Abstract
Background Promoting a more patient‐responsive service has been the focus of policy initiatives in newer EU states. One measure of success should be the patient’s assessment of their consultation with their doctor.
Objectives To measure consultation quality in Polish primary care using patient enablement (a patient‐driven instrument developed in the UK) and to test its theoretical framework. To compare the patient enablement outcome of different types of doctor delivering primary care in Poland following reform.
Design Cross‐sectional quantitative questionnaire survey.
Setting Random sample of primary care doctors practising within a 60‐km radius of Gdansk, Poland.
Subjects and outcome measures Patient Enablement Instrument and correlates were measured in 7924 consecutive adult consultations of 48 doctors, stratified according to training: family medicine specialists (diploma holders), non‐diplomates and general medicine doctors (polyclinic internists).
Results Completion was high (78%). The mean patient enablement score in Poland was 4.0 (SD 3.3) and mean consultation length was 10.3 min (SD 5.4 min). Consultation length and knowing the doctor are independently related to patient enablement in the Polish context. Variation between doctors is significant, but earlier differences in enablement between alternative providers have largely been ameliorated in practice.
Conclusion It is feasible to use patient enablement on a large scale at routine consultation in primary care in Poland: acceptability was good in diverse environments. The internal consistency of enablement and its relationships broadly mirror those found in the UK. The effect of patient expectations shaped by social and cultural issues influencing enablement outcome requires further investigation.
Keywords: consultation, patient enablement, patient evaluation, primary care, reform
Introduction
Primary care is the foundation of a health‐care system, 1 and the doctor–patient interchange is fundamental to delivery. Reform towards a more patient‐centred approach has been gathering pace globally and newer members of the European Union, such as Poland, have sought to develop a more patient‐centred system of primary care with assistance from, e.g. European Union and World Bank programmes. Despite rapid reform in former Communist countries, ‘evidence‐based policy making and greater public participation are needed’. 2 For primary care ‘The key relationship…is with individual patients who consult about problems they have identified themselves’. 3 This paper evaluates change towards more patient‐centred care at the fundamental level of its delivery: the consultation.
Working from a holistic and patient‐centred perspective, Howie et al. 4 has developed a patient‐driven questionnaire relating their need and their experience of the consultation process to the outcome measure of patient enablement. This study uses this Patient Enablement Instrument (PEI) 5 as an outcome measure of the consultation. The PEI consists of six questions about change in patients’ ability to cope and their change in their understanding of their health problem following a consultation. It differs from satisfaction 6 and is more concerned with empowerment. Knowing the doctor is positively related to enablement, 7 , 8 as is receiving a prescription when one is wanted. 5 , 7 Enablement is also associated with patient’s perceptions of empathic 9 and patient‐centred doctors. 10
Duration of consultation has been used as a proxy measure of quality. Longer consultations allow the recognition of patients’ psychological issues 5 , 7 and there is a positive correlation between length of consultation and enablement. 5 In this study consultation length was used as a simple reproducible measure of the process of consultation.
Poland entered the EU in May 2004 following intense reform promoting democracy and harmonization. 11 Primary health‐care development from polyclinics began a decade earlier, and included a move from a paternalistic stance towards a patient‐centred model of care based on Western European practice. A national re‐training programme with the award of a diploma for specialists in family medicine was developed. 12 This supported primary care reform and included a cascade model of training. New to Poland were the training components on core elements of primary care, 13 , 14 patient‐centred approaches, 15 communication 16 and management skills. An exploratory study of primary care doctors in Poland directly after the reform showed differences in enablement could be distinguished between groups expected to have approaches based on different paradigms: 17 specialists in family medicine who were newly trained on the patient‐centred model and had passed the diploma examination, doctors working in general medicine as internists in a polyclinic (expected to have a more biomedical approach) and an intermediate group of non‐diplomates who were working as family doctors. 17 The study we now report builds on this exploratory study.
In this paper we report a large‐scale study of patient enablement at routine consultation in primary care in Poland, and its correlates. We also compare the patient enablement outcome of different doctors delivering primary care in Poland.
Method
The area chosen for this study deliberately encompassed diversity: from the thriving Baltic port of Gdansk to remote poor rural farmland. A random sample of 51 doctors was taken from 178 registered as working in primary health care within a 60‐km radius of Gdansk. Sample size was estimated from prior work. 7 , 17 The sample was stratified to provide equal numbers of each type of possible primary care doctor (family medicine specialists who held the specialist diploma, those working as family doctors who had not taken the new examination and those doctors working in general medicine (internists in polyclinics). Three doctors declined to participate: one was wrongly classified, one was on maternity leave and one was on sick leave.
