Abstract
Objective To describe the decision‐making needs of Canadians when faced with ‘complex’ health decisions characterized by balancing advantages against disadvantages. Although a national report emphasized that public confidence in the health‐care system depends on support for personal knowledge and decision‐making, there has been no systematic investigation of the Canadian population's decision‐making needs.
Design Cross‐sectional telephone survey using random digit dialling.
Participants National sample of 635 adults over 18 years of age, living in Canada.
Results Forty‐two percentage of eligible contacts participated. Sixty‐five percent of contacts reported making ‘complex’ health decisions, commonly about medical or surgical treatments or birth control, and more commonly by women and by married/separated individuals. Most respondents took an active role in their decisions, often sharing the process with their partner or family. Being younger was associated with a more independent role. Physicians were more often involved in the decisions of respondents with less education. Fifty‐nine percent of respondents experienced decisional conflict; more conflict was seen with those who were female and feeling uninformed about options, pressured to select one particular option, and unready or unskilled in decision‐making. Less decisional conflict was seen in those who reported birth control decisions and in those who were 70 years and older. Participants used several strategies when deliberating about choices including: information gathering, clarifying their values, and seeking support and information from others. Personal counselling and printed information materials were commonly preferred methods of learning about options. ‘Essential’ criteria for judging satisfactory decision‐making included: having sufficient knowledge about the options, outcomes, and probabilities; being clear about values; selecting and implementing a choice that agrees with personal values; and expressing satisfaction with the choice.
Conclusions Canadians, particularly women, face difficult decisions and need support and information from credible sources.
Keywords: Canadian, decision‐making, health
Introduction
A report on the health information needs of the Canadian population prepared by the Canadian Institute of Health Information 1 identified several key performance criteria for ensuring public confidence in the health‐care system. These included a shift from a practitioner‐ to client‐centred service model and support for personal knowledge and decision‐making based on credible and accessible information. Consumers increasingly want more control over decisions affecting their health and now have expectations for information and access to information to support their decision‐making. Although several centres and societies are beginning to respond to these needs by developing consumer‐friendly practice guidelines and decision aids, there has been little systematic investigation of the decision‐making experiences of the population. Key issues are the: types of decisions people face; processes used to make decisions; difficulties or decisional conflict people experience; roles people take in decision‐making; preferred types and sources of information about options; and criteria people use to judge that a decision is satisfactory. This is the first survey of its kind to describe the decision‐making needs of Canadians when faced with complex health decisions.
Methods
Design
We conducted a cross‐sectional telephone survey between 20 January and 10 February 1999. The target population consisted of all adults 18 years of age and older residing in Canada. A random sample of telephone numbers was generated from a recent national electronic telephone directory. The last two digits of each number were then also randomized to ensure that all numbers within an exchange would have equal opportunity of being selected. This procedure ensured that new, changed, and unlisted numbers were included in the sample without unduly increasing the non‐working numbers that a fully randomized digit selection procedure produces.
Interviewers solicited the participation of household members, 18 years of age or older, who had the most recent birthday. This selection procedure was used to avoid any bias related to who answered the telephone. Fieldwork was conducted by trained, bilingual interviewing staff experienced in surveys with the general population. All telephone interviews took place from a central office in downtown Ottawa. Data collection was monitored as the interviews were performed.
Selected respondents were contacted by telephone on weekday evenings between 5.00 and 9.00 pm local time or on weekends between 11.00 and 5.00 pm. Up to four call‐backs were performed before a new telephone number was substituted. Respondents who were unable to be interviewed at the time of the initial call had a call‐back scheduled at a time convenient to them. Interviewers maintained full documentation for the outcome of each call made, including notations on refusals. Quality control checks on coding and data entry were conducted with a randomly selected sample of 10% of the questionnaires.
Survey tool
The structured telephone interview included 60 questions, lasted an average of 13 min, and was completed in the respondent's choice of official language (English or French). The interview began by asking participants whether or not they had made a ‘complex’ health decision in the past. Complex decisions were defined as follows:
An example of a simple health decision would be taking an antibiotic for an infection. Usually your doctor recommends a treatment and you do not get very involved in the decision‐making. We are interested in more complex or difficult decisions, when you have to consider the pros and cons of the options, and there is no right or wrong choice. With this type of decision, your choice depends on your personal situation and what is most important to you. These decisions may involve: discussing the decision with your doctor or others, reading written materials, and taking a bit more time to consider what you want to do.
Participants were then prompted with examples if necessary. The broad classifications of examples included decisions about: surgery, medical treatments, birth control, institutionalization of a family member, pregnancy and childbirth, lifestyle changes, and diagnostic testing.
Once respondents identified a particular decision, they were asked a series of closed‐ and open‐ended questions based on the Ottawa Framework of Decision Support. 2 , 3 The framework identifies variables to consider in: (1) assessing determinants of decisions to identify needs; (2) providing or seeking decision support; and (3) evaluating decision‐making. Specific variables in the survey included:
-
1
Determinants of decisions included: (a) perceptions of the decision such as type of decision; time frame of the decision; options faced; perceived advantages and disadvantages of each option; manifestations of decisional conflict or uncertainty (see Table 5); and cognitive factors contributing to decisional conflict such as feeling uninformed and unclear about personal values (see Table 6); (b) perceptions of others involved in the choice such as decision‐making roles (see Table 4); and social factors contributing to decisional conflict such as not knowing what others decide or recommend, pressure from others to select an option, and inadequate support in decision‐making (see Table 6); (c) personal resources for decision‐making such as motivation or readiness to make choices and skill in decision‐making (see Table 6); and (d) personal characteristics such as age, gender, education, civil status, language, employment status, and income adequacy (see Table 1).
