Abstract
Background This study investigated patient opinion about the provision of nurse‐led vs. doctor‐led primary health care in the treatment of minor illness.
Design A postal questionnaire survey including discrete choice experiment (DCE) of a national sample followed by telephone interviews with respondent volunteers.
Setting and participants A large random sample of the population of Scotland from a range of general practices including traditional and extended practice nursing roles was invited to participate.
Main outcome measures Patient satisfaction with, opinion of and preference for practice nurse (PN) vs. doctor consultation in primary care in relation to gender, age, education and income.
Results Questionnaire response rate was 49% (1343 of 2740). Women, younger people, the less well‐educated and those with higher income had a more positive attitude towards the PN. Older people had a more positive attitude to the doctor. Results from the DCE indicated that whilst most respondents would prefer a doctor consultation, many would be happy to consult with a nurse if other aspects of the consultation were improved.
Forty‐eight people were interviewed. The main perceived differences between doctors and nurses were academic ability and qualifications. Most respondents thought nurses could deal with relatively minor problems and should be able to prescribe some drugs.
Conclusion Patients would always want their choice of health professional to be available at first contact. However, this study suggests that, in primary health‐care practices, if nurses take on more roles previously the preserve of doctors, patients would accept them, particularly if patients receive information on nurses’ capabilities.
Keywords: discrete choice experiment, extended role, patient opinion, patient satisfaction, practice nurse, primary health care
Introduction
This study was designed to investigate patients’ and prospective patients’ attitudes to, perceptions of and preference for changes in the delivery of primary health care, with particular reference to an extended role for practice nurses (PN – nurses working in primary health‐care practice centres). The study examined the views of a large number of people using a number of methodologies to increase validity and reliability.
Background and literature search
Since the development of nurse practitioners’ roles in North America in the 1960s, PNs working in health centres have considerably increased in Canada, the United States of America, the United Kingdom and more recently Australia. Specifically in the UK, research has shown that experienced PNs are willing and able to perform much work previously carried out by general practice doctors in primary care surgeries (GPs) and that patients consult with PNs directly in some circumstances. 1 Fundholding, 2 a system in which GP practices held their own budgets, created new opportunities for nurses within the primary care team. Policy changes 3 led to increased workload for GPs and resultant delegation within the team. The new General Medical Services (GMS) contract, 4 with its range of targets, and the impact of the European Working Time Directive 5 appear to be encouraging this further, with nurses increasingly being the first point of contact in out‐of‐hours care and chronic disease management. 6 The NHS plan 7 envisages patient‐centred health care. Historically, Scottish PNs have not required specific post‐registration training or qualification but many have wide experience and hold a variety of specialist qualifications. 1 Development of the nursing workforce has led to increased responsibility for patients with chronic diseases, such as asthma, hypertension and diabetes. 8 Extended nursing roles included in this study have already been implemented in local areas, and benefits to patients and health care have been demonstrated, such as with nurse‐led care for cardiovascular patients 9 , 10 and management of minor illness. 11
Increasingly in developed countries, PNs and nurse practitioners are being measured against the GP for patient outcome and satisfaction with favourable results. 12 , 13 , 14 , 15 Many of the studies, however, are local with small participant numbers. It is not known whether these extended roles are acceptable to patients. Additionally, there is a paucity of information about patient opinion and preference, despite increasing emphasis, in the UK in particular, on public and user involvement in decision‐making. Several studies have looked at patient opinion in relation to hospital or community care 16 , 17 and health professionals’ (HP) opinions on how patients perceive nurses. 18 , 19 Reveley 20 looked at patient satisfaction with nurse triage and although Hegney et al. 21 looked at patient expectation, no studies have been found which specifically investigate patient views on the extended role of the PN.
Methods
The aim of the study was to assess, in a sample of general practices in Scotland, whether patients find the treatment of minor illness by PNs, and the concept of PN consultation as a first‐line contact, acceptable. A cross‐sectional, postal, quantitative questionnaire survey of a sample representative of the general practice patient population of Scotland was conducted. A target of 3000 participants was sought. Given the number and small list size of some of the practices, this was sufficient to assess the population parameter to within 5% and to satisfy subgroup analysis.
Quantitative study
Preliminary focus groups were used to identify factors important to patients when consulting at their general practice. This, along with the literature review, informed the questionnaire design. The questionnaire collected information on experience of surgery visit, demographic details, satisfaction with the last appointment and how this varied according to whether doctor or nurse‐led, attitudes and perceptions towards doctor vs. nurse‐led care, and preferences for doctor vs. nurse‐led care. A pilot study was conducted with 50 people not included in the main sample.
Satisfaction with last appointment
Based on a validated patient satisfaction instrument, 22 respondents were asked to rate their satisfaction with their last surgery appointment overall and for specific aspects on a five‐point Likert scale of 1–5 (excellent, very good, fair, poor, very poor). Eight questions were taken from Davies and Ware 22 – four related to time (waiting time for appointment, getting through to surgery by phone, time waited at surgery, time spent in consultation), three to the consultation (explanation, technical skills of HP, personal manner of HP) and one to the overall visit. Two additional questions relating to continuity and suitability of the professional were also added.
Attitudes and perceptions
Statements were included to investigate attitudes towards, and perceptions of, doctors and nurses. These statements were developed through focus groups conducted with 30 patients from three town practices and one rural practice from different Scottish locations, and analysis of the views expressed. Each statement was rated on a five‐point Likert scale (strongly agree [5], agree [4], not sure [3], mostly disagree [2] and strongly disagree [1]).
Preferences
A discrete choice experiment (DCE) was used to elicit preferences. This technique is increasingly used in health service research, and allows estimation of the relative importance of different attributes in the provision of health care, and how individuals trade between these attributes, and quantifies benefit scores for different configurations of service delivery. 23 Of particular interest was the importance to patients of the HP they see in the practice (doctor or nurse) relative to other characteristics of the consultation, and how they trade between these characteristics. The attributes and levels included in the DCE, defined following discussions between the members of the research team and from the focus groups, together with labels and coding for analysis are shown in Table 1. These attributes and levels gave rise to 192 (22*42*31) configurations of consultations. Using computer software, the number of choices presented to respondents was reduced to 8, which were randomly divided into three questionnaires such that each questionnaire had four choices from the fractional factorial design (for more on the experimental design, see Caldow et al. 24 ).
Table 1.
