Abstract
Background Responding to the preferences of patients is a key focus of current health policy and is especially important in primary care. Responding effectively to patient preferences requires a clear understanding of the way in which patients assess primary care services.
Objective This study was designed to provide a ‘map’ of the content and structure of the key attributes of patient preferences concerning primary care.
Design The development of the ‘map’ used secondary research methods. Electronic databases were searched for published conceptual reviews of patient preferences, which were used to develop a basic ‘map’ through content analysis. A search for recently published primary empirical studies of patient preferences was conducted to extend and develop the ‘map’. The ‘map’ was tested by taking a random sample of patient assessment instruments and categorizing the item content.
Results Seven major categories and multiple subcategories were described. The major categories were access, technical care, interpersonal care, patient‐centredness, continuity, outcomes, and hotel aspects of care. The coverage of these attributes in a selection of patient assessment instruments varied widely, and the coding of a proportion of items in the patient assessment instruments according to the ‘map’ was problematic.
Conclusions The conceptual ‘map’ can be used to plan comprehensive assessment of patient preferences in primary care. It also raises many theoretical issues concerning the nature of attributes and their interrelationships. The implications for the measurement of patient preferences are discussed.
Keywords: patients, preferences, primary care, review
Introduction
Responding to the preferences of patients concerning, the delivery of health care is an important aspect of current health policy worldwide. 1 This is especially relevant to primary care, which has traditionally been viewed as health care, which is oriented to the needs of patients rather than focussed on technology. 2 , 3
Generally, preferences are viewed as ideas about what should happen, which can be distinguished from patient satisfaction, which is the assessment of care that has been provided. 4 It has been hypothesized that preferences will drive assessments of satisfaction, because meeting the needs of patients will generally lead to higher levels of satisfaction. 5
Preferences for and satisfaction with non‐health commodities (e.g. cars) will relate to many key attributes (e.g. comfort, speed and price). Although the exact process of decision‐making in health care may be different, likely patient preferences for primary care will also involve many key attributes. Previous reviews have described several attributes, including availability and accessibility, practice organization, and communication, information and support. 6 However, previous reviews may not exhaust all attributes of relevance, especially in the developing field of health care and health policy. For example, current government policy in the UK has highlighted the issue of ‘patient choice’ in health care. 1
Understanding the key attributes underlying patient preferences concerning primary care is important. Technologies for the assessment of preferences and satisfaction (such as patient assessment questionnaires) are increasingly being linked with mechanisms of change (such as financial incentives). Therefore, the particular attributes included in those assessments may drive change, and if important attributes are omitted, there is a danger that change will prioritize certain attributes at the expense of others. 7 In addition, within the context of the limited resources available to the National Health Service (NHS), patient preferences for certain attributes may be in conflict, 8 which raises issues of priority.
Therefore, it is important to develop a clear understanding of the nature of patient preferences. Such an understanding requires both knowledge about the content of patient preferences (i.e. the different attributes of relevance) and the structure of those preferences (i.e. the way in which different attributes interrelate). Such an understanding can be likened to a conventional ‘map’, which illustrates both the content of an area (e.g. the key towns, rivers and elevation) and the relationships between them (e.g. distance and bearing).
Developing such a conceptual ‘map’ of the key attributes of primary care can involve many different methods. Qualitative work with patients is one obvious approach, but the resource intensive nature of such methods means that only a limited sample of views can be gathered, and the results may be very specific to the particular context of the data collection. In the present study, secondary research methods were used. The aims of the study were:
-
1
To develop a ‘map’ of the key attributes of primary care of importance to patients, indicating (a) the content of those attributes, (b) the relationship between different attributes.
-
2
To test the ‘map’ by examining the relationship between the attributes included in the ‘map’, and the attributes included in current patient assessment questionnaires used in the primary care setting.
Methods
Developing the ‘map’
Two methods were used for the development of the ‘map’.
-
1
Examination of conceptual reviews in the peer reviewed the literature concerning key attributes of primary care.
-
2
Electronic database searches of primary empirical studies of patient preferences concerning key attributes in primary care.
The overall structure of the project and the relationships between the methods are shown in Fig. 1, and described in more detail below.
Figure 1.