-
2
Decision‐support interventions such as the strategies used to deliberate about the options and the preferred delivery methods and sources of information about options (see Table 7).
-
3
Evaluation criteria considered important in judging that a decision was satisfactory. A list of pre‐set criteria from the framework was presented and respondents were asked to judge whether these criteria were: (a) necessary, (b) nice to have, (c) not necessary, or (d) not sure. Participants were also invited to add other criteria.
Table 5.
Reported manifestations of decisional conflict* when respondents were considering their options (n = 402)
| Difficulties | % (CI) | Surgical, n = 122 | Medical, n = 112 | Institutionali zation, n = 24 | Pregnancy, n = 22 | Birth control, n = 100 | Lifestyle, n = 21 |
|---|---|---|---|---|---|---|---|
| 1. Felt unsure about what to choose | 59 (54, 64) | 77 (63) | 66 (59) | 19 (79) | 14 (64) | 48 (48) | 12 (57) |
| 2. Questioned what was important to them | 77 (72, 81) | 89 (73) | 88 (79) | 18 (75) | 18 (82) | 79 (79) | 16 (76) |
| 3. Worried what could go wrong if they made a choice | 61 (56, 66) | 81 (66) | 67 (60) | 18 (75) | 13 (59) | 55 (55) | 11 (52) |
| 4. Felt distressed or upset? | 45 (40, 50) | 56 (46) | 57 (51) | 15 (63) | 6 (27) | 33 (33) | 10 (48) |
| 5. Felt like they couldn't get the decision off their minds | 40 (35, 45) | 52 (43) | 47 (42) | 15 (63) | 6 (27) | 32 (32) | 6 (29) |
| 6. Felt physically stressed (tense muscles, a racing heartbeat, or difficulty sleeping?) | 37 (32, 42) | 46 (38) | 52 (46) | 13 (54) | 6 (27) | 23 (23) | 7 (33) |
| 7. Wanted to delay the decision? | 27 (23, 32) | 24 (20) | 34 (30) | 12 (50) | 6 (29) | 28 (28) | 3 (14) |
| 8. Wavered between the choices that they faced? | 26 (22, 30) | 23 (19) | 36 (32) | 7 (29) | 7 (32) | 25 (25) | 6 (29) |
*These items describe behavioural manifestations of decisional conflict, which is defined as a state of uncertainty about the best course of action. Verbalized uncertainty is the hallmark of decisional conflict. Response categories: 1 – yes, 2 – unsure, 3 – no.
Table 6.
Factors contributing to decisional conflict* (n = 411)
| Factors | Total, n (%) | Sure about choice, n = 170 | Unsure about choice, n = 243 |
|---|---|---|---|
| 1. Did you feel that you were clear about what was personally important to you? | 374 (91) | 158 (93) | 216 (89) |
| 2. Did you feel motivated or ready to make the decision? | 362 (88) | 160 (94) | 202 (83) |
| 3. Did you feel you had the ability or skill to make this type of decision? | 349 (85) | 156 (92) | 192 (79) |
| 4. Did you feel that you had enough support from others to make the decision? | 325 (79) | 138 (81) | 190 (78) |
| 5. Did you feel that you knew enough about the options, their pros and cons? | 304 (74) | 143 (84) | 163 (67) |
| 6. Did you feel that you knew how likely each of the pros and cons were? | 300 (73) | 133 (78) | 170 (70) |
| 7. Did you have enough information on what others decide or recommend? | 247 (60) | 104 (61) | 143 (59) |
| 8. Did you feel pressure from others to select an option you were not sure about? | 82 (20) | 27 (16) | 61 (25) |
*These are the hypothesized factors contributing to decisional conflict. Cognitive factors were items 1, 5, and 6; social factors were items 4, 7, and 8; and resource factors were items 2 and 3. Response categories: 1 – yes, 2 – unsure, 3 – no.
Table 4.
Decision‐making role of respondents (n = 410)
| Role | % (CI) | Surgical, n = 122 | Medical, n = 112 | Institutionalization, n = 24 | Pregnancy, n = 22 | Birth control, n = 100 | Lifestyle, n = 21 |
|---|---|---|---|---|---|---|---|
| I decided on my own | 29 (25, 34) | 23 (19) | 14 (13) | 8 (33) | 9 (41) | 54 (54) | 8 (38) |
| I decided after considering my doctor's opinion | 39 (34, 44) | 56 (46) | 48 (43) | 8 (33) | 6 (27) | 28 (28) | 9 (43) |
| I decided with my doctor | 23 (19, 27) | 37 (30) | 30 (27) | 6 (25) | 3 (14) | 15 (15) | 2 (10) |
| My doctor decided after considering my opinion | 2 (1, 4) | 2 (2) | 5 (4) | 1 (4) | 0 (0) | 1 (1) | 1 (5) |
| My doctor decided on his or her own | 4 (2, 6) | 2 (2) | 10 (9) | 0 (0) | 2 (9) | 0 (0) | 1 (5) |
| Other | 3 (2, 5) | 2 (2) | 5 (4) | 1 (4) | 2 (9) | 2 (2) | 1 (5) |
Table 1.