The research protocol was approved by the Regional Research Ethics Committee of Gdansk Medical Academy, Poland. Participating doctors were briefed by the investigators (WSG, PN and TP). They each recruited adult patients attending 170 consecutive consultations. Patient questionnaires were anonymized but could be related to the doctor consulted. We used a similar approach to Howie’s large‐scale UK study. 7
On entering the waiting room patients were given a written information sheet, they were given the opportunity to ask questions, and those who gave informed consent were given the questionnaire by the research assistant. Patients retained their questionnaire throughout. They completed the needs assessment section of the questionnaire prior to consultation and the PEI (Fig. 1) after the consultation.
Figure 1.
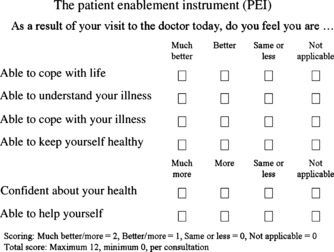
Patient Enablement Instrument (PEI).
The needs assessment captured patients’ overall problems (defined in the analysis as biomedical, social, psychological or administrative, alone or in combination) and which of these they wished to discuss. They were asked demographic details. 7 The Polish version of the 12‐item General Health Questionnaire (GHQ) measuring patients’ psychological morbidity was also included. 18 Patients assessed how well they knew the doctor on a five‐point scale, stated whether they would have preferred to see a different doctor, and whether they expected a prescription. 7
Doctors noted the duration of consultation with a stopwatch and the type of consultation (booked, fit‐in, etc.). The research assistant then collated this information. Following consultation patients placed their questionnaire in a sealed box (as in Howie’s study) 7 which was removed by the research assistant at the end of each session. Patients were told that a summary of the overall results of the study would be made available in written form to them at the practice. Doctors were told that they would be invited to a focus group to discuss these study results.
Data handling
Polish questionnaires were scanned and entered on a database in the UK using formic software (Staines, Middlesex, UK) (3.4). Accuracy was checked visually and analysis was carried out using sas software version 8.02 (SAS Institute Inc., Cary, NC, USA) and R version 2.7.1 (R Development Core Team, Vienna, Austria).
Statistical analysis
Associations between enablement and the two correlates of main interest (consultation length, and the patient’s degree of acquaintance with the doctor) were assessed via rank correlation. The relationships of enablement with three binary factors (receipt of a prescription, preference for a different doctor and psychiatric case‐ness) were estimated via Mann–Whitney U‐tests. A more detailed investigation of the determinants of enablement was performed by fitting a multiple regression model in which the patient’s enablement score was predicted by age, gender, psychiatric case‐ness, consultation length and ‘knowing the doctor’. A second model was fitted in which the doctor’s average PEI score was predicted by the same variables, aggregated to the doctor level (as means or proportions).
Results
A total of 7924 consulting patients participated with 78% (6208) completion of the PEI. The overall mean patient enablement score was 4.0 (SD 3.3, PEI scores range 0–12) and mean consultation length was 10.3 min (SD 5.4). We were unable to follow up non‐responders: their consultation duration was only slightly shorter (10.1 vs. 10.4 min for PEI completers, P = 0.03; two‐sample t‐test).
Consultations
Table 1 shows mean enablement scores and duration of consultation for each of the patient self‐reported ‘needs’.
Table 1.
Mean enablement score and duration of consultation, by ‘needs’ category
| Focus of self‐reported consultation ‘need’ | n (PEI) | Mean PEI score (SD) | n (duration) | Mean (SD) duration (min) |
|---|---|---|---|---|
| Biomedical | 1695 | 4.3 (3.3) | 2027 | 10.3 (5.4) |
| Social | 2408 | 4.1 (3.3) | 2971 | 10.3 (5.3) |
| Psychological | 471 | 4.1 (3.3) | 591 | 11.4 (5.9) |
| Complex | 1298 | 3.8 (3.0) | 1575 | 10.8 (5.6) |
| Administrative | 315 | 2.3 (3.4) | 392 | 8.9 (5.1) |
| Total (including unassigned) | 6208 | 4.0 (3.3) | 7828 | 10.3 (5.4) |
‘Needs’ categories are as defined in Ref. [7].
Mean duration of consultations in Poland were the highest in consultations that included a psychological component. Enablement scores were the highest for biomedical problems and lower for complex problems (biomedical, psychological and social in combination). Enablement was the lowest for patients with administrative needs.
Patient enablement was positively associated with consultation length (rank correlation coefficient of PEI with length: 0.13; P < 0.001; n = 6144), and with knowing the doctor (rank correlation of PEI with knowing the doctor: 0.12; P < 0.001; n = 5835). After controlling for knowing the doctor, the rank correlation of PEI with consultation length remained 0.13 (P < 0.001; n = 5773). The rank correlation of PEI with knowing the doctor, controlling for consultation length, was 0.11 (P < 0.001; n = 5773). This suggests that both consultation length and knowing the doctor were independently related to patient enablement. Enablement was also associated with the receipt of a prescription when one was expected [mean PEI for patients receiving a prescription 4.3 (SD 3.2); mean PEI for patients not receiving a prescription but expecting one 2.8 (SD 3.3); Mann–Whitney U‐test for equivalence of distributions yields P < 0.001].
