Abstract
Objectives To explore patient preferences and acceptability of two forms of larval therapy (‘bagged’ and ‘loose’).
Background Larval therapy is frequently used to treat patients with leg ulcers. However, patient preferences and acceptability of larval therapy when compared with other treatments is not established.
Design A survey of patient preferences between larvae and standard therapy (hydrogel) using randomized allocation of two questionnaires (‘bagged’ or ‘loose’ questionnaire). The questionnaire contained closed and open‐response questions and was administered by a nurse researcher. Open responses enabled exploration of patients’ preferences and the acceptability of larval therapy when compared with a standard treatment. Qualitative data were analysed for thematic content.
Setting and participants Thirty‐five participants, aged 18 years and above, with at least one venous leg ulcer were recruited from a UK Hospital Vascular Outpatients Clinic.
Findings Majority of participants stated that they would consider larval therapy, irrespective of method of containment. Acceptance of therapy was influenced by length of time with (or recurrence of) ulceration, experiences of other treatments, social contact in hospitals and the experiences of others. Visual imagery was a key influence among participants who would refuse larval therapy. Refusal was mostly among older women (aged 70 years or above).
Conclusions Eliciting patient preferences and increasing patient involvement in treatment decisions is an important part of quality improvement and improved health outcomes. These findings have relevance for practitioners offering larval therapy as a treatment option and for the feasibility of clinical trials.
Keywords: larval therapy, patient choice, patient involvement, questionnaire, venous leg ulcers
Background
Venous leg ulcers represent a significant healthcare problem for both patients and health services. Such ulcers impact on many aspects of daily life, with patients reporting pain, impaired sleep, restricted physical activity, reduced ability to work and social isolation as a result of this condition. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 Leg ulceration is a chronic condition, and as such there is a need for long‐term symptom management. 9 In the UK, venous leg ulceration has been estimated to cost the NHS £400 m ($720 m) per year. 10 The effective treatment and management of venous leg ulcers is therefore a high priority for patients, clinicians and health‐care providers.
Larval therapy is frequently used to treat patients with leg ulcers. 11 There is weak experimental evidence that larval treatment effectively debrides leg ulcers. 12 However, there is no evidence that larval therapy makes a difference to patient‐orientated outcomes, such as accelerating the healing of a chronic wound when compared with other treatments. In 2004, the NHS Health Technology Assessment programme commissioned a pragmatic RCT (VenUS II) to assess the clinical and cost effectiveness of larval therapy when compared with standard hydrogel in the treatment of chronic, necrotic, venous or mixed (venous and arterial) aetiology leg ulcers. 13 Larval therapy can be delivered in loose form (larvae are placed directly on the wound) or bagged form (larvae are contained in a small gauze bag placed on the wound). These different formulations might have different patient acceptabilities and potentially different clinical effects. Participants in VenUS II are randomized to one of three trial arms; standard care (hydrogel), loose larvae or bagged larvae.
Trial researchers 13 were keen to ensure that the sample size calculation for the trial was informed by patient‐derived information about the size of a clinically important effect. The trial team also wanted to investigate patient acceptability of the trial treatments because reluctance to try larval therapy would result in poor trial recruitment. Therefore, we undertook a sub‐study to establish whether patient preparedness to try larval therapy is influenced by formulation. We did this by asking potential participants how effective loose and bagged larvae would need to be for them to consider use. We also sought to explore patient acceptability of larval therapy in general terms. Detail of patient preferences related to healing times to inform the sample size calculation is reported elsewhere. 14 This paper presents an analysis of the feelings and thoughts about larval therapy offered by patients during completion of the questionnaire.
Design
We undertook a survey of patient preferences between larvae and standard therapy (hydrogel) using randomized allocation of two questionnaires. 1 Both questionnaires asked about preferences regarding larval therapy compared with standard therapy (hydrogel) for a range of clinical effect. Participants were asked that if hydrogel dressings were to heal their ulcer in 20 weeks, would they consider using larval therapy if it healed their ulcer in 6, 7, 8 weeks and then presented in weekly intervals up to 20 weeks, to determine point of preference. 14 The questionnaire also enabled exploration of patients’ perceptions of larval therapy; participants were asked questions about their leg ulcer (current and past ulceration), their exposure to larval therapy (personally or through contact with others), their occupation (current or previous) and any hobbies which may have involved larvae (such as fishing). In addition, participants were encouraged to offer open comments. A nurse researcher (KS) administered and completed all the questionnaires (see Fig. 1 for questionnaire administration process). This nurse researcher is independent of the VenUS II trial research team. 13
Figure 1.