Demographic characteristics of survey respondents (n = 635)
| Variable | Total sample, % (95% CI) | Canadian census 1996, % |
|---|---|---|
| Age (years) | ||
| 18–24 | 11 (9, 14) | 9* |
| 25–29 | 7 (5, 9) | 10 |
| 30–39 | 23 (20, 27) | 23 |
| 40–49 | 22 (19, 26) | 21 |
| 50–59 | 17 (15, 21) | 15 |
| 60–69 | 9 (7, 12) | 11 |
| 70 or more | 9 (7, 12) | 12 |
| Gender | ||
| Male | 35 (32, 39) | 49 |
| Female | 65 (61, 68) | 51 |
| Marital status | ||
| Single/never married | 23 (20, 27) | 36 |
| Married/separated | 65 (61, 69) | 53 |
| Divorced | 6 (4, 8) | 5 |
| Widowed | 6 (4, 8) | 6 |
| Education | ||
| Less than grade 9 | 5 (4, 7) | 12 |
| High school | 40 (36, 44) | 40 |
| Some college/university | 31 (28, 35) | 34 |
| University degree | 24 (20, 27) | 13 |
| Home language | ||
| English | 73 (69, 76) | 67 |
| French | 20 (17, 24) | 22 |
| Chinese | 0.6 (0, 2) | 2 |
| Italian | 0.3 (0, 1) | 1 |
| Other | 6 (4, 8) | 8 |
| Employment | ||
| Working | 58 (54, 62) | 60 |
| Looking for work | 3 (2, 5) | 5 |
| Other | 39 (35, 42) | 35 |
| Income meets needs | ||
| Very well | 22 (18, 26) | |
| Adequate | 60 (55, 65) | |
| Not very well | 12 (9, 16) | |
| Totally inadequate | 4 (3, 8) | |
| Not reported | 1 (1, 2) |
*Age data for adults 20–24 years old.
Results in bold face indicate the data for which the confidence intervals do not overlap with the census data.
Table 7.
Process used in decision‐making (n = 405)
| Process | % (CI) | Surgical, n = 122 | Medical, n = 112 | Institutiona lization, n = 24 | Pregnancy, n = 22 | Birth control, n = 100 | Lifestyle, n = 21 |
|---|---|---|---|---|---|---|---|
| Considered how important each of the pros and cons were | 82 (78, 86) | 105 (86) | 90 (80) | 20 (83) | 15 (68) | 83 (83) | 15 (71) |
| Got info on options, pros and cons | 80 (76, 84) | 104 (85) | 84 (75) | 20 (83) | 14 (64) | 83 (83) | 16 (76) |
| Got info on likelihood of pros and cons | 74 (69, 78) | 99 (81) | 82 (73) | 18 (75) | 14 (64) | 69 (69) | 15 (71) |
| Got support from others | 69 (64, 73) | 88 (72) | 77 (69) | 21 (88) | 16 (73) | 56 (56) | 15 (71) |
| Got information on what others decide/recommend | 50 (45, 55) | 63 (52) | 57 (51) | 10 (42) | 9 (41) | 50 (50) | 10 (48) |
| Considered ways to handle pressure from others | 19 (15, 23) | 45 (37) | 25 (22) | 6 (25) | 8 (35) | 17 (17) | 3 (14) |
Response categories: 1 – yes, 2 – unsure, 3 – no.
These survey questions were reviewed by a panel of international experts in decision‐making and by survey methodologists.
Analysis plan and sample size
A sample size of 400 participants reporting a complex decision was planned to limit the margin of error to 5% around an estimate of 50% with 95% confidence. Descriptive statistics were used to summarize the decision‐making experiences of respondents including 95% confidence intervals. The following comparisons were made: (a) differences between the sample characteristics and the census; (b) differences in type of decision by demographic characteristics; (c) differences in responses to remaining questions by type of decision; and (d) differences in frequency of factors contributing to decisional conflict by reported decisional conflict (uncertainty). Differences were reported when 95% confidence intervals among subgroups did not overlap.
We planned regression analyses to examine the factors associated with role in decision‐making and the number of manifestations of decisional conflict.
The roles in decision‐making were not normally distributed among categories of independence/dependence; therefore, we used logistic regression to regress the independent factors of decision type and demographic characteristics (education, age, and gender) on: (a) having an independent role in decision‐making; and (b) having a dependent role in decision‐making. In the first analysis, role was dichotomized as follows: those who reported playing an independent role in decision‐making (I decided on my own) vs. those who played a more dependent role in decision‐making (I decided after considering my doctor's opinion, I decided with my doctor, my doctor decided after considering my opinion, or my doctor decided on his/her own. In the second analysis, role was dichotomized as follows: those who reported playing a dependent role in decision‐making (my doctor decided after considering my opinion, or my doctor decided on his/her own) vs. those who played a more independent role in decision‐making (I decided on my own, I decided after considering my doctor's opinion, I decided with my doctor).