Attributes and levels in the discrete choice experiment
| Attribute | Levels of each attribute |
|---|---|
| Who you see (SEE) | A doctor |
| A practice nurse | |
| Waiting time till appointment (WAIT) | No waiting time |
| 2 days | |
| 4 days | |
| 8 days | |
| Length of consultation (LENGTH) | 5 min |
| 10 min | |
| 20 min | |
| 30 min | |
| Continuity of health professional (CONT) | Yes |
| No | |
| Likelihood of having illness cured (CURE) | 75% |
| 80% | |
| 85% |
Respondents were asked to imagine they had been ‘feeling slightly chesty with an irritating cough for 2 weeks. You are still able to do all the things you usually do, but notice that you are a little out of breath when exerting yourself. For the past three or four mornings you have coughed up a little phlegm and you decide to ask for an appointment at your practice’. Respondents were then told that their consultation could vary according to the attributes described in Table 1. For each choice, respondents were asked to choose between two alternative consultations, or neither (to allow for the fact that some respondents might choose not to attend an appointment for the minor condition described).
Rationality of responses was assessed by including additional dominant options (options that were superior on all levels of attributes and therefore would be expected to be chosen). Superiority of some levels was difficult to assume in advance. For example, a doctor may not always be preferred to a nurse, and longer consultations not always preferred to shorter ones. Given this, these attribute levels were the same in dominance tests.
To assess ease of completion, respondents rated their difficultly of completing the questionnaire on a scale from 1 (very easy) to 5 (very difficult).
Qualitative study
A final question in the postal questionnaire asked respondents if they would be willing to be interviewed by telephone. The purpose of the interviews was to explore, in depth, important issues related to consulting with a GP or PN, beliefs about similarities and differences between doctors and nurses, and reasons for visiting a doctor or nurse. The aim here was to provide more insight into the results related to the opinion and preference components of the survey. We wanted to explore the views of people with positive and negative attitudes to, and perceptions of, the PN having an extended role. Respondents willing to be interviewed were therefore categorized according to their questionnaire score on this. All were contacted by telephone, their willingness to participate confirmed, and permission sought to tape‐record the interview.
Sample
The sampling frame was a list of 433 general practices that had responded to a survey assessing PN roles in Scottish general practices which had a practice response rate of 86% and a PN response rate of 96% and has been published previously. 1 Practices were scored and ranked according to the degree of extended nursing role of their PN(s). The 20 most and 20 least extended practices according to the criteria used (cervical smear, contraception advice, counselling, ear syringing, electrocardiogram, high vaginal swab, suturing and travel immunizations performed by PN) were invited to participate. Practices ranged in size from <1500 patients to >15 000 patients and included rural and urban locations. From each practice, a random sample of registered patients over 18 years of age, proportional to the practice list size, was generated (n = 3123) using the Statistical Package for Social Sciences (spss). 25 Patients suffering from terminal illness, recent bereavement, mental incapacity or other reasons identified by the GP were excluded.
Fifty‐six respondents, 28 with a negative attitude/perception score (<42) and 28 with a positive attitude/perception score (selected randomly from 46 respondents with scores >76 of a possible 96) were chosen for interview.
Data collection
Quantitative data were collected by postal questionnaire. Information was provided in a letter accompanying the questionnaire, and return of the questionnaire was taken as implying consent. Questionnaires were coded to ensure anonymity. Names and addresses were stored separately in a secure database only accessible by the researcher to preserve confidentiality. Two reminders were sent at 3 and 6 weeks, respectively.
Interviews were carried out by telephone, up to 8 months after questionnaire completion, using a semi‐structured schedule developed from the questionnaire responses. All telephone interviews were taped and transcribed verbatim. Tapes and transcripts were coded for anonymity and stored securely as described above.
Validity and reliability
Test–retest reliability was measured after the focus groups by asking the 46 participants invited, to complete the questionnaire twice, 3 weeks apart.
Validity and internal consistency of the opinion questions was assessed by factor analysis. Similar themed questions were grouped together and scales created with particular themes of items. Scores were derived for each of the subscales. Cronbach's alpha was calculated to measure internal consistency of the questions that made up each of the five scales (see relevant table). Although there is no well‐documented reference value denoting significant consistency, values close to 1 denote some redundancy in the scale.
The Kappa‐statistic and a measure of absolute reliability were calculated to determine the intra‐subject agreement of each of the 24 questions. 26
Ethics
The study received ethical approval from the Multi‐Centre Research Ethics Committee for Scotland and 14 relevant Local Research Ethics Committees. Issues of informed voluntary consent and confidentiality were addressed as described above.
Data analysis
All missing values were excluded from the analyses and denominators revised. Questionnaire data were analysed using spss. 25
-
1
Satisfaction with last appointment: Chi‐squared or Fisher's exact tests (for small numbers) were used to examine associations between patient satisfaction and gender, age groups, income levels and educational categories. Satisfaction according to whether the last appointment was with a PN or GP was also considered. Numbers seeing the PN at their last surgery visit were small, so for age group, education and income, categories were collapsed into just two categories. This enabled valid chi‐squared tests to be performed. Age categories thus represented younger and older people (≤45 years; >45 years), education was reported as either school education only or further education, and income as ≤£20 000 and >£20 000.
-
2
Attitudes and perceptions: t‐tests were performed to compare the mean score of the subscales of the patient attitudes and perceptions between gender, age group, income level and education categories (as defined above).
-
3
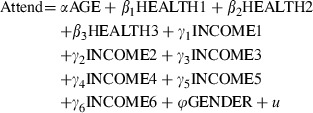
Preferences: The format of the DCE implies that the decision‐making process involves both deciding whether or not to attend the surgery (i.e. whether, or not, to choose the ‘neither’ option), as well as which consultation to choose (e.g. Consultation A or Consultation B). The variables used to explain both these factors are shown in Table 2 alongside the a priori hypotheses (where applicable). To allow for closer substitutability between the consultation alternatives than the attend alternative, the nested logit model was used to analyse the data. The following functions were estimated:
Table 2.