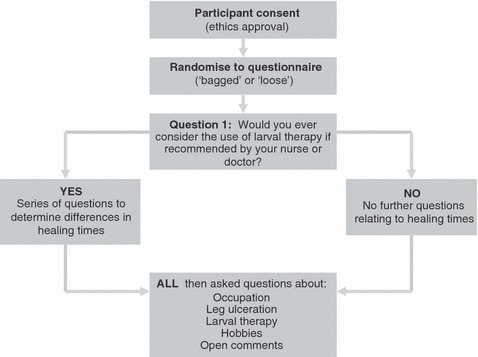
Process of questionnaire administration.
Participants
Participants were patients with leg ulcers, attending a Vascular Clinic in an Outpatients Department of a large teaching hospital in the north of England between December 2004 and March 2005. Forty‐one patients, with at least one leg ulcer of venous or mixed (venous and arterial) aetiology, were approached to take part in the study. Potential participants were provided with study information when arriving for their clinical appointment. Following their clinical consultation, the nurse researcher spent time going through the information sheet and answering any questions or concerns. Participants who consented were interviewed on the same day by the nurse researcher. A few requested time to consider the study information and discuss it with a relative. These participants were followed up at their next clinical appointment. Thirty‐five participants aged 18 years and above agreed to take part; of those who did not consent (three male; three female), they declined because they reported when leaving the clinic that they did not have time (n = 5) or were considered by the research nurse as unable to provide consent because of confusion (n = 1). Eighteen participants were allocated to the ‘bagged’ larvae questionnaire and 17 to the ‘loose’ larvae questionnaire. Table 1 shows the characteristics of the participants. Table 2 provides further data on individual participants and their response to structured questions. These responses have informed the analyses and interpretation of qualitative data.
Table 1.
Mean age, sex and ulcer duration of patients surveyed
| Loose larvae questionnaire | Bagged larvae questionnaire | |
|---|---|---|
| Gender | ||
| Male | 8 | 11 |
| Female | 9 | 7 |
| Mean age of participants, years (SD) | 73.29 (10.09) | 68.56 (12.05) |
| Range, years | 57–93 | 46–92 |
| Mean duration of current ulcer, years (SD) | 3.18 (3.95) | 3.04 (3.1) |
| Range | 2 months–14 years | 3 months–12 years |
Table 2.
Participant responses to structured questions
| Patient ID | Larval therapy questionnaire group | Age (years) | Gender M = male F = female | Would you consider larval therapy if recommended?* | Is this your first leg ulcer? | How many previous leg ulcers have you had? | What is the duration of your current ulcer? (months) | Have you personally experienced larval therapy?† | Do you know someone who has had larval therapy?‡ |
|---|---|---|---|---|---|---|---|---|---|
| M1 | Bagged | 65 | M | √ | × | Multiple§ | 60 | √ | × |
| F2 | Loose | 80 | F | × | √ | 0 | 2 | × | × |
| M3 | Loose | 62 | M | √ | √ | 0 | 17 | × | √ |
| M4 | Bagged | 70 | M | √ | √ | 0 | 18 | √ | × |
| M5 | Loose | 87 | M | √ | × | 1 | 120 | √ | × |
| M6 | Bagged | 74 | M | √ | √ | 0 | 3 | × | × |
| F7 | Loose | 82 | F | × | × | 2 | 168 | × | × |
| F8 | Bagged | 53 | F | √ | × | 2 | 48 | √ | × |
| F9 | Loose | 93 | F | √ | √ | 0 | 30 | × | × |
| M10 | Bagged | 46 | M | √ | √ | 0 | 12 | × | × |
| F11 | Loose | 79 | F | √ | × | 4 | 3 | × | × |
| F12 | Bagged | 73 | F | √ | × | Multiple | 36 | √ | × |
| F13 | Loose | 63 | F | √ | × | Multiple | 18 | × | √ |
| F14 | Loose | 70 | F | × | √ | 0 | 12 | × | √ |
| M15 | Bagged | 61 | M | √ | √ | 0 | 48 | × | × |
| F16 | Loose | 75 | F | × | × | 2 | 60 | × | √ |
| F17 | Loose | 70 | F | √ | × | 1 | 24 | × | × |
| M18 | Bagged | 75 | M | √ | × | 3 | 96 | × | × |
| F19 | Bagged | 60 | F | √ | × | 2 | 6 | √ | √ |
| M20 | Bagged | 52 | M | √ | √ | 0 | 12 | × | × |
| M21 | Loose | 70 | M | √ | × | 8 | 24 | × | √ |
| M22 | Loose | 58 | M | √ | × | 1 | 96 | √ | √ |
| M23 | Bagged | 74 | M | √ | × | 1 | 54 | √ | √ |
| F24 | Bagged | 92 | F | × | × | 1 | 18 | × | × |
| F25 | Bagged | 83 | F | × | × | 1 | 60 | × | √ |