The dependent variable of number of manifestations of decisional conflict ranged from 0 to 8 and was normally distributed. Therefore, we used multiple regression analysis to regress the independent factors of decision type, demographic characteristics (education, age, gender), role in decision‐making, and number of manifestations of decisional conflict.
Results
Of the 7136 telephone numbers dialled, 4597 (64%) were functional residential numbers. Of these, 1630 (35%) resulted in contact with a potential participant. Of the potential participants, 680 (42%) agreed to be interviewed. Forty‐five questionnaires were lost during data cleaning because of errors in following skip patterns and missing demographic data, resulting in a total of 635 completed interviews.
Characteristics of the sample
Table 1 summarizes the demographic characteristics of the sample compared to census statistics for 1996. 4 Our sample estimates overlapped with the census on employment. Each of the provinces was also represented in proportion to their percentage of the population (data not shown). Compared to the census, there were small differences (3–7%) in age, language, and education categories; slightly more participants reported their home language as English and slightly fewer participants were aged 25–29 years, or had less than a grade 9 education. Compared to the census, the sample had appreciable differences (11–14%) in gender, civil status, and higher education; more participants were female, university educated, and married.
Decisions
Of the 635 participants completing the interview, 413 (65%) reported making a complex health decision in the past and 222 (35%) did not. Twenty‐seven percent of the group who had made a decision had made their decision within the 12 months prior to the survey, 38% had made their decision 1–5 years before, and a further 36% had made their decision more than 5 years before the survey. Only thirteen (5%) of the 222 respondents who had not made a complex decision in the past anticipated having to make one in the future. Most of these decisions related to sterilization and birth control.
Figure 1 illustrates the demographic characteristics of the two groups. The groups were balanced in terms of age, education, language, employment, and income. There were differences (16–19%) in terms of gender and civil status. A higher proportion of women (72%) reported making decisions than did men (56%). More married or separated respondents reported making decisions compared to respondents who had never married.
Figure 1.
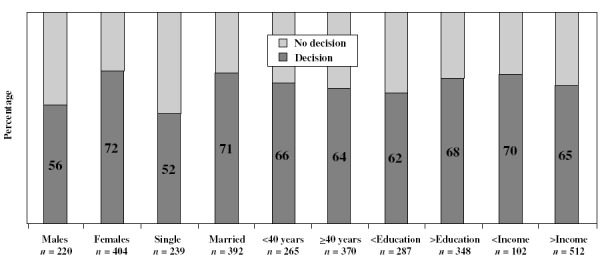
Demographic characteristics of those who reported (n = 413) or did not report decisions (n = 222).
As shown in Table 2, we classified the types of decisions reported by respondents into nine categories. The most common decisions pertained to treatments, including surgical and medical interventions. Respondents 40 years and older were more likely to report making a decision about surgery (36%, CI 30, 42) compared to those under 40 years (22%, CI 16, 29). Those reporting about a birth control decision were likely to be: (a) less than 40 years (37%, CI 30, 44) compared to 40 years and over (16%, CI 12, 22); and (b) single or never married (43%, CI 33, 55) compared to other respondents (21%, CI 17, 25). Respondents under 40 years were more likely to report about pregnancy (11%, CI 7, 17) than older respondents (1%, CI 0.4, 4). There were no statistically significant differences in the distribution of decisions by gender (Table 3).
Table 2.
Decisions discussed by respondents (n = 413)
| Decision | n | % | Decision | n | % |
|---|---|---|---|---|---|
| Surgical | 122 | 29.5 | Medication for ADHD | 6 | 1.5 |
| Circumcision | 17 | 4.1 | Pain management tx | 3 | 0.7 |
| Hysterectomy | 15 | 3.6 | Cessation of life support | 2 | 0.5 |
| Tumour removal | 13 | 3.1 | Epilepsy tx | 2 | 0.5 |
| Spinal sx | 6 | 1.5 | Dermatological tx | 2 | 0.5 |
| Angina tx | 5 | 1.2 | Diabetes tx | 2 | 0.5 |
| Prostate ca | 4 | 1.0 | Other medication | 39 | 9.4 |
| Sinus sx | 4 | 1.0 | |||
| Brain sx | 4 | 1.0 | Birth control | 100 | 24.2 |
| Foot sx | 3 | 0.7 | Methods | 47 | 11.4 |
| Kidney sx | 3 | 0.7 | Sterilization | 38 | 9.2 |
| Hernia repair | 3 | 0.7 | Abortion | 15 | 3.6 |
| Cosmetic sx | 3 | 0.7 | |||
| Joint replacement | 2 | 0.5 | Institutionalization | 24 | 5.8 |
| Transplant | 2 | 0.5 | |||
| Tonsillectomy | 2 | 0.5 | Pregnancy/childbirth | 22 | 5.3 |
| Cataract sx | 2 | 0.5 | Delivery options | 15 | 3.6 |
| Mouth/throat sx | 2 | 0.5 | Parenthood | 5 | 1.2 |
| Leg sx | 2 | 0.5 | Breast/bottle feeding | 2 | 0.5 |
| Knee sx | 2 | 0.5 | |||
| Gall bladder sx | 2 | 0.5 | Lifestyle | 21 | 5.1 |
| Elbow sx | 2 | 0.5 | Nutrition | 6 | 1.5 |
| Varicose veins | 2 | 0.5 | Weight reduction | 4 | 1.0 |
| Other sx | 22 | 5.3 | Stress management | 4 | 1.0 |
| Smoking cessation | 3 | 0.7 | |||
| Medical | 113 | 27.4 | Alcohol/drug cessation | 2 | 0.5 |
| Hormone therapy | 22 | 5.3 | Other lifestyle | 2 | 0.5 |
| Hypertension tx | 8 | 1.9 | |||
| Chemotherapy | 7 | 1.7 | Diagnostic tests | 5 | 1.2 |
| Hypercholesterolemia tx | 7 | 1.7 | |||
| Depression tx | 7 | 1.7 | Unknown | 6 | 1.5 |
| Back pain tx | 6 | 1.5 |
Table 3.
