Abstract
Objective To explore information needs and preferences on diagnostic bowel tests and elicit preferences for CT colonography (CTC) vs. colonoscopy (CC).
Background CTC is a new technology for large‐bowel imaging that has been widely assumed to be more acceptable than CC because it is non‐invasive.
Design Semi‐structured focus groups discussing information choices and procedure preferences.
Setting and participants Non‐patient sample of 26 asymptomatic volunteers (mean age 64 years).
Main outcome measures Information choices and CC‐vs.‐CTC preferences were recorded following stepwise presentation of different test attributes. Qualitative thematic analysis was used to examine transcripts of group discussions.
Results On the basis of minimal information about the two tests, a majority of participants preferred CTC to CC (65% vs. 11%), while 24% had no preference. However, once they had received information on all aspects, this was reversed, with 80% of participants preferring CC compared with 8% preferring CTC. Thematic analysis of the discussion showed that participants almost unanimously considered information about test sensitivity to be the most important feature, and perceived relatively modest differences in test sensitivity to be highly significant. Information about risks and side‐effects was considered to be the second most important aspect and attracted questions about risks of bowel perforation and health consequences following exposure to radiation.
Conclusions Patients place high value on quality rather than comfort for medical investigations. This has important implications for the development of educational materials supporting informed choice as well as future directions in refinement of CTC technology.
Keywords: decision making, diagnostic bowel testing, information needs, information preferences, informed choice, patient involvement
Introduction
For over a decade, there has been interest in the clinical and economic viability of CT colonography (CTC) for both screening for colorectal cancer and investigating patients with symptoms suggestive of colorectal cancer. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 The technology is now being disseminated widely as part of routine clinical services, but continues to attract research interest. 11
Much of the attraction of CTC is related to the belief that patients find it more acceptable than standard diagnostic alternatives such as colonoscopy (CC) and barium enema (BE). For example, in a case‐series of patients undergoing CTC together with either CC (n = 696) or BE (n = 617), CTC was preferred to CC by 72% of patients and to BE by 97%. 7 A questionnaire study of 1233 individuals undergoing same‐day CTC and CC found that CTC was thought to be most convenient by 68% of responders, and was also preferred for future screening, with more than 90% describing their experience with CTC as excellent (41%), very good (33%) or good (18%). 4
These and other studies have demonstrated the potential value of CTC as an alternative bowel test modality. However, as patient preferences in these studies were assessed after patients had experienced both tests, decisions about future preferences may have been dominated by past experience rather than consideration of the characteristics of the tests such as sensitivity or associated risks. As such, these findings may be limited in their ability to predict test preferences in advance of the test following informed and shared decision making.
The study of shared and informed decision making in the context of bowel cancer has predominantly concerned decisions about options available for screening in asymptomatic patients. The modalities that have been appraised in this way have included Faecal Occult Blood Testing, Flexible Sigmoidoscopy, CC and only recently CTC. 12 , 13 , 14 , 15 , 16 These studies have identified substantial variation in patient preferences for screening modality and also suggest that the identification and ordering of key attributes of different screening options is central to weighing up multiple dimensions when choosing a screening test. 15
The emphasis on screening reflects the recommendations by the UK General Medical Council and the American College of Physicians for patient involvement in decision making, which only make explicit reference to screening tests with no consideration of diagnostic tests. 17 , 18 However, Davey and colleagues have pointed out that informed and shared decision making should also be encouraged in the context of appraising test options for symptomatic patients. 19
Currently, little is known about how patients choose between different options for diagnostic bowel testing and how these choices are guided by priorities for different test features. The literature on screening does, however, indicate that participants value not only the aspects of the test that are likely to influence their experience of it (also known as ‘process’ features) but also the quality of the test (so‐called ‘outcome’ features). 12 , 13 , 14 , 20 These findings are important because studies of patient preferences between diagnostic bowel test modalities, particularly those involving CTC, have typically only captured patient satisfaction with process and have rarely addressed outcome features. This over‐emphasis on process in patient appraisal of CTC may give a limited perspective on patients’ preferences. An understanding of the full range of determinants of patient preferences will benefit clinicians and policy makers who are considering the benefits of introducing novel investigative techniques and increasing the options available to patients undergoing diagnostic bowel testing.
