Abstract
Objectives To revise and improve an existing scale to measure health practitioners’ attitudes to partnership in medicine taking and to ascertain the views of medical students, nursing students and pre‐registration pharmacists on concordance.
Background The traditional model of the practitioner‐patient interaction incorporates a practitioner‐centred approach, focusing on the disease rather than the patient. The philosophy of ‘concordance’ (or ‘partnership in medicine‐taking’) puts the patient at the centre of the interaction, with the patient interacting reciprocally with the practitioner. The Leeds Attitude to Concordance (LATCon) scale was developed in 2001 to assess practitioners’ and patients’ attitudes to concordance. However, thinking on concordance has developed since then and the present study aimed to revise the scale to ensure that it reflected current thinking and also to increase its reliability and validity.
Design A pool of potential items was developed and sent to three subject experts for opinion. An attitudinal Likert scale of 31 items was developed. Its completion was followed by statistical item reduction to 20 items. The shorter scale was completed by the same participants 4–6 weeks later.
Setting and participants The study was set in a university in the UK. Participants were 183 medical students, nursing students, and pre‐registration pharmacists.
Results and discussion The study derived a 20 item scale, including five negatively‐worded items, with good levels of internal and test‐retest reliability. Factor analysis suggested five main factors. A statistically significant difference in attitudes was found between student nurses and medical students, and student nurses and pre‐registration pharmacists, with student nurses being more in agreement with the concordant approach. Overall, participants were in agreement with the concordant approach to medicine taking.
The UK National Health Service advocates partnership in medical care and is encouraging both practitioners and patients to work to introduce this. There is increased awareness of the patients’ perspective by practitioners, but its impact on their practice remains unclear. Education and skills teaching must continue for the benefits of a concordant approach to be seen. The LATCon scale could play a useful role in education and training, and in research assessing the movement towards the new approach.
Keywords: adherence, concordance, medicines, partnership, practitioners
Introduction
The benefit to be gained from prescribed medicines depends as much on the patient’s behaviour as it does on the medicine itself. Yet only about half of patients with chronic diseases in the developed world take their medicines as prescribed. 1 Of the £10 billion annual drug bill of the UK National Health Service, 2 patients return medicines worth around £230 million to pharmacies for disposal and they probably dispose of a greater amount themselves. 3 Non‐adherence is a major global health problem and ‘the benefits from (self‐administered medical) treatments are diminished according to the degree of non‐adherence and the efficacy of the treatments’ (p. 14). 4 As many patients are not following prescription guidance, new strategies have to be developed to improve the efficacy and delivery of health care.
The term ‘adherence’ infers that the patient is free to choose whether or not to follow the practitioner’s guidelines, as well as emphasizing the need for agreement in decision‐making. 5 Patients may wish to ‘understand why they should take a medicine, what potential harm they might face, and how they might integrate medicine taking into the pattern of their life, beliefs, and attitudes’ (p. 133). 6 Reasons for non‐adherence differ greatly between individuals, illness and demographic groups, so improving adherence requires tailoring of clinical management decisions to meet individual patients’ needs. 7 The shift towards the concept of concordance (or ‘partnership in medicine‐taking’) indicates that health practitioners and politicians are starting to acknowledge that patients can make reasoned decisions about their own health care. 8 , 9
The model of concordance was originally conceived to counteract the traditionally passive and submissive nature of patients’ roles in consultations. In concordance, patients are viewed as active participants in managing their own health care. Practitioners and patients are encouraged to forge partnerships to work together as equals. Practitioners bring their professional expertise to the table, whilst patients draw on their own experiences, beliefs and wishes. 10 , 11
The UK Medicines Partnership 12 defined three pillars relating to concordance: to provide the patient with tailored, accurate, accessible and sufficiently detailed information about their illness and treatment options; to involve patients as partners, inviting them to talk about their experiences and reaching a joint decision on treatment, as well as assessing their ability to follow the treatment plan; a continued discussion and reviewing of patients’ medicines and issues surrounding their care. Proponents of concordance believe that patients will benefit from the open, two‐way interaction, as they will gain the information and the control they desire, but only if each patient is treated as an individual. Practitioners need to focus on the individual rather than the illness and interact with patients in a way that suits their levels of understanding and desired levels of involvement. 13
Schattner 14 argues that concordance means that those patients who wish to be less involved in decisions about their own health care have just as much right to be so as those who wish to be more actively involved. Therefore practitioners and health care authorities need to identify how involved individual patients wish to become, and not to assume that they all want to participate. 15
Whether or not a concordant approach to prescribing is practised depends on the willingness of both parties to pursue it. Principally, however, practitioners hold the power. If they do not see the merits in, or practicalities of concordance, then they will not involve their patients in decisions, and the practitioner‐centred approach will continue. Arguably this might lead to higher levels of non‐adherence, as patients become more widely informed about their condition, their treatment, as well as alternative treatments available to them from other sources.