Enablement was negatively associated with preference for seeing a different doctor [mean PEI for patients preferring a different doctor 2.9 (SD 3.2); mean PEI for patients not preferring a different doctor 4.1 (SD 3.2); Mann–Whitney U‐test for equivalence of distributions yields P < 0.001]; and psychological morbidity, case‐ness identified by a GHQ‐12 score of 5 or higher [mean PEI for patients with GHQ‐12 scores of 5 or above 3.8 (SD 2.9); mean PEI for patients with GHQ‐12 scores below 5 4.1 (SD 3.4); Mann–Whitney U‐test for equivalence of distributions yields P = 0.01].
Multiple regression modelling found patient’s PEI score was predicted by age (years), gender, psychological morbidity, consultation length (minutes) and knowing the doctor. Table 2 shows that patient enablement is positively associated with increased consultation length and knowing the doctor, and with female patients. Enablement was negatively associated with age and with GHQ case‐ness. The predictive power of the model was low (adjusted r 2: 0.05), indicating that most of the variance in patients’ enablement scores was not explained by these factors.
Table 2.
Regression parameter estimates for effect of five factors on enablement
| Predictor | Estimate | 95% confidence limits |
|---|---|---|
| Age (years) | −0.03 | −0.03 to −0.02 |
| Gender (female) | 0.36 | 0.20 to 0.53 |
| GHQ case‐ness | −0.29 | −0.47 to −0.11 |
| Consultation length (min) | 0.07 | 0.06 to 0.09 |
| ‘Knowing the doctor’ (one unit on five‐point scale) | 0.44 | 0.35 to 0.51 |
Results are based on data from n = 5656 consultations. As the distribution of enablement scores is markedly non‐normal, the confidence limits shown were obtained via bootstrapping. Note that due to the method of their derivation these intervals may not be precisely centred around the original point estimates. 56
Doctors
Mean enablement scores for individual doctors ranged 2.1–6.1; their distribution was approximately Normal (Shapiro–Wilk’s W = 0.97; P = 0.30). Figure 2 shows average enablement scores for the doctors in the study, in the form of a kernel density estimate plot. 19 Kernel density estimation involves estimating a probability density function by averaging across the observed data points to create a smooth approximation. A plot of the resulting values may be thought of as a ‘smoothed histogram’. 20 Mean duration of consultation for each doctor ranged from 6.2 to 16.3 min and followed a similar distribution.
Figure 2.
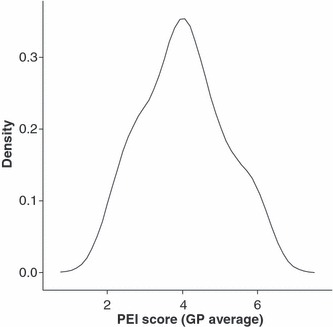
Kernel density estimate plot of doctors’ average PEI scores. NB: one doctor with a very high proportion of missing PEI scores is omitted.
The regression model of Table 2 estimates the predictors of enablement at the level of the individual consultation but provides no information on variation in average PEI scores among individual GPs. In order to provide some insight into the determinants of enablement at the level of the doctor, a second multiple regression model was fitted in which the GP’s average PEI score was predicted by the same factors as those shown in Table 2 but aggregated as doctor‐level means (in the case of age, consultation length and ‘knowing the doctor’) or proportions (for female sex and GHQ case‐ness). The parameter estimates from this doctor‐level model are presented in Table 3. The model was parameterized such that the estimates for gender and GHQ case‐ness represent the effect of each additional 1% of (respectively) female patients and GHQ cases on the doctor’s average PEI score. The adjusted r 2 value for the model was 0.29.
Table 3.
Regression parameter estimates for effect of five factors on Polish doctors’ average enablement scores
| Predictor | Estimate | 95% confidence limits | P |
|---|---|---|---|
| Mean age (years) | −0.07 | −0.12 to −0.01 | 0.02 |
| Proportion of female patients (additional 1%) | 0.04 | −0.00 to 0.07 | 0.06 |
| Proportion of GHQ cases (additional 1%) | 0.01 | −0.01 to 0.04 | 0.31 |
| Mean consultation length (min) | 0.13 | 0.01 to 0.23 | 0.03 |
| Mean ‘knowing the doctor’ score | 0.55 | −0.10 to 1.19 | 0.10 |
As the distribution of doctors’ average PEI scores was approximately normal (see Fig. 2), it was considered unnecessary to estimate confidence intervals for the coefficients via bootstrapping; those reported are based on the asymptotic standard errors derived directly from the model. One doctor with a very high proportion of missing PEI scores is omitted.
