Abstract
Context The use of written decision aids (DAs) in clinical practice has proliferated. However, few DAs have been developed for low literacy users, despite this group having low knowledge about healthcare and lacking involvement in health decisions.
Objective To explore the information needs and understanding of adults with varying literacy in relation to colorectal cancer screening, and to consider their responses to two versions of a decision aid.
Participants Thirty‐three men and women aged 45–74 years were recruited from Adult Basic Education classes (n = 17) and University Continuing Education programs (n = 16).
Methods We used qualitative methods (in‐depth, semi‐structured interviews) to compare and contrast the views of adults with lower and higher literacy levels, to gain a better understanding of how people with lower literacy value and interpret specific DA content and components; and determine whether needs and preferences are specific to lower literacy groups or generic across the broad literacy spectrum.
Results Regardless of literacy perspective, participants’ interpretations of the DA were shaped by their prior knowledge and expectations, as well as their values and preferences. This influenced perceptions of the DAs role in supporting informed decision making. A linguistic theoretical model was applied to interpret the findings. This facilitated considerations beyond the traditional focus on the readability of materials.
Conclusion Decision aids developers may find it useful to apply alternative approaches (linguistic) when creating DAs for consumers of varying literacy.
Keywords: colorectal cancer screening, decision aid, faecal occult blood test, health literacy, informed choice, informed decision‐making
Introduction
Reducing health inequalities is a priority in developed countries 1 , 2 , 3 where there is evidence that disparities in health may be explained, in part, by low levels of literacy. The term ‘health literacy’ has been used to describe the capacity to which an individual can apply literacy skills to enhance their health. In this context, health literacy is defined as not only the ability to read, but as the cognitive and social skills which facilitate individuals and communities to gain access to, and understand information in ways which promote good health. 4
Research indicates that people with limited literacy consistently demonstrate lower levels of knowledge about disease, poorer self‐care management and lack active involvement in health decision making. 5 These factors in turn impact upon health outcomes. Studies also show a negative effect of low literacy on a range of chronic health conditions including hypertension, diabetes, asthma and HIV/AIDS. 6 , 7 , 8 , 9
Low literacy is widespread. The International Adult Literacy Survey (IALS) suggests that levels of literacy in several major developed nations are ‘low’, or even ‘very low’. 10 , 11 Alongside growing awareness of the prevalence of low literacy in Western countries and its negative impact on health, there has been an upward shift in consumers demand for health information and desire for greater involvement in decisions. This has been fuelled by (i) the internet, (ii) availability of more health‐care options and (iii) evidence based medicine and patient centred healthcare, which recognize the importance of ensuring patients are adequately informed about their options.
Informed decision making occurs when ‘an individual understands the nature of the disease or condition being addressed; understands the clinical service and its likely consequences, including risks, limitations, benefits, alternatives and uncertainties; has considered his/her preferences as appropriate;…and makes a decision consistent with his/her preferences and values…’. 12 Decision aids (DAs) are tools which have been developed to support this process. A systematic review showed that DAs increase knowledge, reduce uncertainty and increase involvement in decision making across a range of clinical settings. 13
While the use of DAs has grown dramatically, most are dependent upon high levels of literacy and numeracy. There have been few attempts to encourage people from less literate backgrounds to make informed health decisions through the use of decision support materials. There are, however, a few exceptions. 14 , 15 , 16 These studies used both quantitative and qualitative approaches to tailor decision materials for low literacy populations. However two studies 15 , 16 did not fully examine whether the DA content addressed the consumers’ needs and concerns, to support their decision. One study 14 qualitatively identified patients’ views towards the factual content, language, and design of a DA. However, they did not explore in depth, the comprehension of, and preferences towards specific DA components such as graphical risk information, patient stories–examples of how and why other patients made their decision, and exercises to help patients understand their options and elicit values (values clarification exercises). In addition, the methodological approach (focus groups) may not have been most appropriate for those with low literacy, since they may be reticent in publicly disclosing their difficulties with interpreting written information, due to feeling embarrassed or ashamed. 17 In contrast, participants talking to an interviewer in private, who is sensitive to their literacy level, may be more likely to express the problems they have processing text, enabling the interviewer to fully explore whether the information is understood.
In this study we explored consumers’ information needs, preferences and levels of comprehension, to inform the development of a colorectal cancer (CRC) screening DA tailored for low literacy consumers. In Australia, US and the UK colorectal cancer represents a major public health problem. 18 , 19 There is strong evidence that screening with faecal occult blood testing (FOBT) significantly reduces CRC mortality, 20 and several countries have recently established FOBT screening programmes. 21
Decision aid development is guided by the International Patient Decision Aid Standards (IPDAS), a set of criteria for DA developers to use in the creation of materials supporting informed choice. 22 These guidelines adopt the traditional and dominant approach to developing health information for low literacy groups, including; applying principles of plain language, measuring the readability of text, 23 and assessing the suitability of the materials. An alternative approach, based on systemic linguistic theory, suggests that key ‘linguistic’ features, combined with an evaluation of the factual and visual content should be considered in assessing patient materials. 24 This theoretical model takes into account the significance of context and considers how the reader uses language to make meaning, and how language is organized to enable meanings to be made. This model critiques methods such as readability testing (mathematical formulae based on the number of syllables and sentence length), for failing to recognize that readers’ views and beliefs influence how they engage with information. These different approaches (traditional and linguistic) to developing health materials were considered in the interpretation of our findings.
