Abstract
Objective To assess the effectiveness of an audio‐guided component: an audio‐guided decision aid vs. a stand‐alone booklet decision aid.
Background Despite extensive evaluation of decision aids in clinical settings the presentation style has not been properly assessed, and audio‐guided decision aids are widely used although not supported by evidence‐based research.
Design Randomized controlled trial.
Setting and participants Two obstetric hospitals in Sydney, Australia. A total of 395 pregnant women having their first baby and approximately ≥36 weeks of gestation, planning a vaginal birth of a single infant and with self‐assessed English sufficiency to read and listen to English‐presented material.
Intervention A decision aid for labour and childbirth analgesia that was presented in two ways: an audio‐guided decision aid compared with a booklet only style decision aid.
Main outcome measures Decisional conflict, knowledge and anxiety.
Results Although both groups improved their knowledge scores and decreased their decisional conflict there were no significant differences between groups: mean knowledge score – audio‐guided group, 65.9 vs. booklet group, 64.3; mean difference, 1.7; 95% CI (–7.5, 4.2); mean decisional conflict score – audio‐guided group, 23.6 vs. booklet group, 24.3; mean difference, 0.7; 95% CI (–1.4, 2.9). Acceptability and compliance were high.
Discussion and conclusions This evaluation highlights the lack of additional benefit in using audio‐guided formats for presenting health information to consumers who are from a general English‐speaking population. These results considered together with the increase in costs and work involved in producing audio components suggests that written and pictorial methods may be sufficient for decision aids aimed at a general audience.
Keywords: audio‐guide, decision aid, labour analgesia, pregnancy, RCT
Introduction
The benefits of decision aids in clinical decision making have been well established, and there are a wide variety of decision aids available that present information for a range of clinical issues. A Cochrane systematic review of decision aids identified 221 aids, for screening or treatment decisions, using an array of presentation designs including brochures, video presentations, decision trees, analytical hierarchal processing via personal computers, poster board cards and on‐line presentations. 1 Despite extensive evaluation of decision aids in clinical settings the presentation style has not been properly assessed, and there is conjecture regarding the ideal presentation style. 2 One of the most commonly used formats is an audio‐guided booklet. The booklet highlights key points and the audio component connects these points in a narrative format. The premise behind the audio‐guide is that it increases accessibility. This is thought to be important for individuals with low literacy, particularly those from linguistically diverse backgrounds or who have limited experience of interpreting risk information. However, the utility of audio components needs to be balanced against the difficulty it adds to the development process.
The addition of an audio component to the development of a decision aid increases the difficulty and cost, as appropriate equipment needs to be accessed which may not be readily available to decision aid developers. 1 , 3 Audio components also increase the complexity when updating the decision aid as the whole audio component needs to be re‐recorded. Keeping apace with technological advances in audio formats and community preferences for accessing these is also challenging. For example, early audio decision aid used tapes which have been superseded by compact discs (CDs) and more recently by digital files. The difficulty in preparing audio components has deterred some researchers from using audio‐guides 4 especially considering the lack of supporting evidence.
To the best of our knowledge there are no trials directly comparing an audio decision aid with a non‐audio decision aid. Trials of decision aids either compare the decision aid with usual care, or they compare a more detailed decision aid with a simpler version. 1 Of the second group, the formats and presentation styles are mixed and the results suggest that more detailed decision aids have a positive effect on knowledge compared with simple decision aids. 1 However, the focus of these studies is how much information is required to make a difference rather than how the information should be presented. These investigations do not answer the question which developers are considering; whether print presentation style is as effective as audio‐guided presentation. This article presents the results of a trial assessing the effectiveness of a decision aid presented in two formats; an audio‐guided format vs. a stand‐alone booklet format. The decision aid was designed to facilitate informed decision making for women having their first baby and considering labour and childbirth analgesia options.
