Zoë Lawrence MBA
Office of the Director for Patients and the Public, Department of Health, Quarry House, Quarry Hill, Leeds LS2 7UE, UK. Email: zoe.lawrence@doh.gsi.gov.uk
Introduction
A recent consultation on choice 1 conducted by the Department of Health signifies that patient choice in England is a reality, and that the general public should not be underestimated in their understanding of community needs or issues around balancing the use of resources. This article describes the process through which this national consultation was carried out, describes key findings and considers some of the implications of these findings.
Background
From August 2004 people in the UK waiting more than 6 months for surgery will be offered faster treatment at an alternative hospital. From December 2005 patients who may require surgery will be offered a choice of four to five hospitals at the point the GP refers them to hospital.
Given these recent Government targets, many managers in the UK's National Health Service (NHS) will see patient choice as choice of hospital at the point of referral. Either that or when choice and public services are mentioned in the same sentence it can be considered to be an uncomfortable relationship – one that possibly cannot happen in a tax‐funded system of limited resources, and one that is unable to uphold the founding NHS principle of equity for all.
The notion of extending choice has been in the background of UK health policy for some time. Being able to exercise choices about treatment and care is a key element of a good patient experience, and the bedrock of good clinical practice which is well documented elsewhere. Achieving this needs a cultural shift, which has already begun, and is what the Choice Consultation aimed to facilitate. The consultation asked what choices patients want and what information they would need to exercise those choices.
A national consultation
The process was initiated by Dr John Reid, the Secretary of State for Health, in his speech in July 2003. 2 Dr Reid said:
I am inviting the nation's patient groups to work with us over the next three months and beyond to work up radical proposals on how best to empower patients…. I have in mind the same sort of process used to develop the NHS Plan in which we worked intensively with the public and key stakeholders.
Harry Cayton, the Director for Patients and the Public at the Department of Health, was asked to lead this consultation exercise to find out what choices patients want. The result was a Command Paper entitled Building on the Best that was published on 9 December 2003 1 .
The consultation exercise consisted of four strands:
-
•
A national consultation led by eight task groups. The task groups had a majority of service users on each, but also included clinicians and managers from health and social care. The eight themes were: maternity, children, primary care, emergency care, planned care, mental health, long‐term conditions and older people. The groups intended to map out the patient journey and to work across organisational and professional boundaries, rather than look at disease‐specific groups.
-
•
Local consultations and events for the public and NHS staff led by Strategic Health Authorities.
-
•
A choice consultation survey for the public, staff, patients, users and carers to contribute their individual ideas and views directly.
-
•
Consultation with patient and professional organisations, the voluntary and independent sector, and other stakeholders.
The consultation reached at least 110 000 people, and while it does not claim to be systematic, or totally comprehensive, it has provided a significant level of consensus that choice in the NHS is a good thing, and it is what service users want.
What did they say?
It is interesting that the current political push on choice is the choice of hospital at the point of referral. This type of choice was not one of the louder messages heard through the consultation. As a result this only takes up a small proportion of the overall outcomes. People want accessible, good quality service at convenient locations. Many of the choices identified can be delivered through a change in behaviour, and are not dependent on increasing capacity. The other main messages that came from the consultation were that the public want:
-
•
to be more involved in decisions about their care;
-
•
to have more and better information to help them make decisions and choices about their care and treatment; and
-
•
to have services shaped around the needs of patients instead of patients being expected to fit the system.
Figure 1 was constructed from the responses to the consultation. It begins at the base with enablers to choice – information relationships and self‐management, followed by service and access choices to primary and secondary care. Ending with personal individual treatment choices to reach the desired health outcome or quality of life expectation. This figure not only puts the choice of hospital in its place but also is useful in showing the extent of choice in health. This figure is not included in Building on the Best but illustrates the document's remit.
Figure 1.