| M26 | Loose | 81 | M | √ | × | 1 | 48 | × | √ |
| M27 | Loose | 57 | M | √ | × | 4 | 3 | √ | × |
| F28 | Bagged | 84 | F | × | √ | 0 | 24 | × | × |
| M29 | Bagged | 57 | M | √ | × | 1 | 4 | × | × |
| M30 | Loose | 69 | M | √ | √ | 0 | 8 | × | × |
| M31 | Bagged | 73 | M | × | √ | 0 | 12 | × | √ |
| M32 | Bagged | 68 | M | √ | × | 1 | 3 | × | × |
| F33 | Loose | 80 | F | √ | × | 1 | 2 | × | √ |
| F34 | Bagged | 74 | F | √ | × | 2 | 12 | × | √ |
| F35 | Loose | 70 | F | √ | × | 8 | 12 | × | √ |
*Would you consider larval therapy if recommended by a professional (doctor or nurse)?
†Prior to research interview had experience of larval therapy because had received treatment.
‡Prior to research interview had experience of larval therapy because knew someone else who had larval therapy.
§Patient not able to state number of leg ulcers other than ‘multiple’.
Data collection and analysis
Qualitative data were recorded by the nurse researcher (KS) during administration of the questionnaire in the form of detailed fieldnotes and verbatim quotes; these quotes were checked for accuracy with patients during the interviews. Fieldnotes are an established method of data collection 15 , 16 and recording ‘situated vocabularies’ provides rich data of how participants describe things and the ways in which they organize their perceptions. 16 This approach for recording the qualitative data generated during questionnaire completion was appropriate and ensured that data offered by the participants could be subjected to detailed and systematic analyses.
Data were analysed for thematic content. As such, the analytic process involved (i) data management, using a spreadsheet to preserve participants with their responses, (ii) descriptive accounts to identify key dimensions and map the range and diversity of participants’ comments about larvae on thematic charts, and (iii) explanatory accounts, to establish patterns of association and conflict in the data, with subsequent exploration of why such patterns may be occurring. 17 Data were analysed by the nurse researcher (KS) in consultation with members of the research team (NC, JD, EP) to enhance rigour, ensure trustworthiness of findings and encourage reflexivity during analysis. 16 Ensuring the processes of data collection and analysis are transparent, alongside providing details of the participants, enables readers to judge the authenticity of our conclusions 18 and the transferability of our findings to other groups of patients. 19
Ethical considerations
Research governance and local ethics committee approval were granted for the study. All participants were given written and verbal explanations of the study’s aims, what would be involved if they agreed to take part, and how the information they provided to questions would be used. Participants were reassured that their decision to take part (or not) in the interview would not affect any aspect of their care. Written consent was gained from all participants and they were reassured of the confidentiality and anonymity of their responses.
Findings
Majority (27/35, 77%) of leg ulcer participants interviewed stated that they would consider the use of larval therapy, irrespective of the method of containment (Fig. 2). The findings are presented under three themes. First, the desire to heal an ulcer which was described by the participants who had experienced larval therapy or who said they would consider larval therapy as a treatment option. Secondly, the power of visual imagery which was described by participants who said they would not consider larval therapy. Finally, a theme which spans all groups (including participants who had experienced larval therapy and those who would and would not consider it) and is concerned with the influence of the stories of others.
Figure 2.
