Abstract
Background Although patients are increasingly involved in agenda setting within specific fields of health research, they rarely participate in decision‐making on the entire breadth of health research, including biomedical research. This might be attributable to a widely held view that patients are incapable of adequate research prioritization due to a lack of relevant knowledge, a failure to look beyond their own individual problems or an inability to objectively consider long‐term targets.
Aims By conducting transparent and structured consultations with asthma and chronic obstructive pulmonary disease (COPD) patients regarding their health research priorities, we aim to assess the ability of patients to prioritize research in a well‐argued way.
Methods Patients were consulted through seven focus groups, a feedback meeting, and a questionnaire. The focus groups and the feedback meeting aimed to explore the entire breadth of patients’ problems experienced in relation to their diseases, while the questionnaire aimed to investigate patients’ prioritization of possible research targets focused on solving these problems.
Results The focus groups produced a wide range of problems, including those related to health‐care organization, social environment, therapy and costs. In terms of research prioritization, patients focused primarily on biomedical issues, particularly aetiology, co‐morbidity and effective medication.
Conclusions The consultation procedure successfully elicited patients’ research priorities including the underlying arguments. Our results indicate that asthma and COPD patients are capable of research prioritization in a well‐argued way and that they highly value biomedical research. Furthermore, as they prioritized some research topics that are not covered by current Dutch research programmes, we argue that patient participation can broaden research agenda setting.
Keywords: asthma, consultation, chronic obstructive pulmonary disease, patient participation, research agenda setting, research priorities
Introduction
In the last decade, patients have increasingly become involved in decision‐making on certain types of health research, namely public health research, health services research and clinical research. 1 , 2 , 3 , 4 , 5 Often‐mentioned arguments in favour of patient involvement refer to the enhanced legitimacy of the decision‐making process or to the substantive contribution patients could make to decision‐making outcomes. In spite of these arguments, patients continue to hold little influence in agenda setting concerning the entire breadth of health research, including biomedical research. 1 This is largely because many practitioners have strong reservations about patients’ abilities to prioritize research topics in a well‐argued way, particularly when biomedical issues are involved.
In previous studies on this subject, 6 , 7 many of our interviewees (both researchers and patients) held that patients should not contribute to decision‐making on biomedical research agendas for various reasons. It was argued that patients:
-
•
lack essential knowledge about research issues and procedures;
-
•
do not speak nor understand scientific language;
-
•
are unable to put their own questions and demands into a scientific context;
-
•
have unrealistic expectations of scientific research;
-
•
are strongly influenced by the media;
-
•
are unable to abstract from their own individual situation;
-
•
have difficulty to think in long‐term targets; and/or
-
•
are only interested in subjects concerning care or social issues.
As a result, many concluded that patient involvement in overall health research agenda setting would either be useless or result in an undervaluing and subordination of biomedical research.
Until now, available literature on the subject, such as systematically reviewed by Oliver et al., 4 hardly provides evidence concerning the tenability of above‐mentioned presuppositions. Reports on patient consultations concerning research priorities often concern a restricted field of health research only, or do not distinguish patients’ priorities from the priorities of professionals. 4 But even if many of the above‐mentioned pre‐suppositions can be substantiated, it may be unfair to conclude that patient participation in overall health research agenda setting is useless and undesirable. Scientific knowledge, for example, may not always be a necessary prerequisite for useful participation. Indeed, patients may possess other types of knowledge of value and relevance to research agenda setting, as is argued by several scholars. 8 , 9 , 10 According to these scholars, a distortion of research priorities due to the inclusion of patients’ knowledge can be positive, because this broadening of prioritization can counter potential biases of scientists and health‐care professionals.
Therefore, the objective of this study is to gain greater insight into whether patients can prioritize health research topics in a well‐argued way and can make relevant contributions to current health research agendas. This was achieved by consulting patients for their health research priorities in an explicit and transparent way.
This study was undertaken within the framework of a larger project on interactive agenda setting concerning asthma and chronic obstructive pulmonary disease (COPD) research in the Netherlands that took place from July 2003 to July 2004. The project was executed by the Athena Institute for Research on Communication and Innovation in Health and Life Sciences of the Vrije Universiteit Amsterdam, which had previous experience in developing and implementing interactive and participatory methodologies. 11 , 12 The Netherlands Asthma Foundation (NAF) commissioned the project with additional financial support of the Netherlands Organisation for Health Research and Development (ZonMw). The results of the project would provide an important input for the formulation of research programmes of NAF and ZonMw for the period 2005–08.
