There is a critical need for an updated, more comprehensive, and integrated conceptual model to help health care providers, patients, and consumers, as well as researchers using this theoretical model, to better understand health information, communication, and information seeking of patients and consumers. My colleagues and I have developed such a model, based on an ongoing research agenda and empirical data provided by pilot studies in the area of breast cancer. However, this expanded model is now developed in such a manner that based on deliberations with experts in other clinical disciplines such as arthritis and diabetes, it is likely it can at least be tested with patients diagnosed and consumers at risk for these diseases.
A situation recently unfolded in my neighbourhood which vividly illustrates the need for this conceptual model. It also illustrates how the model is useful beyond the area of breast cancer information.
A 51‐year‐old, college‐educated, married, mother of seven children sat down to read a popular women's magazine for a few minutes while she waited for her physician husband to come home from work. As she scanned the magazine she came across an article about the warning signs of ovarian cancer. As she read the article, she became engrossed in its details because she recognized the signs and symptoms discussed and realized she had experienced each of them. Her pulse raced as she began to realize that what she had attributed to perhaps the aging process and a hectic lifestyle could in reality be ovarian cancer. When her husband came home they discussed the issue, and the next day she made an appointment with her personal physician. A number of tests were ordered, a large abdominal mass was found, and surgery was ordered. This woman has terminal ovarian cancer. In a span of 10 days, her life and that of her family has changed dramatically based on her reading of a journal that prompted her to seek medical care.
This is not a unique experience; such scenarios likely occur with hundreds, if not thousands, of individuals around the globe. However, as a researcher who examines health information use, especially as it relates to health care decision‐making, I noted many implications from this experience that can inform health communication research. First, health information is not always intentionally sought, yet it may be used and have profound consequences. This requires consideration of the existence, role, and importance of ‘passive’ receipt of information vs. ‘active’ information seeking. My neighbour casually came across important information in a magazine written for the general public. The recent professional emphasis on ‘Health Information Seeking Behaviour’ must take into account that some individuals, who have no intent of seeking health information, come across such information as they go about their activities of daily living.
Second, the information received came from traditional print media, not the ‘new media,’ such as the world wide web, that are so frequently cited as playing a major role in health information. This underscores the need for a comprehensive view of health information sources that recognizes not only ‘high tech’ or ‘new media’ sources, but also those that are traditional and easily accessible.
Third, in this case an educated, economically upper class woman received her health information through a medium aimed at women of all educational and socio‐economic classes. Given the current emphasis in the health care professions on targeting ‘at risk’ populations, it is important to recognize that while personal variables such as socio‐economic status play a role in information use, contextual issues, such as relaxing with a popular magazine vs. accessing a medical journal or website, are also important influences.
In 2001, together with colleagues Patrick and Kruse, I published an article titled ‘The natural history of the use of healthcare information by women with breast cancer: a conceptual model.’ 1 The objective of the paper was to fill a significant knowledge gap, as a review of the literature at that time revealed a paucity of empirical studies using a strong conceptual framework or model that could provide the vital theoretical underpinnings for studies of health information use and communication, especially in understanding patient decision‐making, and provide a context in which to analyse and interpret empirical data. More is known today, because of the efforts of many groups including the journal Health Expectations 2 , 3 and in the United States, the National Cancer Institute's ‘Health Information Service,’ 4 , 5 , 6 but far more work is needed. Noting the lack of a strong conceptual model using a broad spectrum of health, we developed the model first described in that 2001 paper.
The first conceptual model 1 illustrated the theoretical underpinnings of our approach and provides a context in which to analyse and interpret the results. In fact the National Cancer Institute's ‘Health Information Service’ 5 cites this model as one of three viable models of health information seeking behaviour together with those of Johnson. 17 Our model depicted the interrelationships among the various personal and situational factors that comprise the patient's information environment and different phases of her use of various types of information to make decisions about her own health care. We were heavily influenced by components of the Health Belief Model (HBM), 7 , 8 the awareness‐to‐adherence model of physician adoption of clinical guideline information, 9 and the patient practice variation theory I published in 1993. 10
Pilot data and the validation study
In an effort to test our model first published in 1991, we collected data from a total of 121 women who had previously been diagnosed with breast cancer and consented to participate in our survey. The pilot study was approved by the University of Missouri Health Sciences Institutional Review Board. The survey was conducted with patients in the Kansas City area, Columbia and mid‐Missouri, and the Newark, New Jersey, area. Following the conceptual model initially developed, there was a logical progression of answers one would expect. For example, if a woman said she was not aware of health information related to breast cancer, one would not expect her to later say that health information influenced her decisions about her personal health care. An initial data analysis indicated that the expected logical pattern was not always followed. In fact only 73 of the women surveyed followed the expected pattern, with 48 not following the pattern.
