Abstract
Objective This study investigates general practitioners’ (GPs) and patients’ attitudes to shared decision making, and how these attitudes affect patient satisfaction.
Background Sharing of information and decisions in the consultation is largely accepted as the ideal in general practice. Studies show that most patients prefer to be involved in decision making and shared decision making is associated with patient satisfaction, although preferences vary. Still we know little about how the interaction of GP and patients’ attitudes affects patient satisfaction. One such study was conducted in the USA, but comparative studies are lacking.
Design Questionnaire survey distributed through GPs.
Setting and participants The results are based on the combined questionnaires of 41 GPs and 829 of their patients in the urban municipality of Bergen in the western part of Norway.
Main variables studied The data were collected using a nine‐item survey instrument constructed to measure attitudes towards patient involvement in medical consultations. The patients were also asked to rate their satisfaction with their GP.
Results and conclusions The patients had a strong preference for shared decision making. The GPs also generally preferred shared decision making, but to a lesser degree than the patients, which is the opposite of the findings of the US study. There was a positive effect of the GP's attitude towards shared decision making on patient satisfaction, but no significant effect of congruence of attitudes between patient and GP on patient satisfaction. The suggested explanation is that GPs that are positive to sharing decisions are more responsive to patients’ needs and therefore satisfy patients even when the patient's attitude differs from the GPs’ attitude. Hence, although some patients do prefer a passive role, it is important to promote positive attitudes towards patient involvement in medical consultations.
Keywords: doctor–patient congruence, general practice, patient involvement, patient satisfaction, shared decision making
Introduction
The relationship between doctor and patient is in many ways the very core of the health‐care system, and doctor–patient interaction remains a central focus of the study of health systems in a range of disciplines–health economics, medical anthropology, sociology and medical science. 1 , 2 Over recent decades there has been a steady development towards greater patient involvement in medical decision making, and the sharing of decisions between doctor and patient is perhaps the subject that has received most attention in the literature on the doctor–patient relationship. 3 The belief that patients are entitled to be informed and have a say in decisions concerning their own medical care is now the prevailing view among patients’ organizations and the medical profession. 4 , 5 , 6 , 7 Many countries (among them the USA, UK and Norway) have passed legislation to ensure the patient's right to be involved in decisions regarding their own health.
Several studies of patients’ stated preferences report that patients in general would like to be informed and involved in the decision‐making process. 8 , 9 Although most patients prefer a participatory role in clinical decision making, patients’ preferences vary according to age, gender, educational level and severity of the disease. It is worth noting that a minority seems to prefer a passive role in the consultation. 4 , 10 A variation in attitudes has also been reported for GPs. 11 , 12 , 13 However comparative studies in this field are scarce, and there is little knowledge about how preferences vary across regions and different health care systems.
Various studies conclude that a consultation style involving patients in the decision‐making process enhances patient satisfaction. 4 , 12 , 14 , 15 , 16 , 17 , 18 and there are also some indications that patients who play an active part in consultations have better health outcomes. 19 , 20 , 21 , 22 , 23 Also a few studies have investigated how patient preferences for consultation style affect patient satisfaction, and their conclusions differ. 4 This might be due to ambiguities relating to the meaning of the concepts and difficulties in finding valid measures of attitudes. 24
There is a lack of studies simultaneously exploring patients’ and doctors’ preferences for patient involvement in medical decision making, and we have only been able to locate a few such studies conducted by Krupat et al. in the USA. 10 , 12 , 25 , 26 The authors developed a questionnaire for assessing and comparing doctors’ and patients’ preferences for sharing decisions and used it to investigate patients’ and doctors’ orientations and how congruence in orientations related to patient satisfaction. The results confirmed that the majority of both GPs and patients prefer shared decision making, GPs even more than patients. The study concluded that both GP attitudes in favour of patient involvement and congruence in attitudes between GP and patients promote patient satisfaction, but GP attitudes seemed to be most decisive.
