Abstract
Objectives Health information is an important resource for patients to understand and engage in the management of their health conditions. We discuss the role of health literacy (HL) in improving patient participation and propose future research in this field.
Methods Literature searches were conducted to review existing definitions and measures of HL and identify empirical findings of its impact on patient health/illness‐related behaviours. We searched MEDLINE using ‘health literacy’ as a keyword and retrieved 371 articles published in English between 1985 and 2006. We also hand‐searched publications of leading researchers and related institutes and followed the reference lists of relevant articles.
Results The World Health Organization has defined HL as ‘the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand, and use information in ways which promote and maintain good health.’ Based on this definition, three levels of HL have been described: functional, communicative and critical. Studies of HL have increased dramatically over the past few years, but there is a gap between the conceptual definition of HL and its application. Thus, empirical evidence of its impact on patient health/illness‐related behaviours is still limited.
Conclusions The prevalence and consequence of inadequate HL as fully defined have not been determined. Further research is needed to develop measures of HL beyond the functional level and that consider the interaction of the individual patient HL with the health and social contexts in which the patient lives.
Keywords: health literacy, information seeking, patient participation, patient–physician communication
Introduction
Health information is an important resource for patients to understand and engage in the management of their health conditions and may also reduce their anxiety and improve their well‐being. Traditionally, it has been suggested that a physician’s ability to control information creates a basic asymmetry in the patient–physician relationship, and professional dominance is grounded in a stratified distribution of technical knowledge. 1 Over the past few decades, however, this traditional model of the patient–physician relationship has gradually shifted toward one involving mutual participation in which patient autonomy is respected and information and decisions are shared between the patient and physician. In particular, with an increase in chronic diseases, patient participation in the health‐care process has been recognized as a critical determinant of successful disease management.
Previous studies have consistently reported that patients want to know information about their diseases. 2 , 3 Although physicians have historically been the primary source for health and medical information, other sources are becoming more available to the general public with the increase in media reports and rapid diffusion of the internet. 4 , 5 , 6 , 7 Thus, patients’ own skills in finding and applying information about health issues may have a substantial impact on their future well‐being. 8
A significant concern is that patients may not be able to understand health information adequately because of limited health literacy (HL), especially in the context of health and medical settings. In these cases, more information may actually cause patients to feel confused and powerless instead of empowering them. Even if patients do not intentionally seek health information, it may be provided by anyone with which they communicate or the media and may have profound impacts on their behaviours and health. 9 The need for improved HL has become apparent as the number of health information sources that are easily accessible by the general public, but of which the quality may not be assured, has increased.
We review existing definitions and measures of HL and empirical findings of its impacts on patient health/illness‐related behaviours. We then discuss the role of HL in improving the participation of patients in their own care and propose future research in this field.
Methods
Literature searches were conducted to identify studies of HL. We searched MEDLINE using ‘health literacy’ as a keyword and retrieved 371 articles published in English between 1985 and 2006: 30 until 1999, 17 in 2000, 26 in 2001, 23 in 2002, 31 in 2003, 61 in 2004, 88 in 2005 and 95 in 2006. We also hand‐searched publications of leading researchers and related institutes and followed the reference lists of relevant articles. Among the retrieved articles, we focused our review on those that defined concepts, developed measures, and/or examined the relationship of HL with patient health/illness‐related behaviours such as information seeking, decision making, self‐management, adherence, and the use of health‐care services.
Concept and definitions
In general, literacy is the ability to read, write and speak the language to compute and solve problems at levels of proficiency necessary to function on the job and in society, achieve one’s goals, and develop one’s knowledge and potential (U.S. Congress, National Literacy Act of 1991, Public Law 102‐73, 1991). The idea of HL is based on this concept of literacy and generally means literacy in the context of health and health care. Given that basic literacy skills are required for HL, it is reasonable to assume that individuals with limited literacy also have limited HL. Indeed, previous studies have reported significant associations between measures of literacy and measures of functional HL such as the REALM and the S‐TOFHLA 10 , 11 On the other hand, it has been noted that even individuals with adequate literacy might not have adequate HL because the literacy demands of the health‐care context is often more complex than that of everyday life. 12 Also, for individuals whose native language is not the national language where they live, HL is affected not only by their literacy in the national language, but also by their literacy and HL in their native language, which makes the relationship between literacy and HL further complex.