In 2001 Raynor et al. developed the Leeds Attitude Towards Concordance (LATCon) scale 16 to ascertain health professionals’ attitudes towards concordance in medicine taking. The scale has been used in a number of studies, including in the UK, Australia and Finland, 17 , 18 and was also adapted to measure patients’ attitudes. 19
However, the scale now needs updating, as opinions on concordance have developed over the 10 years since it was first proposed, and a new key text has been published. 8 The original scale had no negatively worded items (therefore leaving itself open to the response bias of ‘yeah saying’), used a moderately small number of participants in its development (n = 81), and did not employ test‐retest reliability analysis. Therefore the present study aimed to update, develop and refine the LATCon scale. We involved medical and nursing students and pre‐registration pharmacists to determine their attitudes towards concordance. These groups now receive teaching during their course on compliance and concordance and are the next generation of prescribers (pharmacists and nurses can now gain full independent prescribing rights in the UK, although the prevalence of such prescribing is not yet high). Assessing their attitudes would help ascertain the likelihood of concordance becoming mainstream practice.
Aims of the study
The aims were therefore:
-
•
To create a practical, reliable and valid Likert scale to measure practitioners’ attitudes towards concordance (updating the existing LATCon scale)
-
•
To ascertain the views of medical students, nursing students, and pre‐registration pharmacists on concordance.
Method
Design
This was a cross‐sectional, self‐completion questionnaire survey of an opportunistic sample of medical and nursing students and pre‐registration pharmacists. Questionnaire development included item generation and statistical items reduction. Participants completed the questionnaire on two occasions.
Participants
Participants were student nurses, medical students and pre‐registration pharmacists at the same UK University, all of whom had experience of working with patients. The pharmacists were attending courses during their ‘pre‐registration’ year (the 5th of 5 years training); the nurses were Degree or Advanced Diploma course adult branch students, within 6 months of qualification; the medical students were all in their 3rd or 4th year of a five‐year medical undergraduate programme. The participants were recruited as follows: the pre‐registration pharmacists and student nurses were attending lectures at the university and questionnaires were distributed to all students present; the medical students were recruited opportunistically via social networks. Participants were asked to provide a university email address, to contact them if they would be in their practice setting during the second (T2) data collection.
Procedure
A 4‐stage development and testing of an attitudinal scale involved the:
-
1
Generation of pool items;
-
2
Incorporation of expert opinion;
-
3
Completion of 31 item scale, followed by item reduction;
-
4
Completion of shortened (20 item) scale.
Stage 1: generation of pool items
Two source materials were used to generate potential items for the questionnaire. First, a recent and influential book on concordance: 8 one researcher (MJ) highlighted statements throughout the book that described the nature of what concordance is and what it is not. By a process of consensus discussion, we re‐worked the selected statements, where possible, into questionnaire items. We took care to generate items that were:
-
•
unambiguous
-
•
easy for the participant to understand
-
•
monotonic, and
-
•
non‐compound.
We also ensured that items were not wholly or partly duplicated.
Second, we used the existing LATCon scale 16 for situations where the source book 8 had not referred to a topic that we thought relevant, or when the existing wording in the LATCon scale for a particular topic was strong and there was no obvious way of improving it.
Stage 1 generated a pool of 44 potential items that focussed on key aspects of concordance, as outlined by Bond et al. 8 Each item comprised a statement relating to concordance with a Likert four point response format, ranging from ‘strongly disagree’ (scored as 0) to ‘strongly agree’ (scored as 3). A higher score would indicate a more positive attitude to concordance. Negatively‐worded items were reverse‐scored.
Stage 2: incorporation of expert opinion
We sent the pool of 44 potential items to three UK experts for their opinion, chosen because they have been influential contributors to the concordance debate and policy initiatives over the last decade. Two are leading academic researchers; the third has headed several non‐governmental organizations related to prescribing and concordance. They were asked to comment on the content of the draft scale (for example: Are there any included items that are not relevant to concordance? Are there any important aspects of concordance that have been omitted from the item pool?). They were also asked to comment on the wording of the items (Was it clear, unambiguous and accurate?). This stage of the questionnaire generation offered an important check for criterion validity.