Materials and methods
Study setting
The trial was conducted in Sydney, Australia in two obstetric hospitals between September 2004 and April 2006. Of these, one was a tertiary public hospital and the other was a private hospital. In Australia, women can choose to have pregnancy care in a public hospital which is covered by the national health insurance, or choose private care by an obstetrician in a public or private hospital. Public care is usually provided by hospital midwives overseen by salaried doctors. Public patients choose between the midwife antenatal clinic, the midwife run birth centre or use ‘shared care’ (joint antenatal care between the hospital antenatal clinics and their own general practitioner). In the private hospital, all women receive private care from their chosen obstetrician. Both trial hospitals provided a range of non‐drug and anaesthetic options for pain relief in labour. Epidurals were available 24 h a day from anaesthetic staff designated to the labour ward in both hospitals.
Participants and eligibility criteria
Women having their first baby (primiparous), late in pregnancy (≥36 weeks of gestation), who were planning for a vaginal birth of a single infant were eligible for the study. Primiparous women were selected because previous pregnancy has a strong impact on decision making and analgesia use in labour. 5 , 6 Excluded women were those who did not have a choice regarding their analgesic options (e.g. planned epidural for symptomatic heart disease), had contraindications to analgesia (e.g. drug sensitivities, anticoagulants and thrombocytopaenia) or had self‐assessed English insufficiency (insufficient to complete the questionnaires, or use the intervention material which was written in English).
Intervention
We developed a decision aid in two formats that presented information on the options for labour and childbirth analgesia, using methods based on the Ottawa Health Decision Framework. 7 The first presented the information in a stand‐alone booklet. The second decision aid included the same information; however, it was presented as an audio‐guide (booklet and CD). The audio‐guided booklet presented a condensed dot‐point version of the information and the audio presented the entire information using a narrative form on a CD. These combined together presented exactly the same information as the stand‐alone booklet.
The decision aid material was developed and pilot‐tested using an iterative process of review and revision with a multidisciplinary group, including consumers and was based on the method of the Ottawa Health Decision Group. 7 The decision aid content (the booklet and the audio text) was assessed using the Flesch–Kincaid Grade and graded 9.9 demonstrating that is was accessible to the average ninth‐grade student.
The final stand‐alone booklet comprised a 56‐page A5 booklet and a 4‐page A3 worksheet. The audio‐guided decision aid consisted of a 53‐page A5 booklet, a 4‐page A3 worksheet and a 40‐min audio CD. The booklets were similarly sized as each analgesic option was displayed on two face‐to‐face pages, and hence the final size of the book was not altered by the amount of information presented. The CD was narrated from a personal perspective (‘Before you have an epidural, you will be examined to make sure that it is safe for you and your baby’); however, risk information was de‐personalized using the passive voice (‘Out of 100 women who used a bath, 39 had an epidural’).
The content of the decision aid included a wide range of both pharmacological and non‐pharmacological analgesics that were used and accepted in the trial hospitals. This ranged from having a support person to epidural analgesia. Evidence for each option was based on the highest quality evidence available and in most cases this was based on systematic reviews with meta‐analyses (Table 1). The two main outcomes presented for each analgesic option were: women’s satisfaction with the pain relief and need for further pain relief after using the analgesic method. Probabilities of other outcomes for the mother and the baby were synthesized from the evidence base and were presented as a list of pros and cons for each analgesic option.
Table 1.
Labour and childbirth analgesic options included in the decision aid and the evidence base
| Analgesic option | Evidence base |
|---|---|
| Support person | Systematic review 16 |
| Being upright during labour | Three systematic reviews 17 , 18 , 19 |
| Touch and massage | Two systematic reviews, 20 one based on observational data 20 |
| Bath | Systematic review 21 |
| Aromatherapy | Systematic review 22 |
| Acupuncture | Systematic review 22 |
| Hypnosis | Systematic review 22 |
| Transcutaneous electrical nerve stimulation (TENS) | Systematic review 23 |
| Nitrous oxide | Systematic review 24 and population‐based data 25 |
| Opioid analgesia | Two systematic reviews 26 , 27 and population based data 25 |
| Epidural analgesia | Two systematic reviews 28 , 29 and observational research 29 , 30 , 31 |
Procedures and recruitment
The trial made use of the usual schedule of antenatal visits in late pregnancy, and eligible women were identified from the daily patient lists. All eligible women attending for their ∼36‐week antenatal appointment were invited to participate and informed consent was obtained.