Type of decisions reported by gender (n = 401)
| Gender (n) | Total, n = 401 | Surgical, n = 122 | Medical, n = 112 | Institutionalization, n = 24 | Pregnancy, n = 22 | Birth control, n = 101 | Lifestyle, n = 21 |
|---|---|---|---|---|---|---|---|
| Male | 118 | 46 | 36 | 9 | 1 | 21 | 5 |
| Row % | 39 | 31 | 8 | 1 | 21 | 5 | |
| Confidence intervals | 0.31–0.48 | 0.23–0.40 | 0.04–0.14 | 0.00–0.05 | 0.15–0.29 | 0.02–0.09 | |
| Female | 283 | 76 | 76 | 15 | 21 | 80 | 15 |
| Row % | 27 | 27 | 5 | 7 | 28 | 5 | |
| Confidence intervals | 0.22–0.32 | 0.22–0.32 | 0.03–0.08 | 0.05–0.11 | 0.23–0.33 | 0.03–0.08 |
Shared decision‐making
Over half of the survey respondents indicated that someone other than their doctor was involved in making the decision. In most cases, this individual was the respondent's partner or spouse (63%) or another family member (27%). As shown in Table 4, the most common role adopted in decision‐making was making a choice after considering the physician's opinion (39%). Only 6% of the sample reported that the decision was made by the doctor, with or without considering the respondent's opinion. Most respondents (88%) said if they had to make the decision again, they would make it in the same way.
When we regressed demographic characteristics and decision type on independent role in decision‐making, the logistic regression model was statistically significant (P < 0.001). Being younger was associated with a more independent role (P < 0.05). When we regressed demographic characteristics and decision type on dependent role in decision‐making, the logistic regression was also significant (P < 0.001). Having less education was associated with having a more dependent role in decision‐making (P < 0.05).
Manifestations of decisional conflict (uncertainty) and contributing factors
When we asked respondents about behavioural manifestations of decisional conflict (Table 5), 59% (CI 54, 64) reported they were unsure about what to choose, the hallmark of decisional conflict. In terms of other manifestations, the majority of the respondents questioned what was important to them when making the decision (77%, CI 72, 81) and worried about what could go wrong (61%, CI 56, 66). Only one‐fourth of respondents reported wavering between the available choices (26%, CI 22, 30) or wanting to delay the decision (27%, CI 23, 32).
Two manifestations of decisional conflict appeared to be associated with the type of decision: physical stress and decision delay. Higher rates of physical stress were reported by those who had made decisions about institutionalization (54%, CI 33, 74) or medical treatment (46%, CI 37, 56), compared to those pondering birth control decisions (23%, CI 15, 33). The highest rate of decision delay was reported by those making decisions about institutionalization (50%, CI 7, 20). This rate was appreciably different from those making surgical decisions (20%, CI 16, 34).
When we examined the reported factors contributing to decisional conflict (Table 6), the overall prevalence of problems was low, with 9–27% reporting problems such as unclear values, pressure from others, or deficits in motivation, skill, support, or knowledge. However, these problems were much greater in those who had experienced uncertainty when choosing (the main hallmark of decisional conflict) than those who had not. For example, about one‐third of the uncertain group reported information deficits regarding the options, pros, and cons and their likelihood, compared with 16% of the certain group. At least one‐fourth reported social deficits such as not knowing what others decide or recommend, pressure, and lack of support. About 17–19% reported deficits in skills and readiness for decision‐making. The most frequently cited ‘other factor’ contributing to the difficulty of the decision was the highly charged emotional environment in which the decision was made. When we examined the association between decision type and each of the reported factors, more respondents making decisions about birth control felt they had the ability or skill to make the decision (95%, CI 88, 98) compared to those making decisions about surgery (80%, CI 72, 87).
When we summed the number of manifestations of decisional conflict reported by each individual, the average number of manifestations was 3.7 out of 8 (standard deviation = 2.18, range 0–8).When the number of reported manifestations of decisional conflict were regressed on factors contributing to decisional conflict and the decision type, role in decision‐making, age, education, and gender, we obtained a significant (F = 4.9; P < 0.001) multiple correlation coefficient of 0.45. Significant factors associated with higher decisional conflict included (P < 0.05): being female, not knowing enough about options, pros and cons, feeling unmotivated or unready for decision‐making, not having enough skill in decision‐making, and feeling pressure from others to select an option. Factors associated with lower decisional conflict included reporting a decision about birth control and being 70 years and older.