The NAF is both a research funding agency and a patients’ organization focusing on asthma and COPD. At the moment, it funds different types of health research within the context of two research programmes. The Experimental and Descriptive Research (EBO) programme focuses on knowledge production concerning the causes and mechanisms of asthma and COPD, with the long‐term aim to innovatively contribute to optimal prevention and therapy. 13 The Care and Prevention (Z&P) programme finances applied research focusing on the direct advancement of prevention and health‐care quality for asthma and COPD patients. 14 ZonMw, the Dutch medical research council, also funds applied research on asthma and COPD within their Health Promotion and Disease Prevention Programme (http://www.zonmw.nl/index.asp?s=7637).
Methods
From September 2003 to February 2004 we consulted asthma and COPD patients about their priorities on asthma and COPD research using a triangulated strategy. Focus groups were conducted to explore the entire breadth of, and to gain insight into, patients’ problems concerning living with asthma/COPD. A subsequent questionnaire explicitly focused on possible research targets that aspire to solve those problems identified in the focus groups, while making final results more quantitative and representative for the entire patient community. In many consultation studies, focus groups are only used as a preliminary tool to design a subsequent questionnaire. 15 , 16 , 17 However, our focus groups had the additional objective of providing insight into perspectives and arguments that underlie patients’ priorities.
Our research team consisted of: (i) four Athena Institute staff members (including JFCF, JEWB and JT) who were responsible for the design, execution and analysis of the whole process, (ii) three MSc students who assisted in the process as trainees and (iii) six MSc students who were involved in the design, execution and analysis of the focus groups as part of a course on interactive research methodologies. Participants of both focus groups and questionnaire were all NAF members, selected on their willingness to participate.
Focus groups
In September 2003 we organized three workshops in three different regions, geographically spread across the country. Each workshop included a plenary introduction, two or three parallel focus groups, and a plenary discussion of preliminary focus group results. From the three regions, 61 patients 2 participated in seven focus groups of seven to 11 persons each. All focus groups involved a majority of women (42 in total) and the average age was 56 years. More asthma patients than COPD patients were involved. Table 1 shows the distribution of participants among age categories and diseases.
Table 1.
The distribution of focus group participants along sexes, age categories and diseases
| Focus group* | Total number of participants | Sex | Age (years) | Disease | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 0–15 | 16–30 | 31–45 | 46–60 | 61–75 | 76+ | Asthma | COPD | Asthma and COPD | Patient relatives | ||
| A1 | 7 | 2 | 5 | 0 | 1 | 1 | 4 | 1 | 0 | 3 | 2 | 0 | 2 |
| A2 | 7 | 1 | 6 | 0 | 0 | 2 | 3 | 1 | 1 | 3 | 1 | 2 | 1 |
| L1 | 8 | 2 | 6 | 0 | 1 | 3 | 2 | 2 | 0 | 4 | 2 | 1 | 1 |
| L2 | 8 | 4 | 4 | 0 | 0 | 0 | 3 | 4 | 1 | 3 | 2 | 3 | 0 |
| H1 | 11 | 3 | 8 | 0 | 1 | 3 | 4 | 2 | 1 | 6 | 2 | 2 | 1 |
| H2 | 10 | 3 | 7 | 0 | 1 | 2 | 2 | 1 | 4 | 7 | 2 | 1 | 0 |
| H3 | 10 | 4 | 6 | 0 | 0 | 1 | 1 | 5 | 3 | 2 | 7 | 1 | 0 |
| Total | 61 | 19 | 42 | 0 | 4 | 12 | 19 | 16 | 10 | 28 | 18 | 10 | 5 |
| Total (%) | 100 | 31 | 69 | 0 | 6 | 20 | 31 | 26 | 16 | 46 | 30 | 16 | 8 |
*The letters refer to the locations of the different focus groups.
A, Amsterdam; L, Leusden; H, Haren; COPD, chronic obstructive pulmonary disease.