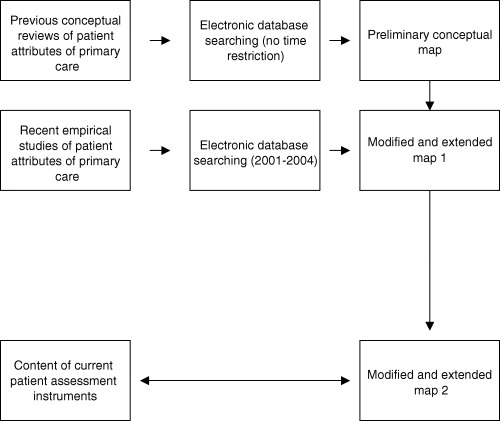
Methods used in the study.
A list of search terms was developed in a short series of brainstorming sessions and expanded by scanning of key articles and reviews for further synonyms. The final list comprised the term ‘patient’ and five synonyms (user, client, carer, consumer and customer), and the term ‘priorities’ and six synonyms (choice, perspective, preference, attitude, views and expectations). All permutations were included, and truncations were used as appropriate. To focus the search and because of the conceptual distinction between preference and satisfaction discussed earlier, 4 terms relating to satisfaction were excluded. The complete search strategy is available from the authors.
The search was conducted in MEDLINE, EMBASE and PsycInfo in August 2004. Thesaurus terms were selected on the basis of those that most closely matched the above terms, and free‐text terms were limited to the title of the document to increase specificity (at some cost of sensitivity).
It was felt that the published conceptual reviews would provide good coverage of a broad range of primary care attributes that have been previously studied, while examination of more recent primary studies would provide a contemporary perspective. Therefore, in the searches for published conceptual reviews, no time restriction was placed on the search, while the search for primary empirical studies was restricted to articles published between 2001 and 2004. Published conceptual reviews were also sought in the reference lists of the research team.
All references were reviewed independently by two researchers. Inclusion criteria were that articles: (a) focused on primary care; (b) the research questions related to patient preferences for particular attributes of primary health care; and (c) were published in the English language. Relevant attributes were extracted from the abstracts of papers. Disagreements were resolved through discussion.
Data synthesis proceeded as follows. The published conceptual reviews were used to develop a basic ‘map’. Attributes were extracted from each review, and the full list subjected to a content analysis to eliminate redundancy and provide an overall structure. Then, the list of attributes derived from the review of primary empirical studies were categorized according to this basic ‘map’, and used to extend and develop it where appropriate (e.g. through the addition of new categories or subcategories).
Testing the ‘map’
Patient assessment instruments used in the primary care setting were identified from colleagues conducting a separate systematic review in this area. A random sample of one‐third (n = 10) of the instruments were selected. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 All the items in each instrument were then listed, and then categorized according to the ‘map’ by two authors working independently.
Results
A total of 227 references were identified by the electronic searches for published conceptual reviews, and 1146 for the electronic searches for primary empirical studies. Many of the studies identified by the former were inappropriate, and the bulk of the published conceptual reviews were identified from the reference lists of the research team. Of the primary empirical studies identified, 219 were included in the analysis after review (reference list available from the first author). References were excluded for many reasons; for example, where they related to preferences concerning specific treatments within primary care, as opposed to primary care service attributes more generally.
Results of the reviews
As expected, there was a significant amount of overlap between the published conceptual reviews. 6 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 Six major attributes related to the process of care from the patient perspective (access, technical care, interpersonal care, patient‐centredness, continuity and hotel aspects of care), together with the attribute of the outcome of care. However, each of these major attributes has multiple subcategories.
Generally, the attributes derived from the search for primary empirical studies could be coded according to this preliminary ‘map’. However, the process of coding led to restructuring of the ‘map’ and the addition of subcategories (Table 1).
Table 1.