After receipt of the expert opinion, we revised and shortened the questionnaire, leading to a 31 item scale that covered the main aspects of concordance. We were mindful of influences on participants, so arranged the question order to avoid topic clustering, and also included 10 items that were negatively‐worded (see 1, 2).
Table 1.
The 20‐item LATCon II scale
| 1 | Prescribing should take account of patients’ expectations of treatment |
| 2 | Doctors and patients should agree a treatment plan that takes account of both their views |
| 3 | Patient involvement in the prescribing process always leads to better outcomes |
| 4 | The best use of treatments is when it is what the patient wants and is able to achieve |
| 5. | Doctors should try to help patients to make as informed a choice as possible about benefits and risks of alternative treatments |
| 6. | During the consultation both the doctor and patient should state their views about possible treatments |
| 7. | Doctors should give patients the opportunity to talk through their thoughts about their illness |
| 8. | Doctors should make clear when the benefits of the medicine are uncertain |
| 9. | Doctors should be more sensitive to how patients reacto the information they give |
| 10. | It is always important for doctors to listen to patients’ personal understanding of their condition |
| 11. | It is sometimes appropriate for the doctor to make treatment decisions without the patient’s input |
| 12. | The doctor and patient should find common ground on what the problem is and jointly agree on what to do |
| 13. | Doctors should encourage patients to express their concerns about medicine taking |
| 14. | Taking account of patients’ views about medicines is not always necessary for appropriate prescribing |
| 15. | The doctor is the expert and the patient’s role is to do as the doctor says |
| 16. | The consultation between the doctor and the patient should be viewed as a negotiation between equals |
| 17. | A good treatment decision is made when both the doctor and patient agree on the treatment to use |
| 18. | During the doctor‐patient consultation the patient’s decision is the most important |
| 19. | Patients should be able to take on as much responsibility as they wish for their own treatment |
| 20. | It is not always necessary for doctors to take account of patients’ priorities |
Each item was scored as follows:
0, strongly disagree; 1, disagree; 2, agree; 3, strongly agree.
Table 2.
The 11 scale items removed between T1 and T2
| 21. | The doctor should take most of the responsibility for treatment decisions in the consultation |
| 22. | When prescribing, it is not always necessary for the doctor and patient to find common ground |
| 23. | Although the doctor‐patient interaction is a two‐way process, the most important decisions are made by the doctor |
| 24. | In return for an increased voice in consultations patients should have to accept increased responsibility for the decisions taken |
| 25. | Partnership in medicine taking would mean the doctor giving in to patients’ demands for inappropriate treatments |
| 26. | The increased time spent in consultations will outweigh any benefits achieved by partnership in treatment decisions |
| 27. | Patients’ beliefs about medicines are often wrong |
| 28. | A high priority in the consultation between doctor and patients is to establish agreement about the need for medicine |
| 29. | It is easy for doctors to be dismissive about patients’ beliefs when they are wrong from the medical view‐point |
| 30. | Patients should be able to choose whether or not to have a medicine prescribed |
| 31. | Consultations that ignore the patient’s viewpoint are more likely to lead to the patient not taking the medicine |
Stage 3: completion of 31 item scale, followed by item reduction
The 31 item questionnaire was distributed to participants (T1). To ensure standardization of the test and to gain informed consent, an information sheet and consent form were distributed along with the questionnaire. Total scores were calculated from those participants who completed all items of the questionnaire; we did not impute scores for missing data.
For ease of use a scale must not contain too many items and we considered the 31 item scale too long. We therefore analysed the data to reduce the number of items, with a target of no more than 25 items, and as few items as would be psychometrically efficient. We were also mindful of the multi‐factorial nature of concordance and we wanted any shortened scale to reflect that. The scale was shortened by using the following criteria:
-
•
the performance of each item in terms of its contribution to the total scale (as assessed by calculating the item‐remainder correlation statistic);
-
•
the scale’s internal reliability (as measured by Cronbach’s Alpha statistic) and the effects on this statistic of removing individual items;
-
•
the number of participants not completing the item (on the basis that a higher non‐completion rate would likely indicate that the item is in some way problematic);
-
•
the number of negatively–worded items, as we wanted to ensure that the final scale included several items of this type.