Decision‐making strategies and preferred information sources and delivery modes
Most respondents (>74%) reported seeking information on the pros and cons of the options and their likelihood and considered how important each of the pros and cons were in making the decision (Table 7). Over half obtained support and information on what others decide. Those who said they sought information on what others would decide or recommend most often cited their personal doctor (32%), friends (29%), other doctors (27%), or other patients (27%). Of those who stated that they would have sought other information to help them make their decision, 62% said they would have done further research on the available options.
Those making decisions about institutionalization of a family member were more likely to seek support from others in making the decision (88%, CI 67, 97) than those making decisions around birth control (56%, CI 46, 66). When asked about their preferred method of receiving information about options (Table 8), most respondents preferred to learn about the available options from their doctor (84%) and many also wanted to receive information materials (75%). Information materials were preferred by participants with more formal education (83%, CI 78, 87) compared to those with less formal education (65%, CI 58, 72). Discussion groups were preferred by more of the female participants (46%, CI 68, 81) compared to males (35%, CI 27, 44). Respondents considering surgical decisions were more likely to want to receive personal counselling from their doctor before making their decision (89%, CI 82, 94) than were those considering lifestyle decisions (57%, CI 34, 77).
Table 8.
Respondents’ preferred methods of receiving information about options
| n (%) | CI | |
|---|---|---|
| Type (n = 413) | ||
| Personal counselling from doctor | 345 (84) | 80, 87 |
| Information materials | 309 (75) | 70, 79 |
| Discussion groups of people facing the same decision | 179 (43) | 39, 48 |
| Information materials (n = 309) | ||
| Booklets or pamphlets | 270 (87) | 83, 91 |
| Internet | 147 (48) | 42, 53 |
| Videos | 145 (47) | 41, 53 |
| CD‐ROMS | 96 (31) | 26, 37 |
| Audiotapes | 59 (19) | 15, 24 |
| Other | 30 (10) | 7, 14 |
| Source (n = 309) | ||
| Medical and health‐care specialists | 267 (86) | 82, 90 |
| Societies | 196 (63) | 58, 69 |
| Community support groups | 124 (40) | 35, 46 |
| Pharmacies | 109 (35) | 30, 41 |
| Consumer associations | 95 (31) | 26, 36 |
| Government | 83 (27) | 22, 32 |
| Private companies that sell drug and health products | 63 (20) | 16, 25 |
| Insurance companies | 40 (13) | 10, 17 |
| Other | 18 (6) | 4, 9 |
Most respondents preferred receiving information materials in the form of booklets or pamphlets (87%). Internet and video informational formats were selected by nearly half of the survey respondents. When asked who should prepare these materials, most respondents selected medical and health‐care specialists (86%), followed by health‐related societies (63%). Only 27% of respondents suggested that governmental agencies should prepare the informational materials.
Evaluation criteria for judging decisions
Respondents were presented with eight criteria suggested as essential for concluding that a decision is satisfactory: knowing the main options and their pros and cons; carrying out the decision that you make; knowing how likely the major pros and cons are; being clear about which pros and cons are important to you; being satisfied with the choice you make; being satisfied with the way you make a decision; making a choice that agrees with what is personally important to you; and knowing what others decide or recommend. There was strong endorsement (>89%) for all factors except the last. When prompted for other criteria, 11% of respondents stated that feeling good about the decision was necessary and 14% felt that a positive final outcome was necessary to consider the decision satisfactory. Endorsement of these criteria did not vary by the type of decision.
Future decisions
One‐fourth (24%) of survey respondents said that they anticipated having to make another difficult health decision in the future. Of those, most stated that the decision would be about a surgical or medical treatment (61%) or the institutionalization of a family member (15%).
Discussion
This first survey of Canadians’ decision‐making needs indicates that the majority of Canadians have faced complex health decisions, commonly about medical or surgical treatments or birth control. Complex decisions are reported more frequently by women and married or separated individuals. Most Canadians take an active role in their decisions, usually considering their physicians’ opinions, and often sharing the process with their partner or family. Physicians are more involved in decision‐making when individuals are less educated. The majority facing complex decisions experience decisional conflict, commonly manifested by expressing uncertainty about what to choose, questioning personal values, and worrying about undesired consequences of options. Reported difficulties in decision‐making are less common in those considering birth control options and those 70 years of age and older and more common in those who are female, and feeling uninformed about options, pressured to select a particular option, and unready for or unskilled in decision‐making. Canadians use several strategies when deliberating about choices including information gathering, values clarification, and seeking support and information from others. Their preferred methods of learning about options are personal counselling and information materials. Information materials are most commonly preferred in print from credible experts. Essential criteria for judging satisfactory decision‐making include: having sufficient knowledge about the options, outcomes, and probabilities; being clear about values; selecting and implementing a choice that agrees with personal values; and expressing satisfaction with the choice.
Limitations
These results need to be examined in light of several study limitations. First, there was a relatively high refusal rate and some imbalance in sample characteristics. There was an 11–14% over‐representation of female, better educated, and married/separated respondents who are more likely to be at home or to participate in surveys. 5 We also had some difficulty encouraging participants to differentiate between complex health decisions and complex health experiences over which they perceived no choice. Thus, the rates of reported decisions may be slightly overestimated and the rates of decision difficulty slightly underestimated. Moreover, we cannot conclude that non‐participants in the survey experienced decisions in the same proportion and in the same manner as participants. The refusal rate may be attributed to the involved and personal nature of the survey topic.