Several definitions of HL are currently in use; they share the basic concept of literacy, but vary in scope. The American Medical Association (AMA) first referred to HL as ‘a constellation of skills, including the ability to perform basic reading and numerical tasks required to function in the health‐care environment. Patients with adequate HL can read, understand, and act on health‐care information.’ 13 This is a relatively narrow definition of HL that focuses on patients in health‐care settings and their understanding of the information provided by health‐care providers. This definition has been updated by adopting the most widely used definition proposed by the National Library of Medicine (NLM), 14 which is also cited in Healthy People 2010. It defines HL as ‘the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.’ Unlike the earlier AMA definition, it includes individuals outside of health‐care settings.
Further, the World Health Organization (WHO) has proposed a somewhat broader definition of HL, 15 although it has been less frequently cited in previous studies. According to the WHO, HL is ‘the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand, and use information in ways which promote and maintain good health.’ It also suggests that HL implies the achievement of a level of knowledge, personal skills, and confidence to take action to improve personal and community health by changing personal lifestyles and living conditions, and thus is critical to the empowerment of patients. This definition seems to be distinct from the others in that it focuses not only on a cognitive element of comprehension, analysis, and application of health information to make decisions about one’s health, but also on social skills to interact with other people and society, e.g. communication, negotiation and organization, which are necessary to put decisions into practice. Also, it refers to motivation in addition to ability. Based on this, Nutbeam 16 proposed a model of HL that includes three levels and assumes both individual and population benefits at each level: (i) functional/basic literacy as sufficient basic skills in reading and writing to be able to function effectively in everyday situations, broadly compatible with the narrow definition of HL; (ii) communicative/interactive literacy as more advanced skills to participate in everyday activities actively, to extract information and derive meaning from different forms of communication, and to apply new information to changing circumstances; and (iii) critical literacy as more advanced skills to analyse information critically and use this information to exert greater control over life events and situations.
All of these definitions define HL as a quality of the individual, although Nutbeam 16 referred to the population benefit of improving individuals’ HL. However, it should be noted that HL is based on the interaction of the individual’s skills with the demands of the society in which the individual lives, including health‐care providers, the health‐care system, the media and the community. 12 Thus, an individual’s HL should be defined and assessed in relation to the ability of the society to communicate health information in a manner appropriate to the audience (i.e. the HL of the population).
Measures of health literacy and related concepts
In general, literacy includes a variety of skills beyond reading and writing such as numeracy, listening and speaking, and relies on cultural and conceptual knowledge. 12 Nonetheless, most existing measures of HL have been designed to measure HL at the level of functional HL, rather than the communicative or critical level, 16 focusing predominantly on the skills to read written materials.
Functional health literacy measures
Frequently used measures of functional HL are the Rapid Estimate of Adult Literacy (REALM) 10 , the Test of Functional Health Literacy in Adults (TOFHLA), 11 , and their abbreviated versions, REALM‐R 17 and S‐TOFHLA 18 . In contrast, several HL assessment methods that can be more easily administered to screen limited HL have recently been proposed. Chew et al. 19 proposed brief screening questions to identify patients with inadequate HL, including ‘How often do you have someone help you read hospital materials’, ‘How confident are you filling out medical forms by yourself’ and ‘How often do you have problems learning about your medical condition because of difficulty understanding written information?’ Based on this, the Single Item Literacy Screener (SILS) was developed to identify adults in need of help with printed health material by asking ‘How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?’ 20 Further, Weiss et al. 21 developed the Newest Vital Sign (NVS) as a quick screening test for primary health‐care settings, which consists of a nutrition label accompanied by six questions.
Communicative and critical health literacy measures
We found no validated instrument that has been created to assess communicative or critical HL for adults. However, some of the concepts of communicative and critical HL might have been studied under different labels. 22 For instance, the Perceived Efficacy in Patient–Physician Interactions (PEPPI) was developed to measure a patient’s self‐efficacy at obtaining medical information and attention to their medical concerns from physicians, 23 and the Patient’s Confidence in Communication Scale (PCCS) was created to assess a patient’s ability to list goals, barriers and necessary skills for effective communication with the physician. 24 Also, patient–physician communication studies have identified the communicative skills of patients such as information seeking, information verifying and information provision as indicators of active participation in medical care. 25 These are closely related to Nutbeam’s 16 definition of communicative literacy. Similarly, a patient’s level of confidence in participating in medical decisions 26 may partly reflect her/his critical literacy.