The overall aim of this paper is to investigate how fit in attitudes between GP and patient affects patient satisfaction. Comparative to the US study, we measure preferences of doctors and patients for patient involvement in a Scandinavian setting, study predictors of patients’ attitudes and investigate the relation between attitudes and patient satisfaction. In particular, we aimed to find out whether doctors that favour patient involvement generate satisfied patients and whether a doctor–patient fit in attitudes is associated with satisfied patients.
Data and methods
Respondents and sample
The study draws on survey data from two sources: one questionnaire completed by GPs and a second by their patients. In June 2004 a letter of invitation was sent to all GPs in Bergen (n = 181), a statistically average urban municipality in western Norway. They were asked to distribute the patient questionnaire consecutively to 50 consulting patients excluding children, as well as to complete a questionnaire of their own. The decision to recruit patients through their GPs instead of using direct mail was based on ethical considerations and on the expectation that this would increase the chances of an adequate response rate. A reminder was sent to the GPs after 3 weeks. The GPs distributed the questionnaire during summer/autumn 2004. To ensure complete anonymity, doctors and patients were linked by corresponding numbers, but no record was kept linking doctors’ names with their numbers. A total of 181 GPs were contacted and 56 (31%) volunteered to contribute by asking their patients to participate. Of these, 15 did not return their own questionnaire, which means that for the purpose of combining GPs’ answers with patients’ answers we have 41 GPs. Because of the considerations of anonymity, we were not able to track which GPs didn't return their own questionnaire (Fig. 1).
Figure 1.
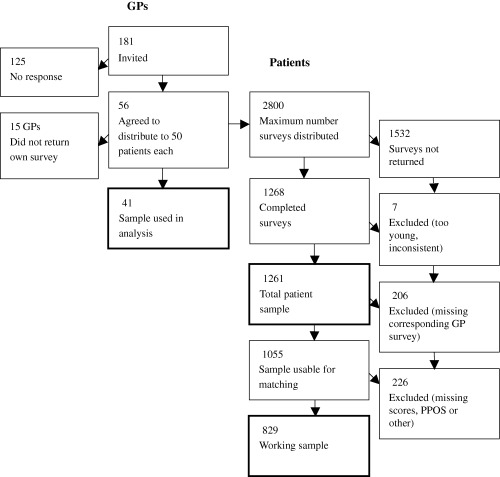
Flow diagram of general practitioners and patient participants.
Operationalizing attitudes to shared decision making
We used the Patient–Practitioner Orientation Scale (PPOS) for measuring preferences for shared decision making. The PPOS is a six‐point Likert‐scale questionnaire developed by Krupat et al., 12 , 26 where patients and doctors assess identical statements on the roles of the doctor and patient in the consultation, where the highest score (=6) reflects preference for sharing influence. The statements express different aspects of influence on the decision‐making process, such as the degree of patient participation in acquiring information (Appendix 1).
Both the doctors’ and patients’ questionnaires included background questions on demographic characteristics such as age, gender, educational level (patients) and years of professional experience (GPs). Additionally, GPs were asked to give some basic information on the practice such as number of patients on the list and satisfaction with list length. Patients were asked about the relationship with the doctor they had consulted (for example whether they had chosen this doctor as their regular GP). The patients were also asked to rate their overall satisfaction with the doctor by indicating a number to answer the following question: ‘On a scale from one to six, where one means not satisfied and six means very satisfied; how satisfied are your with the doctor you visited today'?
Data analysis
We used the software Stata 8.0 (STATA Corporation, College Station, Texas, USA) to analyse the data. In addition to presenting descriptive statistics, we used logistic regression analysis to test our patient satisfaction hypothesis A dichotomous variable distinguished those who were very satisfied (giving the top score on this item in the survey) from those who gave any other response. As educational level has three values, we included dummy variables for two educational levels (upper secondary and college). We adjusted for potential clustering effects as many patients share the same GP.
In addition we estimated a linear regression to investigate predictors of patient ‘sharing score’. The ‘sharing score’ was generated as a mean of the scores of all the PPOS items except item 6. We excluded this item from the analysis because of the extent of missing data (181 = 14%).