Our focus group design was standardized and averagely structured. 18 Each focus group had a moderator, who guided the discussion using six pre‐established questions and exercises, and a monitor, who observed the group dynamics and recorded notes of the proceedings. Focus group discussions were recorded on video and cassette for further analysis. During the first part of each focus group session, patients were asked to discuss disease‐related problems they experience in daily life. 3 In the second part of the session, patients were asked to collectively prioritize the listed problems by negotiation and distribution of urgency points. The main purpose of this prioritization exercise was to generate discussion and elicit explicit arguments that underlie each problem. Finally, each focus group identified specific research questions. At the end of each plenary closing session, feedback forms were distributed. Reports of the discussions were sent to all participants for feedback.
Focus group discussions were analysed by searching the tape‐recordings for mentioned causes of, and mutual relations between, identified problems. All problems, causes and mutual relations mentioned were logically analysed in a so‐called ‘causal tree’. 19 In November 2003, an additional feedback meeting was conducted in order to verify the focus group results. The group of participants (27) consisted of 17 women and 10 men of whom 11 were asthma patients, 12 suffered from COPD, three from both diseases and one was a parent of an asthma patient. The average age of these participants was 63. The main focus of the feedback meeting was to check and complete the causal tree. For this purpose, participants were divided into three groups of eight to 10 persons, each of which focused on a different part of the overall causal tree. Based on the results of this meeting the causal tree was finalized.
Since people below 30 years of age and seriously ill patients were underrepresented in both the focus groups and the feedback meeting, we held four in‐depth interviews with three younger asthma patients and a seriously ill COPD patient. We discussed their main health problems to determine variance with problems of the other participants.
Questionnaire
In order to obtain a quantitative view of patients’ priorities on potential health research topics, the results of the focus groups were used to design a questionnaire. For this purpose, all problems identified in the focus groups were clustered and translated into seven categories of six potential research targets that imply the solution of the problems. The categories included: finances, emotions, social environment, primary care, specialist care, other forms of care and knowledge on aetiology and drugs. These categories roughly reflect the variety of problem fields that emerged during the focus groups (see Fig. 1). An identified problem can be regarded as reflecting (i) a lack of effective solutions, or (ii) a lack of adequate implementation strategies. As health research could focus on the acquirement of knowledge for both the development and implementation of health interventions, we argue that each identified problem reflects a potential target for health research.
Figure 1.
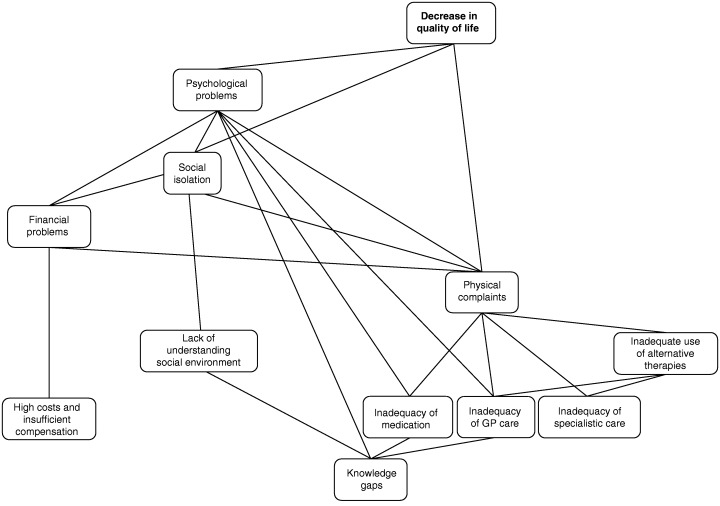
Highly simplified version of the causal tree reflecting problem(cluster)s experienced by asthma and chronic obstructive pulmonary disease (COPD) patients and their mutual relations.
The questionnaire consisted of three blocks of questions. The first block focused on demographic characteristics of respondents. The second and main block involved the prioritization exercises, requesting respondents to divide a maximum number of points among different wishes (a variant of the ‘budget pie’ method). 20 The third block focused on the views of respondents concerning patient participation in decision‐making on research. In the last block, respondents were encouraged to indicate any omissions in the questionnaire, and to give comments.
