without detailed information and the opportunity to discuss screening with their carers, women often accept screening tests as `routine' rather than making informed choices. 32 Trials which could build on these, by looking at individually tailored information interventions combined with assessments of women's views would be valuable.
Giving information about antenatal testing is also an area in which qualitative research has highlighted women's criticisms of carers' communication skills. 33 The single small trial of giving midwives and doctors communication skills training suggested that this may help to improve the transfer of information about antenatal tests. 30 To test this suggestion, it would be important to replicate and extend this trial to include outcomes relating to women's satisfaction, knowledge and well being. Trials of communication skills training outside maternity care have suggested that this kind of intervention has the potential to improve patient satisfaction, knowledge and compliance. 34 , 35, –36 It could even improve more fundamental aspects of well being such as psychological and clinical outcomes. 34 , 35 Trials are needed of focused communication skills training for health professionals in maternity care in order to investigate how best to meet the need for improvements clearly articulated by women.
The trials of woman‐held maternity records suggested some benefits for mothers in terms of their perceptions of communication with carers and their involvement in and control over their care in pregnancy. Woman‐held maternity records are now almost universal, although there is some variation between units in the time that women are given their records and the amount of information that they hold (S. Das – National Maternity Record Project Co‐ordinator, pers. comm.). Given that at least part of the rationale for woman‐held maternity records is improved communication, it is essential that the format of maternity records encourages good communication practice in professionals and presents information in a way that is clear and accessible to women. The National Maternity Record Project (NMRP), funded by the Department of Health in 1995 under the Changing Childbirth initiative, aims to produce just such a record that could be used throughout the country. Although work on this project is still continuing and use of the antenatal module of the NMRP by maternity units is increasing, problems with funding have hampered further progress (S. Das, pers. comm.). A formal evaluation of how the National Maternity Record enhances the clarity and communication of information and knowledge would be welcome.
The trials of computer‐based history taking related to one very specific intervention. 21 , 25 Here the aim was to improve the way specific items of information were obtained from women in order to identify risk factors requiring action, rather than to improve all round communication. These trials provided some evidence that structured checklists in general and computer‐based checklists in particular were more effective than simple checklists for obtaining information from women and improving doctors' response to risk factors. Despite this, results from the one trial that examined interaction between midwives and women also suggested that the flow of information and advice from the midwife to the woman might have been restricted by these systems. 21 Evidence from this trial suggested that this problem might have decreased, as the midwives became more familiar with the system. Nevertheless, it is a cause for concern that should be considered in the design of any similar systems in future.
These trials addressed only a few aspects of communication between maternity carers and women. They all focused on communication in the antenatal period. Research is also needed on other key areas of care. Despite evidence from observational studies that communication between carers and women in labour may be poor, 13 , 14 no studies were identified of any attempt to improve communication between women and their carers while in labour. This is a time when acute and emergent demands on both women and their carers pose particular problems for communication and an area where research is needed.
Studies of women's views also suggest that hospital postnatal care is the aspect of their care with which women generally feel least satisfied. 10 Communication may be particularly difficult after a problematic birth, where the baby is ill, has a more serious abnormality or dies soon after birth. There has been considerable research, outside maternity care, on `breaking bad news', particularly in cases of cancer, 6 but only a handful of observational studies looking at talking to parents of babies or young children with serious disabilities were identified. Similarly, although several studies that examined parents' views of care after the death of their baby were identified, none were trials. While qualitative research in this area is essential, these studies could usefully be supplemented by trials of appropriate interventions to improve communication in this difficult area.
Finally, none of the trials in this review covered the important subject of communication between health professionals and women from non‐English speaking backgrounds. While we are aware of observational studies and other evaluations of linkworker and advocacy services for these women, 37 , 38 we did not identify any trials of these services in maternity care. Further research in this area would be valuable.
Conclusions
In a limited number of areas, these trials point to potentially useful interventions for improving communication between health professionals and women in maternity care. Extra information about antenatal testing, provided in detailed leaflets or in individual advice sessions, is valued by women and may reduce anxiety about testing. It may alter uptake of some specific tests, but it is unclear whether it prompts a more appropriate uptake. Focused communication skills training for midwives and doctors may be of benefit in this and other areas, but further trials, which also assess the impact on women's well being, are required. Woman‐held maternity records also bring benefits to women in terms of their perceived involvement in and control over their care. The lack of trials of interventions aimed at promoting shared decision‐making and increasing the involvement of women in their care in other ways is disappointing. The MIDIRS Informed Choice trial showed the complexities of research in this area however. The lack of controlled trials relating to communication in a number of key areas of delivery and postnatal care is also a major gap in our knowledge. Trials of interventions to improve communication between carers and women in labour and in the postnatal period would be particularly useful.