The whole definition of communicative or critical HL, however, is not covered by any of the previously mentioned measures. Their focus is solely on the patient’s ability to communicate with health‐care providers (mainly physicians) and to make decisions in medical settings partly because patient–physician communication in the medical visit has been the most intensively studied area in health communication research. In addition, many of these measures are based on self‐reporting by patients in which patients are asked to rate their confidence or self‐efficacy, rather than their skills or ability, which departs from the definition of HL. In measuring HL based on a patient’s perception, the overlaps with existing constructs such as self‐efficacy and Health Locus of Control should be carefully considered. 22
In contrast, the development of an objective measure for communicative and critical HL could be a more challenging task than that for functional HL. These skills in clinical encounters might be assessed using a coding system applied to recorded communication between the patient and health‐care providers, such as the Roter Interaction Analysis Systems, 27 whereas the skills in other settings, such as seeking and using information from mass media or the internet, may be more difficult to assess. Difficulty also rests in the fact that the skills necessary will vary depending on the demands placed on the patient by the particular health‐care providers, health‐care system and media, as noted earlier. Thus, an HL level that is ‘adequate’ in one situation might not be adequate in another, which is especially true for communicative and critical HL.
Evidence from empirical studies
It has been widely acknowledged that limited literacy is associated with poor health status, even after controlling for potentially confounding sociodemographic variables such as income, education and ethnicity, and other factors. 28 , 29 Previous empirical studies have examined HL in terms of functional HL, or more precisely, reading skills of health information because currently available instruments of HL are designed to assess functional HL, as described above. Thus, the prevalence and consequence of limited HL as fully defined are unknown. Limited HL in terms of the National Adult Literacy Survey (NALS), REALM and TOFHLA has been frequently explored in the US population, 12 whereas there have been fewer studies outside the USA.
Influence of functional health literacy on patient participation in health care
Limited functional HL is acknowledged to have negative impacts on various patient behaviours and health outcomes, including less knowledge of disease management and health‐promoting behaviours, poorer health status, less use of preventive services and a higher rate of hospitalization and emergency services use (for systematic reviews: 12 , 30 ). Here, we mainly summarize the findings related to patients’ health/illness‐related behaviours and participation in the care process.
Information seeking
Numerous studies have reported the association between limited HL and poor knowledge and understanding of one’s health, disease, medications and treatments. 31 , 32 , 33 , 34 A study of HIV patients reported that patients with limited HL were more likely to use their physician as the sole source of HIV information and less likely to request information from other health‐care providers. 35 In communicating with their physician, diabetes patients with inadequate HL rated their physician’s communication lower in the domains of general clarity, explanation of condition, and explanation of the care process than did patients with adequate HL. 36 Further, Weiss et al. 37 suggested that low‐income elderly had poor reading skills and their main source of medical information came from television, rather than written information.
Decision making
Several studies have suggested that lower literacy might be related to a lower desire to participate in health‐care decision making, 38 and more dependence on family/friends or health‐care providers as the final decision makers. 39 , 40 Further, a study of prostate cancer patients reported that prostate cancer knowledge scores varied among participants after participating in a CD‐ROM‐based program for shared decision making. 41 Kim et al. 41 suggested that low literacy might have hindered patient understanding of the shared decision‐making program because lower HL was associated with lower prostate cancer knowledge scores.
Self‐management behaviours and adherence
A study in a preoperative clinic indicated that patients with limited HL were less likely to be adherent to preoperative medication instructions. 42 In contrast, a study of diabetes patients found that the diabetes self‐efficacy score did not differ significantly with the HL level, whereas self‐efficacy was associated with self‐management behaviours. 43
Health‐care service use
Studies of Medicare‐managed care enrolees found that inadequate HL was associated with a higher hospitalization rate 44 and higher emergency room costs, had marginally significant associations with total and inpatient costs, 45 and was associated with a higher rate of emergency department visits, whereas it was not associated with the mean number of visits or the time to a first visit. 46 Also, it was suggested that people with inadequate HL incur higher medical costs and use an inefficient mix of services. 45 On the contrary, preventive services such as cancer screening tests were less used among those with limited HL. 47 , 48
Studies beyond functional health literacy
Although there have been no studies that quantitatively examined the influence of communicative and/or critical HL on patient behaviours, a few qualitative studies have attempted to explore the components of these advanced levels of HL. A study of adolescents explored HL challenges experienced in searching the internet for online health information. 8 They suggested that judging the credibility of information on a website and managing the volume of information were critical HL issues, whereas finding information before consulting a health‐care provider and applying information to their personal concerns as communicative HL issues.