Final conceptual ‘map’
| Category | Subcategory and definition | Definition and/or examples |
|---|---|---|
| Access | Access to care in general | Practice location, waiting time in the surgery, out of hours services |
| Access to preferred and personalized services | Choice of appointments, availability of specific practitioners (e.g. female doctor) | |
| Technical care | Primary care provider type | General practitioners or nurses |
| Provider training and competence | Knowledge, experience, professionalism | |
| Clinical skills | Physical examination, diagnostic accuracy | |
| Boundaries | Touch and intimacy | |
| Interpersonal care | Attitude | Patience, compassion, respect |
| Communication skills | Clarity of communication and explanation | |
| Boundaries | Privacy and intimacy | |
| Patient‐centredness | Biopsychosocial perspective | Taking account of the medical, psychological and social aspects of medical problems |
| Patient as person | Treating patient as an individual, listening to the patient's story | |
| Sharing power and responsibility | Providing informed consent, engaging in a partnership with patients | |
| Therapeutic alliance | Displaying mutual respect, agreement, collaboration, trust | |
| Doctor as person | Recognition of the influence of the personal qualities of the doctor on the practice of medicine | |
| Continuity | Informational continuity | Copying letters and test results |
| Management continuity | Consistent and coherent approach to management responsive to patient's changing needs, e.g. during hospital stay, post‐discharge | |
| Longitudinal continuity | Care from as a few professionals as possible, consistent with needs | |
| Relational/interpersonal | Providing a named professional with whom a therapeutic relationship can develop | |
| Outcomes | Health status, quality of life, enablement, satisfaction | |
| Hotel aspects | Comfort of the waiting room, car parking, doctor dress |
As well as general issues concerning access to care, several studies examined whether patients could access the specific type of care that they wanted: an example was the desire to consult with a practitioner of a similar cultural background. In response, an additional access subcategory was introduced to the ‘map’ (access to preferred and personalized services) to reflect this. Boundary issues relating both to physical and psychological intimacy were also found in the primary empirical studies, and thus a subcategory relating to ‘boundaries’ was added to both technical and interpersonal care categories.
In addition to the ‘boundaries’ subcategory, the interpersonal care attribute was further divided into two more subcategories. ‘Attitude’ was defined as relating to the personality attributes of the clinician (such as ‘the doctor seems to take my problem seriously’). ‘Skills’ were defined as generic communication behaviour (such as ‘the doctor explains and clarifies information for me’). ‘Patient‐centredness’ was considered an entirely separate attribute, defined in terms of multiple dimensions according to current theoretical models 24 , 27 .
Table 2 shows the sampled patient assessment instruments and the dimensions of the ‘map’ that they covered. As can be seen, although many attributes were common across questionnaires, others were found in some and not others, while some attributes were rarely measured at all. The process of coding items also indicated that individual items in questionnaires often had an ambiguous relationship with the ‘map’. Some examples of ambiguity in the meaning of items are given in Table 3. By far the greatest ambiguity related to issues of ‘interpersonal care’ and ‘patient‐centredness’.
Table 2.
Classification of patient assessment instruments according to the conceptual ‘map’
| Access | Technical care | Interpersonal care | Patient‐centredness | Continuity | Outcomes | Hotel aspects | Other | Ambiguous | |
|---|---|---|---|---|---|---|---|---|---|
| CPCI 12 (19 items) | – | – | 1 | 5 | 11 | – | – | – | 2 |
| PSQ 13 (40 items) | 8 | 5 | 2 | 1 | – | – | 4 | – | 20 |
| IPQ 14 (27 items) | 5 | 2 | 1 | 2 | 1 | – | 1 | 1 | 14 |
| PCAS 9 (48 items) | 8 | 7 | 3 | 13 | 4 | – | – | – | 13 |
| EUROPEP 11 (38 items) | 8 | 7 | 2 | 4 | 5 | 2 | – | 2 | 8 |
| MISS 15 (21 items) | – | 2 | 1 | 7 | – | 1 | – | – | 10 |
| QPP 17 (37 items) | 10 | 7 | 1 | 6 | 1 | – | 5 | – | 7 |
| PHBQ 16 (25 items) | – | – | 3 | 11 | – | – | 1 | – | 10 |
| PDRQ‐9 10 (15 items) | 1 | – | – | 3 | – | 5 | – | – | 6 |
| PEQ 18 (18 items) | – | – | – | 4 | – | 8 | – | – | 6 |
Table 3.