The focus of the present study was on bowel tests in the diagnostic (not screening) context. For this purpose, we examined preferences for two diagnostic tests (CC and CTC). Information about the tests was provided as part of an in‐depth, focus group study using a non‐patient sample of men and women in the age group (over 50) where bowel investigations are fairly common. We decided to use a non‐patient sample because decisions about whether to undergo a diagnostic test are usually the entry point to the health system and may reflect concerns that differ from those influencing satisfaction once patients have entered this system. 21
The aims of this study were: (i) to explore perceptions of the importance of various features of diagnostic bowel cancer tests, (ii) to elicit comments, concerns and queries on specific test features, and (iii) to monitor test preferences in response to comprehensive information.
Methods
Participants
With approval from the local ethics committee, 26 asymptomatic volunteers (16 men, 10 women) were recruited to participate in one of seven focus groups. They were recruited from the Health Behaviour Research Centre Participant Panel, the University of the Third Age (U3A) and poster advertisements in public libraries. Participants received £20 to cover travel costs and a modest reimbursement for their time.
Procedure
Focus groups were carried out between May and July 2007 in a university‐based conference room. Each group was scheduled to last approximately 2 h and was moderated by one of the authors (CVW). Group discussions were guided by a semi‐structured topic guide. Information was presented in a stepwise fashion using a powerpoint presentation projected onto the wall of the meeting room. Each participant completed demographic questions (age, ethnicity and education) and preference judgements in a written format.
Topic guide development
The topic guide was developed using the literature on informed decision making and information needs in the context of mammography testing. 19 Content covering key facts about CTC and CC was reviewed by a radiologist with experience of CTC in both clinical and research settings (SH). Researchers with experience of focus group design, who were not directly involved in the study, took part in a pilot focus group.
Introduction to the tests
The moderator introduced the two tests that were the target of this study with a picture of a CT scanner and a graphical illustration of CC that had been published by the National Cancer Institute 22 . Once participants had seen the picture, the moderator gave them the following instruction: ‘Based on what you have been told so far, if your doctor recommended you to have one of the two tests and you could choose between them, which of the two tests would you prefer?’ Participants responded by choosing one of four response options: (i) I would not have either test, (ii) I have no preference and would have either; (iii) I would prefer CC (iv) I would prefer CTC.
The moderator then presented a list of topics covering in‐depth information on relevant test characteristics including practicalities, outcomes and results, test sensitivity, and risks and side‐effects. Participants were asked which topics they considered to be most important and to rank the remaining topics in order of most to least important.
Test information provision
The moderator then presented detailed information about CC and CTC to further explore test preferences. Table 1 summarizes key information from each of the four sections. In the section on practicalities, participants were shown slides illustrating the tests and their administration. Key differences between the tests that were mentioned included that CTC does not require sedation, is quicker and may avoid bowel preparation. Slides on outcomes and results covered information about how each test would detect and deal with abnormalities. In contrast to CC, CTC generates reconstructed 2D and 3D imagery of the bowel, which includes images outside the colon but does not allow immediate removal of abnormal growths. Information on test sensitivity was presented in both numerical and graphical formats (using an icon display, see Fig. 1) and stated that sensitivity for detecting abnormal growths was lower for CTC than CC. Finally, participants received information about the risks and side‐effects using the same combination of numerical and graphical information as for the communication of test sensitivity. The information stated that while both tests caused mild discomfort, CTC was less likely to cause injury to the bowel but contained a potential risk of radiation‐induced cancer. At the end of each section, participants were asked to make a preference judgement on the basis of the information they had just received. At the end of the entire presentation, they were asked to provide a final preference judgement on the basis of all the information presented during the sessions.
