Abstract
Background There is little knowledge as to whether the chronicity of a disease affects patients’ desire for participation.
Aim To study whether participation preferences vary according to the type of disease.
Design, participants and methods Data of 1393 patients from six trials with different medical conditions (hypertension, depression, breast cancer, schizophrenia, multiple sclerosis, minor traumas) were pooled and analysed, using multiple regression analysis controlling for socio‐demographic variables.
Results Younger age, better education as well as female gender accounted for a small but statistically significantly greater desire to participate. Patients suffering from multiple sclerosis (MS) exhibited significantly higher participation preferences than the other diagnostic groups. There were no major differences between the other diagnostic groups. Age, gender, education and diagnosis explained only 14% of the variance.
Conclusions We found no clear differences between chronic and acute conditions. However, patients suffering from MS, a chronic condition, were clearly different from all other diagnostic groups. The reasons for this difference remain unclear. The predictive value of socio‐demography and type of illness is low.
Keywords: patient autonomy, patient participation, shared decision‐making
Introduction
The interest in patients’ participation preferences has risen since shared decision‐making (SDM) has been proposed as the ideal model of doctor–patient communication. 1 To date, the majority of patients can be expected to prefer a collaborative or active participation in clinical decision‐making, but in daily practice their needs are often not met by physicians. 2 What makes it important to know about individual patients’ participation preferences is the fact that an ‘optimum match’ between patients’ expectations and physicians’ communication style produces better results in terms of patients’ satisfaction and treatment adherence. 2
Research has shown that patients’ desire to participate is often located somewhere midway between the extremes of taking over control of all decisions and leaving it all up to the doctor, 3 , 4 , 5 but there also exist patients with extremely strong or mild preferences. 2
Among the most frequently reported predictors for strong participation preferences are younger age, female gender and higher education. 6 Furthermore, it is hypothesized that the wish to participate in treatment decisions is influenced by the impact of these decisions. Thus, it is theoretically suggested that in the case of decisions which have substantial impact on health outcomes (‘major decisions’) patients should show stronger participation preferences. 7 However, there is some evidence showing that patients with minor complaints showed stronger participation preferences than patients facing major decisions. 8
Whether a decision is viewed as minor or major might be influenced by the severity of the disease and the patient’s experience with the disease. As it is still unclear whether patients’ preferences for participation differ between different diseases and especially between chronic vs. acute conditions, the aim of the present analysis was to investigate the impact of different medical conditions on patients’ participation preferences using a large sample size which allowed controlling for socio‐demographic variables.
We expected patients suffering from ‘chronic’ conditions to show stronger participation preferences than patients with ‘acute’ conditions.
Design and Participants
Data of the Autonomy Preference Index (API), decision‐making preference scale, a measure of patients’ desire to participate in medical decisions, 3 were pooled from six independent trials on SDM. All trials were conducted within a programme funded by the German Ministry of Health between 2001 and 2004 and used the same scale (API) as well as the same coding for socio‐demographic variables (age, gender, education).
All projects focused on medical decisions for patients with specific diagnoses and evaluated interventions to facilitate SDM (e.g. decision aids or communication trainings). Thus patients gave informed consent to the studies and were aware of the topic to be studied. Results of the single trials (including API data) have been published elsewhere (for details see http://www.shared‐decision‐making.org).
There are six groups of patients in the dataset (total n = 1393, see Table 1 for additional data):
Table 1.