This paper explores the information needs and preferences of adults with lower and higher literacy levels towards a FOBT DA designed to support informed decision making. This research forms part of a larger study, to evaluate whether a DA tailored for lower literacy populations can support informed choice and involvement in decision making. We examined key components of the generic DA structure (e.g. communication of risk information, patient stories and exercises for eliciting values), to gain a better understanding of how people with lower literacy value and interpret the content of DAs. To determine whether needs and preferences were specific to lower literacy groups alone or were generic across all consumers, we included higher literacy adults to compare and contrast our findings.
Method
Recruitment procedure
Participants were recruited according to their CRC screening eligibility and literacy level:
-
1
Adults with lower literacy, (n = 17) were recruited from government funded adult basic education literacy classes held at further education colleges (TAFE) in Sydney, Australia. Since our focus was on materials for English speakers, rather than issues of translation, we recruited adults with good spoken English language skills.
-
2
Participants with higher literacy (n = 16) were recruited from the University of Sydney’s Continuing Education Program which offers courses in areas such as philosophy, languages and literature. These courses require a high level of literacy skill.
Ethics approval was obtained from the University of Sydney Human Ethics Committee.
Study materials
For the first stage of DA development we modified a more technical DA for Australian men and women aged 45–74 considering whether to participate in FOBT screening. The original DA was developed and evaluated using the Cochrane Review CREDIBLE criteria – a comprehensive set of criteria for assessing the quality of patient DAs. 25 It was evaluated by randomized trial design and found to increase informed choice among consumers. 26 An updated version of the original DA is available at: http://www.health.usyd.edu.au/shdg/resources/decision_aids.php. However, it was not specifically tailored for consumers with lower literacy. Modification of the original tool to the low literacy version involved the application of plain language, basic design principles and simple strategies to lower the cognitive burden. 27 , 28 This included; simplifying the text, replacing medical terminology with lay language, shortening long paragraphs into smaller segments and providing context prior to factual information. We were guided by IPDAS in the creation of the key DA components (risk information, patient stories and values clarification exercises) to identify understanding and preferences towards different formats of each. 22 , 29 , 30 For the presentation of risk information this included using (i) natural frequencies 31 ; (ii) appropriate time frames across all outcomes; and (iii) consistent denominators. Visual illustrations were integrated into the DA, based on research suggesting that combining pictures with text enhances attention, recall and understanding among low literacy groups. 32
Data collection
Participants were interviewed between May and October 2005. Face‐to‐face interviews were conducted by (SS) using a topic guide (see Table 1). The semi‐structured interviews were designed to combine structure with flexibility and were centred on a set of open‐ended questions. All interviews were carried out in English, audio tape‐recorded and transcribed verbatim. Interviews with lower literacy participants took place at participating TAFE colleges. Higher literacy participants stated their preferred interview location, the University of Sydney campus, or at the participant’s home.
Table 1.
Topic guide: issues addressed in the interviews
| 1. Participants socio‐demographic background |
| 2. Initial impressions of original DA |
| 3. Information needs and preferences towards decision aid content and design |
| Page by page review to assess understanding and preferences for style of information |
| 4. Comprehension and preferences for different risk presentation formats |
| 5. Comprehension and preferences for values clarification exercises |
| 6. Comprehension and preferences for patient stories |
| 7. Knowledge, attitudes and understanding of cancer screening |
| 8. Preferred decision‐making role |
Participants were shown two DAs (original and new version). Participants were asked to express their initial impressions of the original version. A systematic (page‐by‐page) approach was used to review the new version of the DA, affording the interviewer opportunity to specifically inquire about comprehension of sections of text and DA components.
The interviewer gave assistance to those who had difficulties reading the material, and also noted particular words or sections that participants struggled with. A standard ‘teach back’ approach was adopted whereby participants were asked to describe in their own words what the text was describing/explaining and what they did/did not understand. Examples of questions included: ‘Can you describe this information in your own words?’, ‘How could it be made clearer?’, ‘What is this diagram showing you?’.
Data analyses
Framework Analysis method 33 was used to identify emerging themes and analyse the data. This is a matrix‐based approach, with themes making up the columns and cases (participants) making up the rows. A thematic framework was developed by SS and KM through familiarization with a subset of transcripts, independent coding and discussion. All the data were indexed using the thematic framework and summarized within the matrix. This allowed us to examine the synthesized data, both within and across themes and cases. By applying this matrix‐based analytic approach, we were able to explore relationships and explanations for patterns. Issues arising from the qualitative analysis were resolved through ongoing discussion between SS and KM until agreement was reached.