A draft version of the questionnaire was tested by 15 asthma/COPD patients and subsequently slightly adapted. For our analysis we needed at least 200 filled‐in questionnaires. As previous experience of the NAF indicated an average response of about 25%, we sent the questionnaire to 1000 patients, randomly selected from the entire pool of NAF members, and to 42 patients who had participated in the focus groups or the feedback meeting and had indicated a willingness to participate in a questionnaire. In addition, the questionnaire was placed on the Internet site of the NAF. In order to check possible differences in priority setting between NAF members and asthma/COPD patients who are not NAF members, we also distributed questionnaires among non‐members via various hospitals, physiotherapy practices and a respiratory rehabilitation centre in Amsterdam. Questionnaire results were analysed in a stratified way in order to identify possible influences of disease‐related or demographic characteristics on research priorities.
Results
Focus groups
The results of the focus groups consisted of a causal tree of mutually related problems and causes, a list of prioritized problems, and a list of patients’ questions and suggestions for research. In Fig. 1 a simplified version of the overall causal tree of patient problems is depicted. At the highest level there are four problem fields: psychological problems, social isolation, physical complaints and financial problems. Problems with inadequacies of health‐care (both primary care and specialist care) contribute to a large cluster of problems that eventually result in physical and psychological problems. A small additional cluster is created by a lack of knowledge about the aetiology of the diseases and the lack of effective drugs, also eventually resulting in physical and psychological problems.
During the prioritization sessions in the focus groups, two problems consistently received more than twice as many urgency points as other problems: side‐effects of medication and hypersensitivity for all kinds of substances, such as smoke, perfumes, dust and damp. Table 2 lists all problems prioritized during the focus groups and their urgency scores. Problems that were added during the feedback meeting include the lack of (deployment of) asthma nurses as coaches and mediators in health‐care, the lack of attention of specialists for psychological aspects of the diseases, and the non‐recognition of physical causes of some complaints by medical doctors.
Table 2.
Patients’ problems prioritized during the focus groups
| Rank | Problem | Score |
|---|---|---|
| 1 | Side‐effects of medication | 27 |
| 2 | Hypersensitivity for all kinds of substances, such as smoke, perfumes, dust, damp, etc. | 23 |
| 3 | Insufficient coaching and follow‐up with drug use by professionals | 11 |
| 4 | (Obscurity of) long‐term side‐effects of medication | 10 |
| 5 | Obscurity of causes of disease or individual attacks | 9 |
| 6 | Interference with social life | 9 |
| 7 | Co‐morbidity | 7 |
| 8 | Inadequate information and uncertainty on drug use | 7 |
| 9 | Fatigue | 6 |
| 10 | Lack of knowledge among general practitioners and pharmacists | 6 |
| 11 | Inadequate collaboration of health‐care professionals | 4 |
| 12 | High costs for medication, aids and house adaptation | 4 |
| 13 | Non‐understanding by social environment | 3 |
| 14 | Non‐understanding at school and work | 3 |
| 15 | Feelings of grief and frustration about physical constraints and social isolation | 3 |
| 16 | Little attention for alternative therapies in health‐care | 3 |
| 17 | Lack of patients’ empowerment | 2 |
| 18 | Inadequate collaboration between regular and alternative medicine | 2 |
| 19 | Non‐understanding by professionals | 2 |
| 20 | Inconvenience of drug use | 2 |
The score refers to the number of ‘urgency points’ (paperclips) allocated to the problem by the participants.
The interviews with young asthma patients indicated a common set of problems, but a different rate of urgency in relation to older patients. For example, the interviewees gave higher priority to the fear of a sudden asthma attack during social activities and the insufficient knowledge of, and information from, general practitioners. The interview with the seriously ill COPD patient indicated no additional problems.
Patients’ input on specific research questions concerned the causes of the diseases, co‐morbidities and options for the improvement of treatment and of interaction between patients and their environment. Patients’ suggestions for action targeted the improvement of health‐care, prevention and care organization.
On the evaluation forms, a large majority of the participants indicated that the workshop had met their expectations. Main suggestions for improvement included shortening the time‐scheme, using a more convenient location, providing more information beforehand, inviting a research professional who could answer questions, and realizing a better representation of male and young patients. In addition, many participants suggested that the NAF should organize similar meetings on a regular basis.