Stage 4: completion of shortened (20 item) scale
The shortened questionnaire was distributed (T2) 4–6 weeks after completion of the 31 item version to the same student practitioners. We chose a 4–6 week period as sufficiently short for practitioners to be at the same stage of training at T1 and T2, but long enough for any memory of their responses to scale items to have been lost. Distribution of questionnaires was done either in person (when the nurses or pharmacists were attended a lecture later in their course) or by sending copies via email. This process of contacting participants meant that some of those who completed the 31 item version (at T1) did not complete the shorter 20 item version (at T2). Similarly, we were able to recruit some eligible students at T2 only, so they completed the 20 item scale only. Total scores were calculated for the 20 item version, including only those participants who had completed all items on the scale, and comparisons were calculated for the three professional groups.
Data handling
Each item of the completed questionnaires and participants’ scores were entered into a database, with participants assigned a unique numerical identifier. Each item was scored 0 (‘strongly disagree’) to 3 (‘strongly agree’), after the five negatively worded items had been recoded. This gave the possible range of total scores as 0–93 (at T1) and 0–60 (at T2), with higher scores indicating more positive attitudes to concordance. Data were analysed using spss 13.0. 20 No prior sample size calculation was undertaken.
Ethical considerations
Approval was received from the departmental and faculty Research Ethics committees.
Results
Properties of the 31 item scale at Time 1 (see 1, 2)
One hundred forty‐six participants completed the 31 item scale at T1 (37 pre‐registration pharmacists, 71 student nurses, and 38 medical students). All medical students given the questionnaire returned it, so had a return rate of 100%. The nurses were among 111 registered for their course, while the pharmacists were among 58 registered on their course. We did not keep a record of the number of students attending the lectures on the day of questionnaire distribution, so cannot calculate an exact completion rate. However, the rate is no less than 64% (pharmacists) and 64% (nurses). Among the returned questionnaires, 119 (82%) had completed all items. Three of the 146 participants completed the questionnaire and returned it by email; the remainder completed it when the researcher was present. Total questionnaire scores had a wide range (41–82) with a mean score of 59. The distribution of the scores was approximately normal (skewness = 0.135), with the median figure (60) being close to the mean, a standard deviation of 7.0, and an inter‐quartile range of 56–67.
The internal reliability of the scale was assessed by use of Cronbach’s Alpha statistic and the obtained value of 0.77 was sub‐optimal: it suggested that some of the 31 items were contributing little to the overall total, or might be scoring in the opposite direction. Furthermore, we observed that scale completion took 10 min for most participants, which might be too long for its use in many educational and practice settings.
Mean scores of individual items showed a wide range (0.96–2.63), indicating considerable variation among the 31 items. The items also varied in their completion rate: data from the 146 participants revealed that one item had six missing scores; two items had four missing; and five items had three missing.
Reduction of the scale
The number of items was reduced. The three items with four or more ‘non‐completions’ were removed. Then items were removed according to those that had the lowest item‐remainder correlation, after checking whether the item was positively‐ or negatively‐worded, and what construct the item assessed. Item removal resulted in a scale of 20 items, that included five items that were negatively‐worded (see Table 1). The scale formed from the 20 T1 items had a Cronbach’s Alpha statistic of 0.83.
The reduced 20 item scale had a revised possible range of 0–60, and the data from the 119 participants at T1 produced a mean scale value of 42.1 (SD = 5.9; median 42; inter‐quartile range 38–47). Individual item means ranged from 1.1 to 2.6.
Properties of the 20 item scale at Time 2
One hundred thirty‐one participants completed the 20 item scale at T2: 36 pre‐registration pharmacists; 67 student nurses; and 28 medical students. As for T1, we cannot calculate an exact completion rate. Four of the 131 participants completed the questionnaire and returned it by email; the remainder completed it when the researcher was present. Of the 146 participants who completed the questionnaire at T1, 94 (64%) completed it again at T2. There was no difference in T1 scores between those who did and those who did not complete the scale again at T2 (mean difference = 1.42; 95% CIs −1.31 to 4.16; P = 0.306). The additional 37 participants at T2 were completing it for the first time. Among the 131 participants at T2, 121 (92%) completed all items on the questionnaire, and the analysis is based on these 121 sets of complete scores. Total T2 questionnaire scores had a wide range (from 29 to 57) with a mean score of 43.4. The distribution of the scores was approximately normal, with a slight positive skew (skewness = 0.250, see Fig. 1). The median figure (43) was close to the mean, and the scale scores had a standard deviation of 5.8 and inter‐quartile range of 39–48. Individual item means ranged from 1.2 to 2.6.