Treatment allocation was randomly generated by computer using random variable block sizes. The participants were randomized by the research assistant who telephoned a remote location. It was not possible to conceal allocation once randomized; however, to minimize contamination a research assistant worked at each centre and the antenatal staff were kept blinded to the treatment allocation and the actual content of the decision aid. Women were randomly allocated, to one of the study groups and baseline data were collected. Women could review the decision aid at home or in the clinic depending on their own preferences. The following week, immediately before their next appointment the decision aid was reviewed with the research assistant, and the first follow‐up questionnaire was completed. At 3 months postpartum, a second follow‐up questionnaire was mailed with reply paid envelopes to the participants. Data on pregnancy and birth outcomes were obtained from the hospital obstetric records.
The study was approved by the Sydney South West Area Health Service Human Research Ethics Committee, and the Human Research Ethics Committee, University of Sydney.
Outcome measures
The effectiveness of the decision aid to improve patient decision making was determined by assessing primary outcomes of knowledge, decisional conflict (uncertainty regarding decision) and anxiety. These were measured using self‐administered questionnaires that have been extensively used and validated in decision aid analysis and were adapted for this content. Knowledge of labour analgesic options and outcomes were assessed using a 20‐item true/false questions at baseline and at first follow‐up. The question format was based on the style of the Ottawa Health decision group, and on our own previous work. 3 The content was based on general knowledge about labour analgesia, and would be available in many pregnancy handbooks designed for the general public. It did not require any specialist knowledge and would be at an appropriate level for gaining informed consent. The Decisional Conflict Scale was used to measure uncertainty and specific factors such as feeling uninformed, unclear about values and unsupported in decision making. 8 Each item was scored according to the instructions and standardized to a score between 0, representing low decisional conflict, and 100, extreme decisional conflict.
A number of both affective (anxiety, satisfaction and participation in decision‐making) and behavioural outcomes (intention and actual decision taken and acted upon) were also examined. The six‐item short form of the state scale of the Spielberger State‐Trait Anxiety Inventory was used to measure anxiety. 9 Compliance and acceptability of the decision aid materials were also assessed. We asked whether women had used ‘all’ of the materials they received, ‘most’, ‘some’ or ‘hardly any’. Compliance was defined as high when women had read and used all of the interventions they received, either the booklet and worksheet, or the booklet, worksheet and CD. We also asked open‐ended questions in regards to the acceptability of the intervention, and we specifically asked, ‘Would you recommend the decision aid? Why? or why not?’.
Data analysis
The sample size calculations were based on the mean difference in the decisional conflict scale between the two arms of the trial. Meta‐analysis comparing decision aids with a pamphlet reports a pooled mean difference for decisional conflict of –4.35 (95% confidence interval or CI: – 6.8, –1.9), based on the standardized scale of 0–100. Assuming a mean difference of –4.35 and SD of 13.0, 141 women (significance 0.05, power 0.8) in each arm of the trial were required to demonstrate a difference in decisional conflict. Far fewer women were required to change the knowledge scores. 6 The sample size was inflated to allow for loss to follow‐up and we therefore determined that we required 180 women in each arm.
Analyses were by intention to treat. Study groups were compared in terms of baseline characteristics. Univariate analyses were performed for demographic, primary and secondary outcomes. Results for knowledge outcomes were analysed by summing and calculating the percentage of correct responses for each individual. Scoring for affective outcome measures were calculated according to the recommended algorithms. 8 , 9 , 10 , 11 , 12 Measures were then summed and averaged for each woman and the mean score for each study group was calculated for each data collection point. Group differences in categorical outcome variables were assessed using chi‐squared or Fisher exact tests and relative risks with associated 95% CIs. 13 Yates’ correction was applied to tables with one or more cells with frequencies less than five. Continuous variables were examined with the two‐sample t‐tests using Satterwaite correction in cases with unequal variances. 14 For repeated measures, analysis of variance was conducted to assess group differences in outcomes over time. Two‐sided P‐values less than 0.05 were statistically significant and all data were analysed using SAS version 9.1 (SAS Institute, Cary, NC, USA).