Table 3 shows that the GP’s mean patient enablement score is positively associated with average consultation length. Average PEI score is negatively related to the average age of patients. The effects of gender, psychological morbidity and knowing the doctor are not significant.
We also grouped the doctors’ data in terms of their background along the lines of the previous study. 17 Summary statistics for patient enablement scores were calculated separately for the three doctor groups described (Table 4). This suggests that the inter‐group differences are not in fact large, even though a Kruskal–Wallis test for these data returned P < 0.001. A box plot of enablement scores for the three doctor groups is shown in Fig. 3, which confirms that the distributions of PEI are very similar across the groups of doctors.
Table 4.
Summary values of Patient Enablement Instrument (PEI) for consultations hosted by three doctor groups
| Group | PEI mean (95% CI) | PEI median |
|---|---|---|
| Family medicine specialists (diplomates, n = 2030) | 4.1 (3.9–4.2) | 4.0 |
| Family doctors (non‐diplomates in family medicine, n = 1921) | 4.1 (4.0–4.3) | 4.0 |
| General medicine doctors (polyclinic internists, n = 2257) | 3.8 (3.7–3.9) | 4.0 |
Figure 3.

Box plot of PEI scores by doctor group.
Finally, we compared the Polish data from this large‐scale study with the large‐scale UK study 7 in terms of case‐mix (Table 5), and summary values of correlates of enablement (Table 6).
Table 5.
Comparison of case‐mix distribution in Polish and UK enablement studies (after ‘hierarchy of needs’ classification 6 )
| Focus of self‐reported consultation ‘need’ | Polish study, n (% of total) (total n = 7924) | UK study, 7 n (% of total) (total n = 23 799) | P* |
|---|---|---|---|
| Biomedical | 2054 (25.9) | 9413 (39.6) | <0.001 |
| Social | 3001 (37.9) | 5080 (21.4) | <0.001 |
| Psychological | 598 (7.6) | 2287 (9.6) | <0.001 |
| Complex | 1596 (20.1) | 4775 (20.1) | 0.89 |
| Administrative | 395 (5.0) | 2007 (8.4) | <0.001 |
| Unassigned | 280 (3.5) | 237 (1.0) | <0.001 |
| Wished to discuss >1 problems | 2324 (29.3) | 4760 (20.0) | <0.001 |
*Test for equality of unpaired proportions.
Table 6.
Summary values from the Polish study and the large‐scale UK study 7
| Parameter | Polish study (total n = 7924) | UK study 6 (total n = 23 799) | P |
|---|---|---|---|
| Mean (SD) PEI score | 4.0 (3.3) | 3.1 (3.4) | <0.001* |
| Mean (SD) consultation length | 10.3 (5.4) | 8.0 (4.7) | <0.001† |
| Mean (SD) knowing the doctor | 3.0 (1.1) | 3.3 (1.5) | <0.001* |
| Receipt of prescription (%) | 74.0 | 60.2 | <0.001‡ |
| Preference for a different doctor (%) | 9.5 | 10.0 | 0.22‡ |
*Mann–Whitney U‐test; Poland vs. UK.
†Two‐sample t‐test; Poland vs. UK.
‡Test for equivalence of unpaired proportions (with continuity correction); Poland vs. UK.
Discussion
Consultations
This study underlined the importance of time and knowing the doctor for enablement in Poland, as in the UK. The average patient enablement reported was higher than a similar study in the UK, 7 but consultations were longer in Poland. Patient enablement rose with consultation duration and knowing the doctor of care. PEI scores declined with increasing patient age and psychological morbidity. Individual doctor’s ability to enable was related to consultation duration and was inversely related to the patient’s age. Comparison of the different types of doctor delivering primary care in Poland in terms of patient enablement outcome showed that the early differences between the groups with differing backgrounds at the start of the reforms had largely been ameliorated.
The use of any such instrument brings with it the uncertainty of reported outcome reflecting the patient’s internalized experience. Values for Cronbach’s α in Poland were identical with the UK study, 7 and similar to other studies 5 , 21 supporting high internal reliability. Completion was comparable with that attained in the UK 7 despite initial concerns about patient engagement and literacy. Test/re‐test reliability was not measured, but an exploratory study demonstrated consistent values. 17 The higher overall enablement score seen here (relative to the UK study) 7 is consistent with an earlier smaller Polish study, 17 and other language patient–doctor consultations in the UK 22 , 23 and elsewhere. 24 , 25 Mead et al. 8 has found that ethnic groups in the UK report higher enablement even when other inputs are controlled for (e.g. need, knowing the doctor, etc.).