Figure 1.
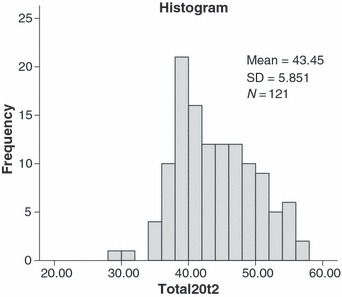
Distribution of total scores on the 20 item scale at T2.
No particular questionnaire item appeared problematic (only items 9, 12 and 18 had two ‘non‐completers’ and none had more than that). The Cronbach’s Alpha statistic on the T2 scale data showed an internal reliability of 0.82.
Test‐retest reliability
Seventy‐eight participants completed all 20 items on the shortened scale at both T1 and T2. A Pearson’s product moment correlation statistic of +0.641 (d.f. = 77; P < 0.001) indicated a statistically significant and positive association between T1 and T2 scores (see Fig. 2). Among these 78 participants, the total scale score rose, from 43.2 at T1 to 43.9 at T2, but these means are not statistically different (mean difference = 0.68; 95% CIs −0.43 to 1.78; P = 0.225).
Figure 2.
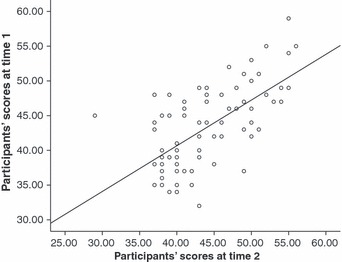
Scatterplot (and Line of Best Fit) indicating participants’ scores at T1 and T2 (n = 78).
Table 3 indicates the comparison between T1 and T2 scores for the 78 participants, with a difference score indicated regardless of whether the difference between scores was positive or negative. Two‐thirds of participants (64%) had scores that were the same or within 4 points on the scale. These various data suggest that the scale scores are stable when measured several weeks apart.
Table 3.
The comparison of participants’ scores at T1 and T2
| Participants’ scores at time 1 compared with time 2 | Number of participants (%) |
|---|---|
| Same score | 9 (12) |
| +/−1 or 2 points | 23 (29) |
| +/−3 or 4 points | 18 (23) |
| +/−5 or more points | 28 (36) |
| Total | 78 (100) |
Differences between practitioner groups
Analysis of variance (anova) statistics were calculated to assess any differences between the three practitioner groups at T2. (These analyses were conducted by using only those questionnaires that had all completed items). (See Table 4).
Table 4.
Means (and SD) statistics for completed 20 item scales at T2.
| T2 Group | Mean score (SD) |
|---|---|
| Pre‐registration pharmacists (n = 31) | 40.5 (4.6) |
| Student nurses (n = 55) | 45.7 (5.7) |
| Medical students (n = 30) | 41.5 (5.4) |
| All (n = 121) | 43.4 (5.8) Analysis of variance among scores of the three groups: (F = 11.57, d.f. = 2.118, P < 0.001) |
Analysis of variance revealed a significant variation among the three groups. Post hoc Bonferroni statistics showed that student nurses achieved higher scores than medical students (P = 0.004) and pre‐registration pharmacists (P < 0.001), with differences equivalent to around 10% mean scores. The scores for medical students and pre‐registration pharmacists showed no statistical difference.
Dimensionality testing – factor analysis
To test the dimensionality of the scale a principal components analysis was conducted on the T2 data (n = 121). This technique identifies clusters of variables that are more highly correlated with each other than with the other variables. The calculation of the Kaiser‐Meyer‐Olkin value (0.748) and Bartlett’s Test of Sphericity (P < 0.001) indicated that the data were suitable for a principal components analysis. It revealed the presence of seven components with eigenvalues >1 (see Table 5). These components accounted for more than 64% of the total variance. It can be seen that component 1 explains a large proportion of the variance (26%).
Table 5.