As the PPOS instrument is identical for doctors and patients, it is possible to construct a difference score as a measure of the fit between doctor and patients. The score was constructed as the absolute value of the difference of the GP sharing score and the patient sharing score. The difference score was tested as predictor of patient satisfaction in the logistic regression model.
Results
A total of 1268 patients responded (45%) The patient response rate varied by doctor from 2% to 76%*. From this sample we eliminated respondents that were younger than 16 years and those who seemed inconsistent or unreasonable (e.g. choosing the first alternative on all the questions). This resulted in a total sample of 1261 patients. In addition, we chose to exclude respondents who had a missing value for one of the items used in the empirical analysis. We thus had a working sample of 829 patients (Fig. 1).
Sample profiles
The GP sample is presented in Table 1. As this is a small and not necessarily representative sample, we have included national statistics for the population of GPs in Bergen and for all Norwegian GPs to illustrate the representativeness of the sample. As can be seen from Table 1, the sample hardly differs from the general population of Norwegian GPs in mean age (47.2 and 46.3 respectively), proportion of male GPs (66% vs. 70%) or number of list patients (1161 vs. 1199). Compared with the population of Bergen GPs, our sample is similar in respect to gender (66% vs. 68% males) but has somewhat shorter lists (1161 vs. 1329). Twenty per cent of the GPs in our sample would prefer more patients on their lists (longer patient list), while another recent Bergen study finds that 21% of Bergen GPs prefer longer lists. 27 The mean GP sharing score is 4.31 (min. value = 3.25; max. value = 5.25; SD = 0.46), and the mean values for female and male GPs are 4.41 (min. value = 3.5; max. value = 5.25; SD = 0.47), and 4.26 (min. value = 3.25; max. value = 5; SD = 0.45) respectively.
Table 1.
Characteristics of the general practitioner (GP)‐sample, mean values of all Norwegian GPs and of GPs in the municipality of Bergen
| Variable | Sample (n = 41) | GP population in Norway1 (n = 3767) | GP population in Bergen (n = 181) |
|---|---|---|---|
| GP age (mean ± SD) | 47.2 ± 7.8 | 46.3 | 45.6 |
| Gender (% male GPs) | 66 | 70 | 68 |
| Listlength (mean ± SD) | 1161 ± 411 | 1199 | 1329 |
| GPs in the practice (mean ± SD) | 3.6 ± 1.6 | ||
| Prefer longer list (%) | 20 | 212 |
In Table 2 the profile of the total patient sample of 1261 patients as well as the smaller working sample used in the regressions are displayed. The mean age of the total sample is 50.2 years and the proportion of female respondents is 70%. In the total sample, 22% has only compulsory education, 43% has upper secondary education and 35% has college or more. The mean of the patient satisfaction score is 5.3 on the six‐point Likert scale. The satisfaction score is skewed, i.e. most patients give their GP the top score on satisfaction. Because of the skewedness we have introduced a dummy variable, ‘satisfied’, which separates the perfectly satisfied from the less than perfectly satisfied in the regression analysis below. The result is that 53% of the sample is perfectly satisfied with their GP while 47% are less than perfectly satisfied. The mean value of the sharing scores of the total patient sample is 4.48 (min. value = 2; max. value = 6; SD = 0.58), and the mean values for women and men are 4.52 and 4.38 respectively (Table 2). This shows that most patients prefer shared decision making. The mean patient sharing score is significantly higher than the mean GP sharing score.
Table 2.
Characteristics of the total patient sample and working sample
| Total patient sample (n = 1261) | Working sample (n = 829) | |
|---|---|---|
| Age (mean ± SD) | 50.2 ± 18.6 | 49.3 ± 17.9 |
| Gender (% females) | 70 | 71 |
| Education (% compulsory) | 22 | 17 |
| Education (% upper second) | 43 | 45 |
| Education (% college) | 35 | 38 |
| Switched GP (%) | 24 | 23 |
| Satisfaction (mean ± SD) | 5.3 ± 1.0 | 5.3 ± 0.9 |
| Satisfied (%) | 53 | 55 |
| Patient PPOS score (mean ± SD) | 4.48 ± 0.58 | 4.47 ± 0.59 |
| Male patient sharing score (mean ± SD) | 4.38 ± 0.60 | 4.38 ± 0.59 |
| Female patient sharing score (mean ± SD) | 4.52 ± 0.57 | 4.51 ± 0.58 |
GP, general practitioner; PPOS, Patient–Practitioner Orientation Scale.