Alternatively Polish patients may have a different expectations and a different ‘threshold’ and are enabled, or disposed to report high enablement due to social and cultural factors. A comparison of scores on individual PEI items between this and the UK study 7 showed that Polish patients’ average score was higher except for the ‘understanding illness’ question. There is evidence that Polish patients not only feel their doctors are important, but trust in doctors remains high and Polish patients ‘viewed medicine as a useful tool…but felt they had responsibility for their own health’; 26 so, patients may enter the consulting room in a frame of mind that facilitates enablement. Consultation outcome depends on the problem presented, patient and doctor characteristics, the nature of their relationship and how these complex issues are explored and resolved. 27 The impact of patient expectations on patient enablement needs to be explored further incorporating a qualitative approach.
Patient need exhibited significant differences from those in the UK. 7 High inflation (10% in 2000) 28 and unemployment (18.1–20.3%) 29 in Poland underpin a higher burden of social problems. A study in Poland found family doctors were expected to provide moral support with social problems in addition to provision of medical care, 26 in contrast to other European countries where social need was not found to be so prominent. 30 , 31 A survey of providers 32 highlights another issue: Polish patients may have a legacy of less confidence in presenting biomedical problems directly to primary care, dating from the previous system, which could account for the lesser prominence of these problems seen here. The reforms have supported capacity building in primary care, but there is an inevitable time lag before this is widely accepted by the public, 2 and patient expectations are key.
There were lesser differences in the psychological and administrative components of case mix between countries. Psychological problems are probably under‐reported in Poland, as has been found in other studies, 30 , 33 , 34 probably due to stigma and under‐representation in Polish primary care. 35 The level of psychological morbidity was consistent with previous work in Poland, 18 and it was more difficult for patients with psychological distress to feel enabled. This agrees with work by Mercer and Watt 36 who found that patients who were GHQ cases in areas of high socio‐economic deprivation in Scotland reported lower enablement, and contrasts with Howie’s UK study 7 where patients who displayed psychological morbidity had normal PEI scores but longer consultations.
Administrative needs were reported as burdensome by Polish GPs in feedback sessions, in fact they were higher in the comparable UK study. 7 This reflects increasing administrative roles undertaken by GPs everywhere due to ongoing reform. 37 Exactly the same proportion of patients in both countries recognized their problem as ‘complex’: the domain of a bio‐psychosocial approach, and holistic patient‐centred primary care.
Relatively more Polish people wished to discuss multiple problems in a consultation, which may relate to problems of access and accessibility. A European comparison of patient experience cited difficulty with access as key. 26 However, a study of primary care in Krakow found that 66% of patients were ‘very much satisfied’ with access, but the financial underpinning was problematic. 38 Studies have found a high rate of prescribing 30 , 32 , 39 , 40 in Poland, consistent with findings here, and patient enablement increased when patients’ expectations of receiving a prescription were fulfilled, as in the UK. 7
Sufficient consultation time is a global concern. 41 The longer mean consultation time in Poland relative to the UK is common in Europe, 32 , 42 and increased enablement would be expected. 7 Mercer et al. 43 has found higher enablement resulted from longer consultations for patients with complex problems in a deprived area of Scotland. A comparison of consultation length across Europe which included Poland and the UK 42 has shown that almost 25% of total variance in consultation length is due to health‐care system factors, a similar amount due to doctor factors and the majority rests with patient factors. The complex interplay of these influences on consultation time, and its relation to enablement, requires further study.
Doctors
Analysis at the doctor level found that consultation length was important for enablement but not knowing the doctor, in contrast to findings elsewhere. 5 This may be due to the fact that patient lists were introduced more recently in Poland by comparison with the UK, where patients were more likely to know their doctor. Polish doctors have longer consultations and may enable their patients more (despite a challenging case mix and an evolving discipline). Little et al. 10 has emphasized the importance of patient‐centred doctors with a positive approach to patient’s problems on their enablement – these doctors could have experienced the reforms themselves as enabling. Mercer et al. 9 , 21 , 44 has highlighted the importance of empathy in supporting enablement. Poland and the Gdansk region, in particular, have had a long tradition of stressing the importance of empathy in practice, from undergraduate training onwards. 45 , 46 , 47
A study examining the results of primary care reform in Poland with the first graduates of the diploma examination in family medicine had demonstrated difference in patient enablement outcome according to whether the doctor involved was a diplomate family medicine specialist, a family doctor who had not participated in the training or obtained the diploma, and a general medical doctor working as an internist in a polyclinic. 17 Patients attending these groups of doctors in this study reported similar enablement (statistical significance appears to be more related to sample size than practice). This may be a failure of the training course, or it may be due to the interplay of other factors.