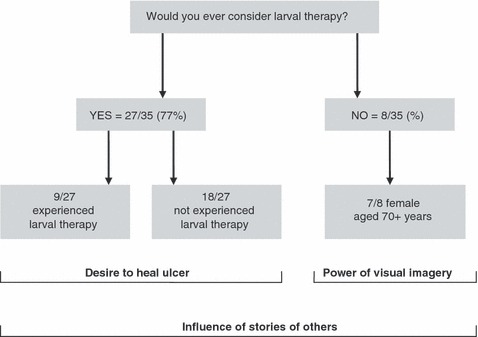
Responses to the question ‘Would you ever consider larval therapy?’.
A desire to heal
Of participants who would consider larval therapy, a third (n = 9) had received some form of larval therapy in the past (Fig. 2). These participants had varied experiences of therapy but commonly associated larval therapy with a desire to heal their ulcer. Two women indicated that when the therapy was offered they were reluctant to accept it because of their negative perceptions of maggots. However, the length of time they had their ulcer (both over 3 years) influenced their decision to accept the larval treatment. Both expressed some reservations about the treatment; one described ‘ putting up with ’ the therapy (F8) and the other ‘ imagined them crawling about ’ (F12). Five participants, all men, described the benefits they had experienced using larval therapy in healing their leg ulcers. All of these patients had experienced their leg ulcer for over 4 years, except one participant (M27) who had only had the current ulcer for 3 months but had an extensive history of leg ulceration (with four previous leg ulcers). These participants described the success of the therapy in healing their leg ulcers and four participants expressed that they had no sensation of the maggots on their wound:
They were brilliant. I couldn’t feel them. They worked and no other treatment had worked. I had a badly infected ulcer and was admitted to hospital. After 9 weeks in hospital, and nothing was working, I was keen to try the maggot therapy. (M27)
Even though one participant had experienced a sensation associated with the larval treatment (described as an itch), he emphasized the positive aspects of treatment in reducing odour and exudate:
I had maggots about 2 years ago. They kept the ulcer cleaner and reduced the smell and infected matter. They felt itchy, I was aware of them moving about. But I was happy that they were getting rid of the infection and the yellowy black gunge. (M22)
Duration of the leg ulcer or repeated incidence of ulcers appears to be related to positive feelings associated with larval therapy. Two patients indicated they had a ‘bad’ experience with larval therapy, experiencing pain and discomfort:
My ulcer healed very well with maggots. On the third night they were very painful. I was in hospital and they gave me oxygen, I was gasping for breath. And I have a high pain threshold. I was told the maggots would be painful but it was very bad. I don’t really want to have them again. (M4)
However, despite these experiences they also commented on the success of the larval therapy for healing. Even though one of these participants commented that he did not want treatment with larval therapy (M4), he contradicted this statement during completion of the questionnaire by indicating that they would consider larval treatment again if their nurse or doctor recommended it.
The perceived benefits of larval treatment (i.e. improved healing, reduced odour and exudate and reduced infection) and professional guidance and recommendation seems to outweigh even negative patient experiences. Many patients experience leg ulcers over long periods of time. Participants in this study indicate that healing times associated with different treatments are therefore very important when making treatment decisions; mean duration of leg ulcers in this study was over 3 years. Participants in this study who would consider larval therapy (n = 27; 77%) indicated that they reached a point in their illness trajectory when they would consider or try any treatment because of their desire to heal the ulcer:
I’m not bothered about the use of maggots, I would try anything that would give the ulcer a chance to heal. Ulcers are the poor relation of the illness family because they are difficult to treat and often not given priority. (M22)
Despite majority of participants expressing a positive feeling towards larval therapy, almost a quarter of participants (8/35, 23%) stated that they would never consider larval therapy; these respondents were distributed equally between those asked about bagged (n = 4) and those about loose (n = 4) larvae. The duration of ulceration for the group that would not consider larval therapy ranged from 2 months to 14 years (mean 3.7 years). Therefore, majority of these participants had also suffered with a leg ulcer for extended periods of time but did not indicate a preference for larval therapy as part of their desire to heal their ulcer. These data were explored for commonalities between the participants who would not consider larval therapy.