A study of chronic disease patients 49 also explored specific skills related to each of the three HL levels: functional HL included the functional use of basic information and understanding the importance of self‐care; communicative HL included identifying the best sources of information, the ability to seek personally adapted information from a medical team, and the application of knowledge on a daily basis; and critical HL included the ability to assess the quality of information critically and to apply it in various situations. Further, Wang 50 illustrated health education approaches to improve the functional, communicative, and critical HL using a case study of schistosomiasis in China.
Possible pathways between health literacy, patient participation and health
The evidence from previous studies of HL clearly demonstrates that a lack of adequate functional HL contributes to poorer health and well‐being. For future research, theoretical frameworks are necessary to identify mediators between HL and health outcomes 51 that would improve our understanding of the causal effects and mechanisms of HL in relation to health.
Lee et al. 52 proposed a conceptual framework that links HL to health status and health service use that incorporates four intermediate factors as pathways to health outcomes: (i) disease and self‐care knowledge, (ii) health risk behaviour, (iii) preventive care and physician visits and (iv) compliance with medication. Also, the authors proposed that the adverse effects of limited HL on health outcomes would be moderated by the availability of social support.
Although this framework provides a good overview of the possible mediators between HL and health that have been implied in previous research, more specific pathway models are necessary to test it in empirical studies. Further, this framework assumes HL as functional HL at the individual level as has typically been measured by REALM or TOFHLA. For this reason, the concept of social support was required as a moderator between HL and health outcomes. However, some of the moderating effects of social support as examined in their empirical study 53 could be explained within the concept of HL if the HL of the population (community/society) were taken into consideration. A population with higher HL can provide health information in an understandable way for the patient, support healthy decisions, influence social norms, act on social and economic determinants of health and improve community empowerment. 16 Thus, the HL of the population to which an individual belongs would moderate the relationship between an individual patient’s HL and health outcomes, as might social support.
Based on Lee’s 52 framework and previous work as reviewed earlier, we developed a preliminary model with which to investigate possible mechanisms through which a patient’s HL affects their participation in the health‐care process and ultimately their health (Fig. 1). In this model, the HL of the individual patient includes cognitive and social skills at the three levels (i.e. functional, communicative and critical) that determine the motivation and ability of individuals to gain access to, understand, and use information to promote and maintain good health. When the patient has a health problem, adequate HL will help the patient to understand the problem, seek information from various sources, and make informed and shared decisions, which would lead to better treatment adherence and subsequent self‐management. Also, HL may be related to perceived control over one’s health and self‐efficacy to participate in the health‐care process directly, as well as indirectly, via the achieved knowledge and understanding of his/her health condition. The relationships among these variables in the health‐care process box have been frequently studied in previous literature of patient–physician interaction and patient education. 54 Because these are the concepts that have been considered critical to empowerment, exploring their relationships with HL would help in understanding the meaning of HL in relation to previous similar concepts such as self‐efficacy and empowerment.
Figure 1.
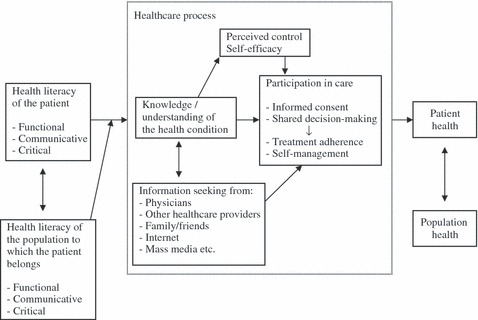
Possible pathways between patient health literacy, participation in the health‐care process and health.
Further, the HL of the individual always interacts with that of the population to which the patient belongs. Higher population HL would not only reduce the demand for individual HL by communicating health information in appropriate ways, but would also moderate the relationship between individual HL and participation in the health‐care process by providing support for patients with lower HL to seek and understand information, make health decisions, and engage in self‐management. Thus, the concept of HL could be a useful link between previous studies on individual patient behaviours within the health‐care process and studies on community and population health.