Individual variation is a feature of patient enablement 5 , 17 and the doctors sampled in the smaller study were exemplars, and those enthusiastic early adopters may have declined in the diploma group as this becomes the norm. Possession of the professional examination in the UK (Membership of the Royal College of General Practitioners) has not been linked to increased patient enablement. 48
Since the first reforms there has been an explosion of pluralism in primary care delivery with a proliferation of public, private and mixed primary care providers working under a variety of contracts. One study of providers in Krakow reports eight such groups, with some doctors working in two sectors. 49 This makes distinguishing between them in terms of approach more difficult, and could account for the later moderation of differences between doctor groups in terms of enablement. There is also some evidence that the pragmatic concerns of contractual negotiations, payment and the development of a competitive free market has distracted doctors from enacting patient‐centred approaches in the consultation more fully. 50
The EU Phare programme funded a 5‐year input supporting harmonization, with western EU educationalists mentoring their Polish colleagues, establishing individual links and an in‐country cascade training programme to establish primary care. However, this was also a time of change for academic family medicine in this region. The professor of family medicine, who had an established reputation for research into empathy and education, 47 , 51 , 52 retired, and the teaching pair of doctors who had been trained directly in western Europe moved on. Others have found leadership and faculty development essential in establishing new educational programmes 53 and in fostering sustainability.
Perhaps it is not that surprising that differences between groups of doctors attenuate post‐harmonization. As such major societal and political shifts have occurred in Poland in a short period of time it is naïve to consider medical education as an isolated input into a complex system. 54 Evaluation of such a complex intervention is acknowledged as difficult. 55 Nonetheless, there are now 20 000 doctors working in primary care in Poland, and of these 10 000 are family medicine diplomates. There is evidence from this study and others that patients in Poland have improved access to primary health care and are more satisfied. 26 , 50
A limitation of this study is that it was conducted in a single area of Poland; however, it successfully involved a large number of patients from disparate socio‐economic backgrounds and a random sample of doctors in a wide variety of environments in routine daily practice in Poland. The PEI is a self‐report measure, and as such may be subject to social desirability bias. However, care was taken to ensure patient and doctor anonymity. The Polish version of the PEI was previously used in an exploratory study, 17 as was the GHQ‐12. 18
In Poland significantly higher enablement scores were attained, and consultations were longer than in the UK. Although many correlates were similar, increasing age and psychological morbidity were negatively related to enablement. Predictive models at the consultation and doctor levels were significant but suggested unmeasured factors are important. Further exploration (using qualitative approaches) would be of value. Early differences in patient enablement between types of doctor delivering primary care in Poland have been ameliorated.
Conclusion
This study supports the use of patient enablement as an outcome measure at routine consultation in primary care in Poland: acceptability was good in diverse environments. The internal consistency of the PEI and its relationships broadly mirror those found in the UK: increased enablement is achieved with a longer consultation time, with greater continuity of care and when the expectation of receipt of a prescription is fulfilled. Although variation between doctors is significant, earlier differences in patient enablement by the different types of doctor delivering primary care have largely been ameliorated in practice. The effect of patient expectations shaped by social and cultural issues impacting on the consultation in primary care and influencing enablement outcome requires further investigation.
Funding
Royal College of General Practice Scientific Foundation Board Grant SFB31. All of the authors were independent of The Royal College of General Practitioners (UK). TP was a consultant in the initial development of primary care in Poland under the terms of the EU Phare Project and PN an original participant.
Acknowledgements
We thank all the patients, doctors and practice managers in the Gdansk region who participated in this study. We thank Parimal Patel and Formic Ltd. for assistance in data handling. Ethical approval was granted by The Medical Academy, Gdansk University.
References
- 1. WHO . Declaration of Alma‐Ata. The International Conference on Primary Health Care, Alma‐Ata, 1978. Available at: http://www.searo.who.int/LinkFiles/Health_Systems_declaration_almaata.pdf, accessed on 4 August 2009. [Google Scholar]
- 2. Fister K, McKee M. Health and health care in transitional Europe. BMJ, 2005; 331: 169–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McWhinney I. Primary care: core values. Core values in a changing world. BMJ, 1998; 316: 1807–1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Howie J, Heaney D, Maxwell M. Quality, core values and the general practice consultation: issues of definition, measurement and delivery. Family Practice, 2004; 21: 458–468. [DOI] [PubMed] [Google Scholar]
- 5. Howie J, Heaney D, Maxwell M. Measuring quality in general practice. Occasional Paper/Royal College of General Practitioners, 1997; 75: 32. [PMC free article] [PubMed] [Google Scholar]
- 6. Howie J, Heaney D, Maxwell M, Walker J. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Family Practice, 1998; 15: 165–171. [DOI] [PubMed] [Google Scholar]
- 7. Howie J, Heaney D, Maxwell M, Walker J, Freeman G, Rai H. Quality at general practice consultations: cross‐sectional survey. BMJ, 1999; 319: 738–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mead N, Bower P, Roland M. Factors associated with enablement in general practice: cross‐sectional study using routinely collected data. The British Journal of General Practice, 2008; 58: 346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mercer S, Reilly D, Watt G. The importance of empathy in the enablement of patients attending the Glasgow Homoeopathic Hospital. The British Journal of General Practice, 2002; 52: 901–905. [PMC free article] [PubMed] [Google Scholar]
- 10. Little P, Everitt H, Williamson I et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ, 2001; 323: 908–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. EC . Commission enlargement: The Phare Programme. Available at: http://ec.europa.eu/enlargement/financial_assistance/phare/index_en.htm, accessed 27 March 2007.