In an effort to better understand this potential validity problem, we took a two‐step approach. First, we conducted a focus group meeting with the staff involved in patient interviews and those who worked on model development to review and discuss the detailed notes taken during the time of the interviews. We then re‐contacted a sample of these women for whom our nurse interviewer had sufficiently detailed notes regarding the women's medical situation and use of health information. What we found was that the initial model had a number of flaws. Perhaps the most notable was the explicit lack of recognition of the role that the ‘passive receipt’ of information played in the process. For example, like the woman in the vignette above, a number of women did not intentionally seek health information. This finding is consistent with the work of Carlsson 11 , who reports that ‘patients actively sought information to a limited degree, but the majority of patients take an interest when cancer issues are presented in newspapers and magazines, or on radio and television. A more passive information seeking strategy was common in her study of Swedish cancer patients, especially among those with lower educational levels. 11 Many women in our study also came across information while they read the newspaper, read magazines, listened to radio shows, watched television, or simply spoke with others about their cancer diagnosis and treatment. So these women initially answered that they were not aware of such information, but ultimately health information became available and was in many cases very useful. In other cases, subjects may have thought only about media as sources as health information, but did not view direct communication with their physician or nurse as a source of information. Finally, there were inconsistencies introduced by the lack of a specific time frame to recall the cancer experience; this was especially true for long‐term survivors. These further investigations clarified the need for more explicit wording in the survey instrument and the related conceptual model, as well as further development of the model to take into account both active and passive receipt of health information. This is now detailed in the expanded conceptual model depicted on page 4. As a further test, we conducted yet another survey using the model's revised instrument with 14 patients; consistently the logical patterns one would expect were found in all cases. Finally, consistent with the approaches taken by Cowin 12 and Ouitmet et al., 13 we convened a focus group of experts in health communications, health services research, biostatistics, and nursing who in reviewing the data along with the supporting documentation determined that the revised model has both face and internal validity.
The expanded model
Our experience shows the necessity of further work in the development, dissemination, and testing of conceptual models that assist in the understanding of this important development in the history and evolution of the role of patients in their own care. Additionally, we also need to better understand the nature, type, source, and use of health information by healthy consumers, including those with a known risk for various diseases, given our advances in knowledge of genetics and the role of family history in disease. Thus, I propose that we include but differentiate ‘patients’ and ‘consumers’ in any such models (Fig. 1).
Figure 1.
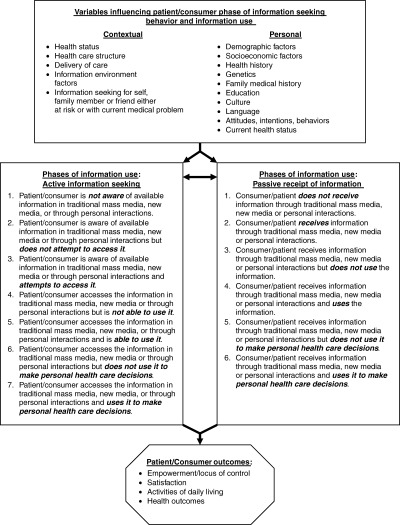
Expanded conceptual model of health information seeking behaviors and the use of information for health care decisions.