Results
The demographic characteristics of higher and lower literacy groups are presented in Table 2. As expected the samples were different in terms of education and working status. Those with lower levels of literacy all had lower educational attainment and a greater number were unemployed. Those with higher levels of literacy were all tertiary educated and were more likely to be employed or retired.
Table 2.
Socio‐demographic characteristics of lower and higher literacy participants (n = 33)
| Variable | All (n = 33) | Lower literacy group (n = 17) | Higher literacy group (n = 16) |
|---|---|---|---|
| Age (in years) | |||
| 45–54 | 8 | 5 | 3 |
| 55–64 | 21 | 12 | 9 |
| 65–74 | 4 | 4 | |
| Gender | |||
| Male | 14 | 9 | 5 |
| Female | 19 | 8 | 11 |
| Country of origin | |||
| Anglo Australian/ New Zealand | 22 | 9 | 13 |
| UK | 3 | 1 | 2 |
| Europe (Spain, Italy) | 4 | 3 | 1 |
| South America | 4 | 4 | |
| English speaking background | |||
| Yes | 26 | 10 | 16 |
| No | 7 | 7 | |
| Age at leaving full time education | |||
| 10–14 | 7 | 7 | |
| 15–19 | 8 | 8 | |
| >20 | 16 | 16 | |
| Did not attend formal schooling | 2 | 2 | |
| Educational status (qualifications) | |||
| No formal qualification | 16 | 16 | |
| Leaving certificate/High | 1 | 1 | |
| School certificate or equivalent | |||
| University degree or equivalent | 16 | 16 | |
| Working status | |||
| Working full or part time | 10 | 4 | 6 |
| Unemployed | 8 | 8 | |
| Retired | 14 | 4 | 10 |
| Other | 1 | 1 | |
The responses of lower literacy participants are compared and contrasted with those provided by higher literacy participants. Verbatim quotations are followed by the participant’s ID number, gender (M or F), age and literacy level: higher literacy (HL) and lower literacy (LL).
Cognitive burden – density, length and organization of information
Higher and lower literacy participants gave similar responses when asked about their initial impressions of the DAs. Many thought the new DA was ‘friendly’, ‘easy to read’, ‘clear’ and ‘not too intricate’. Both groups highlighted the importance of presenting health information in a ‘direct’, ‘short’ and ‘sharp’ way to increase ‘retention’ and motivate the reader to use the material.
The less you have to read the better. I find when you are reading you want it to be straightforward and quick, you don’t want to sit down for half an hour. (ID32 F age 60 HL)
If you present me with lots of pages I probably would look through it and think that’s too much. Probably too many words I don’t understand. I would rather have less reading. (ID6 F age 58 LL)
Those with poorer reading skills described the density of text in the original version as ‘intimidating’ and ‘frightening’. Condensing the amount of text on each page was suggested as a way to improve the DAs readability.
Although several of the higher literacy participants found the new version ‘dumbed down’, they did not indicate feeling overly excluded by the DA material. Instead, they commonly recognized the value of tailoring information to suit readers with different literacy demands, ensuring the information was accessible to a range of readers.
You want the information to be accessible to everybody, but there is a risk of some people feeling like their intelligence is being insulted. But I actually think it is critically important that the information is available to everybody and I think it is better to risk people like me going, oh, than somebody being cut out from that information. (ID27 F age 49 HL)
Participants with higher literacy skills were more likely to make suggestions relating to the order of sections presented in the DA. Both literacy groups found the section headings useful for ‘quick reference’ and directed the reader ‘straight to the subject of interest’.
It’s [section headings] good because you can sort of read through and pick up points you’re more interested in, without going through everything. (ID6 F age 58 LL)
The perceived role of the decision aid in screening
Both literacy groups felt the DA ought to be encouraging screening and struggled to understand that it was not promoting acceptance of screening, but facilitating informed choice.
Really what it should be saying is something a little bit more, more definite, I think it [screening] is really a good idea or but if you are making the decision, it leaves it open and most people would think, well no! (ID18 F age 60 LL)
Many lower literacy participants were unfamiliar with the concept of informed choice in context of screening, whereas higher literacy participants seemed to understand the non directive nature of the DA more readily.
I think it is giving people a chance to make an informed judgment. (ID31 F age 64 HL)
Comprehension of medical terminology
Lower literacy participants had difficulties pronouncing and understanding the medical terminology used in both of the DAs. Such terms included vocabulary specific to CRC screening: ‘faecal’, ‘occult’, ‘colonoscopy’, ‘sigmoidoscopy’, ‘bowel cancer’,‘polyp’, and words commonly used in medical settings: ‘screening’, ‘abnormal’, ‘factors’, ‘symptoms’. These were frequently described as ‘mysterious’, ‘puzzling’ and for ‘scientifically minded’ people.
My reading levels not…I mean I can work out things, by reading bits and pieces and that, but medical words and that, not real good. (ID14 F age 52 LL)
Even those with better reading skills were unfamiliar with the medical language and the translation of medical terms using a simple glossary was valued by both groups. One lower literacy participant saw the explanation of medical terms as a means to inform and empower patients.