Examples of ambiguous items from patient assessment instruments
| Item content | Comments |
|---|---|
| The doctor is always interested | This item may refer to perceptions of the provider's personality (category interpersonal care, subcategory attitude) or is more specific to their interest in the particular views of the patient (category patient‐centredness, subcategory patient as person) |
| The opportunity for making compliments or complaints to this practice about its service and quality of care | This item may refer to the openness of the practice staff to feedback (category interpersonal care, subcategory attitude), or to the physical opportunity to provide feedback, i.e. a suggestion box (category hotel aspects) |
| If a mistake was made in my treatment, my doctor would try to hide it from me | This item may refer to the provider's diagnostic skills (category technical care, subcategory clinical skills), professionalism (category technical care, subcategory training and competence) or to a perception of the quality of the doctor–patient relationship (category patient‐centredness, subcategory therapeutic alliance) |
| Seems knowledgeable and concerned about me and my case | This item may refer to the provider's medical knowledge (category technical care, subcategory training and competence), concern for the patient (category interpersonal care, subcategory attitude) or their knowledge of the individual (category patient‐centredness, subcategory patient as person) |
| I do not feel confident discussing my problems with the doctor | This item may refer to perceptions of the provider's diagnostic skills (category technical care, subcategory clinical skills) or other concerns about the doctor–patient relationship (category patient‐centredness, subcategory therapeutic alliance) or issues of privacy (category interpersonal care and subcategory boundaries) |
Discussion
Limitations of the study
The methods adopted in the present study represent a ‘top‐down’ approach to the development of a ‘map’ of attributes, and can be contrasted with a ‘bottom‐up’ approach best characterized by qualitative methods. Triangulation of the results of the present methods with alternatives would be appropriate. However, it should be noted that the benefit of the ‘top‐down’ approach is access to a wide range of patient populations, in terms of country of origin, age and social groups. For example, in the present study, data were derived from populations in such diverse places as Lithuania, Saudi Arabia, Australia, Denmark, Ireland, Slovenia and Israel. Such a wide sampling of views has significant advantages in terms of the development of a widely generalizable list of attributes. However, the restriction of the search to the studies published in English means that the map may not include issues of relevance to all contexts worldwide. Furthermore, combining findings from such diverse health‐care contexts may have additional disadvantages, because the broad attributes described in the map may be insensitive to differences between the meaning of attributes in different sociocultural contexts.
There were limitations to the search strategies employed. The electronic database search for published conceptual reviews was particularly poor in yield. This may reflect the fact that conceptual issues are generally poorly indexed and inconsistently labelled in the electronic databases. The examination of primary empirical studies used the abstracts to extract data, and possibly the full text might have included additional attributes of relevance.
The content of the ‘map’
Examination of the content of empirical studies of patient priorities in the last 3 years indicates that a wide variety of individual attributes have been examined in the empirical literature. Of course, the amount of coverage of each issue varies very widely, and there are many more studies of the major attributes (i.e. interpersonal care, access and continuity) than other issues.
The ‘map’ presented in the present paper expands on previous reviews of attributes in several ways. Some new content areas have been presented, such as the issue of physical and psychological ‘boundaries’. The latter is of particular interest, because the focus of much of the present literature on interpersonal skills and patient centredness in primary care is on increasing the psychological content of the consultation and encouraging primary care professionals to consider the personal lives of their patients. Far less attention has been given to the possible adverse effects of such a focus. 28
The proposed ‘map’ also makes a tentative distinction between ‘attitude’, ‘communication skills’ and ‘patient‐centredness’. This distinction is supported by recently published qualitative work on characteristics or behaviour that are valued by patients. In this study (conducted outside primary care), patients reported on doctors’ characteristics or behaviour that they valued. The results indicated that enduring personal characteristics and individuality were distinguished from more specific skills such as giving information. 29 However, although this distinction may make some conceptual sense, the present study found that these sorts of distinctions may not be clearly reflected in the items used in patient assessment instruments, which may reduce its practical utility.
It is a reflection of the general consensus in the academic literature concerning the difficulty of associating primary care provision with patient outcomes that the issue of outcome was rarely discussed, especially in the review of primary empirical studies. This may reflect the self‐limiting nature of many primary care disorders and the multiple confounding factors that might equally account for any change. 30 However, it is implicit in the new quality and outcomes framework in the UK that primary care can influence outcomes, 31 and thus this dimension may be a more important aspect of primary care assessment in the future.
The structure of the ‘map’
As noted in the introduction, a conventional ‘map’ shows both the content of the area (e.g. the key towns, rivers and elevation) and the relationships between them. Table 1 functions much more effectively in terms of the former than the latter, but this discussion will consider the relationships between attributes in greater depth.
Some attributes are necessary preconditions for others. For example, ‘access to preferred and personalized services’ is dependent on ‘access’ itself, and likely the former will only become an issue when problems with the latter have been addressed. Therefore, the relevance of particular aspects of the ‘map’ may depend on the level of development of the health‐care system. This would also imply that very advanced systems may gradually develop new attributes of relevance as preferences for more ‘basic’ attributes are met.