Characteristics of the study population
| Diagnosis | Setting | Study center | n (%) | Age (years), mean (SD) | Gender (% female) | Education (%≥12 years) | API mean (SD) | Cronbach α |
|---|---|---|---|---|---|---|---|---|
| Hypertension | Primary care | Erlangen | 164 (11.8%) | 59.4 (10.9) | 60.2 | 18.0 | 45.2 (15.7) | 0.57 |
| Depression | Primary care outpatient setting | Freiburg | 230 (16.5%) | 48.7 (16.8) | 74.0 | 25.2 | 46.2 (21.9) | 0.79 |
| Breast cancer | University hospital | Munich | 178 (12.8%) | 58.5 (10.7) | 100 | 30.0 | 42.8 (25.3) | 0.86 |
| Schizophrenia | State hospitals and a university hospital | Munich | 120 (8.6%) | 37.8 (12.0) | 47.2 | 21.7 | 47.2 (18.4) | 0.59 |
| Multiple sclerosis | University hospital | Hamburg | 105 (7.5%) | 38.3 (7.6) | 78.1 | 11.5 | 66.3 (16.7) | 0.70 |
| Minor traumas | Emergency department | Berlin | 596 (42.8%) | 35.8 (13.4) | 39.1 | 56.2 | 49.6 (17.5) | 0.63 |
| All | – | – | 1393 | 43.7 (16.1) | 58.7 | 37.0 | 48.7 (20.0) | 0.70 |
API, Autonomy Preference Index.
-
•
Outpatients in primary care practices suffering from hypertension. Inclusion criteria: patients with known hypertension, blood pressure <166/110, no serious heart disease.
-
•
Outpatients in primary care practices with depressive disorders: inclusion criteria: patients with newly diagnosed depression.
-
•
Inpatients in two state hospitals and one university hospital suffering from schizophrenia. Inclusion criteria: patients aged 18–65 years who had been admitted to psychiatric hospital for acute schizophrenia, first and multiple episodes.
-
•
Inpatients in a university hospital suffering from breast cancer. Inclusion criteria: women aged 18–75 years, newly diagnosed with breast cancer prior to first surgical intervention.
-
•
Outpatients in a specialized clinic at a university hospital suffering from multiple sclerosis. Inclusion criteria: random sample of patients being treated for multiple sclerosis (MS) in the specialized outpatient clinic.
-
•
Outpatients visiting a university hospital emergency department for the treatment of minor traumas. Inclusion criteria: all patients visiting the emergency department.
All these single studies aimed at recruiting patients consecutively to avoid any selection biases. The API was administered at baseline of the studies before any intervention had taken place.
The API (decision‐making preference scale) is a 6‐item self report instrument devised to measure patients’ general desire to participate in medical decisions. For the API scale, totals were transformed to the range from 0 to 100, where 0 corresponded to complete lack of desire to make decisions and 100 corresponded to the strongest possible desire. For example, if the patient recorded the weakest preference for participation on all six questions he would score 6, which would become 0 on the adjusted scale. If he showed the strongest preference on each question, he would score 30, which would become 100 on the adjusted scale.
Intermediate scores have been interpreted as reflecting a desire for decision‐making that is shared equally between doctor and patient. 9 The API has been validated and utilized in US primary‐care patient populations. Internal consistency was reported as α = 0.82, test–retest reliability r tt = 0.84. 9
For the studies presented, a German version of the API was used. The scale was therefore translated into German and retranslated into English by independent persons and sent to the authors of the original scales to avoid misunderstandings. 10 Data of internal consistency are shown in Table 1. Internal consistency rose if the two items that were reversely coded (items 4 & 6) were removed.
Statistical analysis
A multiple linear regression analysis was performed with the API score as dependent variable, and age, gender, education and diagnosis as independent variables. Because education and diagnosis were categorical variables with more than two values, we recoded them creating one variable per value (e.g. minor trauma: yes/no, >12 years of education: yes/no). To test whether linear regression was the appropriate method, a Q–Q plot of the standardized residuals was performed, which on inspection showed no difference from the normal distribution. For subsequent comparison between the groups, we used minor trauma (‘acute condition’) and education >12 years as reference.
Results
Table 1 shows the patients’ characteristics for each individual diagnostic group and for the pooled dataset, mean API scores ranged from 42 (breast cancer) to 66 (multiple sclerosis). Of the 1393 patients, 1347 patients were entered in the multiple regression analysis (Table 2, 46 cases were excluded due to lacking values). The patient’s age (P < 0.001), gender (P = 0.002) and education (P ≤ 0.001 for patients graduated after >12 years vs. all other categories) significantly predicted participation preferences, with younger patients, women and better educated patients expressing a greater interest in being involved in medical decisions (higher API scores).