Variables included in the discrete choice experiment nested logit regression models
| Variable | Definition | A priori hypothesis |
|---|---|---|
| Decision of non‐attendance (neither) | ||
| AGE | Continuous | − |
| HEALTHi (i = 1, 2, 3) | Categorical variables; reference level = fair–poor health, i = 1 (good health), i = 2 = good–very good health, i = 3 = excellent health | + |
| INCOMEj (j = 1, 2, 3, 4, 5, 6) | Categorical variables; reference level = <£10 000, j = 1 = £10 000–£14 999; j = 2 = £15 000–£19 999; j = 3 = £20 000–£24 999; j = 4 = £25 000–£34 999; j = 5 = £35 000–£54 999; j = 6 = >£55 000 | No a priori hypothesis |
| GENDER | Discrete. 0 = female; 1 = male | No a priori hypothesis |
| Utility function attributes – basic model | ||
| SEE | Difference in staff seen at appointment (0 = doctor and 1 = nurse was initial coding before difference taken) | No a priori hypothesis |
| WAIT | Difference in waiting time till appointment | − |
| LENGTH | Difference in length of consultation | + |
| CONT | Difference in continuity of health professional | + |
| CURE | Difference in likelihood of having illness cured | + |
| Utility function attributes – segmented model1‘Who you see’ weighted by*: | ||
| SEE_AGE | AGE (continuous)* | − |
| SEE_EXROLE1 | EXROLE1 = 1 if practice has extended role; 0 otherwise* | +2 |
| SEE_EXROLE0 | EXROLE0 = 1 if practice has not extended role; 0 otherwise* | −2 |
| SEE_ATTDOC | ATTDOC = score (6–20). Positive attitude for doctor* | − |
| SEE_ATTNUR | ATTNUR = score (3–15). Positive attitude for nurse* | + |
| SEE_PERMED | PERMED = score (3–15). Nurse's capability of medical consultation* | + |
| SEE_PERHIS | PERHIS = score (2–10). Nurse's knowledge of medical history* | + |
 |
(1) |
and the choice between Consultations A and B is defined by:
| ( (2),) |
where Attend is whether or not a ‘neither’ option was answered (1 represents neither, and 0 not choosing ‘neither’), V is the utility from a defined consultation, α, β i (i = 1, 2, 3), γ j (j = 1, 2, 3, 4, 5, 6), ϕ and δ k (k = 1, 2, 3, 4, 5) are the parameters (coefficients) of the model to be estimated, e and u are the unobservable error terms and all other variables are as defined in Table 2.
Equation 2 was used to estimate:
-
1
the relative importance of professional seen, waiting time until appointment, length of consultation, continuity of care and percentage chance of cure. This is shown by the size of the estimated coefficients. It is important to remember the unit of measurement;
-
2
the rate at which individuals trade between these attributes, i.e. how much of one attribute they are willing to give up for improvements in other attributes. This is shown by the ratio of the coefficients in the regression equation, e.g. δ 1/δ 2 shows how much extra waiting time individuals are willing to accept to see their preferred professional and
-
3
a benefit or utility score for changes in the way the consultation is provided.
This equation was also used to assess the theoretical validity of the DCE. A priori we would expect respondents to prefer a lower waiting time, resulting in this coefficient having a negative sign. Length of consultation, continuity of care and likelihood of cure are expected to have positive signs. No a priori assumptions were made about preferences for doctor or nurse.
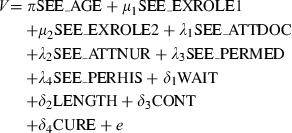
Segmentation analysis was carried out to establish what factors influenced preferences for staff seen. This also allowed theoretical validity of the DCE to be investigated. The following equation was estimated:
 |
(3) |
ATTDOC, ATTNUR, PERMED and PERHIS represent scales derived from factor analysis of attitudes and opinion questions (see above). All four are continuous scores: the higher the score, the more positive the attitude/perception. A priori hypotheses concerning these attributes are stated in Table 2.
Qualitative data were analysed by an iterative process using a content analysis framework devised for the purpose, which enabled the data to be descriptively and theoretically categorized according to themes identified in the quantitative analysis. 27
Results
Questionnaire study
Twenty‐two practices (55%; 11 high scoring and 11 low scoring for extended PN roles) agreed to participate and provided patient lists for selection of the random patient sample. A sample of 3123 patients were selected to allow for some patients being unsuitable to approach. General practitioners excluded 174 patients, leaving a sample size of 2949. A total of 1886 questionnaires were returned (1343 completed, 334 blank and 209 ‘unknown at address’) giving an adjusted response rate of 49% (1343 of 2740). Of those who completed the question, 41% (535 of 1308) were male and 59% (773 of 1308) were female. Most respondents (88%; 1134 of 1293) had visited their general practice at least once in the previous year. Over half (61%) (813 of 1343) reported they had attended the PN for themselves and 9% (126 of 1343) for someone else during the previous year.
Table 3 shows demographic data for the survey population. There was no significant difference for gender (P = 0.93), age (P = 0.40), education (P = 0.20), income (P = 0.66) or health status (P = 0.64) between patients attending practices with an extended role PN(s) and those with traditional role PN(s).
Table 3.
Demographic data for the whole sample (n = 43)
| n (%) | Total (n) | |
|---|---|---|
| Practice location | ||
| City | 835 (62) | 1341 |
| Town/large town | 450 (34) | |
| Rural | 56 (4) | |
| Practice nursing role | ||
| Extended | 780 (58) | 1341 |
| Traditional | 561 (42) | |
| Health professional visited in last year | ||
| Doctor | 1101 (85) | 1292 |
| Practice nurse | 142 (11) | |
| Doctor and nurse | 31 (2.4) | |
| Other (e.g. physiotherapist) | 18 (1.5) | |
| Self‐reported health status | ||
| Excellent | 569 (44) | 1304 |
| Good | 434 (33) | |
| Fair or poor | 301 (23) | |
| Gender | ||
| Male | 535 (41) | 1308 |
| Female | 773 (59) | |
| Age (years) | ||
| 16–44 | 530 (41) | 1289 |
| 45–64 | 472 (37) | |
| 65–74 | 190 (15) | |
| 75+ | 97 (7) | |
| Education | ||
| School leaving 15/16 | 350 (31) | 1131 |
| O/H/A grades | 273 (24) | |
| Further education | 292 (26) | |
| Degree/higher education | 216 (19) | |
| Income (£; per annum) | ||
| <10 000 | 369 (32) | 1153 |
| 10 000–19 999 | 370 (32) | |
| 20 000–34 999 | 279 (24) | |
| >35 000 | 135 (12) | |
Satisfaction with appointment
Respondent satisfaction with the last visit is shown in Table 4. The categories ‘excellent’ and ‘very good’, and ‘fair’, ‘poor’ and ‘very poor’ are combined to give a dichotomous variable because of low numbers in the extremes of excellent and poor/very poor. Women who visited a GP were significantly less satisfied with the time spent at the surgery compared with women who saw a PN (P ≤ 0.05). Similarly, younger people and those who had a lower level of education were also significantly less satisfied with the time spent if they had seen a GP compared with a PN (P ≤ 0.05). Finally, among respondents in the higher income bracket, those who saw a PN were significantly more satisfied with the time spent compared to those who saw a GP (P ≤ 0.01). There was no significant difference in patient satisfaction between practices with an extended nursing role and those with a traditional nursing role, with one exception: patient satisfaction with time spent at the surgery, including arranging the appointment, was significantly better when visiting the PN (56%) compared with the GP (45%) in practices where the PN had an extended role (P ≤ 0.05).
Table 4.