Future research and practice implications
Studies of HL have increased dramatically over the past few years, but there is still a gap between the conceptual definition of HL and its application. Thus, the empirical evidence of the effect of HL on patient health/illness‐related behaviours and the interconnecting pathways is still limited. The pathway model proposed here is preliminary and should be tested and refined in future empirical studies. Further research is needed, first, to develop measures of HL beyond the functional level to explore the problem with limited communicative and critical HL. Then, the relationships of such HL with patient behaviours and health outcomes should be investigated, incorporating the frameworks of previous studies on patient–physician interaction and patient education. Further, HL of the population should be also considered to explore the interaction of individual patient HL with the health and social contexts in which the patient lives.
Traditionally, prevention and health education have tended to take a high risk approach, which seeks to protect susceptible individuals, 55 such as providing information for diabetes patients or educating HIV patients to adhere to their medication. On the contrary, the introduction of the concept of HL may increase the opportunity for a population approach that seeks to control the causes of incidence, such as eliminating barriers for patients with limited HL to participate in the health‐care process and improving the population HL. Previous interventions have often attempted to decrease specific barriers for patients with limited HL, such as teaching health‐care providers how to communicate better with these patients or developing simple and attractive health education materials at lower reading levels. 56 , 57 , 58 Future interventions should also consider methods of improving people’s HL by improving the system of health education for children and youth at schools, as well as for adults. Improved HL could provide people with the ability and motivation to find a way to solve health‐related problems of their own as well as of the population, which would be used for various health problems they face throughout their lives. This is considered as a process of community empowerment. Although previous studies tended to have a disease‐oriented framework and typically focused on improving individual patient’s HL to achieve a higher level of patient adherence with medical advice, research should be expanded to consider HL within an empowerment paradigm to improve HL at population level and promote health of the population.
Acknowledgements
This study was supported by a Grant‐in‐Aid for Young Scientists (B) from Japanese Ministry of Education, Culture, Sports, Science and Technology.
References
- 1. Freidson E. Professional Dominance: The Social Structure of Medical Care. New York, NY: Atherton Press, 1970. [Google Scholar]
- 2. Benbassat J, Pilpel D, Tidhar M. Patients’ preferences for participation in clinical decision making: a review of published surveys. Behavioral Medicine, 1998; 24: 81–88. [DOI] [PubMed] [Google Scholar]
- 3. Hashimoto H, Fukuhara S. The influence of locus of control on preferences for information and decision making. Patient Education and Counseling, 2004; 55: 236–240. [DOI] [PubMed] [Google Scholar]
- 4. Hesse BW, Nelson DE, Kreps GL et al. Trust and sources of health information: the impact of the internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Archives of Internal Medicine, 2005; 165: 2618–2624. [DOI] [PubMed] [Google Scholar]
- 5. Napoli PM. Consumer use of medical information from electronic and paper media In: Rice RE, Katz JE. (eds) The Internet and Health Communication: Experiences and Expectations. Thousand Oaks, CA: Sage Publications Inc., 2001: 79–98. [Google Scholar]
- 6. Passalacqua R, Caminiti C, Salvagni S et al. Effects of media information on cancer patients’ opinions, feelings, decision‐making process and physician–patient communication. Cancer, 2004; 100: 1077–1084. [DOI] [PubMed] [Google Scholar]
- 7. Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Education and Counseling, 2005; 57: 250–261. [DOI] [PubMed] [Google Scholar]
- 8. Gray NJ, Klein JD, Noyce PR, Sesselberg TS, Cantrill JA. The internet: a window on adolescent health literacy. Journal of Adolescent Health, 2005; 37: 243. [DOI] [PubMed] [Google Scholar]
- 9. Longo DR. Understanding health information, communication, and information seeking of patients and consumers: a comprehensive and integrated model. Health Expectations, 2005; 8: 189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Davis TC, Long SW, Jackson RH et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Family Medicine, 1993; 25: 391–395. [PubMed] [Google Scholar]