Table 1.
Summary table of test attributes provided during discussion groups
| CC | CTC | |
|---|---|---|
| Practicalities | ||
| Bowel preparation | Full bowel cleansing | Full bowel cleansing or iodine‐based contrast liquid |
| Sedation | Yes | No |
| Length of procedure | 1–2 h | 20–30 min |
| Outcomes and results | ||
| Image type | Real‐time unprocessed imagery | Reconstructed 2D–3D imagery |
| Able to take biopsies | Yes | No |
| Detects problems outside the colon | No | Yes |
| Test sensitivity | ||
| Small polyps | 75 out of 100 | 60 out of 100 |
| Large polyps | 95 out of 100 | 90 out of 100 |
| Risks and side‐effects | ||
| Discomfort | Mild | Mild |
| Heavy bleeding | 1 in 330 | No |
| Perforation | 1 in 800 | 1 in 3300 |
| Radiation‐induced cancer fatality | None | 1 in 4000 (for a 50‐year‐old person) |
Figure 1.
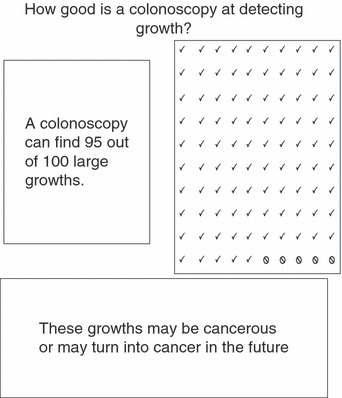
An example of numerical and graphical illustration of test sensitivity.
Analysis
Preference data were recorded in an SPSS v.14 (SPSS Inc., Chicago, IL, USA) spreadsheet and analysed using frequency counts. Focus groups were tape‐recorded and transcribed and analysed using Framework Analysis. 23 The thematic framework followed the focus group schedule outlined above with themes organized within four areas: practical issues, outcomes and results, test sensitivity, and risks and side‐effects. One of the authors (CVW) summarized data in a matrix with rows for individual focus groups and columns for themes. Two authors (SH, JW) reviewed the analysis and guided selection of quotes representing different themes.
Results
Sample
Participants (n = 26) were on an average 64 years old and predominantly white, 62% were male and 80% had a university degree. They were seen in seven groups: one female‐only, two male‐only and four mixed‐gender.
Medical background
The majority of participants had no personal experience of diagnostic bowel testing, but two had experienced a BE and four a CC. Two participants had taken part in a routine surveillance programme as a result of a family history of bowel cancer and two had been diagnosed with cancer (one prostate, one undisclosed).
Information preferences
On the basis of minimal information consisting only of two pictures depicting the concepts of CC and CT scanning, participants were asked to rank the importance of each of the four domains of information. Table 2 indicates a clear hierarchy of preferences. Information about the sensitivity of the tests was considered to be most important (ranked top by 67%), followed by risk (ranked top by 25%). Very few participants identified outcomes and results (ranked top by 4%) or practicalities (ranked top by 4%) to be the most important.
Table 2.
Ranking of the importance of the different information domains
| Sensitivity | 67% voted this the most important; 96% voted it in the top two |
| Risks | 25% voted this the most important; 67% voted it in the top two |
| Outcomes | 4% voted this the most important; 29% voted it in the top two |
| Practical issues | 4% voted this the most important; 8% voted it in the top two |
Two participants did not provide information preferences (n = 24).
Test preferences
Initial test preference
On the basis of minimal information, the majority of participants expressed a preference for CTC (65%), 12% preferred CC and 23% declared no preference (see Table 3). Participants described their initial impressions of CTC as less invasive and less effort, as in this case: ‘I would go for the colonography, because I like the idea of lying down, and being non‐invasive but I am not that bothered’ (Group 5, male, 61). However, there were negative features associated with CTC. Several participants described themselves as ‘claustrophobic’, and enquired whether they would have to lie ‘head first’ inside the scanner and expressed concern about being enclosed for a long period of time.