Numbers (and percentages) of responders’ satisfaction with last surgery visit (doctor vs. nurse)
| Question (ex/vg) | Gender, n (%) | Age [years; n (%)] | Education, n (%) | Income [per annum, n (%)] | ||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | <45 | ≥45 | School | Further | <£20 000 | ≥£20 000 | |
| Visit doctor overall (n = 1065) | 360 (81) | 483 (78) | 301 (69) | 533 (86) | 419 (82) | 307 (75) | 488 (80) | 251* (76) |
| Visit nurse overall (n = 146) | 44 (86) | 77 (81) | 45 (76) | (73) 88 | 61 (90) | 48 (76) | 61 (80) | 48 (89) |
| Time spent visit doctor (n = 1016) | 190 (45) | 248* (42) | 128* (31) | 306 (52) | 233* (45) | 152 (39) | 270 (47) | 112** (35) |
| Time spent visit nurse (n = 125) | 24 (55) | 44 (54) | 22 (47) | 44 (58) | 36 (61) | 23 (44) | 33 (52) | 27 (55) |
| Consultation doctor (n = 1036) | 341 (77) | 443 (75) | 294 (68) | 484 (82) | 381 (77) | 302 (75) | 458 (78) | 231 (71) |
| Consultation nurse (n = 140) | 41 (82) | 71 (79) | 42 (71) | 68 (86) | 57 (85) | 44 (75) | 56 (78) | 45 (83) |
| Suitability of seeing doctor (n = 1025) | 347 (84) | 513 (84) | 334 (78) | (89) 544 | 431 (85) | 431 (84) | 503 (83) | 280 (85) |
| Suitability of seeing nurse (n = 144) | 46 (90) | 81 (87) | 51 (88) | 73 (89) | 62 (91) | 52 (87) | 64 (84) | 51 (94) |
| Continuity care doctor (n = 1029) | 346 (80) | 445 (75) | 286 (68) | 495 (83) | 398 (80) | 281 (72) | 468 (79) | 224 (71) |
| Continuity care nurse (n = 126) | 38 (86) | 61 (74) | 37 (79) | 59 (79) | 49 (82) | 37 (74) | 53 (79) | 37 (79) |
*P ≤ 0.05; **P ≤ 0.01.
P‐values based on chi‐square test of satisfaction with doctor vs. nurse within subgroups of gender, age, education and income.
Ex, excellent; vg, very good.
Attitudes and perceptions
Table 5 shows patient attitudes to and perceptions of GPs and PNs. A number of significant relationships were observed. Women had a significantly more positive attitude to, and perception of, PNs than did men (P ≤ 0.001). They also thought that a PN would know their family history as well as a GP would (P ≤ 0.05). Older people had a more positive attitude to, and perception of, the GP whereas younger people had a more positive attitude to, and perception of, the PN (both P ≤ 0.001). Younger people also perceived the PN as knowing their family history as well as a GP would (P ≤ 0.001). Less well‐educated people had a more positive attitude to (P ≤ 0.001), and perception of, the GP (P ≤ 0.01). However, that same group perceived a PN would know their medical condition as well as a GP would (P ≤ 0.001). Those with a lower income had a more positive attitude to the GP (P ≤ 0.001). Patients with a lower income registered with extended role practices had a more significant positive perception of the GP (P ≤ 0.001), although patients in both traditional and extended role practices perceived that the PN knew their medical condition. Patients with a higher income perceived that the PN knows their history.
Table 5.
Patient attitudes and perceptions
| Gender | Age (years) | Education | Income (per annum) | |||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | <45 | ≥45 | School | Further | <£20 000 | ≥£20 000 | |
| Extended role practices | ||||||||
| Attitude positive for doctor | 15.92 (2.82) | 15.52 (2.99) | 14.43 (2.95) | 16.51 (2.60)*** | 15.92 (2.90) | 15.11 (3.01)*** | 16.00 (2.85) | 14.95 3.09)*** |
| Attitude positive for nurse | 9.42 (2.72) | 10.18 2.93)*** | 10.58 (2.70) | 9.39 (2.87)*** | 9.77 (2.90) | 10.15 (2.79) | 9.89 (2.88) | 10.12 (2.84) |
| Perception positive for nurse | 15.19 (2.66) | 15.67 (2.70)* | 15.76 (2.53) | 15.29 (2.79)* | 15.48 (2.72) | 15.43 (2.65) | 15.58 (2.69) | 15.41 (2.67) |
| Perception positive for doctor | 7.07 (1.49) | 6.99 (1.45) | 6.75 (1.32) | 7.19 (1.54)*** | 7.11 (1.46) | 6.80 (1.34)** | 7.11 (1.49) | 6.80 (1.43)* |
| Perception nurse know history | 6.49 (2.16) | 6.83 (2.13)* | 7.08 (1.99) | 6.43 (2.22)*** | 6.66 (2.23) | 6.84 (2.01) | 6.63 (2.17) | 7.00 (1.96)* |
| Perception nurse know medical condition | 6.93 (2.35) | 7.20 (2.49) | 7.27 (2.37) | 6.95 (2.48) | 7.35 (2.38) | 6.62 (2.46)*** | 7.29 (2.31) | 6.63 (2.49)*** |
| Traditional role practices | ||||||||
| Attitude positive for doctor | 15.61 (2.92) | 15.59 (2.99) | 14.71 (2.97) | 16.32 (2.76)*** | 15.84 (2.68) | 15.10 (3.30)** | 15.74 (2.84) | 15.07 (3.12)* |
| Attitude positive for nurse | 9.44 (2.68) | 9.95 (2.81)* | 10.21 (2.56) | 9.40 (2.86)*** | 9.88 (2.70) | 9.77 (2.79) | 9.72 (2.80) | 10.01 (2.60) |
| Perception positive for nurse | 14.78 (2.88) | 15.34 (2.75)* | 15.39 (2.62) | 14.94 (2.92) | 15.28 (2.73) | 14.97 (2.84) | 15.30 (2.82) | 15.05 (2.64) |
| Perception positive for doctor | 7.04 (1.54) | 6.80 (1.58) | 6.76 (1.45) | 7.02 (1.64) | 7.02 (1.53) | 6.73 (1.49)* | 6.94 (1.59) | 6.80 (1.40) |
| Perception nurse know history | 6.40 (2.14) | 6.79 (2.16)* | 6.88 (2.00) | 6.47 (2.25)* | 6.59 (2.16) | 6.81 (2.10) | 6.75 (2.07) | 6.64 (2.22) |
| Perception nurse know medical condition | 6.98 (2.32) | 7.04 (2.41) | 7.12 (2.38) | 6.97 (2.36) | 7.24 (2.33) | 6.66 ((2.42)** | 7.48 (2.23) | 6.38 (2.36)*** |
Values are expressed as mean (SD). *P ≤ 0.05; **P ≤ 0.01; ***P ≤ 0.001. P‐values based on t‐test of mean attitude/perception score between gender, age, education or income groupings.