Post‐hoc sub‐group analysis was performed among women with lower education levels (n = 163). We defined low education based on whether women had completed university education or not, that is, those without university education were in the low education group. We then tested the hypothesis that audio decision aids will be more effective for people with lower educational levels.
Results
Study recruitment and follow‐up
Between September 2004 and April 2006 a total of 426 eligible women were approached. Of these, 395 (92%) women agreed to participate and were recruited into the trial and were randomly allocated to one of the two arms.
Baseline measurements
Brief socio‐demographic data were collected to assess the comparability of the two groups. Table 2 demonstrates the comparability in demographic measures of women randomized to the two decision aid groups. The mean age was approximately 30 years and the mean gestation at enrolment was 36 weeks. An equal proportion of both groups of women were university‐educated and most were either married or living with their partner. The majority of women reported they were not currently smokers.
Table 2.
Baseline measures of maternal characteristics and primary outcomes by trial group
| Maternal characteristics | Audio‐guided decision aid (n = 193), n (%) | Booklet decision aid (n = 202), n (%) |
|---|---|---|
| Maternal age [mean years] (range) | 30.9 (22–43) | 30.7 (21–44) |
| Gestational age at recruitment [mean weeks] (range) | 35.8 (29–40) | 35.8 (28–38) |
| Education | ||
| School | 37 (19.2) | 36 (17.9) |
| Technical/other | 42 (21.8) | 59 (29.4) |
| University | 114 (59.1) | 106 (52.7) |
| Marital status | ||
| Living with partner | 186 (96.0) | 185 (92.8) |
| Not living with partner | 7 (3.6) | 16 (8.0) |
| Smoking status at first antenatal appointment [self‐report] | ||
| Current smoker | 9 (4.7) | 15 (7.4) |
| Ex‐smoker | 18 (9.3) | 20 (13.4) |
| Never smoked | 167 (86.5) | 169 (79.0) |
| Definite plans to use analgesia for labour (%) [proportion of respondents who had definite plans] | ||
| Support person | 125 (88.0) | 137 (85.6) |
| Bath | 71 (46.1) | 76 (43.2) |
| Nitrous oxide | 30 (19.1) | 42 (24.0) |
| Pethidine | 5 (2.9) | 5 (2.8) |
| Epidural | 10 (6.3) | 18 (10.0) |
| Knowledge mean score (SD) [% of correct responses] | 52.46 (20) | 54.33 (22) |
| n missing (%) | 6 (3) | 8 (4) |
| Decisional conflict (SD) [0–100, 0 = low decisional conflict] | 31.37 (13.03) | 31.47 (12.61) |
| n missing (%) | 4 (2) | 5 (2) |
| Anxiety mean score (SD) [20–80, 20 = low anxiety] | 33 (10) | 34 (9) |
| n missing (%) | 2 (1) | 3 (1) |
SD, standard deviation.
The baseline measures for the primary outcomes were similar between the two study groups. There were no differences between the audio‐guided decision aid group and the booklet‐only group in their knowledge of analgesic options, with both correctly answering approximately half of all the questions. Women in both the groups reported a decisional conflict score of 31. Scores of this magnitude are associated with delays in decision making or low level continuing uncertainty regarding options to choose. Anxiety levels of both the groups were slightly elevated suggesting that women were experiencing mild anxiety (Table 2).
Primary analyses
At first follow‐up (primary outcomes), the overall response rate was 88%, and there were no significant differences between groups (χ2 = 0.12, d.f. = 1, P = 0.827). The overall response at second follow‐up was 78% and was similar for each group (χ2 = 1.41, d.f. = 1, P = 0.234; Fig. 1).
Figure 1.