Table 3.
An overview of test preferences during the focus groups
| Introduction to the tests | Information provision | Final test judgement | ||||
|---|---|---|---|---|---|---|
| Preference after introduction to the test section1 | Preference after practicalities information1 | Preference after outcomes and results information1 | Preference after test sensitivity information1 | Preference after risks and side‐effects information2 | Preference after information about all test aspects1 | |
| CC | 3 (11.5) | 2 (7.7) | 15 (57.7) | 23 (88.5) | 4 (16.7) | 21 (80.8) |
| CTC | 17 (65.4) | 16 (61.5) | 4 (15.4) | 2 (7.7) | 16 (66.7) | 2 (7.7) |
| No preference | 6 (23.1) | 8 (30.8) | 7 (26.9) | 1 (3.8) | 4 (16.7) | 3 (11.5) |
Values refer to number of participants, percentages in brackets.
1 n = 26, 2 n = 24.
Responses to information on practicalities
Following information about practical issues, 61% of participants preferred CTC over CC, 32% had no preference and 8% would choose CC. In their open comments, participants reaffirmed their impression that CTC offered advantages over CC in terms of the procedure; specifically the absence of sedation with CT scanning was perceived as allowing a greater degree of independence.
Despite participants who had previously undergone CC reporting on the unpleasantness of bowel preparation, the potential to avoid bowel preparation with a CT scan did not attract much interest. In fact, some participants were quite positive about the value of bowel preparation for test sensitivity, e.g. ‘I suppose it makes good sense to clear the gut out and get that out of the way’ (Group 5, male, 61).
Responses to information on outcomes and results
The repercussions of detecting abnormalities during the tests were addressed as part of this information section. Following this, fewer people (15%) said that they would choose CTC, while 58% would choose CC and 27% had no preference. The majority of participants were put off by the fact that a subsequent CC would be necessary to remove polyps detected during CTC. Indeed, several participants reported that while the procedure itself may be quicker than CC, having CTC could potentially delay diagnosis and treatment: ‘Well, you could put it the other way round with a CT, the good news is, we have a good picture, the bad news is we think it is a polyp; the good news is it might be benign, the bad news is you have to come back in three weeks time for another thing. You went nowhere and instead of having a three week period you have now an eight week period’ (Group 2, male, 58).
Several participants made favourable comments about CTC’s ability to detect problems outside the colon, which one participant likened to an ‘MOT’ (a car safety check in the UK). However, the absence of a clear demarcation of organs included in a CTC was considered to be problematic: ‘(…) Maybe I would prefer a test that would actually look at the liver, the kidneys (...). It just depends on whether they actually look at the scans’ (Group 2, male, 62).
Several participants were also concerned that CTC could lead to diagnosing unrelated and benign conditions, or serious conditions for which there may be no cure and no benefit of earlier diagnosis, e.g. ‘(...) you pick up things that are completely benign, you could end up not knowing whether you investigate it further (…)’ (Group 4, female, 63).
Responses to information on test sensitivity
Two‐thirds of participants had identified information about sensitivity as the most important feature when deciding between the tests. This was confirmed as soon as they were given the information that CC had slightly higher sensitivity than CTC, when almost 90% of participants preferred CC, while less than 10% preferred CTC. They commented that they had expected CTC – as the more recent development – to be technologically superior and therefore more sensitive, and they expressed disappointment that this was not borne out by statistics: ‘I am frankly surprised, I thought the colonography would pick up much more because first the colonoscopy is purely visual and here (CTC) you have got the whole focus of science, you have electron microscopes. I don't know how powerful these scanning devices are, but I would have thought it could pick up the smallest deviation in cell structure, if necessary, so why? ' (Group 6, male, 67).