The survey results may also be limited by bias in participants’ reporting of decisions that are socially acceptable. For example, this may have played a role in the lower rates of decisions about birth control in single individuals and in the strong endorsement of criteria for evaluating decisions. Recall bias may have also played a role as respondents were asked to recall details about decisions that may have been made several years earlier. However, this may have been mitigated by the importance of the decisions they faced. Finally, hindsight bias may have affected responses as respondents reported their experiences of decision‐making after they had experienced the outcomes of those decisions.
Decision‐making needs
We have identified several modifiable determinants in our framework that are sub‐optimal for decision‐making, with particular groups expressing more difficulties than others. The proportion expressing decisional conflict (uncertainty) was high (59%) and comparable to rates reported in other regional surveys and prospective clinical cohorts of individuals facing complex decisions. 3 , 6 Several of the factors associated with decisional conflict (social pressures, deficits in knowledge, readiness, and decision‐making skills) that have been observed in clinical studies 3 , 7 are now confirmed in this population survey for a broader range of decisions. Many of these factors that lead to sub‐optimal decision‐making are amenable to decision‐supporting interventions such as decision aids. Decision aids are adjuncts to counselling that provide: (a) evidence‐based and tailored information about options, outcomes, and probabilities; (b) exercises for clarifying personal values; (c) examples of how others make decisions; and (d) guidance and coaching in the skills of shared decision‐making. Recent reviews of their efficacy 8 , 9 indicate that decision aids improve knowledge of options and outcomes; create realistic perceptions of the likelihood of outcomes; reduce decisional conflict; and promote more active involvement in decision‐making without increasing anxiety. Several decision aids 10 have been developed on topics such as medical or surgical treatments, screening or diagnostic tests, preventive therapies and clinical trial participation. However, these decision aids have not yet been distributed widely to the public.
The decision to seek institutional care for a family member was the most common single decision next to birth control and was commonly reported by participants anticipating future decisions. This decision resulted in the greatest decisional conflict as manifested by delay and physical stress. This observation has been confirmed in a prospective study of caregivers’ decisions for family members with dementia. 11 Current efforts to develop better decision‐support tools for this difficult choice are in progress to meet the needs of the population who anticipate making this decision in the future.
Women's needs
Policies devoted to improving the decision‐making of the population need to focus on women because they report more decisions with more difficulty. The higher rates of reporting complex decisions may be explained by the longer period they use health services, beginning earlier with reproductive services and lasting longer because of a greater lifespan. Moreover, women commonly serve as gatekeepers to the health of their families, in which they take prime responsibility for the health‐care of their children and ageing relatives. Our finding of higher decisional conflict scores in women is consistent with the findings of a randomized trial of men and women who were exposed to decision aids and who had comparable post‐decision aid knowledge scores. 12 Even when other potential confounders were controlled (age, health status, and education), gender exerted an independent effect on decisional conflict. 12 The reasons behind the gender differences need to be examined. For example, are women more likely to express difficulties or do their social roles pose different sets of problems for them compared to men? A final issue is the delivery of decision support to women. More women reported a preference for discussion groups.
Need of individuals with less formal education
Those with less formal education reported more difficulties making decisions and relied more on physicians to advise them in decision‐making. They also preferred to rely less on written materials. Degner and others 13 , 14 have confirmed that those with less education are less likely to take an active role in treatment decision‐making. Nevertheless, decision‐support interventions do improve knowledge, decisional conflict and distress among those who are less educated. 15 , 16 , 17 These interventions need to be delivered in a manner acceptable to the group and to take into account preferences for participation in decision‐making.
Needs of older people
Degner and Russell 13 have found that older participants are less likely to take an independent role for cancer decisions, compared to their younger counterparts. Part of this may be a cohort effect where in the past the common practice was to defer to authorities. Another plausible explanation is the complexity of the clinical issues (e.g. co‐morbidity, increased risk of complications) and instrumental support that need to be considered when a senior faces treatment options compared to younger individuals. In this particular survey, the types of decisions may have played a role, in that younger participants reported more reproductive decisions.
The lower decisional conflict scores among seniors 70 years and older was surprising and inconsistent with a study of older people considering treatments for atrial fibrillation, 12 which showed higher scores among older participants, even when other potential confounders were controlled (gender, health status, and education). The possible reasons for lower decisional conflict in those 70 years and older may be because of the larger number in this age group who had their doctors make the decision for them. With lower responsibility for decision‐making, there may have been less decisional conflict.
Evaluation criteria
Identifying appropriate criteria for evaluating decisions is a challenge when the best choice depends on personal situations and personal valuing of benefits vs. harms. Nevertheless, in this study, there was uniform endorsement of most criteria we presented and remarkable uniformity across decision types. Moreover, the opinions of participants in this survey are comparable with opinions of physicians and researchers in decision‐making. Opinions expressed by others in essays or surveys 2 , 18 , 19 , 20 indicate consistent agreement that decisions should be informed and compatible with personal values and some agreement that consumers should express satisfaction with the decision‐making process and should implement the choice.