The power of visual imagery
Majority of participants who would refuse larval therapy were women (7/8) and were older (aged 70 years or above). Reasons provided for not considering larval therapy were largely related to visual imagery that these participants associated with larvae. Five women expressed that they did not like ‘the thought’ of the maggots. Some comments made include:
The thought of them makes me feel sick. I really don’t want to talk about it. (F25)
I have met people in the clinic who have had maggots. They say they haven’t seen them. I don’t, I don’t like the thought of it. I wouldn’t want them. (F16)
Further explanations of why participants did not like the thought of maggots were offered. One reason related to fear that the maggots might escape from the dressing and how the patient felt and might react to such a situation:
If I had them and woke up with maggots in the bed I would go nuts. (M31)
However, a more common reason was related to a ‘bad’ visual image or memory. It is interesting to note that participants referring to such imagery had previously worked in occupations where maggots may have been associated with poor hygiene practices, decaying food or dirty work. Previous occupations of participants in this group who would not consider larval therapy included cleaners (n = 4), caterers (n = 2) and factory workers (n = 2):
I’ve only seen them on rotten meat. (F16)
You get maggots where there is badness, for example a dead cat. (M31)
This can be contrasted with participants who expressed a positive image of maggots because of their fishing hobby and did not have any fear of handling maggots. All of the participants who went fishing (n = 12) would consider larval therapy.
A further explanation for not wanting to consider larval therapy related to the way in which the therapy was described to patients. Participants reported that they were repulsed by the thought that the larvae would be ‘eating’ their body tissue. When combined with existing successful treatments, these patients felt they did not have to consider such therapies:
The nurses said they put them on to eat tissue. I didn’t want to hear anymore. The thought alone would put me into an early grave. (F14)
I like my current treatment; it’s helping my ulcer to heal and I wouldn’t want to change it. (F24)
However, another important influence on the decision making of patients about ‘novel’ treatment options relates to how they come to understand treatments through the stories of their peers.
The influence of the stories of others
Patients are cared for within a social system and come into contact with others who may be experiencing similar conditions. This study highlighted that the stories shared between patients are important influences on how patients are informed about treatments (n = 14; 40%). Vascular clinics and wards are important areas of influence for patients with leg ulceration. As patients sit in waiting rooms or ward areas they share their histories and stories of care, treatment and management. These stories are also shared in social interactions with friends. These exchanges can have both positive and negative accentuations.
The information transferred between patients relates to sensations associated with the application of larval therapy (ranging from no sensation or a tickle to pain), the success of the treatment (ranging from no success to reduced odour, exudate and slough) and detail of how the maggots are perceived to aid healing (‘eating’ tissue):
A few people at the clinic have told me they’re not painful, although you might feel a tickle. They have said the maggots were marvellous and helped clear up the ulcer. I’m interested in the idea of maggot therapy. (F34)
A lady here at the clinic had them but had to have them taken off they were so itchy and painful. (M26)
I’ve heard from other patients in the clinic that they are good and you can’t feel them. The maggots take away the badness, you see. I wish they had been available when I had my last ulcer because it lasted 12 years. (F33)
A quarter (n = 4) of patients who had discussed larval therapy with other patients were put off considering this treatment option as result of these conversations. Therefore, the clinical environment and the social interactions that patients have with each other may be an important influence and contributing to patients’ decision making and treatment choices.
Discussion
This sub‐study, using a structured questionnaire, aimed to establish whether patient preparedness to try larval therapy is influenced by formulation. When completing the questionnaire, patients offered their perceptions of larval therapy. These data provide useful insights into patient decision making about a treatment whose clinical and cost effectiveness is not yet established.
This study highlights possible gender differences in preferences and acceptability of larval therapy. Majority of participants who would not consider larval therapy were older women. Reluctance to try larval therapy was related to visual imagery as a result of previous experiences with maggots, descriptions of how the therapy works by health‐care professionals and patients’ perceptions of the success of their existing treatments.