Table 2.
Regression model for participation preferences
| B | 95% CI | P‐value | ||
|---|---|---|---|---|
| Lower bound | Upper bound | |||
| Age | −0.208 | −0.284 | −0.131 | <0.001 |
| Gender | 3.552 | 1.361 | 5.743 | 0.002 |
| Education (compared with graduation after >12 years) | ||||
| Graduation after 10 years | −5.900 | −8.287 | −3.513 | <0.001 |
| Graduation after 8/9 years | −10.870 | −13.698 | −8.042 | <0.001 |
| No graduation | −13.668 | −21.697 | −5.640 | 0.001 |
| Diagnosis (compared with ‘minor trauma’) | ||||
| Depression | 2.266 | −0.862 | 5.393 | 0.156 |
| Multiple sclerosis | 18.213 | 14.156 | 22.269 | <0.001 |
| Breast cancer | −0.758 | −4.635 | 3.118 | 0.701 |
| Schizophrenia | 1.384 | −2.496 | 5.264 | 0.484 |
| Hypertension | 3.670 | −0.105 | 7.446 | 0.057 |
Constant: 55.2.
The participation preferences for the diagnostic groups (as shown by API scores) are shown in Fig. 1 (without adjustment for age, gender, education). On inspection, patients with an ‘acute condition’ (minor trauma) and patients with most of the ‘chronic conditions’ (hypertension, depression, schizophrenia) appeared very similar; breast cancer patients tended toward lower desire for participation; and patients with multiple sclerosis were clearly different, with higher preferences for participation.
Figure 1.
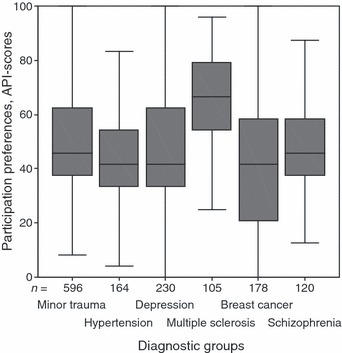
Participation preferences of members of different diagnostic groups (box plot).
Linear regression analysis confirmed that the patient group suffering from relapsing‐remitting multiple sclerosis and reporting to a university outpatient clinic showed API scores significantly different (P < 0.001) from those of patients in the reference group (acute condition/patients with minor traumas). There was also a trend for patients with hypertension in a primary‐care outpatient setting (P = 0.057) to express higher participation preferences after socio‐demographic variables were controlled for. There were, however, no significant differences between the reference group and the other conditions.
The model explained 14% of the variance (adjusted R 2 = 0.14).
Discussion
All patient groups studied showed participation preferences that indicate the wish for being actively involved in medical decisions but not for taking over complete control. Younger patients, women and better educated patients expressed a stronger desire to be involved in medical decisions. The group of patients suffering from relapse‐remitting multiple sclerosis had significantly higher API scores (independently of their socio‐demographic characteristics) than patients with other conditions.
Strengths and limitations
The strengths of the present study are founded in the large sample size, the possibility of adjusting for socio‐demographic variables and in the existence of well defined groups of patients with different diagnoses. In all trials, the aim was to recruit patients consecutively to avoid bias, but differences in trial designs and inclusion criteria might still have had an influence on the inter‐group comparisons.
In addition, the internal consistency of the API scale was relatively low for some patient groups. Adaptations of the scale for specific indications would probably be necessary.
In our study, we were able to show that most patients express interest in being included in medical decisions. It can be stated that patients neither want to decide everything on their own nor to leave the decisions solely up to their doctors. This also holds for patients with severe somatic (MS, breast cancer) or mental illness.
Our study shows that patients with multiple sclerosis have a significantly greater desire to participate in medical decision‐making than the patients studied with the other conditions. At first sight, this result is in accordance with our hypothesis that a chronic condition (MS) might yield higher participation preferences than an acute condition (minor trauma). However, the other conditions studied (hypertension, schizophrenia, depression, breast cancer) are also supposed to be chronic conditions and which in our study did not lead to higher API‐scores than the acute conditions.