Other attributes may have ‘causal’ linkages. For example, the attribute of ‘primary care provider type’ may imply certain levels of training and competence, which in turn imply certain clinical skills. Similarly, judgements of outcome might be dependent on judgements about other process characteristics. For example, health status may be viewed as a consequence of high technical and interpersonal care rather than as an independent attribute. Equally, certain attributes of patient‐centredness (e.g. trust and collaboration) may be a result of continuity, if they are dependent on an ongoing relationship over time. In this sense, continuity may function as a ‘platform’ for the delivery of other attributes rather than a fundamental attribute in its own right.
Other attributes may represent the same common concept, but reflect different ways of conceptualizing it. For example, in relation to the distinction made between ‘attitude’ and ‘communication skills’, it might be hypothesized that doctors’ behaviour in the consultation is the basis for judgements of both. Similarly, the distinctions made in the ‘map’ in relation to ‘interpersonal care’ and ‘patient‐centredness’ may not be perceived by patients, because of the operation of processes such as the ‘halo effect’ which means that patients do not made the sort of fine‐grained distinctions implied by the ‘map’. 32 , 33 However, this does not mean that the distinctions made are redundant. Previous work has suggested that a doctor displaying similar behaviour may be judged differently if that behaviour is seen as a reflection of contextual pressures (e.g. workload and lack of time) rather than an enduring personality characteristic. 34 In some contexts, the different labels may reflect important distinctions. Clearly, this is an area that would benefit from further primary research.
Making sense of patient responses to attributes of primary care
The attributes included in the ‘map’ represent a mix of concrete service attributes (e.g. waiting times and type of provider), and broader attributes (e.g. respect and trust). Generally, measurement technologies such as patient assessment instruments treat such variables as operating at similar levels of meaning (in the sense that they will be weighted and scored similarly). However, it is not clear that they should necessarily be viewed in this way.
Possibly the distinction made earlier between articulated and basic values 35 may have relevance here. According to the theory of basic values, patients only have pre‐determined preferences for a small set of issues of immediate concern. For example, everyday experience with primary care in the UK NHS probably highlights the importance of waiting times for consultations, and likely patients will have articulated preferences relating to this issue. However, when faced with novel attributes (such as issues around ‘choice’), patients may not have an experiential basis within health care to make an immediate response, and therefore construct preferences only when faced with such issues.
Possibly these constructed responses may relate to more basic values. Values are abstract, meaning‐producing cognitive structures, and relate to fundamental needs, desires and conflicts. 36 It is hypothesized that there are a finite number of universal values. Making a judgement of preference for a novel entity means judging it with reference to this abstract value system structure. It is noteworthy that a recent systematic review found that one of the strongest predictors of patient preferences was religion, 4 where values might be expected to be highly salient. This might also be consistent with recent work on expression of dissatisfaction, which suggest that negative evaluations of health care are related to ‘perceived identity threat’ through processes such as being dehumanized, disempowered and devalued. 37 If judgements of concrete service attributes (such as access times) are a function of values, judgements about health care may need to be conceptualized very differently from those of other commodities.
The relationship between service attributes and values may not always be clear. For example, offering patients longer consultations in primary care may relate to values concerning safety (because of the greater scope for high quality medical care), relationships (because of the greater time for discussion and the development of a therapeutic relationship) or respect (because the option to spend longer with a doctor is a reflection of the value placed on the individual patient within the health‐care system). Examining such relationships might be important, as possibly services with different attributes may be assessed in the same way if they meet the same values. For example, access to a doctor who is of the same ethnic background (i.e. the category of ‘access to preferred and personalized services’) may be important to the degree it implies ease of communication, lack of stereotyping and suchlike. But if the same communication and sensitivity can be displayed by a doctor from a different background, then does the initial attribute become less important? If this model has some validity, it raises questions concerning the fundamental values that underpin patient perceptions of health care and primary care.
Methodological implications of the study
The results of the present study have implications for assessment technologies such as patient assessment instruments and discrete choice experiments. 38 The final ‘map’ provides a comprehensive assessment of the full range of attributes of relevance to patients. However, the wide scope of potential attributes may be problematic. Reflecting the wide range of attributes may make these methodologies unwieldy for practical use, but limiting assessments to a subset of attributes may mean that responses simply reflect the limited nature of the comparison. Clearly, care must be taken in the interpretation of scores from patient assessment instruments that may be based on very different content domains.