Questionnaire
From the 1042 questionnaires sent by mail, 244 patients responded (23.4% response of which 63% female and 36% male). In addition, six patients filled‐in the questionnaire from the Internet. Fig. 2 shows the distribution of respondents according to age, educational level and disease. Equal numbers of respondents suffered from asthma and COPD. Of the asthma patients, 17% regarded the degree of their disease as serious, while this was 42% among COPD patients. The median age of respondents was between 46 and 60. However, the average ages within different types of patients varied; while many respondents with COPD were above 60, respondents with asthma were often younger. Finally, most respondents had received lower secondary education, but middle and higher educated people were also amply represented. Although NAF's membership includes twice as many asthma patients as COPD patients, 21 the other characteristics of our respondents roughly corresponded with the results of an earlier investigation on the demographic characteristics of NAF members. 22 They also corresponded with characteristics of asthma and COPD patients in general, as investigated in a national study by the Netherlands Institute for Health Services Research. 23
Figure 2.
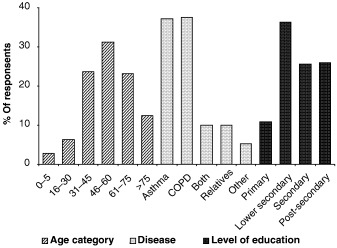
Distribution of questionnaire respondents along age categories, diseases and levels of education.
Table 3 shows the 15 highest priorities 4 of patients. Patients prioritized research on the aetiology of asthma/COPD, co‐morbidity and effective medication above research on health‐care or social issues. One might assume that this is the result of calculating the means because not all patients will experience, for example, problems with their general practitioners, specialists or social environment, while they will all experience the obscurity of the origin(s) of their diseases and the inadequacy of medication. Further investigation of questionnaire results, however, showed that about 50% of the respondents prioritized biomedical issues higher than other issues on an individual basis.
Table 3.
Patient priorities concerning potential research targets as resulting from the questionnaire
| Rank | Potential research target | Final score |
|---|---|---|
| 1 | More knowledge on the origins of asthma/COPD | 11.6 |
| 2 | New and more effective drugs | 11.3 |
| 3 | More knowledge on the relation between asthma/ COPD and other diseases (co‐morbidity) | 9.8 |
| 4 | Drugs that have less side‐effects | 9.4 |
| 5 | More knowledge on the mutual interaction of drugs | 6.3 |
| 6 | The adaptation of governmental rules concerning public places and workplaces | 5.6 |
| 7 | More compensation for medication and aids | 4.9 |
| 8 | Reduction of contributions for health insurances | 4.4 |
| 9 | Improvement of understanding and consideration by family and friends | 4.0 |
| 10 | Reduction of physical complaints that hamper daily life functioning | 4.0 |
| 11 | Reduction of fear for hypersensitivity and/ or symptoms during activities outside | 4.0 |
| 12 | Compensation of costs for house adaptation | 3.6 |
| 13 | Knowledge on effects and efficacies of alternative therapies* | 3.5 |
| 14 | Compensation of costs for activities | 3.4 |
| 15 | More time and understanding by general practitioners | 3.4 |
Final scores refer to the average score given by all respondents.
*Alternative therapies or complementary therapies comprise all kinds of non‐traditional therapies, including homeopathy, orthomolecular medicine, yoga, breathing therapy, movement therapy, etc.
COPD, chronic obstructive pulmonary disease.
A stratified analysis of questionnaire results indicated that neither sex nor age of patients significantly influenced their prioritization. Only the youngest group, the respondents below 15 years, had somewhat different priorities. This group prioritized research on ‘reduction of fear for hypersensitivity and/or symptoms during activities outside’ as highest. Other high priorities of this group concerned topics that aim to improve the overall functioning of general practitioners.
Differences between the priorities of asthma patients, COPD patients and relatives were limited as well. All types of patients and their relatives prioritized research on the causes of the diseases and on new medication as most important. Besides these top priorities, many asthma patients also prioritized issues related to their social environment, while seriously ill COPD patients and patients with both asthma and COPD focused on the reduction of costs.