Total variance explained through the principal components analysis (n = 121)
| Component | Initial eigenvalue | % of variance explained | Cumulative % variance explained |
|---|---|---|---|
| 1 | 5.14 | 26 | 26 |
| 2 | 1.89 | 9 | 35 |
| 3 | 1.50 | 7 | 42 |
| 4 | 1.27 | 6 | 48 |
| 5 | 1.22 | 6 | 54 |
| 6 | 1.06 | 5 | 59 |
| 7 | 1.03 | 5 | 64 |
Factor rotation was used as a further interpretative tool. A Varimax rotation was chosen and the five extracted components (see Table 6) explained just over 54% of the overall variance. The results suggest that there are five sub‐components which together can explain the majority of the variance. These being:
Table 6.
Analysis of variance after factor rotation (n = 121)
| Component | Total rotated sums of squared loadings | % of variance explained | Cumulative % variance explained | Items loading onto the component |
|---|---|---|---|---|
| 1 | 2.90 | 14 | 14 | 6, 7, 8, 9, 11 |
| 2 | 2.27 | 11 | 25 | 5, 10, 15, 20 |
| 3 | 2.15 | 11 | 36 | 1, 2, 13, 14 |
| 4 | 1.86 | 9 | 45 | 3, 4, 17 |
| 5 | 1.84 | 9 | 54 | 12, 19, 16, 18 |
-
•
the level of participation and involvement that the respondents feel patients’ should have within the consultation (Component 1),
-
•
the continued use of a paternalistic style of interaction (Component 2),
-
•
the necessity to find common ground and be in agreement over decisions (Component 3),
-
•
the perceived benefits of partnership in medicine taking (Component 4) and
-
•
the equality and shared control within the interaction (Component 5).
Discussion
The aim of the present study was to update, develop and refine the current LATCon scale and in so doing to create a reliable and valid Likert scale to measure the attitudes of health practitioners and student practitioners towards concordance. Statistical analysis indicates that a reliable and valid scale to measure such attitudes was developed. The revised scale takes account of contemporary thinking on the concept of concordance, has been revised to include negatively‐worded items, and has undergone more detailed statistical analysis than the original scale.
Item analysis revealed that the 20 item scale was found to be internally reliable: the Cronbach’s Alpha statistics on the 20 item scale at both T1 and T2 were both above 0.7, the threshold often applied to the measurement of psychological constructs. 20 Further, the test‐retest analysis showed a significant positive association between participants’ scores at T1 and T2, indicating that the scale is consistent over time. Scores for the three respondent groups did increase slightly (but not statistically significantly) in the 4–6 weeks between T1 and T2, but further analysis revealed that at T2, two‐thirds of participants scored within five marks of their earlier score, which again signifies consistency over time.
Looking at the data from the 119 participants who completed all items at T1 and the 121 participants who did so at T2, the small increase in scores at T2 does not appear to be due to a response bias. That is, participants who scored higher at T1 were no more likely to complete the questionnaire at T2, (around one third of participants who completed the scale at T1 were either unavailable or did not return the scale at T2). An alternative explanation is that T1 scale completion itself produced a change in attitude, by prompting people to consider the issue for the first time or more deeply than before, producing a small mean increase seen in the scale score at T2.
The resultant 20 item scale could be used in various settings, such as in research, in education (as a teaching aid and to analyse any effect of course teaching on attitudes) and in practice (to assess practitioners’ and, more likely, patients’ views).
Practitioners’ attitudes towards concordance
The UK National Health Service promotes increased patient involvement, including a concordant approach to medicine prescribing and taking, and so the attitudes of today’s students have implications for future health care. The present study found that overall the three respondent groups were in agreement with the concordant approach. This suggests that, on the whole, they would be likely to practise the concepts of concordance if the circumstances allowed, although the link between attitudes and behaviour is not straight forward and can depend on other factors. 21 A wide range of scores was seen both within and between the respondent groups indicating that there was not universal agreement with concordance. Four items appear to be the most open to individual interpretation and seem to be the most wide ranging statements (items 4, 5, 16 and 20), in that participants’ responses to the item might vary, depending on the particular situation to which they see it applying. Therefore the scale’s use in some clinical settings might be enhanced by these items being worded more specifically. This might result in data that that offer a truer reflection of practitioners’ attitudes, although this change would likely impact on total scale scores and the scale’s psychometric properties might not remain the same.
Analysis of the differences between the respondent groups found that student nurses were significantly more in agreement with the concept of concordance than medical students and pre‐registration pharmacists. There is no obvious explanation of this finding. Nurses have always been involved in the administration of medicines to patients, but following the drive for modernization and efficiency within the NHS nurses have, with appropriate training, now been given the authority to prescribe medicines. Throughout their training for a prescribing role, nurses are taught specifically about the principles of concordance, 22 but the effects of such training cannot explain the results of this study, conducted among student nurses who had not received such training.