Semantic content, previous experience, knowledge representation and decision framing are intricately linked. Experience with a ‘content domain’ (in this case the ‘maggots’ in larval therapy) affects the ways in which a person represents information and by implication the relative attractiveness of different decision options. 20 It is proposed that semantics are an important influence on the choices made by individuals. For example, Plous 21 illustrates how semantics can influence an individual’s choice when presented with the phrases ‘feeling safe’ and ‘feeling safer’. This study reveals that the description ‘eating tissue’ was not liked by some participants. This may have important implications for the ways in which health‐care professionals inform and present information to patients about larval therapy. It is possible that if health‐care professionals rephrase the ways in which they present the potential benefits of larval therapy, for example by emphasizing ‘cleaning tissue’ rather than ‘eating tissue’, then there may be similar scope for influencing patient choice and shared decision making between clinicians and patients. However, caution should be exercised by health‐care professionals to ensure that their choice of language is not inappropriately manipulative. For the purposes of describing larval therapy to patients, health‐care professionals could use patients’ words to reflect patients’ descriptions of the ways in which they perceive larval therapy to promote healing.
Patients in the study, who had experienced larval therapy, described the larvae as reducing odour and exudate from their leg ulcer, reducing infection and improving the healing process. In addition, some patients perceived that larvae reduced pain associated with ulceration. These findings resonate with the findings of two other studies that explored patients’ perceptions and experiences of larval therapy and factors influencing their acceptance of the treatment in the UK 22 and Netherlands. 23 These studies describe reduced symptoms (such as smell and exudate) and the ‘hope’ attached to larval therapy, because of a difficult to heal leg ulcer. This corresponds with the findings of this study and patients’ desire to heal their leg ulcer. However, it should also be noted that some patients in our study associated larval therapy with the negative experiences of pain, discomfort and itching. Therefore, whilst patients expressed a desire to heal their ulcer, the experience of larval therapy has some side‐effects which may not be acceptable to all patients.
It has been noted that nursing staff were viewed as influential in the decision making of patients because they provided the information for patients to make an informed choice about accepting therapy. 22 This is further supported in this study because majority of patients (77%) agreed that they would consider larval therapy if their nurse or doctor recommended the therapy to them. This highlights the important role of health‐care professionals and their ability to provide information in ways which enable shared decision making about treatment decisions. This also raises questions about how the acceptability of larval therapy to health‐care professionals may influence their ability to provide such information and to offer larval therapy.
The studies by Kitching 22 and Steenvorde et al. 23 concentrate on patients who have experienced some form of larval therapy for a chronic or non‐healing wound. This study contributes to the evidence‐base by investigating the acceptability of larval therapy for patients with a chronic wound who have and have not undergone, or even considered, this treatment option. If larval therapy proves to be both clinically and cost effective then it is equally important to establish whether this treatment option and its mode of delivery (‘bagged’ or ‘loose’) is acceptable to a range of patients. Eliciting patient preferences and increasing patient involvement in treatment decisions have become important for health‐care professionals because these are considered an important part of quality improvement and improved health outcomes. 24 , 25 , 26 It is therefore essential to consider patient preferences when considering ‘novel’ treatment interventions and when conducting trials to evaluate the effectiveness of these treatment options.
Social comparison theory 27 proposes that (i) people have a tendency to evaluate their decision choices against social benchmarks; (ii) where objective information is unavailable, people evaluate their decisions, opinions and perspectives by comparing them to the decisions, opinions and perspectives of others; and (iii) when faced with a choice, people prefer to compare themselves with others who are close to them in opinions and abilities. This study highlights the importance of patients’ narratives, ‘war stories’ and evaluations as influences on shaping the perceptions of others. The clinic and wards were described as social spaces in which these exchanges occurred and which could influence patients’ decisions relating to the acceptability of larval therapy. This study did not capture the exchanges between patients treated in the community. A challenge for health‐care professionals will be to understand the importance of these social arenas in shaping patients’ perceptions across multiple health‐care settings and to promote timely information giving to leg ulcer patients that supports their decision making.
Study limitations
It is important to highlight that our study findings should be cautiously interpreted. The main objective of the study was to elicit patient preferences for, and acceptability of, larval therapy to inform the sample size calculation for a clinical trial (VenUS II), 13 with patient‐derived information about the size of a clinically important effect. 14 Qualitative data collection was limited to participants’ open responses to specific questions (relating to their clinical history of leg ulceration, their exposure to larval therapy, their occupation and hobbies) with limited opportunity at the end the questionnaire interview to offer additional comments. In addition, we recognize that interviews using a structured questionnaire may limit the responses provided by patients because of the way in which participants experience the interview. The style of focused questioning may mimic a clinical consultation and so participants may only raise issues which they feel ‘safe’ and appropriate to disclose to the health‐care professional. Therefore, the findings do not represent detailed in‐depth exploration of patients’ views.