Factor analysis on the attitude and perception questions identified seven scales (first column, Table 6). Cronbach's alpha scores were 0.45 and above. Opinion questions were shown to have good reliability as illustrated by the Kappa‐statistic. Eleven questions had a κ > 0.4 (range: 0.4–0.7). The mean absolute reliability for the remaining 13 questions was very good at 0.84 (range: 0.69–1.0).
Table 6.
Opinion question subscales after factor analyses and reliability of questions in each scale
| Scales | Questions | Variance explained by subscale (%) | Chronbach's alpha | Total score (SD) |
|---|---|---|---|---|
| Attitude positive doctor1 | If I saw the practice nurse I would want the doctor to be in overall charge Important to see doctor for reassurance I would like to make the decision about whether I consult with a doctor or practice nurse Would not like to see practice nurse first under any circumstances | 28.1 | 0.62 | 1277 (2.93) |
| Attitude positive nurse1 | Nurses should be able to give prescriptions for common medications Like to consult a practice nurse instead of a doctor in certain circumstances Don't mind seeing a practice nurse first | 24.1 | 0.61 | 1289 (2.83) |
| Perception positive nurse | Practice nurse able to decide if I needed a doctor's appointment Practice nurse able to reassure Practice nurse able to judge own limitations Practice nurse suitably trained to consult for some medical conditions | 18.6 | 0.73 | 1292 (2.75) |
| History1 | I think a practice nurse could know my family history as well as a doctor I think a practice nurse could know my medical history as well as a doctor | 14.2 | 0.82 | 1297 (2.16) |
| Medical conditions1 | Practice nurses are suitably trained to be able to consult with patients for all medical conditions Reverse – practice nurses are not suitable trained I think nurses know more than doctors | 13.3 | 0.62 | 1281 (2.41) |
| Perception positive doctor | Seeing the practice nurse would be second best Practice nurse would not be able to decide if I needed a doctor's appointment | 11.0 | 0.47 | 1287 (1.51) |
| Confidentiality | Believe that a consultation with the doctor is confidential Believe a consultation with a practice nurse is confidential | 10.5 | 0.45 | 1323 (1.10) |
1Variables included in the discrete choice experiment (DCE) analysis.
Preferences
The mean difficulty score was 2.25. Almost all (98%) respondents satisfied the dominance tests. The results from the DCE regression model are shown in Table 7. Only significant variables were included. Respondents with income level between £10 000 and £14 999 and between £25 000 and £34 999 were less likely to attend the practice than respondents in any other income group. The attributes of the utility function were all well‐defined and significant at the 1% level and suggest that:
Table 7.
Results from the nested logit regression model – basic model
| Variable | Coefficient | Lower | Upper | P‐value |
|---|---|---|---|---|
| Decision of non‐attendance (neither) | ||||
| INCOME0 (reference level: <£10 000) | – | – | – | – |
| INCOME1 (γ 1) (£10 000–£14 999) | 0.566 | 0.28 | 0.83 | ≤0.001* |
| INCOME2 (γ 2) (£15 000–£19 999) | 0.23 | −0.08 | 0.54 | 0.15 |
| INCOME3 (γ 3) (£20 000–£24 999) | 0.207 | −0.1066 | 0.52 | 0.21 |
| INCOME4 (γ 4) (£25 000–£34 999) | 0.37 | 0.05 | 0.68 | 0.02** |
| INCOME5 (γ 5) (£35 000–£54 999) | −0.095 | −0.51 | 0.3166 | 0.65 |
| INCOME6 (γ 6) (>£55 000) | 0.218 | −0.33 | 0.75 | 0.43 |
| Utility function attributes | ||||
| SEE (δ 1) (doctor = 0; nurse = 1) | −1.13 | −1.21 | −1.04 | ≤0.001* |
| WAIT (δ 2) (days) | −0.27 | −0.28 | −0.25 | ≤0.001* |
| LENGTH (δ 3) (min) | 0.010 | 0.0051 | 0.015 | ≤0.001* |
| CONT (δ 4) (yes = 1; no = 0) | 0.79 | 0.682 | 0.897 | ≤0.001* |
| CURE (δ 5) (%) | 0.088 | 0.866 | 0.893 | ≤0.001* |
| Number of observations | 12033 | |||
| McFadden R 2 | 0.4207 | |||
| Chi‐squared | 4384.6 | |||
| P‐value | 0.001 | |||
*P ≤ 0.01 **P ≤ 0.05
-
1
being seen by a doctor results in higher benefit than being seen by a nurse, i.e. a general preference for seeing a doctor;
-
2
the longer the waiting time for an appointment, the lower the benefit;
-
3
longer consultations were preferred to shorter ones;
-
4
patients preferred to be seen by the same professional and
-
5
the greater the likelihood of having the illness cured, the higher the utility.
The most important attribute was the professional seen (with GP preferred to PN), followed by continuity of the professional seen. Waiting time was the next most important factor followed by the likelihood of having the illness cured and the length of the consultation. However, it must be noted that such importance relates to a unit measure. That is, being seen by a doctor rather than a nurse was more important than a unit change in any other attribute, e.g. more important than a 1 day reduction in waiting time, 1 min increase in length of consultation, or 1% change in chance of cure. However, whilst seeing a GP was the most important attribute, patients might prefer to see a PN if they were ‘compensated’ by changes in the level of other attributes. This can be seen by calculating what respondents were willing to give up of one attribute to get more of another. This is given by the ratio between the coefficients of those attributes.
-
•
Respondents would accept seeing a PN if the waiting time was reduced by four 4 days (−1.13/−0.27).
-
•
Respondents would be willing to see a PN if their chances of having the illness cured increased by 13% (−1.13/0.088).
This can also be shown by calculating the utility score of moving from a hypothetical consultation with a GP to a hypothetical consultation with a PN. Table 8 shows that a positive benefit (0.89) is derived from moving from a consultation with a GP to one with a PN if such change is compensated by improvements in the other attributes. In the hypothetical case presented below, patients obtain higher utility if they see a PN instead of a GP when their waiting time is reduced from 4 days to the same day, the length of consultation is increased from 5 to 20 min and they see the same PN rather than an unknown GP.
Table 8.
Utility score of moving from a hypothetical consultation with a doctor to a nurse
| Attribute | Coefficient (C) | Consultation with doctor | Consultation with nurse | Difference in attribute levels (D) | Attribute score (C × D) |
|---|---|---|---|---|---|
| SEE | −1.13 | 1 | 2 | 1 | −1.13 |
| WAIT | −0.27 | 4 | 0 | −4 | 1.08 |
| LENGTH | 0.01 | 5 | 20 | 15 | 0.15 |
| CONT | 0.79 | 0 | 1 | 1 | 0.79 |
| CURE | 0.088 | 0.75 | 0.75 | 0 | 0 |
| Utility score | 0.89 |
The results from the segmented model are shown in Table 9. Again, only significant variables are presented. Patients’ age had a significant effect on non‐attending the practice, i.e. older respondents were more likely to attend the practice. Self‐reported health status was also significant. This implies that (given the negative sign) respondents in good or very good health were more likely to attend the practice than those in fair or poor health. Those respondents with income level £10 000–£14 999 were more likely not to attend the practice than respondents in any other income group.