Empirical support for the present study’s findings comes from Latter et al. 22 who looked into the practice of nurses’ prescribing and found that they believed they were adopting the fundamental principles of concordance by establishing relationships with patients and working in partnership with them. Patients report positive views about their prescribing interactions with nurses and value the two‐way communication style that nurses adopt along with the greater information provision and consideration that nurses engaged in compared with other practitioners. 23
Doctors and pharmacists often underestimate the amount of information, particularly regarding the side effects and alternative medicines, that their patients desire and do not initiate patient involvement in decision making as nurses. 24 Patients regard spoken information from a practitioner as their preferred primary source of medicines information. 25 Pharmacists are usually a patient’s first port of call after receiving a new prescription and therefore are an important communication line for patients. However, the present study found that pharmacists were generally in agreement with the concordant approach, but were less so than nurses. This finding supports previous work showing that, in most interactions, pharmacists did not offer counselling or advice about prescriptions, and that only a small minority of pharmacists asked patients if they had any questions or concerns. 26 , 27
Limitations of the study
The study used a 4‐point Likert scale, which has the advantage of not giving participants a ‘middle ground’, or ‘unsure’ response choice, therefore forcing participants to offer an opinion. As a result, people who are genuinely unsure of their opinions are forced either into producing an untrue response or leaving the question blank. This might explain the number of incomplete questionnaires the study received.
The sample comprised student practitioners and it cannot be assumed that qualified, practising professionals would express similar attitudes. Validation of the scale among qualified professionals would be valuable. The sample was also relatively small, with fewer than 100 participants completing all items on both occasions, meaning that some analyses (particularly the factor analysis results) require confirmation. The initial response rate was high, although the drop‐out rate between T1 and T2 was also relatively high and this might have impacted on the data obtained. The samples were obtained in an opportunistic way, and confirmation of these results among participants recruited after random sampling, would strengthen the conclusions.
Further research
Although the study has produced a questionnaire to measure health professionals’ attitudes towards concordance, further work is needed to test the scale among established, qualified practitioners, particularly those communicating with patients about their medicines. Work is also needed to test or adapt the scale for completion by patients, since successful partnership in medicine taking depends on the attitudes of both parties.
The scale assesses attitudes to concordance, but it is not possible to say how these attitudes will translate into behaviours in practice. Practitioners’ attitudes towards concordance may change when presented with differing situations, or they may decide for one reason or another not to act in line with their attitude. Therefore further research should study how practitioners’ attitudes towards concordance change between situations and over time. It should also study how in real life situations practitioners cope with balancing patients’ desires and their concerns to provide the best possible care based on clinical evidence.
Acknowledgements
The authors should like to thank the three experts who reviewed the initial pool of potential questionnaire items (Alison Blenkinsopp, Professor of the Practice of Pharmacy at Keele University; Christine Bond, Professor of Primary Care: Pharmacy at the University of Aberdeen; and Joanne Shaw, Chair of ‘Ask About Medicines’ and past Director of the Medicines Partnership), teaching staff at the University of Leeds for facilitating access to participants, Dr Daryl O’Connor for methods advice, Hazel French for her assistance in formatting and preparing the questionnaires, and two anonymous reviewers for their valued comments on a previous version of this article.
References
- 1. Sabaté E. Adherence to Long‐Term Therapies: Evidence for Action. Geneva: World Health Organisation, 2003. [Google Scholar]
- 2. Office of Health Economics Compendium . http://www.ohecompendium.org/ , 200506.