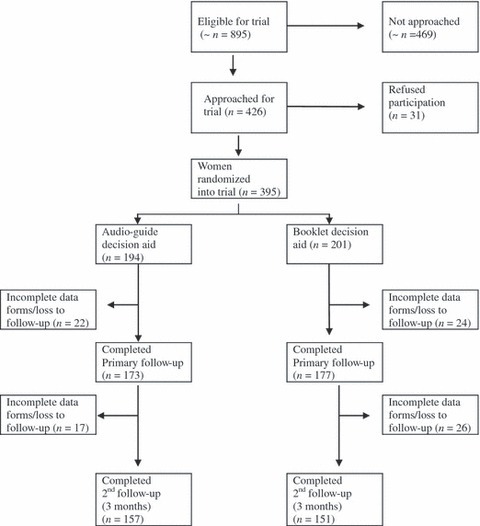
Flow of participants through trial.
At primary follow‐up, there was no difference in the average decisional conflict scores for women who received the audio‐guided decision aid (mean 24.3) compared with those who received the booklet (mean 23.6; Table 3). Overall, women had higher decisional conflict scores for the sub‐scales measuring uncertainty and effectiveness of decision making, but were more likely to feel informed, supported and valued in their decision making, reflected in the lower scores (Table 3). Compared with baseline, mean decisional conflict scores after intervention were significantly reduced in both arms of the trial (F = 179.83, d.f. = 1, P = <0.0001), although this reduction in decisional conflict was not different between the two groups (P = 0.376).
Table 3.
Primary outcomes and sub‐group analysis at primary follow‐up by trial group
| Cognitive outcomes | Audio‐guided decision aid (n = 193), mean (SD) | Booklet decision aid (n = 202), mean (SD) | Mean difference (95% CI) |
|---|---|---|---|
| Knowledge score | 65.93 (29.0) | 64.26 (29.5) | −1.7 (–7.5, 4.2) |
| (% of correct response) | |||
| Analgesia | 68.56 (35.4) | 67.33 (35.2) | 1.2 (−5.7, 8.2) |
| Support person | 72.15 (34.1) | 68.32 (34.6) | 3.8 (−2.9, 10.7) |
| Pethidine | 62.05 (31.0) | 60.40 (31.9) | 1.6 (−4.5, 7.8) |
| Epidural | 62.49 (34.3) | 62.28 (34.5) | 0.2 (−6.6, 7.0) |
| Decisional conflict | 24.32 (10.8) | 23.56 (10.4) | 0.7 (−1.4, 2.9) |
| (0–100, 0 = low decisional conflict) | |||
| Sub‐scales | |||
| Informed | 19.28 (13.4) | 19.37 (12.1) | −0.1 (−2.8, 2.6) |
| Values | 21.32 (12.6) | 21.35 (13.3) | −0.1 (−2.7, 2.7) |
| Support | 18.56 (13.3) | 17.28 (12.9) | 1.2 (−1.4, 4.1) |
| Uncertainty | 35.54 (20.1) | 35.18 (19.7) | 0.4 (−3.8, 4.5) |
| Effective | 29.93 (11.6) | 24.33 (11.2) | 2.0 (−0.4, 4.4) |
| Anxiety | 33 (9) | 33 (9) | 0.2 (−1.7, 2.7) |
| (20–80, 20 = low anxiety) | |||
| Sub‐group: lower education | |||
| Knowledge score | 57.6 (33.0) | 60.5 (28.4) | −2.9 (−12.4, 6.6) |
| Decisional conflict | 24.1 (11.9) | 22.5 (10.7) | 1.5 (−2.7, 5.3) |
| Anxiety | 31.9 (9.2) | 34.7 (9.4) | −2.8 (−5.9, 03) |
SD, standard deviation; CI, confidence interval.
After intervention, overall and specific sub‐scale knowledge scores were similar for women in both the study groups (Table 3). The sub‐scales measured knowledge of analgesia, support person, pethidine and epidural analgesia. Women’s knowledge scores improved significantly by between 10 and 13 points between baseline and primary outcome measures, but there were no differences in the average change in scores between the groups (mean difference: –2.8; 95% CI: –5.9, 0.34). Anxiety scores for women in both the groups remained similar to pre‐intervention scores and did not differ between the groups (mean difference: –0.23; 95% CI: –2.23, 1.74).