A convenience sample was recruited to the study from one Vascular Outpatients Department of a large teaching hospital in the north of England. Therefore, the study does not capture the preferences of patients receiving treatment and care in a range of primary and secondary care settings. There was a high percentage of men (54.3%) recruited to the study; this may not be representative of the population suffering leg ulceration. 28 It was also not possible to recruit patients of minority ethnic origin, because of convenience sampling (i.e. who was in the clinic on particular days) and timescales. The demographics of participants and the clinical setting need to be considered as the context for interpretation of the findings. Despite these limitations, the study provides useful insights which require further discussion. However, it is also important to reiterate that the clinical and cost effectiveness of larval therapy, when compared with standard treatments, for the healing of chronic, necrotic, venous or mixed (venous and arterial) aetiology leg ulcers has not yet been established.
Conclusion
Eliciting patient preferences and increasing patient involvement in treatment decisions is an important part of quality improvement and improved health outcomes. This study highlights that patients do not have a widespread resistance to the idea of using larval therapy for the treatment of leg ulcers, regardless of their method of containment (‘bagged’ or ‘loose’). Patients who were resistant tended to be older women. These findings have relevance for practitioners offering larval therapy as a treatment option and for the feasibility of clinical trials, especially as older women comprise the most prevalent group of leg ulcer patients. Future studies should focus on gathering in‐depth data of patients’ experiences with a wider range of patients (representative of the population who suffer leg ulceration and including patients of minority ethnic origin) and across the variety of clinical settings providing treatment and care for patients. In addition, it would be revealing to understand more about the perceptions that health‐care professionals may have towards larval therapy to understand how they present information about ‘novel’ treatments and what influence this may have on patient decision making. An in‐depth study of staff and patient perceptions is ongoing as part of the Venus II trial and will provide insights into these important areas that currently remain unaddressed. 29
Acknowledgements
The authors wish to thank the participants and staff at the Vascular Clinic. The study was financially supported by a grant from the NHS R&D HTA Programme. The views and opinions expressed do not necessarily reflect those of the Department of Health.
Footnotes
Once participants provided informed written consent they were randomly allocated to receive one of these questionnaires using sealed opaque envelopes which were sequentially numbered.
References
- 1. Phillips T, Stanton B, Provan A, Lew R. A study on the impact of leg ulcers on quality of life: financial, social and psychological implications. Journal of American Academy of Dermatology, 1994; 31: 49–53. [DOI] [PubMed] [Google Scholar]
- 2. Chase SK, Melloni M, Savage A. A forever healing: the lived experience of venous ulcer disease. Journal of Vascular Nursing, 1997; 15: 73–78. [DOI] [PubMed] [Google Scholar]
- 3. Jull A, Walker N, Hackett M et al. Leg ulceration and perceived health. A population based case– control study. Age and Ageing, 2004; 33: 236–241. [DOI] [PubMed] [Google Scholar]
- 4. Hamer C, Cullum NA, Roe BH. Patients’ perceptions of chronic leg ulcers. Journal of Wound Care, 1994; 3: 99–101. [DOI] [PubMed] [Google Scholar]
- 5. Krasner D. Painful venous ulcer: themes and stories about their impact on quality of life. Ostomy/Wound Management, 1998; 44: 38–50. [PubMed] [Google Scholar]
- 6. Walshe C. Living with a venous leg ulcer: a descriptive study of patients’ experiences. Journal of Advanced Nursing, 1995; 22: 1092–1100. [DOI] [PubMed] [Google Scholar]