Table 9.
Results from the regression model – segmented model
| Variable | Coefficient | Lower | Upper | P‐value |
|---|---|---|---|---|
| Decision of non‐attendance (neither) | ||||
| AGE (α) | −0.053 | −0.063 | −0.042 | 0.001* |
| HEALTH0 (reference level: fair–poor) | – | – | – | – |
| HEALTH1 (β 1) (good health) | −0.14 | −0.45 | 0.17 | 0.35 |
| HEALTH2 (β 2) (good–very good health) | −0.35 | −0.66 | −0.036 | 0.03* |
| HEALTH3 (β 3) (excellent health) | −0.18 | −0.59 | 0.23 | 0.38 |
| INCOME0 (reference level: <£10 000) | – | – | – | – |
| INCOME1 (γ 1) (£10 000–£14 999) | 0.47 | 0.15 | 0.78 | 0.005* |
| INCOME2 (γ 2) (£15 000–£19 999) | 0.18 | −0.19 | 0.55 | 0.32 |
| INCOME3 (γ 3) (£20 000–£24 999) | −0.022 | −0.39 | 0.35 | 0.912 |
| INCOME4 (γ 4) (£25 000–£34 999) | 0.29 | −0.08 | 0.66 | 0.131 |
| INCOME5 (γ 5) (£35 000–£54 999) | −0.30 | −0.79 | 0.19 | 0.224 |
| INCOME6 (γ 6) (>£55 000) | 0.098 | −0.50 | 0.70 | 0.756 |
| Utility function attributes | ||||
| SEE_AGE (π) | −0.023 | −0.028 | −0.017 | 0.001* |
| SEE_EXROLE1 (μ 1) | −0.85 | −1.35 | −0.34 | 0.01* |
| SEE_EXROLE0 (μ 2) | −0.92 | −1.42 | −0.41 | 0.001* |
| SEE_ATTDOC (λ 1) | −0.033 | −0.05 | −0.01 | 0.001* |
| SEE_ATTNUR (λ 2) | 0.085 | 0.06 | 0.106 | 0.001* |
| SEE_PERMED (λ 3) | 0.050 | 0.026 | 0.07 | 0.001* |
| WAIT (days) (δ 1) | −0.32 | −0.345 | −0.29 | 0.001* |
| LENGTH (min) (δ 2) | 0.013 | 0.007 | 0.018 | 0.001* |
| CONT (yes = 1; no = 0) (δ 3) | 0.92 | 0.79 | 1.04 | 0.001* |
| CURE (%) (δ 4) | 0.068 | 0.049 | 0.086 | 0.001* |
| Number of observations | 9975 | |||
| McFadden R 2 | 0.4625 | |||
| Chi‐squared | 4006 | |||
| P‐value | <0.001 | |||
*P ≤ 0.05
The segmentation of the ‘who you see’ attribute shows that older patients were less likely to prefer being seen by a PN. No significant differences were found between respondents who visited a practice with an extended role PN and those where PNs had a traditional role. Segmentation according to the ‘attitude’ scores shows that respondents with a more positive attitude for the GP were less likely to prefer seeing a PN. Similarly, respondents who had a positive attitude for the PN were more likely to prefer seeing a PN. Respondents who perceived that PNs have capability for medical consultation were more likely to prefer being seen by a PN. Respondents’ perception of the PN's knowledge of the patients’ history was not significant.
Telephone interviews
Sixteen men and 32 women with an age ranging from 18 to 73 years were interviewed. Nine major themes emerged relating to the professional and process aspects of the consultation: perceived expertise, academic ability, qualifications, respect, approachability, understanding, nature of the illness, prescribing and waiting time. Quotes from the interviews are shown in Table 10. The most important factors to patients when visiting the surgery were to like and feel confident with the person they consulted with and to have the problem addressed with reassurance or diagnosis and/or treatment given. There was a general willingness to wait to see the doctor of their choice. Negative issues were the length of waiting time and the ‘receptionist barrier’. Generally, it was felt that GPs and PNs should be kind, understanding, trustworthy and respect confidentiality. The main perceived differences between doctors and nurses were academic ability and qualifications. Many people thought that if nurse training were longer and more in‐depth, then nurses would be as able to deal with medical problems as well as doctors. Differences between respect for doctors and nurses were also highlighted.
Table 10.
Perceptions of doctors and nurses from the in‐depth interviews
| Descriptor | Doctor related | Nurse related |
|---|---|---|
| Perceived expertise | ‘I'm not running them (nurses) down or anything, they're good at their job, but the doctor is in charge and he says what's what’ (Int 4, male, age 65) | ‘…I mean a nurse takes medicine to a certain level and doctors are further … (it's) just … my confidence in them’ (Int 24, female, age 53) |
| Approachability | ‘He's (the doctor), he's more likely to tell you, you know … rather than some kind of interaction between you’ (Int 31, male, age 43) | ‘I find the practice nurse more approachable than the doctor … puts your mind at rest very easily … make you feel a wee bit more comfortable. I'm not saying they're not as professional (as doctors), I don't mean that at all’ (Int 20, female, age 28) |
| Nature of illness | ‘…if it was something, you know, quite serious, they (the doctor) would know’ (Int 26, female, age 21) | ‘I think, probably, that a nurse could make simple diagnoses (common colds, coughs, headaches…) as well … probably more effectively as well, you know take some of the … (pressure off the doctor)’ ‘I have no objection to nurses being in charge of their patients and whatever condition I had, if the nurse was the most appropriate person for me, I would be quite happy’ (Int 12, male, age 51) |
| Qualifications | …I mean a doctor is more qualified (Int 39, male, age 72) | ‘I don't think the nurse would have the qualifications to diagnose problems … but in saying that, a practice nurse with experience could maybe know more than a doctor’ (Int 39, male, age 72) |
| Respect | ‘…they just seem to have a different standing – doctors from nurses’ (Int 35, female, age 61) | ‘they (nurses) would still be seen as slightly inferior to doctors…’ (Int 15, female, age 27) |
| Academic ability | ‘As I say, a doctor's got to be really clever … a nurse – I'm no’ saying that they don't need to be clever, but…’ (Int 47, female, age 53) | ‘…if a nurse has had university further training, I'm sure she could be every bit as good as a doctor (Int 24, female, age 53) |
| Understanding | ‘…not all doctors and surgeons take time to be with or to understand how the patient feels about the situation that they are in’ (Int 8, male, age 44) | ‘if it's a female problem you're along with, you know, the nurse is kind of much more understanding of how you might be feeling about things’ (Int 21, female, age 48) |
| Waiting time | ‘Generally, it's the time involved. When you see the doctor in particular, you're generally hanging about for a while’ (Int 31, male, age 43) | ‘I would definitely be prepared to see a nurse if it meant seeing someone more promptly’ (Int 8, male, age 44) |
| Prescribing | ‘…if it's a case of well maybe the flu then they (nurses) should be able to prescribe maybe antibiotics or inhalers for asthma, things like that, … especially when the patients repeat prescriptions, where it's something simple that they could take the load off the doctors hands by taking care of them’ (Int 11, female, age 19) |
Doctors were seen to diagnose and were perceived to be competent, confident, reassuring and more searching in their questioning. Most people thought they should be in overall charge. The negative aspects of consulting a GP were that doctors were busy, lacked time, could appear uninterested and were not always easily available.