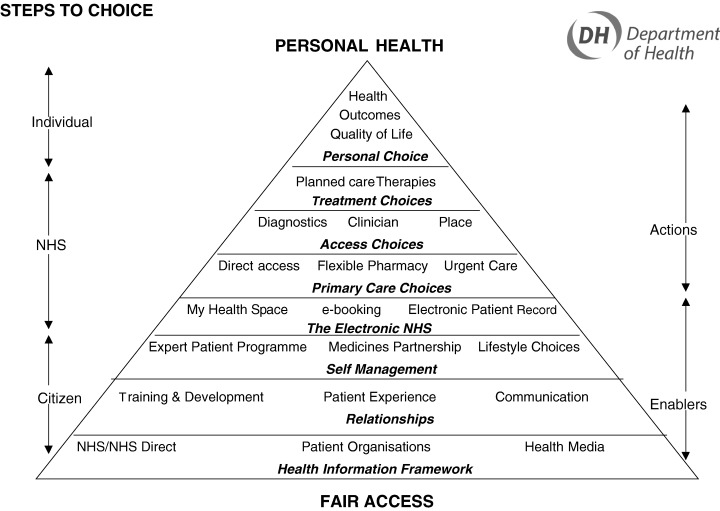
Steps to choice: the above figure shows the extent of the choice consultation. It is significantly more than choice of place for elective care.
These findings may appear nothing new in themselves and are what could have been expected from this sort of exercise. However, it is of value to have these messages confirmed in a consultation exercise principally with patients, service users and the public. The Government now has real evidence about what patients want from their health service.
The command paper – building on the best
The results of the consultation were published in a Command Paper Building on the Best – Choice, Responsiveness and Equity in the NHS in December 2003. It took this title because just about all the ideas generated through the consultation were already happening somewhere in the country. The document includes a number of examples of best practice to try to show that enabling choices is not that difficult and that NHS organisations may be doing it already but not actually realising it. Also if it is being done somewhere, it shows it is possible and transferable.
Building on the Best is different to other policy documents the Department of Health usually publishes. It is not about implementing new initiatives with timescales and targets to be met. It contains very little by way of direct instruction to health service managers. This document is about cultural change, a change in people's behaviours – behaviours of patients and NHS staff. Patients should see the service as their service. They should feel enabled to be involved not only in choices about services, but also in choices about their treatment and care. NHS staff also need to see patients differently. They are not a burden or just part of a process of care. Patients are individuals and have something of value to offer the healthcare encounter. All these amount to a new relationship between patients and the NHS. One where the NHS involves patients and users, listens to what they have to say and then acts.
But how can a document change behaviour? It can signal an intention and begin to obtain the desired notions in people's thinking. It shows how patient choice can be extended beyond the initial concept of choice of hospital – which in some areas people are having difficulty in understanding. It also suggests actions that will impact on behaviours. For example, the simple action of copying letters to patients alters the doctor–patient interaction to one that is more open and inclusive.
Building on the Best is also explicit that choices should be available to all and the NHS needs to make more effort to ensure this happens, especially including the most disadvantaged and marginalised groups. Extending choice to everyone – not just the white middle classes could help reduce health inequalities. We already have evidence that patient and public involvement improves health outcomes and well being 3 – exercising choice is part of that.
The crunch point is that all choices, whether in a market or healthcare environment, are based on information. In the absence of information there are no choices. The delivery of Building on the Best is dependent on information. Information must start with asking what patients want and need to know – it should not be assumed. It has to be driven by local people in partnership with local stakeholders.
Supporting resources
Building on the Best is available for downloading from the Department of Health website http://www.doh.gov.uk/choiceconsultation. The report's subtleties may be considered powerful and its arguments convincing. It contains examples of best practice, which in most cases can be easily transposed into other settings. On the website there is also a powerpoint presentation which can be used to present the main points of the document.
The reports from the task groups, mentioned above, are also available on the website, one for each of the eight themes. The detail may be of specific interest for people working in each of the related areas. The main themes from each of these were included in the Command Paper, but it was impossible to include all the recommendations of each group.
Conclusion
Building on the Best signals a new era in health services. It may look like another Department of Health policy document on the outside but its contents are quite different, e.g. there are no targets and no must dos. It aims to set the cultural scene of a modern health service. Cultural change will not happen solely because of this document. Culture is after all an elusive commodity. But as with all things we have to begin somewhere. This is about shifting the balance of power, away from politicians, and into the arms of patients and citizens, who then need to learn how to use it to its fullest capacity to make the health service, a service we all want.
References
- 1. Department of Health . Building on the Best – Choice, Responsiveness and Equity in the NHS. London: The Stationery Office, 2003. [Google Scholar]
- 2. Secretary of State for Health . Speech to the New Health Network, 16 July 2003. [Google Scholar]
- 3. Department of Health . Patient and Public Involvement in Health: the evidence for policy implementation, 2004. [Google Scholar]