You can arm yourself with some information to go and ask your doctor. (ID10 M age 51 LL)
Use of visual images: illustrations and medical diagrams
Attitudes towards the illustrations varied. Lower literacy participants were generally positive about their use, and perceived the visuals to ‘grab’ the reader’s attention and enhance text comprehension.
I thought they were quite good. So, even if you’ve missed out a bit of the information, the picture helps a little bit. (ID15 M age 54 LL)
Higher literacy participants perceived their function as allowing the reader to take a ‘visual break’ from the text. The images were often viewed by this group as ‘patronising’, ‘childish’, and ‘meaningless’, and there was a strong emphasis on the importance of creating illustrations closely related to the text.
Irrelevant pictures don’t really add very much to the text…I think that any illustrations for something involving health should have a purpose behind them. (ID31 F age 64 HL)
In contrast, the use of medical diagrams (images of the colon) were universally well received by both groups and seen to convey important anatomical information. Again, this was seen to ‘arm’ patients during the consultation.
A very good illustration...doctors talk to you about large intestines, small intestines and if you don’t have a medical background, you have no idea exactly which bit of you anatomy they are talking about. You could go in, informed and know exactly which bit of your body they were talking about. (ID31 F age 64 HL)
You really want to know what cancer is, you want to know where it is situated, how it affects you. Yeah, that’s good. (ID10 M age 51 LL)
Presentation format of quantitative risk information
Quantitative risk information was represented using absolute risk (see Fig. 1a,b extracted from the new version of the DA) and relative risk reduction. Probabilistic information framed in terms of relative risk (i.e. having the bowel cancer screening test every 2 years will reduce your chance of dying from bowel cancer by 23%) generated confusion among both literacy groups. This misinterpretation led them to overestimate the likely benefits of screening.
Figure 1.
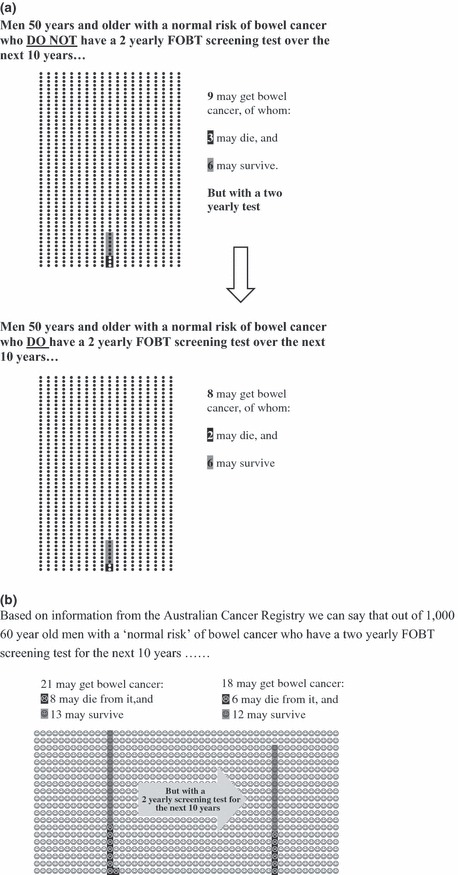
Examples of absolute risk information. (a) systematic ovals format; (b) Smiley face’ format.
[23%] That’s 23 out of 100, it’s nearly a quarter. So it’s best to be safe than sorry. (ID17 F age 60 HL)
When the same information was expressed as absolute risk data, using graphical formats (e.g. smiley faces/systematic oval diagrams), both literacy groups were surprised that the figures did not produce a more ‘compelling argument’ in favour of screening:
I don’t know if they’re good odds. I don’t know if I’d want to back a racehorse on those. (ID24 M age 67 LL)
Although framing risk information in absolute terms enhanced comprehension, some lower literacy participants misunderstood the concept of one face/oval representing one person. Conveying absolute risk information using an analogy was suggested as a way to facilitate understanding:
I’m just picturing half of the Enmore theatre. Nine people in there have bowel cancer. That’s the way I look at it. (ID11 M age 55 LL)
There was variation in feedback about the use of smiley faces and systematic ovals. Higher literacy participants generally felt that the faces were suitable for a younger age group. In contrast, most of the lower literacy participants were indifferent towards the faces but found them difficult to interpret. Both literacy groups expressed a preference for systematic ovals.
Values clarification exercise and patient story examples
Two versions of the interactive values clarification exercises (VCEs) were created to help participants evaluate outcomes in the context of their own values and preferences (see Fig. 2a,b extracted from the new version of the DA). Participants were also presented with two different patient story examples. These stories act as implicit, non‐interactive exercises to exemplify the processes which others have used to make their decision. Higher literacy participants thought the patient stories were useful for someone with no prior knowledge.
Figure 2.