Johnson 14 cites Summers et al., 15 who in reporting about the critical nature of cancer‐related information seeking, describe information seeking as ‘the result of a complex set of interactions among multiple variables each with different capabilities to predict information use’ 15 and propose the need for good theory that promotes deeper understanding of the issues involved. 14 Bower and Bilbody 16 write that ‘models are abstract representations of complex areas’ and cite the original work of Siegler and Osmond, 17 who describe models as ‘inventions of the human mind to place facts, events and theories in an orderly manner. As such, they help place empirical data, research evidence, and systematic reviews in a broad perspective and ‘can assist in the interpretation of evidence in a policy context … which may provide a more solid bridge between evidence and the policy context.’ 16 However, they also add that conceptual models must be continually evaluated; consequently, the proposed revised model is presented in this paper.
A number of cautions are in order to fully understand this model. The model is indeed derived from the experience and reports of patients themselves. As such, it is consistent with a ‘patient‐centred’ view of care, and may be useful in placing research findings in a broad patient perspective. However, when applied in an individual patient clinical setting, caution must be taken consistent with Barnett et al., 18 who write that a ‘patient‐centred approach must involve tailoring information to individual patient requirement’ as ‘it is difficult to predict how much information patients feel they need.’ While it is widely recognized that appropriate information can increase knowledge, reduce anxiety and distress, reduce decisional conflict, and increase adherence to various regimens, 15 , 16 , 19 , 20 many patients do not want any health information other than that provided by their personal physician. Friis et al. 21 report this is more likely in the elderly, but it may also occur with other types of patients. For example, most studies focus on outpatients and little is known about the information needs of severely ill cancer patients treated in hospital. 21 Therefore, the revised model takes these situations into account as some patients/consumers may decide not to access information. While the traditional medical perspective may not recognize such a view, a ‘patient‐centred’ model must recognize patient needs and wants even when they are contrary to what the professional may view as necessary or helpful. Despite that fact that ‘being informed and seeking information are discussed as society's expectations of today's cancer patient,’ 21 it may be in the best interests of a given patient to not seek information, ‘as a strategy to maintain hope.’ This also was identified in our study by at least one participant.
The next step is more vigorous testing of the proposed model in various populations and cultures. This will provide not only important data for the model's enhancement, but also help us to better understand the current status of the use of health information by both patients and consumers, and clarify some of the confusion found in the current literature. For example, some articles point to the tremendous growth in health information and especially internet‐based information, 22 while others report that at least in the United States, as of 2001, only one‐half of adults ‘place a high priority on seeking health information.’ 23 Finally, Tu and Hargraves 24 report that ‘contrary to [the] popular belief that Americans avidly seek health information – especially on the internet – a majority of Americans in 2001 sought no information about health concerns, according to a Center for Health System Change study.’ Interestingly, this study found that, like the woman in the above vignette, ‘instead of surfing the internet, the 38% of Americans who did obtain health information relied more often on traditional sources such as books or magazines.’ However, they report that level of education was shown to explain a large difference in health seeking information.
While popular opinion and the reality of health information use are not yet consistent, it is anticipated that over time this situation will change as information increases, health awareness is heightened, literacy improves, education levels rise, and the consumer movement continues to evolve and mature. More rigorous studies using a model such as the one proposed here are needed as we attempt, as health professionals, to better understand patient and consumer desires for health information, how they will change over time, and how we must modify and develop new and more appropriate types of information that patients will use and find helpful as they face an illness, or simply wish to remain proactive in maintaining health.