Secondly, the results suggest a lack of linkage between theoretical concepts in primary care research, and the content of items used in relation to current assessment instruments. Clearly, the development of item content is a complex undertaking, and theoretical coherence is only one determinant among other important factors, such as readability and clarity. However, the difficulties faced in categorizing a significant proportion of patient assessment items according to the categories of the ‘map’ suggests the need for a closer link between the empirical process of questionnaire development and the theoretical and conceptual basis of patient preferences.
Acknowledgements
The authors would like to thank Ros McNally (Library and Information Manager, NPCRDC) for assistance with the literature searches. The NPCRDC is funded by the Department of Health, but the views expressed in the paper are those of the authors alone.
References
- 1. Department of Health . Building on the Best: Choice, Responsiveness and Equity in the NHS. London: HMSO, 2003. [Google Scholar]
- 2. Starfield B. Primary Care: Concept, Evaluation and Policy. New York: Oxford University Press, 1992. [Google Scholar]
- 3. Fry J, Horder J. Primary Health Care in an International Context. Abingdon: Wace Burgess, 1994. [Google Scholar]
- 4. Jung H, Baerveldt C, Olesen F, Grol R, Wensing M. Patient characteristics as predictors of primary health care preferences: a systematic literature analysis. Health Expectations 2003; 6: 160–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Linder‐Pelz S. Social psychological determinants of patient satisfaction: a test of five hypotheses. Social Science and Medicine 1982; 16: 583–589. [DOI] [PubMed] [Google Scholar]
- 6. Wensing M, Jung H, Mainz J, Olesen F, Grol R. A systematic review of the literature on patient priorities for general practice care. Part 1: description of the research domain. Social Science and Medicine 1998; 47: 1573–1588. [DOI] [PubMed] [Google Scholar]
- 7. Marshall M, Davies H. Public release of information on quality of care: how are health services and the public expected to respond? Journal of Health Services Research and Policy 2001; 6: 158–162. [DOI] [PubMed] [Google Scholar]
- 8. Bower P, Roland M, Campbell J, Mead N. Setting standards based on patients’ views on access and continuity: secondary analysis of data from the general practice assessment survey. British Medical Journal 2003; 326: 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gelb Safran D, Kosinski M, Tarlov M et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Medical Care 1998; 36: 728–739. [DOI] [PubMed] [Google Scholar]
- 10. Van der Feltz‐Cornelis P, Van Oppen P, Marwijk H, De Beurs E, Van Dyck R. A patient–doctor relationship questionnaire (PDRQ‐9) in primary care: development and psychometric evaluation. General Hospital Psychiatry 2004; 26: 115–120. [DOI] [PubMed] [Google Scholar]
- 11. Grol R, Wensing M, Mainz J et al. Patients’ priorities with respect to general practice care: an international comparison. Family Practice 1999; 16: 4–11. [DOI] [PubMed] [Google Scholar]
- 12. Grogan S, Conner M, Norman P, Willits D, Porter I. Validation of a questionnaire measuring patient satisfaction with general practitioner services. Quality in Health Care 2000; 9: 210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rodney W, Quigley C, Werblun M, Sumbureru D, Shear C. Satisfaction of continuity patients in a family medicine residency: validation of a measurement tool. Family Practice Research Journal 1986; 5: 167–176. [PubMed] [Google Scholar]
- 14. Greco M, Powell R, Sweeney K. The Improving Practice Questionnaire (IPQ): a practical tool for general practices seeking patient views. Education for Primary Care 2003; 14: 440–448. [Google Scholar]
- 15. Meakin R, Weinman J. The ‘Medical Interview Satisfaction Scale’ (MISS‐21) adapted for British general practice. Family Practice 2002; 19: 257–263. [DOI] [PubMed] [Google Scholar]
- 16. Weaver M, Ow C, Walker D, Degenhardt E. A questionnaire for patients’ evaluations of their physicians’ humanistic behaviours. Journal of General Internal Medicine 1993; 8: 135–139. [DOI] [PubMed] [Google Scholar]