We correlated the response rate per GP with the satisfaction scores of the corresponding patients to check whether satisfied patients are more likely to respond. We found that the correlation between the response rate and patient satisfaction was close to zero (r = −0.09). We also checked for the possibility that GPs would select patients with similar attitudes to their own by correlating response rate with difference score, this result was again, ignorable (r = −0.1).
Determinants of the patients’ sharing scores
We ran a linear regression with the patient sharing score as dependent variable and GP sharing score, GP age, GP gender, patient age, patient gender and patient educational level as independent variables. The results show that female gender has a positive and significant effect on patient sharing score (coeff. = 0.13; CI = 0.05–0.21). Compared with compulsory education completion of upper secondary education and college education had a positive and significant effect on patient sharing scores; (coeff. = 0.12, CI = 0.03–0.22) and (coeff. = 0.29, CI = 0.19–0.39) respectively.
Determinants of patient satisfaction
We investigated whether GP attitudes to sharing and congruence in attitudes between doctor and patient influence patient satisfaction. To test this we used logistic regression with the patient's satisfaction score as dependent variable, and the GP sharing score and the difference score as independent variables. In the same operation, we corrected for a range of other characteristics that are known to influence patient satisfaction (such as the patient's and doctor's age and gender, the doctor's work load and satisfaction with list length). The results are shown in Table 3. A high positive coefficient indicates a strong positive effect of the variable on patient satisfaction.
Table 3.
Logistic regression: determinants of patient satisfaction
| Variable | Odds ratio | 95% CI | Coefficients |
|---|---|---|---|
| GP sharing score | 1.57785* | 1.06161 2.34512 | 0.11293 |
| Difference score | 1.35852 | 0.96394 1.91462 | 0.07587 |
| Patient age | 1.01930** | 1.00963 1.02910 | 0.00473 |
| Patient gender1 | 0.60042** | 0.42781 0.84270 | −0.12660 |
| Education (upper second)2 | 1.09025 | 0.78092 1.52211 | 0.02138 |
| Education (college)3 | 0.92960 | 0.63070 1.37011 | −0.01809 |
| Switched GP1 | 0.87912 | 0.61336 1.26003 | −0.03190 |
| GP age | 1.00176 | 0.97650 1.02768 | 0.00044 |
| GP gender1 | 1.08505 | 0.70361 1.67328 | 0.02023 |
| GPs in the practice | 0.99441 | 0.85117 1.16176 | −0.00139 |
| List length/1000 | 1 | 0.99962 1.00038 | 0.00119 |
| Prefer longer list1 | 1.26732 | 0.75188 2.13611 | 0.05803 |
Figures presented are odds ratio, 95% confidence interval and coefficients as marginal effects.
1The effect is for discrete change of dummy variable from 0 to 1, where 0 represents female gender, no wish of longer list and not switched GP.
2Dummy variable: 1, upper secondary; 0 otherwise.
3Dummy variable: 1, college; 0 otherwise.
*P < 0.05; **P < 0.01.
We found that the GP sharing score is a strong and significant predictor of patient satisfaction. GP sharing score is included both as a main effect and as part of the difference score in Table 3. Thus, the effect of GP sharing score is a combination of the coefficients on those two variables. Increasing GP sharing score by one unit on the six‐point Likert scale increases patient satisfaction by 18 percentage points. We found no significant association between the difference score and satisfaction.
We did not find any significant effects of other GP characteristics (age, gender, list length, satisfaction with list length) on patient satisfaction. We found significant effects of both patient's age and gender on satisfaction. Older patients are more likely to be satisfied than younger. There is a strong effect of gender on satisfaction. Female patients report significantly higher satisfaction scores than male patients (13 percentage points).