Secondary analyses
Women’s satisfaction with decision making was also measured at first follow‐up and was found to be high with no differences between the groups. Although women who reviewed the audio‐guided decision aid were slightly more likely to feel ‘satisfied with their decision making’ (83%) compared with women who reviewed the booklet (80%), there was no significant difference between the two groups (P = 0.112).
Both groups reported high compliance with using the intervention and there were no significant differences between the groups (99.4% of audio‐guided compared with 98.3% of booklet who highly complied; d.f. = 1, χ2 = 0.808, P = 0.369). Only two women used their decision aids in the clinic (audio‐guided group). Data collected from the open‐ended questions regarding the acceptability of the decision aids suggest that there were very small differences among the two groups, and that all women (100%) would recommend the intervention they received. There were very few (<12) negative comments received, and more of these concerned the audio disc than the stand‐alone booklet. Among these negative responses the most common was that the audio was ‘not necessary’ as the booklet was sufficient. The other main comment was that the audio was a ‘bit slow’ or ‘too long’. Overall, however both interventions received overwhelmingly positive comments suggesting that women really liked the decision aids, found them interesting, informative and useful.
Sub‐group analyses
Similar results for primary outcomes were found at baseline and first follow‐up among women with lower levels of education. The mean knowledge score after intervention for women who received the audio decision aid was 58% (n = 79) compared with a mean score of 61% (P = 0.547) for the booklet‐only group (n = 84). These scores were similar to those for the whole group. There were also no differences in decisional conflict and mean anxiety scores between the two groups (Table 3).
Discussion
Although decision aids with audio components are widely used and accepted there is a lack of evidence to support the inclusion of an audio component for a general English‐speaking population. This study is the first to test the relative effectiveness of an audio‐guided format compared with a written version of a decision aid. For the primary outcomes there were no differences in mean knowledge, decisional conflict or anxiety levels between the two decision aid groups. These results suggest that decision aids are not necessarily enhanced by auditory presentation and that written and pictorial methods of presenting risk information which are traditionally used in decision aids may be sufficient to increase knowledge, without increasing decisional uncertainty or anxiety.
Audio components of decision aids are expected to increase accessibility for sub‐groups of the population who are less educated, have lower literacy, are not familiar with risk information or the decision aid material is not presented in their home language. Findings from our post‐hoc analysis among women without university education compared with those women with university education were consistent with the primary analysis. Among this sample of women we found no differences in knowledge, decisional conflict or anxiety between the two sub‐groups and scores replicated those of the entire trial population. Although generalizability of this analysis is limited, as it is a comparison of university education vs. non‐university education, and this may not necessarily be a sufficient measure of low education or of low literacy. These results suggest that further research into the advantages of audio‐guided formats for low literacy groups is needed. However, other work by our group has found similar results that suggest it is possible that ‘traditional’ methods of presenting information in written decision aid formats may be sufficient for sub‐groups in the population with lower levels of education. Consumers from lower educational backgrounds were just as likely as others to become better informed about bowel cancer screening using a standard written decision aid. 4 There is also emerging evidence that written formats can be effective for low literacy groups especially if they incorporate linguistic frameworks. 15
Although the randomized controlled design provides confidence in the results of this study, a number of issues need to be considered when generalizing these results to other populations. The main issue is that a large proportion of study participants were university educated. This may be attributed to the hospitals from which eligible women were recruited from, which generally services women from higher socioeconomic areas. Overall we had very high participation among eligible and approached women; however, it is not known whether women who declined to participate in the study were more likely to be from lower educational groups.
Further generalizability may also be limited by the exclusion criteria of self‐assessed English sufficiency, resulting in low participation from women who speak a language other than English at home. This group is one of the main target groups for auditory decision aids and thus, we were unable to assess whether an auditory component to a decision aid increases accessibility for this population and as suggested before should be the focus of future research.