It was apparent that most participants perceived the difference in detection rates of large polyps (CC: 95% vs. CTC: 90%) to be highly significant, particularly because, as one participant put it, ‘you might be one of the 5% that gets missed’ (Group 1, female, 62). Only two participants perceived the difference to be less significant, because they believed it to be unlikely that someone would only have one polyp, and therefore the follow‐up CC would be able to detect and deal with the rest.
Responses to information on risks and side‐effects
Table 3 illustrates the shift in preferences caused by information on risks and side‐effects, with 66% of participants preferring CTC, 17% preferring CC and 17% having no preference after hearing about the risks. In the open discussion, participants concentrated on risk of physical injury and the issue of radiation. The risk of bowel perforation was perceived as the most serious risk associated with either test. Participants agreed that neither test was ‘high risk’, but they felt that there was a higher risk of perforation with CC than with CTC: ‘The risk of the tear seems significantly higher, I mean still small, but significantly higher’ (Group 3, male, 61).
Several participants mentioned concerns about radiation‐induced disease when they initially considered the idea of CT scanning, and as part of the risk information, the moderator presented specific information on radiation‐induced cancer. In this respect, CT scanning was seen as presenting patients with a life‐threatening risk, albeit very small, while the other test was not. However, participants also noted that the risk reduced with age and that it would take decades for radiation‐induced cancer to develop. Most therefore concluded that the risk of radiation would be acceptable for people over the age of 60.
Final preference
The final preference (on the basis of all information presented) clearly reflected the importance assigned to information about test sensitivity, with over 80% of participants choosing CC on the basis of its greater sensitivity, while only 8% remained in favour of CTC and 12% had no preference.
It is important to note from the open discussion that there was a consensus in all groups that both tests were acceptable and none would refuse a CTC if it was recommended or was the only test available at the time. Participants appreciated several aspects of the non‐invasive approaches to diagnostic investigations, particularly in terms of avoiding sedation and associated complications. However, they clearly made test sensitivity their top priority in a diagnostic test, and because most participants were not satisfied with the sensitivity of CTC, CC was considered to be the test of choice: ‘I suppose accuracy is the overriding theme apart from that on everything else I would have gone for CT but that overrides everything’ (Group 3, male, 61).
Discussion
The aim of this study was to explore responses to information about two different diagnostic bowel tests. Specifically, participants were able to describe how much they valued different pieces of information and to use these to establish a preference between CC and CTC.
With regard to the order of importance of information about test features, these are in line with findings reported in bowel cancer screening preferences. 12 , 13 , 14 The fact that the majority of participants reported a preference for information about sensitivity and risks indicated that they emphasized outcome features rather than process features in choosing between diagnostic bowel tests.
The results of test preferences demonstrated that the non‐invasiveness of CTC was valued as demonstrated by the majority of participants initially preferring it over CC. This initial enthusiasm was only qualified by concerns about ‘lying inside a tube’. Information on practicalities, the only section dealing with ‘process’ features of the test, substantiated the preference for CTC which was perceived as physically less demanding and offering a greater degree of independence after the test. The potential to avoid bowel preparation with CTC received an unexpectedly critical response and was considered to impede diagnostic quality. This is an important observation, because this feature has been highlighted as one of the most promising aspects of this new technology. 24
Discussion of outcomes and results produced a dramatic shift in preferences between the two tests, because the inability to take biopsies was perceived as a significant drawback for CTC. Similarly, participants also expressed concern over how much attention radiologists would allocate to the examination of extra‐colonic areas. Participants also valued information about the risks and side‐effects. The risk of perforation was seen as higher with CC, but the majority did not regard this as a major drawback. There was also considerable concern about radiation exposure, which was somewhat mitigated by information about the time scale necessary to develop radiation‐induced cancers.