- 7. Franks PJ, Moffat CJ, Doherty DC, Smithdale R, Martin R. Longer‐term changes in quality of life in chronic leg ulceration. Wound Repair and Regeneration, 2006; 14: 536–541. [DOI] [PubMed] [Google Scholar]
- 8. Persoon A, Heinen MM, Van Der Vleuten CJ, De Rooij MJ, Van Der Kerkhof PCM, Van Achterberg T. Leg ulcers: a review of their impact on daily life. Journal of Clinical Nursing, 2004; 13: 341–354. [DOI] [PubMed] [Google Scholar]
- 9. Briggs M, Flemming K. Living with leg ulceration: a synthesis of qualitative research. Journal of Advanced Nursing, 2007; 59: 319–328. [DOI] [PubMed] [Google Scholar]
- 10. Simon DA, Dix FP, McCollom CN. Management of venous leg ulcers. BMJ, 2004; 328: 1358–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thomas S, Jones M, Wynn K, Fowler T. The current status of maggot therapy in wound healing. British Journal of Nursing, 2001; 10: S5–S12. [DOI] [PubMed] [Google Scholar]
- 12. Wayman J, Nirojogi V, Walker A, Sowinski A, Walker MA. The cost effectiveness of larval therapy in venous ulcers. Journal of Tissue Viability, 2000; 10: 91–94. [DOI] [PubMed] [Google Scholar]
- 13. Raynor P, Dumville J, Cullum N. A new clinical trial of the effect of larval therapy. Journal of Tissue Viability, 2004; 14: 104–105. [DOI] [PubMed] [Google Scholar]
- 14. Petherick ES, O’Meara S, Spilsbury K, Iglesias CP, Nelson EA, Torgerson DJ. Patient acceptability of larval therapy for leg ulcer treatment: a randomised survey to inform the sample size calculation of a randomised trial. BMC Medical Research Methodology, 2006; 6: 43. Available at: http://www.biomedcentral.com/content/pdf/1471‐2288‐6‐43.pdf, accessed on 31 July 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bryman A. Social Research Methods. Oxford: Oxford University Press, 2001. [Google Scholar]
- 16. Hammersley M, Atkinson P. Ethnography: Principles in Practice, 2nd edn London: Routledge, 1995: 175–204. [Google Scholar]
- 17. Ritchie J, Spencer L, O’Connor W. Carrying out qualitative analysis In: Ritchie J, Lewis J. (eds) Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage, 2003: 219–262. [Google Scholar]
- 18. Mays N, Pope C. Quality in qualitative health research In: Pope C, Mays N. (eds) Qualitative Research in Health Care, 2nd edn London: BMJ Books, 2000: 89–101. [Google Scholar]
- 19. Lincoln YS, Guba EG. Naturalistic Inquiry. Beverley Hills, CA: Sage, 1985. [Google Scholar]
- 20. Goldstein WM, Weber EU. Content and discontent: indications and implications of domain specificity in preferential decision making In: Busemeyer JR, Hastie R, Medin DL. (eds) The Psychology of Learning and Motivation (vol 32): Decision Making from a Cognitive Perspective. San Diego: Academic Press, 1995: 83–136. [Google Scholar]
- 21. Plous S. The Psychology of Judgment and Decision Making. New York: McGraw‐Hill, 1993. [Google Scholar]
- 22. Kitching M. Patients’ perceptions and experiences of larval therapy. Journal of Wound Care, 2004; 13: 25–29. [DOI] [PubMed] [Google Scholar]
- 23. Steenvoorde P, Buddingh TJ, Van Engeland A, Oskam J. Maggot therapy and the ‘yuk’ factor: an issue for the patient? Wound Repair and Regeneration, 2005; 13: 350–351. [DOI] [PubMed] [Google Scholar]
- 24. Say RE, Thomson R. The importance of patient preferences in treatment decisions – challenges for doctors. BMJ, 2003; 327: 542–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ryan M, Scott DA, Reeves C et al. Eliciting patient preferences for health care: a systematic review of techniques. Health Technology Assessment, 2001; 5: 5. [DOI] [PubMed] [Google Scholar]
- 26. NHS Management Executive . Local Voices: The Views of Local People in Purchasing for Health. London: NHS Management Executive, 1992. [Google Scholar]
- 27. Festinger L. A theory of social comparison processes. Human Relations, 1954; 7: 117–140. [Google Scholar]
- 28. Graham ID, Harrison MB, Nelson EA, Lorimer K, Fisher A. Prevalence of lower‐limb ulceration: a systematic review of prevalence studies. Advances in Skin & Wound Care, 2003; 16: 305–316. [DOI] [PubMed] [Google Scholar]
- 29. Cullum N. VenUS II: larval therapy venous ulcer study. 2007. Available at: http://www.controlled‐trials.com/ISRCTN55114812, accessed on 31 July 2007.