Discussion
As expected, we found that patients in general have a preference for shared decision making. More unexpected was the finding that the patients were more oriented towards shared decision making than the doctors, which is the opposite of what Krupat et al. 12 found using US data. The Norwegian GPs score lower on the PPOS instrument than the US GPs (4.31 as compared with 4.62), and the Norwegian patients score higher than the US patients (4.47 as compared with 4.25). An explanation for the higher scores of the US GPs compared with the Norwegian GPs could be the more market‐based health care system in the US where there is a tradition of emphasis on consumerism. However, it is difficult to explain why the Norwegian patients had a stronger preference for patient involvement than the US patients.
We found clear evidence that GPs who have a positive attitude to shared decision making have more satisfied patients. Furthermore, there is a positive effect of patient age and female gender on satisfaction. This is consistent with earlier studies which generally conclude that age is a positive predictor of satisfaction, while the association between gender and satisfaction is found to be more complex. 28 , 29 , 30
We did not, however, find that a fit in attitudes predicts patient satisfaction. This negative result merits emphasis. A plausible explanation for this could be that those GPs who focus on patient involvement are able to adapt their style to each patient's preferences. This implies that people appreciate a GP who allows them the possibility to participate in medical decisions even when they generally do not request information or influence in decision making. When patients use their freedom of choice to transfer the responsibility of making clinical decisions back to the GP, GPs who focus on patient preferences are also open to alleviating the patient of the responsibility and thereby taking a paternalistic role in the consultation. This is in line with earlier research suggesting that GPs tailor their approach to the patient's preferences for consultation style and that doctors with a participatory decision‐making style are the most flexible. 12 , 13
A possible weakness of the study that needs to be discussed is the outcome measure of patient satisfaction with the GP. This variable is based on the respondents’ assessment of their overall satisfaction with the doctor on a six‐point scale from not satisfied to very satisfied. The reason for using a crude and overall question was to simplify and shorten the questionnaire. Several studies of patient satisfaction distinguish between satisfaction with different aspects of the practice as accessibility and quality of services. 12 , 18 , 30 However, there is some previous evidence about what an overall question measure as compared with a multi‐item scale. This literature suggests that overall satisfaction scores are more closely related to assessment of the GP's professional skills and dimensions of the doctor–patient relationship then to issues of access and type of service. 30 , 31 Yet, as the aim of the paper was a first attempt to investigate the association between satisfaction as a crude measure of quality of services and attitudes to patient involvement, the specificities of what aspects of satisfaction we are measuring seem less important at this stage.
Another aspect of the satisfaction score that deserves some comment is the finding that 55% of the respondents of the working sample score six, which is the maximum score for satisfaction. One could ask whether this reflects a weakness of the measure. Still this finding was expected as Krupat et al. also found that the distribution of satisfaction scores was markedly skewed towards the top score, 12 and we know that overall satisfaction has a tendency to be rated higher than satisfaction with specific aspects of the doctor's service. 30 A recent UK study used in‐depth interviews to investigate what lies behind such findings, and concluded that respondents differentiate clearly between being ‘satisfied’ and ‘very satisfied’. 32
There are some specific limitations to this study connected to the respondent samples indicating that the results should be interpreted with a degree of caution: Firstly, the GP sample is small and we know little about what lies behind the decision to join the study. Although they seem to represent the Norwegian GP population in terms of observable characteristics (Table 1), we do not know whether there is a selection bias in terms of attitudes. We note that the participating GPs seem to have a preference for shorter lists than the average GP, which could be an indication of a bias in terms of attitudes. The expected bias would be that those doctors who are relatively concerned with how decisions are shared and are focused on patient involvement would be inclined to participate.