Acknowledgements
This review forms part of a larger report commissioned and funded by CESDI. 17 The authors would like to thank the members of the CESDI Communications Working Group for their helpful comments and advice.
References
- 1. Royal College of Obstetricians and Gynaecologists Royal College of Midwives. Communication Standards – Obstetrics. Report of the Audit Committee's Working Group London: RCOG, 1995.
- 2. Royal College of Physicians of London. Improving Communication Between Doctors and Patients. A report of a working party London: Royal College of Physicians, 1997.
- 3. General Medical Council. Tomorrow's doctors: recommendations on undergraduate medical education London: General Medical Council, 1993.
- 4. Hargie O, Dickson D, Boohan M, Hughes K. A survey of communication skills training in UK schools of medicine: present practices and prospective proposals. Medical Education, 1998; 32 : 25–34. [DOI] [PubMed] [Google Scholar]
- 5. Department of Health. The NHS Plan, a Plan for Investment, a Plan for Reform. Cm 4818–4811 London: TSO, 2000.
- 6. Ong LML, De Haes JCJM, Hoos AM, Lammes FB. Doctor–patient communication: a review of the literature. Social Science and Medicine, 1995; 40 : 903–918. [DOI] [PubMed] [Google Scholar]
- 7. Stewart MA. Effective physician‐patient communication and health outcomes: a review. Canadian Medical Association Journal, 1995; 152 : 1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 8. Department of Health. Changing childbirth. Part 1 Report of the Expert Maternity Group (Chair: Baroness Cumberlege). London: HMSO, 1993.
- 9. Department of Health. Changing childbirth. Part 2: Survey of good communication practice in maternity services (Chair: Baroness Cumberlege). London: HMSO, 1993.
- 10. Garcia J, Redshaw M, Fitzsimons B, Keene J. First Class Delivery. A National Survey of Women's Views of Maternity Care. London: Audit Commission, 1998.
- 11. National Childbirth Trust. Birth Choices: Women's Expectations and Experiences. Report of a research project `Choices: childbirth options, information and care in Essex' London: NCT, 1995.
- 12. Drew NC, Salmon P, Webb L. Mothers′, midwives' and obstetricians' views on the features of obstetric care which influence satisfaction with childbirth. British Journal of Obstetrics and Gynaecology, 1989; 96 : 1084–1088. [DOI] [PubMed] [Google Scholar]
- 13. Garcia J, Garforth S. Parents and new‐born babies in the labour ward. In: Garcia J, Kilpatrick R, Richards M (eds.) The Politics of Maternity Care. Services for Childbearing Women in Twentieth‐Century Britain. Oxford: Oxford University Press, 1990: 163–182.
- 14. Kirkham M. Midwives and information‐giving in labour. In: Robinson S, Thomson A (eds.) Midwives, Research and Childbirth, Vol. I. London: Chapman & Hall, 1989: 117–138.
- 15. Hall JA, Roter DL, Katz NR. Meta‐analysis of correlates of provider behavior in medical encounters. Medical Care, 1988; 26 : 657–675. [DOI] [PubMed] [Google Scholar]
- 16. Anderson LA, Sharpe PA. Improving patient and provider communication: a synthesis and review of communication interventions. Patient Education and Counseling, 1991; 17 : 99–134. [Google Scholar]
- 17. Rowe RE, Garcia J, Macfarlane AJ, Davidson LL. Communication issues in stillbirth and infant death: a review of communications within the CESDI framework Oxford: NPEU, 1999.
- 18. Rowe RE, Garcia J, Macfarlane AJ, Davidson LL. Does poor communication contribute to stillbirths and infant deaths? A review. Journal of Public Health Medicine, 2001; 23 : 23–34. [DOI] [PubMed] [Google Scholar]
- 19. Green JM, Curtis P, Price H, Renfrew MJ. Continuing to care. The organization of midwifery services in the UK. a structured review of the evidence. Hale: Books for Midwives, 1998.
- 20. Jüuni P. Altman DA, Egger M. Assessing the quality of randomised controlled trials. In. Egger M, Davey Smith G, Altman DA (eds.) Systematic Reviews in Health Care: Meta‐Analysis in Context London: BMJ Publishing, 2001: 87–108.