- 12. Windak A, Tomasik T, Kryj‐Radziszewska E. The Polish experience of quality improvement in primary care. Joint Commission Journal on Quality Improvement, 1998; 24: 232–239. [DOI] [PubMed] [Google Scholar]
- 13. Starfield B. Primary Care: Concept, Evaluation and Policy. New York: Oxford University Press, 1992. [Google Scholar]
- 14. Pringle M. Core Values in Primary Care. London: BMJ Books, 1998. [Google Scholar]
- 15. Stewart M, Brown J, Weston W, McWhinney I, McWilliam C, Freeman T. Patient‐Centred Medicine, Transforming the Clinical Method. Thousand Oaks, CA: Sage, 1995. [Google Scholar]
- 16. Silverman J, Kurtz S, Draper J. Skills for Communicating with Patients, 2nd edn Abingdon: Radcliffe Publishing Ltd, 2005. [Google Scholar]
- 17. Pawlikowska T, Nowak P, Szumilo‐Grzesik W, Walker J. Primary care reform: a pilot study to test the evaluative potential of the Patient Enablement Instrument in Poland. Family Practice, 2002; 19: 197–201. [DOI] [PubMed] [Google Scholar]
- 18. Makowska Z, Merecz D, Moscicka A, Kolasa W. The validity of general health questionnaires, GHQ 12 and GHQ 28, in mental health studies of working people. International Journal of Occupational Medicine and Environmental Health, 2002; 15: 353–362. [PubMed] [Google Scholar]
- 19. Silverman BW. Density Estimation for Statistics and Data Analysis. New York: Chapman & Hall, 1986. [Google Scholar]
- 20. Hintze JL, Nelson RD. Violin plots: a box plot – density trace synergism. American Statistician, 1998; 52: 181–184. [Google Scholar]
- 21. Mercer S, Howie J. CQI‐2‐ a new measure of holistic interpersonal care in primary care consultations. British Journal of General Practice, 2006; 56: 262–268. [PMC free article] [PubMed] [Google Scholar]
- 22. Freeman GK, Rai H, Walker J, Howie J, Heaney D, Maxwell M. Non‐English speakers consulting with the GP in their own language: a cross‐sectional survey. British Journal of General Practice, 2002; 52: 36–38. [PMC free article] [PubMed] [Google Scholar]
- 23. Denley J, Rao J, Stewart A. How do patients rate the quality of consultations in primary care? A patient enablement survey within a primary care trust in Sandwell Quality in Primary Care, 2003; 11: 181–187. [Google Scholar]
- 24. Wensing M, Wetzels R, Hermsen J, Baker R. Do elderly patients feel more enabled if they have been actively involved in primary care consultations? Patient Education and Counseling, 2007; 68: 265–269. [DOI] [PubMed] [Google Scholar]
- 25. Jaturapatporn D, Dellow A. Does Family Medicine training in Thailand affect patient satisfaction with primary care doctors? BMC Family Practice, 2007; 8: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Coulter A, Magee H. The European Patient of the Future. Maidenhead: Open University Press, 2003. [Google Scholar]
- 27. Baerheim A. The diagnostic process in general practice: has it a two‐phase structure? Family Practice, 2001; 18: 243–245. [DOI] [PubMed] [Google Scholar]
- 28. Kwasnicki W. Inflation in Poland. Wroclaw: Institute of Economic Sciences, Wroclaw University, 2001. Available at: http://prawo.uni.wroc.pl/~kwasnicki/inflation_in_poland.htm, accessed 24 January 2007. [Google Scholar]
- 29. Gardawski J. The Dynamics of Unemployment in Poland. Poland: The European Industrial Relations Observatory (EIRO), 2002. Available at: http://www.eiro.eurofound.eu.int/2002/10/feature/pl0210110f.html. [Google Scholar]
- 30. Van der Brink‐Muinen A, Verhaak P, Bensing J et al. An International Comparative Study in Six European Countries on Doctor–Patient Communication in General Practice. Utrecht: Netherlands Institute for Health Services Research (NIVEL), 1999. [Google Scholar]
- 31. Gulbrandsen P, Fugelli P, Sandvik L, Hjortdahl P. Influence of social problems on management in general practice; multi‐practice questionnaire survey. BMJ, 1998; 317: 28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Boerma W. Profiles of General Practice in Europe. An International Study of Variation in the Tasks of General Practitioners. Utrecht: Netherlands Institute for Health Services Research (NIVEL), 2003. [Google Scholar]
- 33. Ustun T, Sartorius N. Mental Illness in General Health Care. Chichester: Wiley for WHO, 1995. [Google Scholar]