Another complicating factor in the study is that we delegated the distribution of questionnaires to the GPs. Hence we could not control any tendency to discriminate when distributing the questionnaires. One could argue that GPs would be likely to select the patients with whom they communicated best or those they believed thought well of them. However, Norwegian GPs generally are accustomed to anonymous participation in research projects and there is no obvious advantage they would gain by not following our instructions. Nevertheless, we tested for associations between response rate and satisfaction and between response rate and agreement in attitudes, but the associations were very weak. Additionally on the positive side, the patient sample has a majority of older and female patients, which is as expected as older and female patients consult their GP more frequently than younger and male patients. 13 , 33 , 34 , † We also find that female gender and high level of education are determinants of preference for shared decision‐making in the patient sample. This is also consistent with earlier literature (including Krupat's studies), which in addition indicate young age as a positive determinant. 4 , 12 , 31 , 35 However, the latter association is not supported in our study.
Finally, connected to the former point, the average patient response rate per GP is low. However, it is difficult to know if this reflects non‐responses from patients or if some GPs stopped the distribution of questionnaires. The remarkable variation in response rate per GP suggests that the real response rate is considerably higher than the response rate we are able to register.
Concluding remarks
The study shows that the great majority of patients prefer to be involved in medical decision making, but contrary to an earlier US study, we find that Norwegian GPs are less oriented towards shared decision making than are their patients.
Interestingly patients are more satisfied when the GP is in favour of shared decision making even when the patient is less positive to shared decision making. It seems like the success of the high‐scoring doctors is not so much their attitudes towards sharing of information and decisions as their aspiration to recognize the patients’ differing orientations and respond to these. Therefore, even though patients’ preferences vary there is reason to continue promoting the participatory consultation style.
There is a need for further European studies mapping attitudes towards patient involvement in medical consultations, and it would be valuable if such future studies were to utilize already established measures.
Acknowledgements
This study was financed by the Research Council of Norway through the Programme for Health Economics in Bergen. The opinions expressed in this paper are those of the authors, not necessarily those of the Research Council.
The authors gratefully acknowledge the contribution of the GPs participating in collecting the data and the patients who answered our questionnaire. We would like to thank Ole Frithjof Norheim for valuable editing and advice in the preparation of the survey and the manuscript. We also thank Sturle Næss for suggestions and guidance in the construction of the survey and John Cairns for helpful comments on the revised version of the manuscript.
Appendix 1
Patient–provider orientation scale items (PPOS) (Krupat et al.) 12
-
1
The patient is the one who should decide what gets talked about during a visit.
-
2
It is often best for patients if they do not have a full explanation of their medical condition.
-
3
Patients should not only rely on their doctor's knowledge but try to find out about their conditions on their own.
-
4
Many patients continue asking questions until they understand the information given by the doctor.
-
5
Patients should be treated as if they were partners with the doctor, equal in power and status.
-
6
When patients disagree with their doctor, this is a sign that the doctor does not have the patient's respect and trust.
-
7
Most patients appreciate to take their time in the doctor's office.
-
8
The patient must always be aware that the doctor is in charge.
-
9
When patients look up medical information on their own, this usually confuses more than it helps.
Footnotes
Some physicians had very few responding patients, which we interpret as a sign that the physician had withdrawn from the study, as it is unlikely that the response rate was so low. This interpretation is supported by the fact that the distribution of the response rate is skewed: the mean response rate is 22.64 and the median response rate is 25.
According to the consultation rates for general practice presented in Carr‐Hill et al., 33 about 60% of consultations include female patients. Kaplan et al.’s study of physicians’ participatory decision‐making styles verified a similar gender ratio in consultations (61.3% females). The mean age of the patients in Kaplan et al.’s study was 46.5 years (1995).