Perhaps the most noteworthy observation in this study is that although we presented an optimistic estimate of sensitivity for CTC (compared with more conservative estimates suggested elsewhwere 25 , 26 ), participants nonetheless took exception to the relatively modest difference in the detection rate of large polyps (CC: 95% vs. CTC: 90%). The strong response to information about test sensitivity was in line with previous research demonstrating that health‐care users assume that medical tests always provide a definitive answer, and any information to the contrary has a profound impact on preferences. 19
Overall, we would like to draw attention to two implications of this study for public health specialists and health‐care providers interested in public/patient participation in health care. Firstly, a responsible approach to communicating both strength and weaknesses of new health‐care technologies is becoming increasingly important with the growing number of developments in diagnostic and screening technology. CTC, in this respect, is only one example where initial enthusiasm for a ‘new’ health technology may be tempered by information about its effectiveness. Second, this study demonstrated the value of informed and shared decision making which allows health‐care users to weigh up information about multiple test features and to impose their own priorities when choosing between different diagnostic test options.
The results of this study have to be interpreted with some caution. To begin with, these data were from a relatively small set of well‐educated individuals, making it necessary to replicate the findings in a larger‐scale survey to assess the extent to which the concerns raised in these focus groups generalize to a wider spectrum of the population. Another limitation was the omission of information about test specificity and the failure to explicitly address the concept of false positives. This would have been very relevant to our information about extra‐colonic findings. Finally, caution is needed in extrapolating these findings to other patient groups such as those undergoing CC or CTC as part of routine bowel cancer screening, because they may hold different beliefs about the relative importance of process and outcome associated with these tests.
Conclusions
This series of focus groups is the first to assess responses to comprehensive information about the two most promising modalities for diagnostic bowel testing. Results highlight the risk of under‐estimating the value patients place on the quality rather than the comfort of these investigations. Future research developing a more comprehensive and sophisticated model of the values associated with CTC could guide efforts to improve this relatively new health technology, and optimize its potential to increase compliance with testing in both diagnostic and screening contexts.
References
- 1. Pickhardt PJ, Hassan C, Laghi A, Zullo A, Kim DH, Morini S. Cost‐effectiveness of colorectal cancer screening with computed tomography colonography: the impact of not reporting diminutive lesions. Cancer, 2007; 109: 2213–2221. [DOI] [PubMed] [Google Scholar]
- 2. Taylor SA, Halligan S, Saunders BP, Bassett P, Vance M, Bartram CI. Acceptance by patients of multidetector CT colonography compared with barium enema examinations, flexible sigmoidoscopy, and colonoscopy. AJR American Journal of Roentgenology, 2003; 181: 913–921. [DOI] [PubMed] [Google Scholar]
- 3. Taylor SA, Halligan S, Bartram CI. CT colonography: methods, pathology and pitfalls. Clinical Radiology, 2003; 58: 179–190. [DOI] [PubMed] [Google Scholar]
- 4. Ristvedt SL, McFarland EG, Weinstock LB, Thyssen EP. Patient preferences for CT colonography, conventional colonoscopy, and bowel preparation. American Journal of Gastroenterology, 2003; 98: 578–585. [DOI] [PubMed] [Google Scholar]
- 5. Burling D, Taylor S, Halligan S. Computerized tomography colonography. Expert Review of Anticancer Therapy, 2004; 4: 615–625. [DOI] [PubMed] [Google Scholar]