Both the audio‐guided and booklet decision aids were appropriately used and accepted by women, and all participants would recommend the decision aid they received. This finding enhances our primary analysis results, as decision aids need to be both acceptable (so that consumers use them) and effective (increase knowledge and decrease decisional conflict). This result suggests that both styles of decision aids are equally effective and useful; however, the increased complexity and costs associated with the production of the audio component without any apparent benefit bring their role into question. 1 , 3 The fast pace of change in technology also increases the difficulty of keeping audio components in a suitable format for the intended audience. Even in the time frame of this study new technology was an issue as CDs were superseded by digital files. Considering all of these factors shifts the balance in favour of the written and pictorial presentation styles.
In conclusion, this is the first trial to evaluate the relative benefit of an audio‐guided decision aid format. This evaluation highlights the lack of additional benefit in using audio‐guided formats for presenting health information to consumers who are from a general English‐speaking population. These results considered together with the increase in costs and work involved in producing audio‐guided components suggests that there is no benefit gained from audio‐guides and that written and pictorial decision aids may be sufficient, thus alleviating developers of the pressure to produce these components in the realm of limited resources.
References
- 1. O’Connor AM, Bennett CL, Stacey D et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No.: CD001431. DOI: DOI: 10.1002/14651858.CD001431. Pub 2. [DOI] [PubMed]
- 2. Iredale R, Rapport F, Sivell S et al. Exploring the requirements for a decision aid on familial breast cancer in the UK context: a qualitative study with patients referred to a cancer genetics service. Journal of Evaluation in Clinical Practice, 2008; 14: 110–115. [DOI] [PubMed] [Google Scholar]
- 3. Nassar N, Roberts C, Raynes‐Greenow C, Barratt A, Peat B, Decision Aid for Breech Presentation Trial Collaborators . Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG: An International Journal of Obstetrics and Gynaecology, 2007; 114: 325–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Trevena L, Irwig L, Barratt A. Randomized trial of a self‐administered decision aid for colorectal cancer screening. Journal of Medical Screening, 2008; 15: 76–82. [DOI] [PubMed] [Google Scholar]
- 5. Ranta P, Spalding M, Kangas‐Saarela T et al. Maternal expectations and experiences of labour pain – options of 1091 Finnish parturients. Acta Anaesthesiologica Scandinavica, 1995; 39: 60–66. [DOI] [PubMed] [Google Scholar]
- 6. Roberts C, Raynes‐Greenow C, Nassar N, Trevena L, McCaffery K et al. Protocol for a randomised controlled trial of a decision aid for the management of pain in labour and childbirth [ISRCTN52287533]. BMC Pregnancy and Childbirth, 2004; 4: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O’Connor A. Ottawa Decision Support Framework to Address Decisional Copyright 2006. Available at: http://ohri.ca/decisionaid.2006 [cited 2006].
- 8. O’Connor A. Validation of a decisional conflict scale. Medical Decision Making, 1995; 15: 25–30. [DOI] [PubMed] [Google Scholar]
- 9. Marteau TM, Bekker H. The development of a six‐item short‐form of the state scale of the Spielberger State‐Trait Anxiety Inventory (STAI). British Journal of Clinical Psychology, 1992; 31: 301–306. [DOI] [PubMed] [Google Scholar]
- 10. Degner LF, Sloan JA, Venkatesh P. The control preferences scale. Canadian Journal of Nursing Research, 1997; 29: 21–43. [PubMed] [Google Scholar]
- 11. Holmes‐Rovner M, Kroll J, Schmitt N et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Medical Decision Making, 1996; 16: 58–64. [DOI] [PubMed] [Google Scholar]