Interviewees thought that nurses were easier to see and were approachable; they listened, understood, and were interested and more involved with the patient. They gave holistic advice and care. Most interviewees thought PNs could deal with what they thought was a relatively minor problem, and that PNs should be able to prescribe some drugs. It was generally thought that PNs were limited in what they could do, but would recognize their limitations and seek advice or refer patients to a GP if necessary. Several interviewees expressed concern that a PN may ‘miss something’ if she/he were allowed to diagnose. The majority thought that although PNs were ‘not their own boss’, they could have their own patients.
The nature of the illness would be the deciding factor for many patients as to which HP they would consider consulting. Most people, however, wanted to be seen initially by a GP and would certainly want to see a GP for what they thought was a major problem or for an unknown or new problem. Several interviewees, however, would be happy to consult with a PN for any problem.
If they felt their problem was minor, many interviewees said they would self‐medicate, ask a pharmacist or ‘wait and see’. About half would favour a screening system where they would be seen by the PN first, although most people interviewed were unsure of what PNs could do beyond their own experience of the PN.
Discussion
This was a large study representing patient views from general practices throughout Scotland. The full range of age groups, educational background and income was well represented in views from frequent, occasional and non‐attenders at general practices. Practices were well represented in size, location and extended or traditional roles of PNs. The mixed design, using quantitative and qualitative methods and a DCE, was one of the strengths of the study, providing greater depth and opportunity to clarify and explore patients’ views fully. The questionnaire was found to be reliable and valid to explore attitudes and opinions, with further validation provided by interview. It is acknowledged that a higher response rate would have been better. However, although the percentage of male respondents was slightly less (41%) than national rates (48% male; 52% female), it was greater than practice attendance rates for males so there was good representation of gender. 28
It is recognized that preferences for seeing a PN or GP may be related to the perceived seriousness of the condition. Future work should include different levels of illness and examine the impact on preference and the circumstances under which different patient groups would accept PN consultation. In the DCE analysis we assumed a simple linear additive model, but future analysis could extend this to allow for non‐linearities in preferences for service attributes and the interaction with respondent characteristics.
The role for PNs in the UK has been developing rapidly, with much innovation in delivery of care. 29 Other countries, e.g. Australia, have introduced government funding for GPs to employ PNs because of the apparent success of PNs in the UK although limited scope in practice has also been reported. 21 , 30 Some, 31 have described the roles of professionals working within new configurations within the service model, and others, 32 an increasingly complex health‐care environment. Much has been written on PNs’ widening and changing role. 8 , 33 , 34
While delivery is without doubt very important, there is little published research on patients’ attitudes to the changes that are taking place, despite the apparent importance attributed to users’ opinions. Nor is there much reported information on patients’ perception of the skills and capability of those giving treatment and care, which was traditionally the role of the doctor. This study showed that many patients, especially younger patients and women, were happy to consult with PNs in many circumstances, but knowledge of what PNs could do was limited to personal experience. A significant minority, however, particularly older and more deprived patients, continued to view the doctor as having the important role as diagnostician in serious illness. Most patients would want their choice of health‐care professional to be available at first contact.
This is an important study in the context of the changing delivery of primary health care. Increasingly, roles and responsibilities of doctors and nurses are changing and some previously distinct roles are becoming blurred and can be equally undertaken by nurses. 35 In the UK, there has been a change towards specialization of skills in graduate doctors with changes in undergraduate medical teaching methods and medical students being encouraged to follow specialist training courses at an earlier stage in their professional development. Nurse training has become university‐based, encouraging independent thought and confidence in abilities, and altering nurses’ previous ‘handmaiden status’. There has also been a considerable increase in postgraduate training and development not only in the nursing profession, but also among other members of the health‐care team, such as physiotherapists and pharmacists. The gateway to primary health care, which has traditionally been through GPs, may not be sustainable in all practices in the future. There is already a shortage of GPs in the UK and this is set to increase as a result of retirement of substantial numbers in the next few years and increasing recruitment difficulties. 36 , 37
Patients are changing too, in knowledge of their own condition and knowledge of services available consequently increasing demands on primary health care. The climate is changing in relation to whether patients should consult with doctors for all consultations. Advice regarding drugs and medication interaction is now routinely given by pharmacists in the pharmacy, 38 and many patient consultations in the surgery are being undertaken by specialist nurse practitioners and, increasingly, PNs. This could expand further with increased education of the public, particularly regarding awareness of skills learned in modern nurse training programmes, which would inform on specialist skills and allow patients’ confidence in PNs to grow and develop further. However, while substitution of nurses for doctors could alleviate pressures on GPs and increase motivation for some nurses, attention will need to be given to this potential, given continuing concerns about nursing shortages. 39 The health economics of such a solution are as yet unqualified.
Conclusions
This study focuses on patient views and shows patient acceptance of an extended nursing role in primary care. It confirms previous findings that if nurses take on roles previously the preserve of doctors, patients will accept them. However, the study suggests the implementation of such changes must take patients’ opinions into account. It is our intention to repeat the study in order to identify further changes that may have taken place as extended and specialist nursing roles have continued to develop in Scotland.
Acknowledgements
The study was funded by the Chief Scientist Office, Department of Health, Scottish Executive, Edinburgh, Scotland. The authors would also like to thank Jill Mollinson and Julie Simpson for early statistical advice, Mrs Netta Clark for clerical support and data entry, participating General Practices and all participating patients without whom, this study would not have been possible.