Conclusions
The majority of Canadians face challenging decisions regarding their health at some time in their life and the majority of these experience difficulties making these choices. Decision‐support strategies need to be deployed to address the unmet needs of people who feel uninformed, pressured, unready, and unskilled in decision‐making. Particular efforts should be devoted to the decision‐making needs of women and individuals with less formal education.
Acknowledgements
This project was supported by the Medical Research Council of Canada. Annette O'Connor held an Ontario Ministry of Health Career Scientist Award and Andreas Laupacis held an MRC Scientist Award. The questionnaire was designed with the input of our decision scientist advisory panel comprising the following individuals: Michael Barry, Michael Brundage, James Dolan, Deb Feldman‐Stuart, Floyd Fowler Jr., Margaret Holmes‐Rovner, Hilary Llewellyn‐Thomas, Robert Nease Jr., and Anne Stiggelbout. We appreciate the helpful comments of the anonymous reviewers.
References
- 1. Health Canada, Statistics Canada , Canadian Institute for Health Information. Health Information Needs in Canada. Ottawa: Health Canada, 1998. [Google Scholar]
- 2. O'Connor AM, Tugwell P, Wells GA et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Education and Counseling, 1998; 33: 267–279. [DOI] [PubMed] [Google Scholar]
- 3. O'Connor AM, Drake ER, Fiset V, Graham ID, Laupacis A, Tugwell P. The Ottawa Patient Aids. Effective Clinical Practice, 1999; 2: 163–170. [PubMed] [Google Scholar]
- 4. Statistics Canada. Canadian Statistics , 1999. Available from: URL: http://www.statcan.ca/english/census96/nation.htm.
- 5. Dillman DA. Mail and Telephone Surveys: the Total Design Method. New York: John Wiley, 1978. [Google Scholar]
- 6. Lange I, Campos MS, Urrutia M et al Decision making needs of low income Chilean women. Poster presented at the International Society of Technology Assessment in Health Care, 2023 June 1999, Edinburgh, Scotland (abstract #P470, p. 130).
- 7. O'Connor AM. Validation of a decisional conflict scale. Medical Decision Making, 1995; 15: 25–30. [DOI] [PubMed] [Google Scholar]
- 8. O'Connor AM, Rostum A, Fiset V et al. Decision aids for patients facing health treatment or screening decisions: a Cochrane systematic review. British Medical Journal, 1999; 319: 731–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Molenaar S, Sprangers MAG, Postma‐Schuit FCE et al. Feasibility and effects of decision aids. Medical Decision Making, 2000; 20: 112–127. [DOI] [PubMed] [Google Scholar]
- 10. O'Connor AM, Fiset V, DeGrasse C et al. Decision aids for patients considering health care options: evidence of efficacy and policy implications. Journal of the National Cancer Institute Monograph, 1999; 25: 67–80. [DOI] [PubMed] [Google Scholar]
- 11. Comeau C. Evaluation of a decision aid for family members considering long term care options for a relative with dementia. MScN thesis, University of Ottawa, Ottawa, 2001. [Google Scholar]
- 12. Man‐Son‐Hing M, Laupacis A, O'Connor AM et al. A randomized trial of a decision aid for patients with atrial fibrillation. Journal of the American Medical Association, 1999; 282: 737–743. [DOI] [PubMed] [Google Scholar]
- 13. Degner LF, Russell C. Preferences for treatment control among adults with cancer. Research in Nursing Health, 1988; 11: 367–374. [DOI] [PubMed] [Google Scholar]
- 14. Blanchard CG, Labrecque MS, Ruckdeschel JC, Blanchard EB. Information and decision‐making preferences of hospitalized adult cancer patients. Social Science and Medicine, 1988; 27: 1139–1145. [DOI] [PubMed] [Google Scholar]
- 15. Lerman C, Biesecker B, Benkendorf JL et al. Controlled trial of pretest education approaches to enhance informed decision‐making for BRCA1 gene testing. Journal of the National Cancer Institute, 1997; 89: 148–157. [DOI] [PubMed] [Google Scholar]
- 16. Grant C, Laupacis A, O'Connor A, Rubens F, Robblee J. Evaluation of a decision aid for patients considering autologous donation of blood before open heart surgery. Canadian Medical Association Journal, 2001; 164: 1139–1144. [PMC free article] [PubMed] [Google Scholar]
- 17. Dunn RA, Shenouda PE, Martin DR, Schultz AS. Videotape increases parent knowledge about poliovirus vaccines and choices of polio vaccine schedules. Pediatrics, 1998; 102: 26. [DOI] [PubMed] [Google Scholar]
- 18. O'Connor A, Llewellyn‐Thomas H, Sawka C, Pinfold S, To T, Harrison D. Physicians’ opinions about decision aids for patients considering systemic adjuvant therapy for axillary‐node negative breast cancer. Patient Education and Counseling, 1997; 30: 143–153. [DOI] [PubMed] [Google Scholar]
- 19. What is a good decision? [Editorial]. Effective Clinical Practice, 1999; 2: 185–200. [PubMed] [Google Scholar]
- 20. Entwistle VA, Sowden AJ, Watt IS. Evaluating interventions to promote patient involvement in decision‐making: by what criteria should effectiveness be judged? Journal of Health Services Research and Policy, 1998; 3: 100–107. [DOI] [PubMed] [Google Scholar]