- 12. Marteau TM, Dormandy E, Michie S. A measure of informed choice. Health Expectations, 2001; 4: 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hennekens CH, Buring JE. Epidemiology in Medicine. Boston: Little, Brown and Company, 1987. [Google Scholar]
- 14. Armitage P, Berry G. Statistical Methods in Medical Research, 3rd edn Oxford: Blackwell Science Ltd, 1994. [Google Scholar]
- 15. Smith SK, Trevena L, Nutbeam D, Barratt A, McCaffery K. Information needs and preferences of low and high literacy consumers for decisions and about colorectal cancer screening: utilizing a linguistic model. Health Expectations, 2008; 11: 123–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hodnett ED, Gates S, Hofmeyr GJ, Sakala C et al Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD003766. DOI: DOI: 10.1002/14651858.CD003766.pub2. [DOI] [PubMed] [Google Scholar]
- 17. Bloom SL, McIntire DD, Kelly MA et al. Lack of effect of walking on labor and delivery. New England Journal of Medicine, 1998; 339: 76–79. [DOI] [PubMed] [Google Scholar]
- 18. Gupta JK, Hofmeyr GJ, Smyth RMD. Position in the second stage of labour for women without epidural anaesthesia Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No.: CD002006. DOI: DOI: 10.1002/14651858.CD002006.pub2. [DOI] [PubMed] [Google Scholar]
- 19. MacLennan AH, Crowther C, Derham R. Does the option to ambulate during labour confer any advantage or disadvantage? Journal of Maternal and Fetal Medicine, 1994; 3: 43–48. [Google Scholar]
- 20. Simkin P. Non‐pharmalogical methods of pain relief during labour In: Chalmers I, Enkin M, Keirse MJN. (eds) Effective Care in Pregnancy and Childbirth. Oxford: Oxford University Press, 1989: 1182–1195. [Google Scholar]
- 21. Cluett ER, Burns E. Immersion in water in labour and birth. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No.: CD000111. DOI: DOI: 10.1002/14651858.CD000111.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith CA, Collins CT, Cyna AM, Crowther CA et al. Complementary and alternative therapies for pain management in labour. Cochrane Database of Systematic Reviews, Issue 4 Art. No.: CD003521. DOI: DOI: 10.1002/14651858.CD003521.pub2, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carroll D, Moore RA, Tramer MR, McQuay HJ. Transcutaneous electrical nerve stimulation does not relieve labor pain: updated systematic review. Br J Obstet Gynaecol, 1997; 104:169–175. [DOI] [PubMed] [Google Scholar]
- 24. Rosen MA. Nitrous oxide for relief of labour pain: a systematic review. American Journal of Obstetrics and Gynecology, 2002; 186 (Suppl. 5): S110–S126. [DOI] [PubMed] [Google Scholar]
- 25. NSW Department of Health . NSW mothers and babies 1998 NSW Public Health Bulletin. Sydney: NSW Department of Health, 2000. [Google Scholar]
- 26. Bricker LM, Lavender TP. Parenteral opioids for labor pain relief: a systematic review. American Journal of Obstetrics & Gynecology, 2002; 186: S94–S109. [DOI] [PubMed] [Google Scholar]
- 27. De Kornfeld TJ, Pearson JW, Lasagna L. Methotrimeprazine in the treatment of labor pain. New England Journal of Medicine, 1964; 270: 391–394. [DOI] [PubMed] [Google Scholar]
- 28. Anim‐Somuah M, Smyth RMD, Howell CJ. Epidural versus non‐epidural or no analgesia in labour Cochrane Database of Systematic Reviews 2005, Issue 4. Art. No.: CD000331. DOI: DOI: 10.1002/14651858.CD000331.pub2. [DOI] [PubMed] [Google Scholar]
- 29. Leighton BL, Halpern SH. The effects of epidural analgesia on labor, maternal, and neonatal outcomes: a systematic review. American Journal of Obstetrics and Gynecology, 2002; 186: S69–S77. [DOI] [PubMed] [Google Scholar]
- 30. Liu EH, Sia AT. Rates of caesarean section and instrumental vaginal delivery in nulliparous women after low concentration epidural infusions or opioid analgesia: systematic review. BMJ, doi:DOI: 10.1136/bmj.38097.590810.7C (published 28 May 2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Paech MJ, Gurrin LC. A survey of parturients using epidural analgesia during labour. Considerations relevant to antenatal educators. Australian and New Zealand Journal of Obstetrics and Gynaecology, 1999; 39: 21–25. [DOI] [PubMed] [Google Scholar]