- 11. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. Journal of General Internal Medicine, 1995; 10: 537–541. [DOI] [PubMed] [Google Scholar]
- 12. Nielsen‐Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press, 2004. [PubMed] [Google Scholar]
- 13. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association . Health Literacy: Report of the Council on Scientific Affairs. JAMA 1999; 281: 552–557. [PubMed] [Google Scholar]
- 14. Selden CR, Zorn M, Ratzan S, Parker RM. Health Literacy. Current Bibliographies in Medicine. Bethesda, MD: National Library of Medicine, 2000. No.2000‐1. Available at: http://www.nlm.nih.gov/archive/20061214/pubs/cbm/hliteracy.pdf, accessed on 11 April 2008. [Google Scholar]
- 15. Nutbeam D. Health promotion glossary. Health Promotion International, 1998; 13: 349–364. [Google Scholar]
- 16. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 2000; 15: 259–267. [Google Scholar]
- 17. Bass PF, Wilson JF, Griffith CH. A shortened instrument for literacy screening. Journal of General Internal Medicine, 2003; 18: 1036–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Education and Counseling, 1999; 38: 33–42. [DOI] [PubMed] [Google Scholar]
- 19. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine, 2004; 36: 588–594. [PubMed] [Google Scholar]
- 20. Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Family Practice, 2006; 7: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Weiss BD, Mays MZ, Martz W et al. Quick assessment of literacy in primary care: the newest vital sign. Annals of Family Medicine, 2005; 3: 514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tones K. Health literacy: new wine in old bottles? Health Education Research, 2002; 17: 287–290. [DOI] [PubMed] [Google Scholar]
- 23. Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived efficacy in patient–physician interactions (PEPPI): validation of an instrument in older persons. Journal of the American Geriatrics Society, 1998; 46: 889–894. [DOI] [PubMed] [Google Scholar]
- 24. Tran AN, Haidet P, Street RL, O’Malley KJ, Martin F, Ashton CM. Empowering communication: a community‐based intervention for patients. Patient Education and Counseling, 2004; 52: 113–121. [DOI] [PubMed] [Google Scholar]
- 25. Cegala DJ. Patient communication skills training: a review with implications for cancer patients. Patient Education and Counseling, 2003; 50: 91–94. [DOI] [PubMed] [Google Scholar]
- 26. Arora NK, Ayanian JZ, Guadagnoli E. Examining the relationship of patients’ attitudes and beliefs with their self‐reported level of participation in medical decision‐making. Medical Care, 2005; 43: 865–872. [DOI] [PubMed] [Google Scholar]
- 27. Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Education and Counseling, 2002; 46: 243–251. [DOI] [PubMed] [Google Scholar]
- 28. Weiss BD, Hart G, Pust RE. The relationship between literacy and health. Journal of Health Care for the Poor and Underserved, 1991; 1: 351–363. [DOI] [PubMed] [Google Scholar]
- 29. Weiss BD, Hart G, McGee DL, D’Estelle S. Health status of illiterate adults: relation between literacy and health status among persons with low literacy skills. Journal of the American Board of Family Practice, 1992; 5: 257–264. [PubMed] [Google Scholar]
- 30. Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. Journal of General Internal Medicine, 2004; 19: 1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gerber BS, Pagcatipunan M, Smith EV et al. The assessment of diabetes knowledge and self‐efficacy in a diverse population using Rasch measurement. Journal of Applied Measurement, 2006; 7: 55–73. [PubMed] [Google Scholar]
- 32. Guerra CE, Dominguez F, Shea JA. Literacy and knowledge, attitudes, and behavior about colorectal cancer screening. Journal of Health Communication, 2005; 10: 651–663. [DOI] [PubMed] [Google Scholar]
- 33. Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J, Rompa D. Health literacy and health‐related knowledge among persons living with HIV/AIDS. American Journal of Preventive Medicine, 2000; 18: 325–331. [DOI] [PubMed] [Google Scholar]
- 34. Paasche‐Orlow MK, Riekert KA, Bilderback A et al. Tailored education may reduce health literacy disparities in asthma self‐management. American Journal of Respiratory and Critical Care Medicine, 2005; 172: 980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wolf MS, Davis TC, Cross JT, Marin E, Green K, Bennett CL. Health literacy and patient knowledge in a Southern US HIV clinic. International Journal of STD and AIDS, 2004; 15: 747–752. [DOI] [PubMed] [Google Scholar]