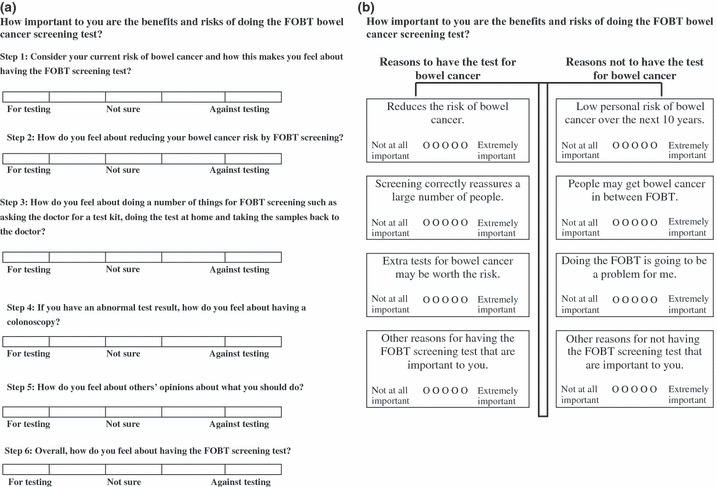
Examples of the values clarification exercise for people making a decision about FOBT screening. (a) ‘Steps’ format; (b) Weigh Scale’ format.
It returns us to a real life situation of someone else’s predicament and forces you to make an assessment of your situation. (ID5 M age 65 HL)
In contrast lower literacy participants seemed confused by the patient stories and VCEs which highlighted the choice to screen or not. This notion was apparently unfamiliar and confusing, and raised concerns that the exercises may ‘set up a situation which encourages people not to screen’.
Regardless of literacy, most participants expressed a preference for the weigh scale format, describing it as ‘concise’, ‘simple’ and ‘direct’.
In contrast, the ‘step’ format was referred to as ‘repetitive’ and ‘overwhelming’. Some, however, felt that the weigh scale design may not be culturally appropriate. One participant described the meaning of a weigh scale in her culture as representing equilibrium rather than choosing one option over another.
The balance tells you…it is very important in our culture [Chilean] because normally you have to be right in the middle…If you go one up, one down, that means it’s not right. (ID7 F age 59 LL)
Evaluating scientific information for quality and credibility
The provision of scientific references as ‘extra information’ was generally welcomed by those with higher literacy and reassured them that the factual content had been rigorously researched. References were seen to enhance the DA’s ‘authenticity’ and not ‘interfere’ with the overall comprehension of material.
It comes back to knowing where to go to get relevant or informed information from a reliable source. (ID28 F age 58 HL)
In contrast, those with limited literacy generally referred to them as ‘meaningless’, ‘irrelevant’, and exclusively for academics.
I don’t think you need to know who did all the looking and searching for it and everything. It is not going to mean anything to you. (ID 33 M age 63 LL)
Concerns were expressed by both literacy groups about the perceived barriers to obtaining and understanding scientific information. The provision of additional sources of information (other than scientific references), such as telephone helplines were proposed as ways to make the information more accessible to lay people.
Discussion
Few studies have directly involved adults with lower literacy in the development of written health‐care materials designed to facilitate decision making. Using colorectal cancer screening as a case study, this study sought to explore the similarities and differences in the information needs and comprehension of adults with lower and higher literacy levels towards DA materials. It should be noted that we did not directly measure literacy among our sample. Instead, participants enrolled in adult education classes to develop basic literacy skills were deemed to have lower levels of literacy, and those possessing a tertiary education were deemed to have higher levels. Adults enrolled in adult basic education programs have their literacy level and language skills assessed on entry, so we feel confident that our sample reflected adults with lower levels. None of our tertiary educated sample demonstrated reading difficulties, and were all attending classes, requiring high levels of literacy to participate. Although our sample may not be considered representative of all adults across Australia, our findings may be transferable to other groups in similar contexts or settings. 34
Our methodological approach has several advantages. Our data collection method (face‐to‐face interviews) allowed us to tailor interviews to the individual literacy level of the participant, and reduce feelings of stigma and embarrassment associated with low literacy. 17 This provided a rigorous understanding of how a cancer screening DA can meet the needs of people with varying literacy. Excluding participants who had limited English language skills, allowed us to focus on issues of literacy, as opposed to issues of translation. We consider these to be two distinct issues. Yet, much health literacy research fails to distinguish between the two. There is a lack of recognition for non‐English speakers who may be highly literate in their primary language. Thus, the challenges of low literacy, and low health literacy may be confused with the challenges of second language; this confusion is avoided in our study.
The findings from this study have general implications for the design of written health communication materials, and specific lessons for DA development. In line with evidence on communicating risk information, 31 , 35 , 36 we found that consumers had a more accurate perception of the chances of colorectal cancer mortality (with and without screening), if expressed in terms of absolute risk rather than relative risk. Similarly, communicating the outcomes of screening as natural frequencies (10 out of 1000) was better understood by our sample. Although visual aids, such as smiley faces, improved comprehension, several lower literacy participants misinterpreted this visual representation, and higher literacy participants found them juvenile. Developers of DAs may consider simplifying the representation of risk information through analogies, 37 to help patients anchor risk information and/or concepts that relate to more familiar, everyday situations. This technique may be especially helpful for low literacy populations. Given that risk information is a key DA component, research is needed to formally test understanding and accuracy of different graphical risk formats and the use of analogies, especially among low literacy groups.