References
- 1. Frank RG. Behavioral economics and health economics In: NBER Working paper series. Cambridge, MA: Cambridge National Bureau of Economic Research, 2004: 10881. [Google Scholar]
- 2. Scott A. Economics of General Practice In: Culyer AJ, Newhouse JP. (eds) Handbook of Health Economics. Amsterdam: Elsevier Science, 2000: 1175–1200. [Google Scholar]
- 3. Steinhart B. Patient autonomy: evolution of the doctor–patient relationship. Haemophilia, 2002; 8: 441–446. [DOI] [PubMed] [Google Scholar]
- 4. Benbassat J, Pilpel D, Tidhar M. Patients’ preferences for participation in clinical decision making: A review of published surveys. Behavioral Medicine, 1998; 24: 81–88. [DOI] [PubMed] [Google Scholar]
- 5. Charles C, Gafni A, Whelan T. Shared decision‐making in the medical encounter: What does it mean? (or it takes at least two to tango). Social Science & Medicine, 1997; 44: 681–692. [DOI] [PubMed] [Google Scholar]
- 6. Jones IR, Berney L, Kelly M et al. Is patient involvement possible when decisions involve scarce resources? A qualitative study of decision‐making in primary care. Social Science & Medicine, 2004; 59: 93–102. [DOI] [PubMed] [Google Scholar]
- 7. Sculpher M, Gafni A, Watt I. Shared treatment decision making in a collectively funded health care system: possible conflicts and some potential solutions. Social Science & Medicine, 2002; 54: 1369–1377. [DOI] [PubMed] [Google Scholar]
- 8. Schattner A, Rudin D, Jellin N. Good physicians from the perspective of their patients. BMC Health Services Research, 2004; 4: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ogden J, Ambrose L, Khadra A et al. A questionnaire study of GPs’ and patients’ beliefs about the different components of patient centredness. Patient Education and Counseling, 2002; 47: 223–227. [DOI] [PubMed] [Google Scholar]
- 10. Stiggelbout AM, Molewijk AC, Otten W, Timmermans DRM, Van Bockel JH, Kievit J. Ideals of patient autonomy in clinical decision making: a study on the development of a scale to assess patients’ and physicians’ views. Journal of Medical Ethics, 2004; 30: 268–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haug MR, Lavin B. Practitioner or Patient‐Who's in Charge? Journal of Health and Social Behavior, 1981; 22: 212–229. [PubMed] [Google Scholar]
- 12. Krupat E, Rosenkranz SL, Yeager CM, Barnard K, Putnam SM, Inui TS. practice orientations of physicians and patients: the effect of doctor – patient congruence on satisfaction. Patient Education and Counseling, 2000; 39: 49–59. [DOI] [PubMed] [Google Scholar]
- 13. Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians’ participatory decision‐making style. Results from the medical outcomes study. Medical Care, 1995; 33: 1176–1187. [DOI] [PubMed] [Google Scholar]
- 14. Cecil D, Killeen I. Control, compliance and satisfaction in the family practice encounter. Family Medicine, 1997; 29: 653–657. [PubMed] [Google Scholar]
- 15. Finkler K, Correa M. Factors influencing patient perceived recovery in Mexico. Social Science & Medicine, 1996; 42: 199–207. [DOI] [PubMed] [Google Scholar]
- 16. Grol R, Maeseneer Jd, Whitfield M, Mokkink H. Disease‐centred versus patient‐centred attitudes: comparison of general practitioners in Belgium, Britain and The Netherlands. Family Practice, 1990; 7: 100–103. [DOI] [PubMed] [Google Scholar]
- 17. Langewitz W, Phillipp E, Kiss A, Wossmer B. Improving communication skills: a randomized controlled behaviorally‐oriented intervention study for residents in internal medicine. Psychosomatic Medicine, 1998; 60: 268–276. [DOI] [PubMed] [Google Scholar]
- 18. Little P, Everitt H, Williamson I et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. British Medical Journal, 2001; 323: 908–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Greenfield S, Kaplan S, Ware JE, Expanding patient involvement in care. Effects on patient outcomes. Annals Of Internal Medicine, 1985; 102: 520–528. [DOI] [PubMed] [Google Scholar]