The level of education hardly influenced the outcomes of the questionnaire, although people with only primary education deviated somewhat in their prioritization. This group prioritized research on causes and on co‐morbidity somewhat lower and asked for more attention on ‘improvement of understanding by the social environment’, ‘the adaptation of governmental rules concerning public places and workplaces’, and ‘the effects and efficacies of alternative medication’.
As became apparent from the results of the additional questionnaire among non‐NAF members, the priorities of NAF members did not deviate from the priorities of non‐members. Apparently, the membership of the NAF does not provide a bias in patients’ priorities on health research.
There was some overlap between priorities identified in the focus groups and the questionnaire. In both exercises, the side‐effects of medication, the obscurity of causes of diseases and symptoms, and complaints related to hypersensitivity were prioritized highly. As a difference, in the focus groups problems concerning the quality of health‐care, including issues of coaching, information and co‐ordination, received much attention, while in the questionnaire patients gave knowledge on co‐morbidity and reduction of costs a higher priority.
Concerning patient participation in research policy in general, the majority of respondents considered patients’ contributions relevant to research agenda setting and were prepared to be involved in future consultations. Most of them preferred questionnaires, but about one‐fourth of the respondents was willing to be interviewed or to participate in workshops or committees as well. Because of the relatively low response, the overall percentage of NAF members that are prepared to be involved in future agenda‐setting processes is likely to be lower.
Discussion
In this study we aimed to sample the entire range of patients’ problems concerning living with asthma/COPD. We, thus, had to be concerned whether all types of patients were represented during the focus groups – after all, different types of patients might experience different problems. Because younger patients and seriously ill patients were underrepresented in our focus groups, we held additional interviews. This, however, did not reveal new problems, but proved to indicate only slight differences in urgency and prioritization, as discussed above. We therefore think our focus group results adequately cover the entire range of patients’ problems.
Although the response rate to our questionnaire was low, the respondents covered a representative variation in sex, disease, age and educational level. We therefore consider our results as an adequate representation of research priorities of NAF members. In addition, as a smaller supplementary survey among non‐NAF members resulted in the same research priorities, our questionnaire results can be considered to reflect research priorities of asthma/COPD patients in general.
Differences between priorities identified in the questionnaire and the preliminary priorities that were expressed during the focus groups are probably related to differences in objectives and ways of asking between the two methods used. Whereas, for example, lack of knowledge on aetiology may not be the most obvious answer when asking for experienced problems, the acquirement of this knowledge can be considered highly relevant when presented in a list of potential research targets. This argument is substantiated by the fact that patients’ research questions, as formulated during the last part of the focus groups, correspond very well with priorities resulting from the questionnaire. In addition, group dynamics within focus groups can hamper fair prioritization exercises. When discussing problems, patients will influence each other, easily resulting in potential (unintentional) over‐emphasizing of a particular kind of problem and the underexposing of other problems. When patients are confronted with a questionnaire, they can prioritize a complete series of potential research targets individually.
The patient consultation resulted in a list of priorities that reflects solutions to problems identified during the focus groups. At first sight, some of these research targets, such as those focussing on the reduction of costs or the improvement of understanding of the social environment, may seem to have little relevance for scientific research. However, we argue that all these targets could be addressed directly or indirectly by different disciplines within the broad field of health research. For example, economic research could focus on the financial aspects of diseases, while social scientific research could elaborate societal patterns of interaction between patients and their social environment.
Our results indicate that asthma and COPD patients (NAF members) prioritized biomedical research – research on the aetiology of the diseases and on new and better medication – above research on health‐care, social or political issues. After comparison of the patients’ priorities identified with the research priorities as formulated in the current asthma/COPD research programmes of the NAF 13 , 14 and ZonMw (http://www.zonmw.nl/index.asp?s=7637), we found that patients’ highest two priorities, concerning more knowledge about the causes of the diseases and more effective medication, correspond with priorities of the current NAF programme on EBO. Priorities of the current Z&P programme and of the Health Promotion and Disease Prevention programme of ZonMw were addressed (and partly prioritized) by patients when discussing problems during the focus groups, but were not prioritized as important research targets in the questionnaire.