Our results provide qualitative data on the value of combining visual illustrations with written health information. A recent review discussed how using illustrations, in conjunction with text, can play a significant role in aspects of health communications. 32 The integration of illustrations generated different responses. Lower literacy participants felt visuals attracted attention to the material and enabled the reader to make sense of the textual message; whereas the higher literacy participants found the pictures patronising, and only enhanced understanding if they were closely related to the meaning of the text.
In addition to the presentation characteristics highlighted above, participants described other factors that influenced how they processed and engaged with the information. Regardless of literacy perspective participants considered the intended message of the DA in the context of what they knew and understood about screening in general. Based on their pre‐existing knowledge and experiences participants often came to the text with predefined questions and expectations about where information could be located. As such, they highlighted features of the DA (use of topic headings and colour coding) which enabled them to scan for information perceived as salient. Their response to these elements demonstrated that patients and consumers are not ‘empty vessels’ 38 and come to health information with their own views, ideas and priorities.
These additional factors, however, are not captured by the conventional methods for designing health education materials or DAs. In this regard we found the linguistic theoretical model 24 to be helpful in making sense of the results as it encompasses a broader range of features. In line with the linguistic model, our findings suggest that the order in which different sections were presented (generic structure) was perceived as important.
In keeping with both the linguistic and traditional approach, participants referred to the complexity of medical terms (lexical density); and the value of topic headings, in that they serve to direct the reader to areas of interest, without having to read the material from beginning to end. 39 Thus, the reader may not necessarily read health materials in a linear process, but purposively search for relevant sections of text, to answer questions (e.g. what is bowel cancer screening? what does screening involve?). 40
The linguistic model also stresses the importance of presenting quality, up‐to‐date evidence‐based information. Consistent with this model, higher literacy participants perceived scientific references to enhance the DAs authenticity, even though they said they would be unlikely to actively seek scientific information to inform their decision.
An important component of participant’s response to the material was their perception and understanding of the role of the DA. The linguistic model describes this as the metadiscourse. We found that many participants were confused by the metadiscourse of the DA in supporting informed choice, as opposed to encouraging a particular health behaviour. The concept of informed decision making in cancer screening was unfamiliar to some, and whether or not to accept screening was not perceived as a decision to deliberate. This difficulty to comprehend choice exists in screening has been previously documented 41 and may be partly explained by the ‘enthusiasm’ surrounding cancer screening. 42 Our study showed that even when explicitly informed that there is a choice in CRC (to screen or not), those with limited literacy still had difficulties understanding the concept of choice. Whereas those with higher literacy grasped this concept more readily. It could be argued that this is understandable given the large volume of patient education materials defining patient involvement in terms of compliance rather than autonomy. We suggest that screening DAs should first clarify to the reader that there is a choice, and explain the reasons why a person may or may not choose to participate in screening. 41 This will help to ensure that the role of screening DAs are clearly understood by individuals with limited access to evidence based information and choice.
In contrast to measuring readability of materials, the linguistically based model posits a wider range of linguistic aspects to draw on when assessing health information. These include; the overall organization of the text (generic structure), the purpose of each section e.g. to define, explain, instruct or inform (rhetorical elements), the main purpose of the material (metadiscourse), complexity of vocabulary, role relationships expressed in the text (e.g. academic to lay person), the use of subject headings, density of ‘content’ words in the text (lexical density), and the quality of factual content. This model is based upon systemic functional linguistic theory which recognizes that the interplay between text and cultural and situational context enables the reader to construct meaning from the text. It takes into account how the reader uses language and how language is organized to help the reader make sense of the text. In other words, the readers’ interpretations of text may be shaped by their prior experience, beliefs and situation, that extend beyond the information presented. 43 These issues are not well explored in DA research.
Written health information is conceptualized in different ways: (i) to educate and (ii) to empower. 44 The first is guided by a biomedical model whereby patients are constructed as passive. The second reflects a sociological orientation towards empowering people to be involved in health decisions through the use of health‐care texts. DAs are part of the patient empowerment discourse, in that they view scientific information as valuable for consumers to support choice. 22 The linguistic model also fits within this discourse by recognizing that the reader is active in creating meaning from the text.
Our findings lend support to the broader conceptualization of health literacy, which expand beyond the functional approach. We found that participants used cognitive, social and analytical skills to make meaning from the information. Thus, using the linguistic model to interpret the data gave us a better understanding of what a reader does with information and how they use more than just reading skills to engage with it.
At present the IPDAS guidelines recommend using readability formulas to improve the comprehensibility of DAs for low literacy users. However, as demonstrated in this study, understanding of health‐care texts involves a wider range of features not assessed by readability measures.