- 21. Brownbridge G, Lilford RJ, Tindale Biscoe S. Use of a computer to take booking histories in a hospital antenatal clinic. Acceptability to midwives and patients and effects on the midwife–patient interaction. Medical Care, 1988; 26 : 474–487. [DOI] [PubMed] [Google Scholar]
- 22. Elbourne D, Richardson M, Chalmers I, Waterhouse I, Holt E. The Newbury Maternity Care Study: a randomized controlled trial to assess a policy of women holding their own obstetric records. British Journal of Obstetrics and Gynaecology, 1987; 94 : 612–619. [DOI] [PubMed] [Google Scholar]
- 23. Homer CSE, Davis GK, Everitt LS. The introduction of a woman‐held record into a hospital antenatal clinic: The bring your own records study. Australian and New Zealand Journal of Obstetrics and Gynaecology, 1999; 39 : 54–57. [DOI] [PubMed] [Google Scholar]
- 24. Graham W, Smith P, Kamal A, Fitzmaurice A, Smith N, Hamilton N. Randomised controlled trial comparing effectiveness of touch screen system with leaflet for providing women with information on prenatal tests. British Medical Journal, 2000; 320 : 155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lilford RJ, Kelly M, Baines A et al Effect of using protocols on medical care: randomised trial of three methods of taking an antenatal history. British Medical Journal, 1992; 305 : 1181–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lovell A, Zander LI, James CE, Foot S, Swan AV, Reynolds A. The St. Thomas's Hospital maternity case notes study: a randomised controlled trial to assess the effects of giving expectant mothers their own maternity case notes. Paediatric and Perinatal Epidemiology, 1987; 1 : 57–66. [DOI] [PubMed] [Google Scholar]
- 27. Michie S, Smith D, McClennan A, Marteau TM. Patient decision making: An evaluation of two different methods of presenting information about a screening test. British Journal of Health Psychology, 1997; 2 : 317–326. [Google Scholar]
- 28. O'Cathain A, Walters SJ, Nicholl JP, Thomas KJ. Cluster randomised trial of Informed Choice leaflets. In: NHS Centre for Reviews and Dissemination Informed Choice in Maternity Care: an Evaluation of Evidence‐Based Leaflets. York: NHS Centre for Reviews and Dissemination, University of York, 2001: 33–44.
- 29. Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Prescott RJ. Uptake and acceptability of antenatal HIV testing: randomised controlled trial of different methods of offering the test. British Medical Journal, 1998; 316 : 262–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Smith DK, Shaw RW, Slack J, Marteau TM. Training obstetricians and midwives to present screening tests: evaluation of two brief interventions. Prenatal Diagnosis, 1995; 15 : 317–324. [DOI] [PubMed] [Google Scholar]
- 31. Thornton JG, Hewison J, Lilford RJ, Vail A. A randomised trial of three methods of giving information about prenatal testing. British Medical Journal, 1995; 311 : 1127–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. NHS Centre for Reviews and Dissemination. Informed Choice in Maternity Care: an Evaluation of Evidence‐Based Leaflets York: NHS Centre for Reviews and Dissemination, University of York, 2001.
- 33. Al Jader LN, Parry Langdon N, Smith RJ. Survey of attitudes of pregnant women towards Down syndrome screening. Prenatal Diagnosis, 2000; 20 : 23–29.DOI: 10.1002/(sici)1097-0223(200001)20:1<23::aid-pd746>3.0.co;2-t [DOI] [PubMed] [Google Scholar]
- 34. Inui TS, Yourtee EL, Williamson JW. Improved outcomes in hypertension after physician tutorials. A controlled trial. Annals of Internal Medicine, 1976; 84 : 646–651. [DOI] [PubMed] [Google Scholar]
- 35. Lewis CC, Pantell RH, Sharp L. Increasing patient knowledge, satisfaction, and involvement: randomized trial of a communication intervention. Pediatrics, 1991; 88 : 351–358. [PubMed] [Google Scholar]
- 36. Evans BJ, Kiellerup FD, Stanley RO, Burrows GD, Sweet B. A communication skills programme for increasing patients' satisfaction with general practice consultations. British Journal of Medical Psychology, 1987; 60 : 373–378. [DOI] [PubMed] [Google Scholar]
- 37. Parsons L, Day S. Improving obstetric outcomes in ethnic minorities: an evaluation of health advocacy in Hackney. Journal of Public Health Medicine, 1992; 14 : 183–191. [PubMed] [Google Scholar]
- 38. Warrier S. Consumer Empowerment: a Qualitative Study of Linkworker and Advocacy Services for Non‐English Speaking Users of Maternity Services London: Maternity Alliance, 1996.