- 36. Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician–patient communication among diabetes patients. Patient Education and Counseling, 2004; 52: 315–323. [DOI] [PubMed] [Google Scholar]
- 37. Weiss BD, Reed RL, Kligman EW. Literacy skills and communication methods of low‐income older persons. Patient Education and Counseling, 1995; 25: 109–119. [DOI] [PubMed] [Google Scholar]
- 38. Mancuso CA, Rincon M. Asthma patients’ assessments of health care and medical decision making: the role of health literacy. Journal of Asthma, 2006; 43: 41–44. [DOI] [PubMed] [Google Scholar]
- 39. Collins M, Crowley R, Karlawish JH, Casarett DJ. Are depressed patients more likely to share health care decisions with others? Journal of Palliative Medicine, 2004; 7: 527–532. [DOI] [PubMed] [Google Scholar]
- 40. Barragán M, Hicks G, Williams MV, Franco‐Paredes C, Duffus W, Del Rio C. Low health literacy is associated with HIV test acceptance. Journal of General Internal Medicine, 2005; 20: 422–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kim SP, Knight SJ, Tomori C et al. Health literacy and shared decision making for prostate cancer patients with low socioeconomic status. Cancer Investigation, 2001; 19: 684–691. [DOI] [PubMed] [Google Scholar]
- 42. Chew LD, Bradley KA, Flum DR, Cornia PB, Koepsell TD. The impact of low health literacy on surgical practice. American Journal of Surgery, 2004; 188: 250–253. [DOI] [PubMed] [Google Scholar]
- 43. Sarkar U, Fisher L, Schillinger D. Is self‐efficacy associated with diabetes self‐management across race/ethnicity and health literacy? Diabetes Care, 2006; 29: 823–829. [DOI] [PubMed] [Google Scholar]
- 44. Baker DW, Gazmararian JA, Williams MV et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American Journal of Public Health, 2002; 92: 1278–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. American Journal of Medicine, 2005; 118: 371–377. [DOI] [PubMed] [Google Scholar]
- 46. Baker DW, Gazmararian JA, Williams MV et al. Health literacy and use of outpatient physician services by Medicare managed care enrollees. Journal of General Internal Medicine, 2004; 19: 215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Guerra CE, Krumholz M, Shea JA. Literacy and knowledge, attitudes and behavior about mammography in Latinas. Journal of Health Care for the Poor and Underserved, 2005; 16: 152–166. [DOI] [PubMed] [Google Scholar]
- 48. Garbers S, Chiasson MA. Inadequate functional health literacy in Spanish as a barrier to cervical cancer screening among immigrant Latinas in New York City. Preventing Chronic Disease, 2004; 1: A07. [PMC free article] [PubMed] [Google Scholar]
- 49. Levin‐Zamir D, Peterburg Y. Health literacy in health systems: perspectives on patient self‐management in Israel. Health Promotion International, 2001; 16: 87–94. [DOI] [PubMed] [Google Scholar]
- 50. Wang R. Critical health literacy: a case study from China in schistosomiasis control. Health Promotion International, 2000; 15: 269–274. [Google Scholar]
- 51. Johnston MV, Diab ME, Kim SS, Kirshblum S. Health literacy, morbidity, and quality of life among individuals with spinal cord injury. Journal of Spinal Cord Medicine, 2005; 28: 230–240. [DOI] [PubMed] [Google Scholar]
- 52. Lee SY, Arozullah AM, Cho YI. Health literacy, social support, and health: a research agenda. Social Science and Medicine, 2004; 58: 1309–1321. [DOI] [PubMed] [Google Scholar]
- 53. Arozullah AM, Lee SY, Khan T et al. The roles of low literacy and social support in predicting the preventability of hospital admission. Journal of General Internal Medicine, 2006; 21: 140–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Roter D. The medical visit context of treatment decision‐making and the therapeutic relationship. Health Expectations, 2000; 3: 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Rose G. Sick individuals and sick populations. International Journal of Epidemiology, 1985; 14: 32–38. [DOI] [PubMed] [Google Scholar]
- 56. Gerber BS, Brodsky IG, Lawless KA et al. Implementation and evaluation of a low‐literacy diabetes education computer multimedia application. Diabetes Care, 2005; 28: 1574–1580. [DOI] [PubMed] [Google Scholar]
- 57. Kalichman SC, Cherry J, Cain D. Nurse‐delivered antiretroviral treatment adherence intervention for people with low literacy skills and living with HIV/AIDS. Journal of the Association of Nurses in AIDS Care, 2005; 16: 3–15. [DOI] [PubMed] [Google Scholar]
- 58. Van Servellen G, Nyamathi A, Carpio F et al. Effects of a treatment adherence enhancement program on health literacy, patient–provider relationships, and adherence to HAART among low‐income HIV‐positive Spanish‐speaking Latinos. AIDS Patient Care and STDS, 2005; 19: 745–759. [DOI] [PubMed] [Google Scholar]