References
- 1. Longo DR , Patrick TB , Kruse RL . The natural history of the use of healthcare information by women with breast cancer: a conceptual model. Proceedings of AMIA Symposium 2001; 413–417. [PMC free article] [PubMed] [Google Scholar]
- 2. Moumjid N , Bremond A , Carrere MO . From information to shared decision‐making in medicine. Health Expectations 2003; 6: 187–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Coulter A . Whatever happened to shared decision‐making? Health Expectations 2002; 5: 185–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Freimuth VS , Stein JA , Kean TJ . Searching for Health Information: the Cancer Information Service Model. Philadelphia, PA: University of Pennsylvania Press, 1989. [Google Scholar]
- 5. Squiers L , Treiman K . Cancer Information Service Research Agenda (Draft). Bethesda, MD: National Cancer Institute, Cancer Information Service, NCI Office of Communications, CIS Program Office, 2005. [Google Scholar]
- 6. Squiers L . The CIS Research Program 2005. Bethesda, MD : National Cancer Institute, Cancer Information Service, NCI Office of Communications, CIS Program Office, 2005. [Google Scholar]
- 7. Degner LF , Kristjanson LJ , Bowman D et al. Information needs and decisional preferences in women with breast cancer. JAMA 1997; 277: 1485–1492. [PubMed] [Google Scholar]
- 8. Engel GL . The clinical application of the biopsychosocial model. American Journal of Psychiatry 1980; 137: 535–544. [DOI] [PubMed] [Google Scholar]
- 9. Pathman DE , Konrad TR , Freed GL , Freeman VA , Koch GG . The awareness‐to‐adherence model of the steps to clinical guideline compliance – the case of pediatric vaccine recommendations. Medical Care 1996; 34: 873–889. [DOI] [PubMed] [Google Scholar]
- 10. Longo DR . Patient practice variation: a call for research. Medical Care 1993. (5 Suppl.); 31: YS81–YS85. [DOI] [PubMed] [Google Scholar]
- 11. Carlsson M . Cancer patients seeking information from sources outside the health care system. Supportive Care in Cancer 2000; 8: 453–457. [DOI] [PubMed] [Google Scholar]
- 12. Cowin LS . Study 1 results: the development, reliability and validity of the NSCQ and nature of nurses’ self‐concept. The Self‐Concept of Nurses and Its Relationship to Job Satisfaction and Retention. Thesis. University of Western Sydney, Sydney. [Google Scholar]
- 13. Ouimet JA , Bunnage JB , Carini RM , Kuh GD , Kennedy J . Using focus groups to establish the validity and reliability of a college student survey Research in Higher Education 2004; 45: 233–250. [Google Scholar]
- 14. Johnson JD . Cancer‐Related Information Seeking. Cresskill, NJ: Hampton Press, Inc., 1997. [Google Scholar]
- 15. Summers EG , Matheson J , Conry R . The effect of personal, professional, and psychological attributes, and information seeking behavior on the use of information by educators. Journal of the American Society for Information Science 1983; 34: 75–85. [Google Scholar]
- 16. Bower P , Gilbody S . Managing common mental health disorders in primary care: conceptual models and evidence base. British Medical Journal (Clinical Research Ed) 2005; 330: 839–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Siegler M , Osmond H . Models of Madness, Models of Medicine. New York: Macmillan, 1974. [Google Scholar]
- 18. Barnett GC , Charman SC , Sizer B , Murray PA . Information given to patients about adverse effects of radiotherapy: a survey of patients’ views. Clinical Oncology (Royal College of Radiologists) 2004; 16: 479–484. [DOI] [PubMed] [Google Scholar]
- 19. Michie S , Rosebert C , Heaversedge J , Madden S , Parbhoo S . The effects of different kinds of information on women attending an out‐patient breast clinic. Psychology, Health & Medicine 1996; 1: 285–296. [Google Scholar]
- 20. Cancer Information Strategy Team . Towards a Cancer Information Strategy. Highcroft, Winchester, UK: NHS Information Authority, 2005. http://www.nhsia.nhs.uk/pdf/cis.pdf (last accessed 2/6/05). [Google Scholar]
- 21. Friis LS , Elverdam B , Schmidt KG . The patient's perspective: a qualitative study of acute myeloid leukaemia patients’ need for information and their information‐seeking behaviour. Supportive Care in Cancer 2003; 11: 162–170. [DOI] [PubMed] [Google Scholar]
- 22. Cline RJ , Haynes KM . Consumer health information seeking on the Internet: the state of the art. Health Education Research 2001; 16: 671–692. [DOI] [PubMed] [Google Scholar]
- 23. Navarro FH , Wilkins ST . A new perspective on consumer health Web use: ‘valuegraphic’ profiles of health information seekers. Managed Care Quarterly 2001; 9: 35–43. [PubMed] [Google Scholar]
- 24. Tu HT , Hargraves JL . Seeking health care information: most consumers still on the sidelines. Issue Brief/Center for Studying Health System Change 2003; 1–4. [PubMed] [Google Scholar]