- 34. Fleming D, Pavlic D. Information from primary care: its importance and value, a comparison of information from Slovenia, England and Wales viewed from the “Health 21” perspective. European Journal of Public Health, 2002; 12: 249–253. [DOI] [PubMed] [Google Scholar]
- 35. Jenkins R, Klein J. Mental health in post‐communist countries. BMJ, 2005; 331: 173–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mercer S, Watt G. The Inverse Care Law: Clinical Primary Care Encounters in Deprived and Affluent Areas of Scotland. Annals of Family Medicine, 2007; 5: 503–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Helman C. The culture of general practice. British Journal of General Practice, 2002; 52: 619–620. [PMC free article] [PubMed] [Google Scholar]
- 38. Margas G. Ocena jakosci opeiki medycznej oswiadczonej przez lekarzy rodzinnych [An evaluation of the quality of medical care offered by family doctors]. Krakow: University of Krakow, 2003. [Google Scholar]
- 39. Windak A, Tomasik T, Jacobs H, De Melker R. Are antibiotics over‐prescribed in Poland? Family Practice, 1996; 13: 445–449. [DOI] [PubMed] [Google Scholar]
- 40. Touw‐Otten F, Johansen K. Diagnosis, antibiotic treatment and outcome of acute tonsillitis: report of a WHO Regional Office for Europe study in 17 European countries. Family Practice, 1992; 9: 255–262. [DOI] [PubMed] [Google Scholar]
- 41. Morrison I, Smith R. Hamster health care. BMJ, 2000; 321: 1541–1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Deveugele M, Derese A, Van Den Brink‐Muinen A, Bensing J, De Maesener J. Consultation length in general practice: cross‐sectional study in six European countries. BMJ, 2002; 325: 472–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mercer S, Fitzpatrick B, Goulay G, Vojt G, McConnachie A, Watt G. More time for complex consultations in a high‐deprivation practice is associated with increased patient enablement. The British Journal of General Practice, 2007; 57: 960–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mercer S, Reynolds W. Empathy and quality of care. The British Journal of General Practice, 2002; 52: S9–S13. [PMC free article] [PubMed] [Google Scholar]
- 45. Koseda M, Hebanowski M. Examination of medical graduates. Polski Tygodnik Lekarski, 1982; 37: 837–840. [PubMed] [Google Scholar]
- 46. Turczynska K, Ksiezoplska‐Kaczorowska A, Hebanowski M, Komorowska‐Szczepanska W. Empathy and motives in choosing medical studies as possible predictors of future physician’s career performance. Polski Merkuriusz Lekarski, 2003; 14: 243–247. [PubMed] [Google Scholar]
- 47. Kliszcz J, Hebanowski M. Studies on empathy in doctors and medical students. Polski Merkuriusz Lekarski, 2001; 11: 154–157. [PubMed] [Google Scholar]
- 48. McKinstry B, Guthrie B, Freeman G, Heaney D. Is success in postgraduate examinations associated with family practitioners’ attitudes or patient perceptions of the quality of their consultations? Family Practice, 2005; 22: 653–657. [DOI] [PubMed] [Google Scholar]
- 49. Chawla M, Berman P, Windak A, Kulis M. Provision of ambulatory health services in Poland: a case study from Krakow. Social Science and Medicine, 2004; 58: 227–235. [DOI] [PubMed] [Google Scholar]
- 50. Marcinowicz L, Konstantynowicz J, Chlabicz S. The patient’s view of the acceptability of the primary care in Poland. International Journal for Quality in Health Care, 2008; 20: 277–283. [DOI] [PubMed] [Google Scholar]
- 51. Kliszcz J, Hebanowski M, Rembowski J. Emotional and cognitive empathy in medical schools. Academic Medicine, 1998; 73: 541. [DOI] [PubMed] [Google Scholar]
- 52. Kliszcz J, Trzeciak B, Hebanowski M. Communication skills: how do we teach them to medical students? Medical Education, 1999; 33: 628–629. [DOI] [PubMed] [Google Scholar]
- 53. Mennin S, Krackov K. Reflections on relevance, resistance and reform in medical education. Academic Medicine, 1998; 73: S60–S64. [DOI] [PubMed] [Google Scholar]
- 54. Ijsselmuiden C. Towards unity for health: time to think systems. Education for Health, 2007; 20: 59. [PubMed] [Google Scholar]
- 55. Musick D. A conceptual model for program evaluation in graduate medical education academic medicine. Academic Medicine, 2006; 81: 759–765. [DOI] [PubMed] [Google Scholar]
- 56. Efron B, Tibshirani R. Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Statistical Science, 1986; 1: 54–77. [Google Scholar]