Topics that were prioritized by the patient community as third, fourth and fifth (co‐morbidity, side‐effects of medication and interaction between medications respectively) are not covered by the current research programmes. Possibly, research concerning the side‐effects of, and interaction between, medications is considered the territory of the pharmaceutical industry, and thus is not included in the NAF and ZonMw programmes. The fact that co‐morbidity is not included in current research programmes could be explained by the strong differentiation of current medical practice and (bio)medical research; both the Dutch health‐care system and the biomedical research field are highly structured around individual diseases and professional disciplines. These three priorities can be considered significant ‘alternative’ research priorities that originate from the experiential knowledge and interests of patients.
The priorities of patients also deviate from the priorities within the current research programmes with respect to psycho‐social aspects of asthma/COPD, such as fear of hypersensitivity and the (non)‐understanding by the social environment. These topics were considered main problems by patients but are not explicitly addressed in any of the current research programmes.
A third difference is that patients did not focus on targets addressing smoking addiction – a priority in both NAF programmes. A possible explanation for this absence among patients’ problems and priorities is that for some patients smoking addiction is a highly sensitive subject, while for others it might be irrelevant because they no longer, or never did, smoke.
Conclusion
The combination of focus groups and a questionnaire can be considered an appropriate methodology for investigating patients’ priorities on research. The questionnaire appeared a suitable tool for explicitly consulting a representative group of patients on their research priorities, without becoming obscured by group effects. The input from focus groups was indispensable for getting a proper design of the questionnaire as well as for gaining insight into underlying arguments and perspectives.
Our final results contradict the assumption of many people that patients are not capable of participating in broad health research agenda setting in a well‐argued way. Firstly, NAF members in general seem to have sufficient knowledge to formulate and prioritize health research topics covering the entire health research field. The focus group discussions have indicated that participants were able to substantiate their perspectives on priorities. Secondly, NAF members appeared to be able to think in biomedical, long‐term targets and in favour of future generations, and did not only focus on individual health‐care and social problems. Thirdly, they were capable of introducing some new research topics that were not covered by current research agendas, such as co‐morbidity, side‐effects of medication and mutual effects of medication. One could reasonably assume that other patients will be able to do the same.
Based on this study, we thus conclude that patients are capable of participating in research agenda setting in a well‐argued way. Indeed, although, just as medical professionals, patients have their own biases, they have something new to contribute to research agendas, which pleads for their participation in research agenda setting.
Acknowledgements
Authors are grateful to the Netherlands Asthma Foundation and ZonMw for funding this research project and for assisting in the recruitment of focus group participants and in the distribution of the questionnaire among NAF members. Further, authors would like to thank Gert‐Jan van der Wilt and some of our colleagues at the Institute, as well as the anonymous reviewer for their helpful comments on earlier drafts of this article. In addition, they thank all participants and respondents for their valuable contributions.
Footnotes
We define biomedical research as the scientific research field that brings together fundamental and applied aspects of biology and medicine with the ultimate aim to contribute to the understanding and improvement of human health, for example, by searching for causes and working mechanisms of, or therapies for, pathological disorders.
Because we only occasionally distinguish different kind of Netherlands Asthma Foundation (NAF) members, in this article the term ‘patients’ can refer to both actual patients and relatives or carers of patients.
The discussion commenced with the problems patients experience in relation to their diseases; only towards the end we explicitly discussed research. The main reasons for this is that talking about problems better fits in with daily experiences of patients than talking about research.
In the remaining part of this article, we will use term ‘priorities’ when referring to the wishes or potential research targets as prioritized by patients during the questionnaire.