- 3. Stoate H. Concordance and Wasted Medicines. House of Commons All Party Pharmacy Group. London: House of Commons, 2000. [Google Scholar]
- 4. Haynes RB, Yao X, Degani A, Kripalani S, Garg A, McDonald H. Interventions for enhancing medication adherence (Cochrane Review). The Cochrane Library. Issue 1. England: Oxford, 2008, Updated Software. [Google Scholar]
- 5. Stevenson FA, Cox K, Britten N, Dundar Y. A systematic review of the research on communication between patients and health care professionals about medicines: the consequences for concordance. Health Expectations, 2004; 7: 235–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elwyn G, Edwards A, Britten N. “Doing prescribing”: how might clinicians work differently for better, safer care. Quality & Safety in Health Care, 2003; 12: 33–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carter S, Taylor D, Levenson R. A Question of Choice – Compliance in Medicine Taking. London: Medicines Partnership, Royal Pharmaceutical Society, 2003. [Google Scholar]
- 8. Bond C. (Ed.). Concordance. London: Pharmaceutical Press, 2004. [Google Scholar]
- 9. Bajramovic J, Emmerton L, Tett SE. Perceptions around concordance – focus groups and semi‐structured interviews conducted with consumers, pharmacists and general practitioners. Health Expectations, 2004; 7: 221–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Royal Pharmaceutical Society of Great Britain . From Compliance to Concordance: Towards Shared Goals in Medicine Taking. London: Royal Pharmaceutical Society, 1997. [Google Scholar]
- 11. Horne R, Weinman J, Barber N, Elliott R, Morgan M. Concordance, Adherence and Compliance in Medicine‐Taking. Southampton: National Co‐ordinating Centre for NHS Service Delivery and Organisation R&D, 2005. [Google Scholar]
- 12. Medicines Partnership . Project Evaluation Toolkit. London: Medicines Partnership, 2003. [Google Scholar]
- 13. Auerbach SM. Do patients want control over their own health care? A review of measures, findings, and research issues. Journal of Health Psychology, 2001; 6: 191–203. [DOI] [PubMed] [Google Scholar]
- 14. Schattner A. What do patients really want to know? Quarterly Journal of Medicine, 2002; 95: 135–136. [DOI] [PubMed] [Google Scholar]
- 15. Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making: a national study of public preferences. The Journal of General Internal Medicine, 2005; 20: 531–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Raynor DK, Thistlethwaite JE, Hart K, Knapp P. Are health professionals ready for the new philosophy of concordance in medicine taking? International Journal of Pharmacy Practice, 2001; 9: 81–84. [Google Scholar]
- 17. Kansanaho HM, Puumalainen II, Varunki MM, Airaksinen MSA, Aslani P. Attitudes of Finnish community pharmacists toward concordance. The Annals of Pharmacotherapy, 2004; 38: 1946–1953. [DOI] [PubMed] [Google Scholar]
- 18. Thistlethwaite JE, Knapp P, Raynor DK. Medical students’ attitudes towards concordance in medicine taking: the impact of an educational intervention. Education for Health, 2003; 16: 307–317. [DOI] [PubMed] [Google Scholar]
- 19. Stokes M, Knapp P, Thistlethwaite JE, Raynor DK (2002). Using the LATCon scale to measure patients’ attitudes to concordance. Presented at the Health Services Research & Pharmacy Practice conference, Leeds 2002. (http://www.hsrpp.org.uk/abstracts/2002_18.shtml, accessed 21 April 2008).
- 20. SPSS Inc . SPSS Base 13.0 for Windows User’s Guide. Chicago IL: SPSS Inc, 2006. [Google Scholar]
- 21. Kaplan RM. Behaviour as the central outcome of health care. American Psychologist, 1990; 45: 1211–1220. [DOI] [PubMed] [Google Scholar]
- 22. Department of Health . Extending Independent Nurse Prescribing Within the NHS in England: A Guide for Implementation. London: Department of Health, 2002b. [Google Scholar]
- 23. Latter S, Maben J, Myall M, Young A. Perceptions and practice of concordance in nurses’ prescribing consultations: findings from a national questionnaire survey and case studies of practice in England. International Journal of Nursing Studies, 2007; 44: 9–18. [DOI] [PubMed] [Google Scholar]
- 24. Brooks N, Otway C, Rashid C, Kilty E, Maggs C. The patients’ view: the benefits and limitations of nurse prescribing. British Journal of Community Nursing, 2001; 6: 342–348. [DOI] [PubMed] [Google Scholar]
- 25. Raynor DK, Blenkinsopp A, Knapp P et al. A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines. Health Technology Assessment, 2007; 11: 5. [DOI] [PubMed] [Google Scholar]
- 26. Nair K, Dolovich L, Cassels A et al. What patients want to know about their medications. Canadian Family Physician, 2002; 48: 104–110. [PMC free article] [PubMed] [Google Scholar]
- 27. Cox K, Stevenson F, Britten N, Dundar Y. A Systematic Review of Communication Between Patients and Healthcare Professionals about Medicine Taking and Prescribing. London: Medicines Partnership, 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]