- 6. Halligan S, Fenlon HM. Virtual colonoscopy. British Medical Journal, 1999; 319: 1249–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pickhardt PJ, Choi JR, Hwang I et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. New England Journal of Medicine, 2003; 349: 2191–2200. [DOI] [PubMed] [Google Scholar]
- 8. Von Wagner C, Knight K, Halligan S et al. Patient experiences of colonoscopy, barium enema and CT colonography: a qualitative study. British Journal of Radiology, 2009; 82: 13–19. [DOI] [PubMed] [Google Scholar]
- 9. Xiong T, McEvoy K, Morton DG, Halligan S, Lilford RJ. Resources and costs associated with incidental extracolonic findings from CT colonogaphy: a study in a symptomatic population. British Journal of Radiology, 2006; 79: 948–961. [DOI] [PubMed] [Google Scholar]
- 10. Khan KY, Xiong T, McCafferty I et al. Frequency and impact of extracolonic findings detected at computed tomographic colonography in a symptomatic population. British Journal of Surgery, 2007; 94: 355–361. [DOI] [PubMed] [Google Scholar]
- 11. Burling D, Halligan S, Taylor SA, Usiskin S, Bartram CI. CT colonography practice in the UK: a national survey. Clinical Radiology, 2004; 59: 39–43. [DOI] [PubMed] [Google Scholar]
- 12. Schroy PC III, Lal S, Glick JT, Robinson PA, Zamor P, Heeren TC. Patient preferences for colorectal cancer screening: how does stool DNA testing fare? American Journal of Managed Care, 2007; 13: 393–400. [PubMed] [Google Scholar]
- 13. Ling BS, Moskowitz MA, Wachs D, Pearson B, Schroy PC. Attitudes toward colorectal cancer screening tests. Journal of General Internal Medicine, 2001; 16: 822–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pignone M, Bucholtz D, Harris R. Patient preferences for colon cancer screening. Journal of General Internal Medicine, 1999; 14: 432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Marshall DA, Johnson FR, Phillips KA, Marshall JK, Thabane L, Kulin NA. Measuring patient preferences for colorectal cancer screening using a choice‐format survey. Value in Health, 2007; 10: 415–430. [DOI] [PubMed] [Google Scholar]
- 16. Phillips KA, Van BS, Marshall D, Walsh J, Thabane L. A review of studies examining stated preferences for cancer screening. Preventing Chronic Disease, 2006; 3: A75. [PMC free article] [PubMed] [Google Scholar]
- 17. American College of Physicians . Clinical guideline part III: screening for prostate cancer. Annals of Internal Medicine, 1997; 126: 480–484. [PubMed] [Google Scholar]
- 18. General Medical Council . Seeking Patients’ Consent: The Ethical Considerations. London: General Medical Council, 1998. [Google Scholar]
- 19. Davey HM, Lim J, Butow PN, Barratt AL, Houssami N, Higginson R. Consumer information materials for diagnostic breast tests: women’s views on information and their understanding of test results. Health Expectations, 2003; 6: 298–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pignone M. Patient preferences for colon cancer screening: the role of out‐of‐pocket costs. American Journal of Managed Care, 2007; 13: 390–391. [PubMed] [Google Scholar]
- 21. Davey HM, Barratt AL, Davey E et al. Medical tests: women’s reported and preferred decision‐making roles and preferences for information on benefits, side‐effects and false results. Health Expectations, 2002; 5: 330–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Cancer Institute . Colonoscopy. Available at: URL: http://www.cancer.gov/images/cdr/live/CDR415504, accessed on 26 February 2007.
- 23. Richie J, Spencer L, O’Connor W. Carrying out qualitative analysis In: Ritchie J, Lewis J. (eds) Qualitative Research Practice. London: Sage Publications, 2003: 219–262. [Google Scholar]
- 24. Thomeer M, Bielen D, Vanbeckevoort D et al. Patient acceptance for CT colonography: what is the real issue? European Journal of Radiology, 2002; 12: 1410–1415. [DOI] [PubMed] [Google Scholar]
- 25. Cotton PB, Durkalski VL, Pineau BC et al. Computed tomographic colonography (virtual colonoscopy): a multicenter comparison with standard colonoscopy for detection of colorectal neoplasia. Journal of American Medical Association, 2004; 291: 1713–1719. [DOI] [PubMed] [Google Scholar]
- 26. Rockey DC, Paulson E, Niedzwiecki D et al. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet, 2005; 365: 305–311. [DOI] [PubMed] [Google Scholar]