References
- 1. Ong BN, Hooper H. Involving users in low back pain research. Health Expectations, 2003; 6: 332–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hanley B, Truesdale A, King A, Elbourne D, Chalmers I. Involving consumers in designing, conducting, and interpreting randomised controlled trials: questionnaire survey. British Medical Journal, 2001; 322: 519–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Telford R, Beverley CA, Cooper CL, Boote JD. Consumer involvement in health research: fact or fiction? British Journal of Clinical Governance, 2002; 7: 92–103. [Google Scholar]
- 4. Oliver S, Clarke‐Jones L, Rees R et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence‐based approach. Health Technology Assessment, 2004, 8: 1–148. [DOI] [PubMed] [Google Scholar]
- 5. Stevens T, Wilde D, Hunt J, Ahmedzai SH. Overcoming the challenges to consumer involvement in cancer research. Health Expectations, 2003; 6: 81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. De Cooker D, Koningstein M. De patiënt in biomedisch onderzoek: Patiëntenparticipatie in biomedisch astma‐ en COPDonderzoek. Amsterdam, the Netherlands: Vrije Universiteit, Department of Biology and Society, 2003. [Google Scholar]
- 7. Caron‐Flinterman JF, Broerse JEW, Bunders JFG. Patient Participation in Decision Making on Biomedical Research: Changing the Network. Amsterdam, the Netherlands: Vrije Universiteit, Department of Biology and Society, 2004. [Google Scholar]
- 8. Entwistle VA, Renfrew MJ, Yearley S, Forrester J, Lamont T. Lay perspectives: advantages for health research. British Medical Journal, 1998; 316: 463–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goodare H, Lockwood S. Involving patients in clinical research improves the quality of research. British Medical Journal, 1999; 319: 724–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Popay J, Williams G. Public health research and lay knowledge. Social Science and Medicine, 1996; 42: 759–768. [DOI] [PubMed] [Google Scholar]
- 11. Broerse JEW, Bunders JFG. Pitfalls in implementation of integral design approaches to innovation: the case of the Dutch Special Programme on Biotechnology In: Leeuwis C. (ed.) Integral Design: Innovation in Agriculture and Resource Management. Wageningen, the Netherlands: Mansholt Institute/Backhuys, 1999: 245–265. [Google Scholar]
- 12. Zweekhorst MBM, Broerse JEW, Bunders JFG. Institutionalising a transdisciplinary approach to technology development in a Bangladeshi NGO. Interdisciplinary Environmental Review, 2002; 4: 43–65. [Google Scholar]
- 13. Astma Fonds . Programma Experimenteel en Beschrijvend Onderzoek. Leusden, the Netherlands: Nederlands Astma Fonds, 2000. [Google Scholar]
- 14. Astma Fonds . Programma Zorg en Preventie. Leusden, the Netherlands: Nederlands Astma Fonds, 2000. [Google Scholar]
- 15. Berry S, Mangione CM, Lindblad AS, McDonnell PJ. Development of the National Eye Institute refractive error correction quality of life questionnaire: focus groups. Ophthalmology, 2003; 110: 2285–2291. [DOI] [PubMed] [Google Scholar]
- 16. Chen AY, Frankowski R, Bishop‐Leone J et al. The development and validation of a dysphagia‐specific quality‐of‐life questionnaire for patients with head and neck cancer. Archives of Otolaryngology – Head and Neck Surgery 2001; 127: 870–876. [PubMed] [Google Scholar]
- 17. Steine S, Finset A, Laerum E. A new, brief questionnaire (PEQ) developed in primary health care for measuring patients’ experience of interaction, emotion and consultation outcome. Family Practice, 2001; 18: 410–418. [DOI] [PubMed] [Google Scholar]
- 18. Morgan DL. Focus groups. Annual Review of Sociology, 1996; 22: 129–152. [Google Scholar]
- 19. Klinkers L. Beleid begint bij de samenleving; Een zoektocht naar de menselijke maat; Over de essentie van interactief beleid maken. Utrecht, the Netherlands: Lemma. [Google Scholar]
- 20. Mullen PM. Public involvement in health care priority setting: an overview of methods for eliciting values. Health Expectations, 1999; 2: 222–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nederland T, Tabibian N, Kromontono E. Ledenmonitor Astma Fonds; het oordeel en de wensen van de leden over de individuele en collectieve belangenbehartiging. Utrecht, the Netherlands: Verwey‐Jonker Instituut, 2004. [Google Scholar]
- 22. Kerklaan M, Vermelis W. Imago en Bekendheidsonderzoek leden t.b.v. het Astma Fonds. Breda: Bureau Heliview Marketing Services, 2002. [Google Scholar]
- 23. Heijmans MJWM, Rijken PM. Monitor zorg‐ en leefsituatie van mensen met astma en mensen met COPD. Kerngegevens 2001/2002. Utrecht, the Netherlands: NIVEL, 2003. [Google Scholar]