Although the current study concerned designing an intervention for low literacy populations, our findings also highlight the importance of developing decision tools for different cultural groups. The idea that values clarification exercises which use balancing techniques to help people weigh up the benefits and harms of options, may have diverse meanings in different cultural contexts is an important, yet under researched area in the literature. 45
Conclusion
While most guidelines for producing and appraising written health information have focused on the readability of materials, our analysis lends support to alternative ways of thinking about the role and use of decision support materials. These alternative models of communication draw on linguistic and sociological approaches, and place greater emphasis on context and how the reader’s beliefs and experiences shape their interpretations of the text. Regardless of the reader’s literacy level, health‐care information providers and DA developers may find it useful to, not only identify information needs and preferences, but also consider how the reader’s prior knowledge and expectations may affect how they interact with the material. This alternative approach is particularly important for interventions concerned with empowering consumers to participate in health‐care decisions.
Acknowledgements
This study was funded by the University of Sydney Cancer Research Fund and supported, in part, by a program grant (no. 211205) awarded to the Screening and Test Evaluation Program from the National Health and Medical Research Council (NHMRC) of Australia. Kirsten McCaffery is supported by a Career Development Award from the NHMRC (grant no. 402836).
The authors wish to thank the study participants for giving their time and valuable feedback, and to the TAFE Adult Basic Education teachers (based at TAFE NSW Sydney Institutes Petersham College, Randwick College, Western Sydney Institute Blacktown College) who assisted in the recruitment of participants for this study.
We would also like to acknowledge colleagues Associate Professor Judy Simpson and Professor Phyllis Butow at the University of Sydney for their constructive suggestions with regards to the development of the research project.
References
- 1. Acheson D, Alleyne GA, Casas JA et al Round table discussion. Health inequalities and the health of the poor. Bulletin of the World Health Organisation, 2000; 78: 75–85. [PMC free article] [PubMed] [Google Scholar]
- 2. Acheson D. Independent Inquiry into Inequalities in Health Report. London: The Stationery Office, 1998. [Google Scholar]
- 3. Dixon JM, Douglas RM, Eckersley RM. Making a difference to socioeconomic determinants of health in Australia: a research and development strategy. Medical Journal of Australia, 2000; 172: 541–544. [DOI] [PubMed] [Google Scholar]
- 4. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 2000; 15: 259–267. [Google Scholar]
- 5. DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes. A systematic review of the literature. Journal of General Internal Medicine, 2004; 19: 1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Archives of Internal Medicine, 1998; 158: 166–172. [DOI] [PubMed] [Google Scholar]
- 7. Schillinger D, Grumbach K, Piette J et al. Association of health literacy with diabetes outcomes. Journal of American Medical Association, 2002; 288: 475–482. [DOI] [PubMed] [Google Scholar]
- 8. Kalichman SC, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. Journal of General Internal Medicine, 1999; 14: 267–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self‐care. Chest, 1998; 114: 1008–1015. [DOI] [PubMed] [Google Scholar]
- 10. OECD . Literacy, Economy and Society: Results of the First International Adult Literacy Survey. Paris: OECD, 1995. [Google Scholar]
- 11. OECD . Literacy Skills for the Knowledge Society: Further Results from the International Adult Literacy Survey. Paris: OECD, 1997. [Google Scholar]
- 12. Briss P, Rimer B, Reilley B et al. Promoting informed decisions about cancer screening in communities and healthcare systems. American Journal of Preventive Medicine, 2004; 26: 67. [DOI] [PubMed] [Google Scholar]
- 13. O’Connor AM, Stacey D, Entwistle V et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews, 2003; 2: CD001431. [DOI] [PubMed] [Google Scholar]
- 14. Holmes‐Rovner M, Stableford S, Fagerlin A et al. Evidence‐based patient choice: a prostate cancer decision aid in plain language. BMC Medical Informatics and Decision Making, 2005; 5: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jibaja‐Weiss ML, Volk RJ, Friedman LC et al. Preliminary testing of a just‐in‐time, user‐defined values clarification exercise to aid lower literate women in making informed breast cancer treatment decisions. Health Expectations, 2006; 9: 218–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lawrence VA, Streiner D, Hazuda HP, Naylor R, Levine M, Gafni A. A cross‐cultural consumer‐based decision aid for screening mammography. Preventive Medicine, 2000; 30: 200–208. [DOI] [PubMed] [Google Scholar]
- 17. Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient Education and Counseling, 1996; 27: 33–39. [DOI] [PubMed] [Google Scholar]