References
- 1. Caldow JL, Bond CM, Russell EM. Independent nursing practice: a national survey of attitudes of practice employed nurses in Scotland. Health Bulletin, 2001; 59: 21–28. [PubMed] [Google Scholar]
- 2. Department of Health . General Practice in the National Health Service: The 1990 Contract. London: HMSO, 1989. [Google Scholar]
- 3. Department of Health . The Health of the Nation. London: HMSO, 1992. [Google Scholar]
- 4. Scottish Executive Health Department . Standard General Medical Services Contract. Edinburgh: Scottish Executive Health Department, 2004. [Google Scholar]
- 5. Council of the European Union . European Working Time Directive, Directive 93/104/EC. Brussels: The Council of the European Union, 1993. [Google Scholar]
- 6. Department of Health . Investing in Practice: The New General Practitioner Services Contract. London: DOH, 2003. [Google Scholar]
- 7. Department of Health . The NHS Plan: a Plan for Investment, a Plan for Reform. London: DOH, 2000. [Google Scholar]
- 8. Laurenson S. Changing roles of nurses in Scotland. A survey of developing clinical roles within NHS Trusts in Scotland. Health Bulletin, 1997; 55: 331–337. [PubMed] [Google Scholar]
- 9. Campbell NC, Ritchie LD, Thain J, Deans HG, Rawles JM, Squair JL. Secondary prevention in coronary heart disease: a randomised trial of nurse‐led clinics in primary care. Heart, 1998; 80: 447–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bjornsen KD. Health care transition in congenital heart disease: the providers point of view. Nursing Clinics of North America, 2004; 39: 715–726. [DOI] [PubMed] [Google Scholar]
- 11. Pritchard A, Kendrick D. Practice nurse and health visitor management of acute minor illness in a general practice. Journal of Advanced Nursing, 2001; 36: 556–562. [DOI] [PubMed] [Google Scholar]
- 12. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. British Medical Journal, 2002; 324: 819–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Edwards JB, Oppewal S, Logan CL. Nurse‐managed primary care: outcomes of a faculty practice network. Journal of the American Academy of Nurse Practitioners, 2003; 15: 563–569. [DOI] [PubMed] [Google Scholar]
- 14. Lenz ER, Mundinger MO, Kane RL, Hopkins SC, Lin SX. Primary outcomes in patients treated by nurse practitioners or physicians: two year follow up. Medical Care Research and Review, 2004; 61: 332–351. [DOI] [PubMed] [Google Scholar]
- 15. Laurent M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database of Systematic Reviews, 2005; 2: CD001271. [DOI] [PubMed] [Google Scholar]
- 16. Hill J. Patient satisfaction in a nurse‐led rheumatology clinic. Journal of Advanced Nursing, 1997; 25: 347–354. [DOI] [PubMed] [Google Scholar]
- 17. Wright FL, Wiles RA, Moher M. Patients and practice nurses perceptions of secondary preventative care for established ischaemic heart disease: a qualitative study. Journal of Clinical Nursing, 2001; 10: 180–188. [DOI] [PubMed] [Google Scholar]
- 18. Hegedus KS. Providers’ and consumers’ perspective of nurses’ caring behaviours. Journal of Advanced Nursing, 1999; 30: 1090–1096. [DOI] [PubMed] [Google Scholar]
- 19. McKenna H, Keeney S. Community nursing: health professionals and public perceptions. Journal of Advanced Nursing, 2004; 48: 17–25. [DOI] [PubMed] [Google Scholar]
- 20. Reveley S. The role of the triage nurse practitioner in general medical practice: an analysis of the role. Journal of Advanced Nursing, 1998; 28: 584–591. [DOI] [PubMed] [Google Scholar]
- 21. Hegney D, Price K, Patterson E, Martin‐McDonald K, Rees S. Australian consumers’ expectations for expanded nursing roles in general practice. Australian Family Physician, 2004; 33: 845–848. [PubMed] [Google Scholar]
- 22. Davies A, Ware J. Group Health Association of America Consumer Satisfaction Survey. Washington, DC: GHAA Inc., 1991. [Google Scholar]
- 23. Ryan M, Farrar S. Eliciting preferences for health care using conjoint analysis. British Medical Journal, 2000; 320: 1530–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Caldow JL, Bond CM, Ryan M et al. Treatment of Minor Illness in Primary Care: a National Survey of Patient Attitudes to a Wider Nursing Role. Edinburgh: Scottish Home and Health Department, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Innear P, Gray C . SPSS for Windows. Hove: Psychology press Ltd, 1997. [Google Scholar]
- 26. Chin S, Burney PGJ. On measuring repeatability of data from self administered questionnaires. International Journal of Epidemiology, 1987; 16: 121–127. [DOI] [PubMed] [Google Scholar]
- 27. Weber RP. Basic Content Analysis, 2nd edn. Newbury Park, CA: Sage Publications, 1990. [Google Scholar]
- 28. IDS Scotland . Scottish Health Statistics. Information and Statistics Division; NHS Scotland, 1998. [Google Scholar]
- 29. Riley AJ, Harding G, Meads G, Underwood MR, Carter YH. An evaluation of personal medical services: the times they are a changing. Journal of Professional Care, 2003; 17: 127–139. [DOI] [PubMed] [Google Scholar]
- 30. Parker JM. Patient or customer? Journal of the Royal College of Nursing Australia, 1999; 6: 16–23. [DOI] [PubMed] [Google Scholar]
- 31. Gerrish K. A pluralistic evaluation of nursing/practice development units. Journal of Clinical Nursing, 2001; 10: 109–118. [DOI] [PubMed] [Google Scholar]
- 32. Morse CJ. Advance practice nursing in heart transplantation. Progress in Cardiovascular Nursing, 2001; 16: 21–24. [DOI] [PubMed] [Google Scholar]
- 33. Brown SJ. Patient‐centered communication. Annual Review of Nursing Research, 1999; 17: 85–104. [PubMed] [Google Scholar]
- 34. Rees M, Butler C. Coughs and colds: nurse management of upper respiratory tract infection. Nursing Standard, 2001; 15: 33–35. [DOI] [PubMed] [Google Scholar]
- 35. Jones AM. Changes in practice at the nurse‐doctor interface. Using focus groups to explore the perceptions of first level nurses working in acute care. Journal of Clinical Nursing, 2003; 12: 124–131. [DOI] [PubMed] [Google Scholar]
- 36. Evans J, Lambert T, Goldacre M. GP recruitment and retention: a qualitative analysis of doctors’ comments about training for and working in general practice. Occasional Paper Royal College of General Practitioners, 2002; 83(iii–vi): 1–33. [PMC free article] [PubMed] [Google Scholar]
- 37. Sibbald B, Bojke C, Gravelle H. National survey of job satisfaction and retirement intentions among general practitioners in England. British Medical Journal, 2003; 326: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Scottish Executive . The Right Medicine: A Strategy for Pharmaceutical Care in Scotland. Edinburgh: Scottish Executive, 2002. [Google Scholar]
- 39. AACN . Nursing Shortage Resource – About the Nursing Shortage. Washington, DC: American Association of Colleges of Nursing, 2005. [Google Scholar]