Thus explaining the difference between the MS‐group and the other conditions must remain speculative with a plethora of possible reasons:
-
•
The nature of multiple sclerosis (e.g. the fear of loss of control that most patients with MS experience).
-
•
The treatment options for MS (e.g. only partial efficacy of interferon therapy).
-
•
The setting of the MS‐trial (specialized outpatient unit, possible selection bias towards more active patients).
The question of which factors prove responsible for the findings of our study should be subject to further research.
Apart from the findings on MS, we note that the differences in participation preferences among the other conditions are small, with only one group (hypertension) approaching (but not reaching) significance. These results are also of interest as for example one might have expected patients with schizophrenia to express higher participation interests than patients suffering from depression. Thus our results might help in destigmatizing both groups of patients by showing that those with schizophrenia do not want to take over complete control (and therefore can be included in treatment decisions) and that depressed patients still show interest in their treatment process and responsibility for their care can be handed over to them.
We also replicated earlier findings that age, gender and education have an influence on participation preferences. 6 Thus women, younger patients as well as patients with a higher level of education have stronger participation interests.
All of the factors identified in our study, however, account for only 14% of the total variance. The differences from one person to the next are so strong as to dominate all other factors. Thus our predictive ability is low when using only socio‐demographic and illness specific variables. In daily practice, physicians need to look at the individual patient and implicitly or explicitly address the issue of patients’ preferences.
Acknowledgements
The participating projects were funded individually by the German Ministry of Health. Furthermore, the data collection and analysis were made possible by grants from the German Ministry of Health (Grants # 217‐43794‐5/6 and ‐5/11).
References
- 1. Coulter A. Partnerships with patients: the pros and cons of shared clinical decision‐making. Journal of Health Service Research & Policy, 1997; 2: 112–121. [DOI] [PubMed] [Google Scholar]
- 2. Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision‐making and interpersonal behavior: evidence, models and interventions. Patient Education and Counseling, 2006; 61: 319–341. [DOI] [PubMed] [Google Scholar]
- 3. Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients’ desire for autonomy: decision making and information‐seeking preferences among medical patients. Journal of General Internal Medicine, 1989; 4: 23–30. [DOI] [PubMed] [Google Scholar]
- 4. Krantz DS, Baum A, Wideman M. Assessment of preferences for self‐treatment and information in health care. Journal of Personality and Social Psychology, 1980; 39: 977–990. [DOI] [PubMed] [Google Scholar]
- 5. Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Canadian Journal of Nursing Research, 1997; 29: 21–43. [PubMed] [Google Scholar]
- 6. Benbassat J, Pilpel D, Tidhar M. Patients’ preferences for participation in clinical decision making: a review of published surveys. Behavioral Medicine, 1998; 24: 81–88. [DOI] [PubMed] [Google Scholar]
- 7. Whitney SN. A new model of medical decisions: exploring the limits of shared decision making. Medical Decision Making, 2003; 23: 275–280. [DOI] [PubMed] [Google Scholar]
- 8. Schneider A, Korner T, Mehring M, Wensing M, Elwyn G, Szecsenyi J. Impact of age, health locus of control and psychological co‐morbidity on patients’ preferences for shared decision making in general practice. Patient Education and Counseling, 2006; 61: 292–298. [DOI] [PubMed] [Google Scholar]
- 9. Nease RF Jr., Brooks WB. Patient desire for information and decision making in health care decisions: the Autonomy Preference Index and the Health Opinion Survey. Journal of General Internal Medicine, 1995; 10: 593–600. [DOI] [PubMed] [Google Scholar]
- 10. Giersdorf N, Loh A, Harter M. [Measuring shared decision making]. Zeitschrift für ärztliche Fortbildung und Qualität im Gesundheitswesen, 2004; 98: 135–141. [PubMed] [Google Scholar]