- 18. NHMRC . Guidelines for the Prevention, Early Detection and Management of Colorectal Cancer. A Guide for General Practitioners. Canberra: NHMRC, 2000. [Google Scholar]
- 19. Greenlee RT, Hill‐Harmon MB, Murray T, Thun MJ. Cancer statistics, 2001. Cancer Journal for Clinicians, 2001; 51: 15–36. [DOI] [PubMed] [Google Scholar]
- 20. Towler BP, Irwig L, Glasziou P, Weller D, Kewenter J. Screening for colorectal cancer using the faecal occult blood test, hemoccult. Cochrane Database of Systematic Reviews, 2000; 2: CD001216. [DOI] [PubMed] [Google Scholar]
- 21. Australian Commonwealth Department of Health and Ageing . National Bowel Cancer Program. Available at: http://www.cancerscreening.gov.au/bowel/bcaust/program.htm (accessed March 2006). [Google Scholar]
- 22. Elwyn G, O’Connor A, Stacey D et al. The International Patient Decision Aids Standards Collaboration. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ, 2006; 333: 417 Available at: http://www.bmj.com/cgi/content/abstract/333/7565/417, accessed on 19 February 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ley P, Florio T. The use of readability formulas in health care. Psychology, Health & Medicine, 1996; 1: 7–28. [Google Scholar]
- 24. Clerehan R, Buchbinder R, Moodie J. A linguistic framework for assessing the quality of written patient information: its use in assessing methotrexate information for rheumatoid arthritis. Health Education Research, 2005; 20: 334–344. [DOI] [PubMed] [Google Scholar]
- 25. O’Connor AM, Rostom A, Fiset V et al. Decision aids for patients facing health treatment or screening decisions: systematic review. BMJ, 1999; 319: 731–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Trevena L. Overcoming Barriers to the Application of Evidence in General Practice. Sydney: University of Sydney, 2006. [Google Scholar]
- 27. Hibbard JH, Peters JH. Supporting informed consumer health care decisions: data presentation approaches that facilitate the use of information in choice. Annual Review of Public Health, 2003; 24: 413–433. [DOI] [PubMed] [Google Scholar]
- 28. Doak CC, Doak LG, Root JH Teaching Patients with Low Literacy Skills, 2nd edn Philadelphia, PA: J.B. Lippincott., 1996. [Google Scholar]
- 29. Feldman‐Stewart D, Kocovski N, McConnell BA, Brundage MD, Mackillop WJ. Perception of quantitative information for treatment decisions. Medical Decision Making, 2000; 20: 228–238. [DOI] [PubMed] [Google Scholar]
- 30. Gigerenzer G, Edwards A. Simple tools for understanding risks: from innumeracy to insight. British Medical Journal, 2003; 327: 741–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gigerenzer G, Hoffrage U. How to improve Bayesian reasoning without instruction: frequency formats. Psychological Review, 1995; 102: 684–704. [Google Scholar]
- 32. Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Education and Counseling, 2006; 61: 173–190. [DOI] [PubMed] [Google Scholar]
- 33. Ritchie J, Spencer L, O’Connor W. Carrying out qualitative analysis In: Ritchie J, Spencer L. (eds) Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications, 2003: 219–262. [Google Scholar]
- 34. Lincoln Y, Guba EG. Naturalistic Inquiry. Newbury Park, CA: SAGE, 1985. [Google Scholar]
- 35. Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Annals of Internal Medicine, 1997; 127: 966–972. [DOI] [PubMed] [Google Scholar]
- 36. Man‐Son‐Hing M, O’Connor AM, Drake E, Biggs J, Hum V, Laupacis A. The effect of qualitative vs. quantitative presentation of probability estimates on patient decision‐making: a randomized trial. Health Expectations, 2002; 5: 246–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Edwards A. Communicating risk through analogies [letter]. British Medical Journal, 2003; 327: 749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Charles C, Gafni A, Whelan T. Shared decision‐making in the medical encounter: what does it mean? (or it takes at least two to tango) Social Science & Medicine, 1997; 44: 681–692. [DOI] [PubMed] [Google Scholar]
- 39. Wright P. Writing and information design of healthcare materials In: Candlin C, Hyland K. (eds) Writing Texts, Processes and Practices. London: Longman, 1999: 85–98. [Google Scholar]
- 40. Schriver K. Dynamics in Document Design. New York/London: John Wiley & Sons, 1997. [Google Scholar]
- 41. Barratt A, Trevena L, Davey HM, McCaffery K. Use of decision aids to support informed choices about screening. British Medical Journal, 2004; 329: 507–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schwartz LM, Woloshin S, Fowler FJ Jr, Welch HG. Enthusiasm for cancer screening in the United States. Journal of American Medical Association, 2004; 291: 71–78. [DOI] [PubMed] [Google Scholar]
- 43. Halliday MAK An Introduction to Functional Grammar, 2nd edn London: Edward Arnold, 1994. [Google Scholar]
- 44. Dixon‐Woods M. Writing wrongs? An analysis of published discourses about the use of patient information leaflets Social Science & Medicine, 2001; 52: 1417–1432. [DOI] [PubMed] [Google Scholar]
- 45. Charles C, Gafni A, Whelan T, O’Brien MA. Cultural influences on the physician‐patient encounter: the case of shared treatment decision‐making. Patient Education and Counseling, 2006; 63: 262–267. [DOI] [PubMed] [Google Scholar]