- 20. Hibbard JH. Perspective: Moving Toward A More Patient‐Centered Health Care Delivery System. Health Affairs, 2004: Web exclusive: 1377/hlthaff.var.133. [DOI] [PubMed] [Google Scholar]
- 21. Kaplan SH, Greenfield S, Ware JE. Assessing the effect of physician‐patient interaction on the outcomes of chronic disease. Medical Care, 1989; 27: 110–127. [DOI] [PubMed] [Google Scholar]
- 22. Rost KM, Flavin KS, Cole K, McGill JB. Change in metabolic control and functional status after hospitalization. Impact of patient activation intervention in diabetic patients. Diabetes Care, 1991; 14: 881–889. [DOI] [PubMed] [Google Scholar]
- 23. Greenfield S, Kaplan SH, Ware JE, Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. Journal Of General Internal Medicine, 1988; 3: 448–457. [DOI] [PubMed] [Google Scholar]
- 24. Mead N, Bower P. Patient‐centredness: a conceptual framework and review of the empirical literature. Social Science & Medicine, 2000; 51: 1087–1110. [DOI] [PubMed] [Google Scholar]
- 25. Krupat E, Bell R, Kravitz R, Thom D, Azari R. When physicians and patients think alike: patient‐centered beliefs and their impact on satisfaction and trust. Journal of Family Practice, 2001; 50: 1057–1062. [PubMed] [Google Scholar]
- 26. Krupat E, Yeager CM, Putnam S. Patient role orientations, doctor – patient fit, and visit satisfaction. Psychology and Health, 2000; 15: 707–719. [Google Scholar]
- 27. Hetlevik Ø, Hunskår S. Listelengde, arbeidstid, ventetid og jobbtilfredshet blant fastleger i Bergen. (Length of patient list and workload, waiting time and job satisfaction among general practitioners.). Tidsskrift for Den Norske Lægeforening, 2004; 124: 813–815. [PubMed] [Google Scholar]
- 28. Campbell JL, Ramsay J, Green J. Age, gender, socioeconomic, and ethnic differences in patients’ assessments of primary health care. Quality in Health Care, 2001; 10: 90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Finnvold JE, Lurås H, Paulsen B. Fastlegeordningen. De fleste fikk den de ville ha. (The regular general practitioner scheme: most people got the GP they wanted). Samfunnsspeilet, 2003; 17: 2–11. [Google Scholar]
- 30. Williams S, Calnan M. Key determinants of consumer satisfaction with general practice. Family Practice, 1991; 8: 237–242. [DOI] [PubMed] [Google Scholar]
- 31. Krupat E, Hsu J, Irish J, Schmittdiel JA, Selby J. Matching Patients and Practitioners Based on Beliefs About Care: Results of a Randomized Controlled Trial. The American Journal of Managed Care, 2004; 10: 814–822. [PubMed] [Google Scholar]
- 32. Collins K, Cathain A. The continuum of patient satisfaction–from satisfied to very satisfied. Social Science & Medicine, 2003; 57: 2465–2470. [DOI] [PubMed] [Google Scholar]
- 33. Carr‐Hill RA, Rice N, Roland M. Socioeconomic determinants of rates of consultation in general practice based on fourth national morbidity survey of general practices. British Medical Journal, 1996; 312: 1008–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Finnvold JE, Svalund J. Kontinuitet mellom lege og pasient: Blanda resultat av fastlegereforma. (Continuity of care. Mixed results of The regular general practitioner scheme.). Samfunnsspeilet, 2004; 18: 27–33. [Google Scholar]
- 35. Weisman CS, Teitelbaum MA. Physician gender and the physician‐patient relationship: recent evidence and relevant questions. Social Science & Medicine, 1985; 20: 1119–1127. [DOI] [PubMed] [Google Scholar]
- 36. Rikstrygdeverket . Styringsdata for fastlegeordningen. (The National Insurance Administration: Statistics of The regular general practitioner scheme). 2004. [Available at http://www.trygdeetaten.no/tallmrog_mrfakta/Statistikker/folgerapporter/20040211/02.html] (accessed December 7th 2004). [Google Scholar]
- 37. Taraldset A. Allmennleger–antall og utvikling. (General Practitioners – Numbers and development). Utposten, 2003; 4(32). [Available at http://www.uib.no/isf/utposten/2003nr4/utp03410.htm] (accessed December 7th 2004). [Google Scholar]