- 17. Narthorst‐Boos J, Munck I, Eckerlund I, Ekfeldt‐Sandberg C. An evaluation of the QSP and the QPP: two methods for measuring patient satisfaction. International Journal for Quality in Healthcare 2001; 13: 257–264. [DOI] [PubMed] [Google Scholar]
- 18. Steine S, Finset A, Laerum E. A new, brief questionnaire (PEQ) developed in primary health care for measuring patients’ experience of interaction, emotion and consultation outcome. Family Practice 2001; 18: 410–418. [DOI] [PubMed] [Google Scholar]
- 19. Wensing M, Grol R, Smits A. Quality judgements by patients on general practitioner care: a literature analysis. Social Science and Medicine 1994; 38: 45–53. [DOI] [PubMed] [Google Scholar]
- 20. Buetow S. What do general practitioners and their patients want from general practice and are they receiving it? A framework. Social Science and Medicine 1995; 40: 213–221. [DOI] [PubMed] [Google Scholar]
- 21. Campbell S, Roland M, Buetow S. Defining quality of care. Social Science and Medicine 2000; 51: 1611–1625. [DOI] [PubMed] [Google Scholar]
- 22. Gulliford M, Figueroa‐Munoz J, Morgan M et al. What does ‘access to health care’ mean? Journal of Health Services Research and Policy 2002; 7: 186–188. [DOI] [PubMed] [Google Scholar]
- 23. Freeman G, Olesen F, Hjortdahl P. Continuity of care: an essential element of modern general practice? Family Practice 2004; 20: 623–627. [DOI] [PubMed] [Google Scholar]
- 24. Mead N, Bower P. Patient‐centredness: a conceptual framework and review of the empirical literature. Social Science and Medicine 2000; 51: 1087–1110. [DOI] [PubMed] [Google Scholar]
- 25. McGuiness C, Sibthorpe B. Development and initial validation of a measure of coordination of health care. International Journal for Quality in Health Care 2003; 15: 309–318. [DOI] [PubMed] [Google Scholar]
- 26. Jung H, Van Horne F, Wensing M, Hearnshaw H, Grol R. Which aspects of general practitioners’ behaviour determine patients’ evaluations of care. Social Science and Medicine 1998; 47: 1077–1087. [DOI] [PubMed] [Google Scholar]
- 27. Stewart M, Brown J, Weston W, McWhinney I, McWilliam C, Freeman T. Patient‐Centred Medicine: Transforming the Clinical Method. London: Sage, 1995. [Google Scholar]
- 28. Chew‐Graham C, May C, Roland M. The harmful consequences of elevating the doctor–patient relationship to be a primary goal of the general practice consultation. Family Practice 2004; 21: 229–231. [DOI] [PubMed] [Google Scholar]
- 29. Burkitt Wright E, Holcombe C, Salmon P. Doctors’ communication of trust, care, and respect in breast cancer: qualitative study. British Medical Journal 2004; 328: 864–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Crombie I, Davies H. Beyond health outcomes: the advantage of measuring process. Journal of Evaluation in Clinical Practice 1998; 4: 31–38. [DOI] [PubMed] [Google Scholar]
- 31. Shekelle P. New contract for general practitioners. British Medical Journal 2003; 326: 457–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Phillips K, Johnson F, Maddala T. Measuring what people value: a comparison of ‘attitude’ and ‘preference’ surveys. Health Services Research 2002; 37: 1659–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Murphy K, Jako R, Anhalt R. Nature and consequences of halo error: a critical analysis. Journal of Applied Psychology 1993; 78: 218–225. [Google Scholar]
- 34. Williams B, Coyle J, Healy D. The meaning of patient satisfaction: an explanation of high reported levels. Social Science and Medicine 1998; 47: 1351–1359. [DOI] [PubMed] [Google Scholar]
- 35. Fischoff B. Value elicitation: is there anything in there? American Psychologist 1991; 46: 835–847. [Google Scholar]
- 36. Rohan M. A rose by any other name? The values construct. Personality and Social Psychology Review 2000; 4: 255–277. [Google Scholar]
- 37. Coyle J. Exploring the meaning of ‘dissatisfaction’ with health care: the importance of ‘personal identity threat’. Sociology of Health and Illness 1999; 21: 95–124. [Google Scholar]
- 38. Ryan M, Bate A, Eastmond C, Ludbrook A. Use of discrete choice experiments to elicit preferences. Quality in Health Care 2001; 10: i55–i60. [DOI] [PMC free article] [PubMed] [Google Scholar]


