Abstract
Objective The National Infarct Angioplasty Project assessed the feasibility of establishing a comprehensive primary angioplasty service. We aimed to compare satisfaction at intervention hospitals offering angioplasty‐based care and control hospitals offering thrombolysis‐based care.
Design Mixed methods, with postal survey of patients and their carers, supported by semi‐structured interviews.
Setting and participants Survey of 682 patients and 486 carers, and interviews with 33 patients and carers, in eight English hospitals.
Interventions Primary angioplasty or thrombolysis.
Main outcome measures Satisfaction with treatment.
Results Responses were received from 595/682 patients (87%) and 418/486 carers (86%). Satisfaction with overall care was high at both intervention and control sites (78% vs. 71% patients rated their care as ‘excellent’, P = 0.074). Patient satisfaction was higher at intervention sites for some aspects of care such as speed of treatment (80% vs. 67%‘excellent’, P = 0.001). Convenience of visiting was rated lower at intervention sites by carers (12% vs. 1%‘poor’, P = 0.001). During interviews, carers reported that they accepted the added inconvenience of visiting primary angioplasty sites in the context of this life‐saving treatment. Patient satisfaction with discharge and aftercare was lower in both treatment groups than for other aspects of care.
Conclusions Reorganization of care to offer a primary angioplasty service was acceptable to patients and their carers. Satisfaction levels were high regardless of the type of care received, with the exception of discharge and aftercare.
Keywords: angioplasty, myocardial infarction, patient satisfaction
Primary angioplasty as an alternative to intravenous thrombolysis for patients with acute ST‐elevation myocardial infarction (STEMI) has been shown to reduce mortality, re‐infarction, stroke and the need for coronary artery bypass grafting. 1 Economic analyses suggest that if both treatments are routinely available, primary angioplasty is likely to be cost‐effective if it can be delivered in a timely manner. 2 In the United Kingdom (UK), primary angioplasty is not currently the standard treatment for patients with STEMI, although rates are increasing rapidly with over one in five STEMI patients receiving reperfusion having primary angioplasty in England and Wales in 2007/8. 3 Health policy makers in England have advocated expediting the process of making primary angioplasty the principal treatment for STEMI patients. 4
In 2004, the British Cardiac Society and the Department of Health established a working group to consider the feasibility of implementing a countrywide primary angioplasty service for patients with STEMI in England. Ten hospitals offering primary angioplasty took part in the National Infarct Angioplasty Project (NIAP) during 2005–6 and collected data on call and treatment times, clinical measures and outcomes for all patients admitted to their hospitals during the year. The sites represented a range of potential service models, including single centres, centres taking referrals from local hospitals and networks of centres working together to serve local populations. 5 Due to the specialist facilities and staffing required, the routine provision of primary angioplasty required significant reorganization of services, with patients transferring from, or bypassing, local emergency departments to go to a primary angioplasty centre. There are concerns that centralization of services will adversely affect patient satisfaction, 6 , 7 , 8 and in this case that carers would be inconvenienced by having to travel greater distances to primary angioplasty centres.
To date there has been little consideration of the views of patients or their carers regarding the development of primary angioplasty services. Existing research focuses largely upon experiences of angioplasty as an elective procedure. 9 As part of an independent evaluation of the NIAP pilot sites, we undertook a study of patients’ and carers’ views of care provided at NIAP sites compared with views of patients and carers at hospitals providing mainly thrombolysis‐based care.
Methods
Design and setting
The study was part of a wider evaluation which included studies of the workforce and economic implications of NIAP. The patient and carer satisfaction component of this wider study was a cross‐sectional comparison of care provided in four hospitals offering mainly primary angioplasty (intervention sites) and four hospitals offering mainly thrombolysis‐based care (control sites) in England. A mixed methods design was used 10 drawing on the strengths of quantitative research to measure differences in patient and carer satisfaction between hospitals offering mainly primary angioplasty and those offering mainly thrombolysis, and the strengths of qualitative research to understand the important components of satisfaction and elaborate on the findings from the quantitative research. 11 The study was undertaken in three phases: qualitative interviews with patients and carers to understand the key aspects of their experience and to develop a questionnaire for use in the survey; a survey of patients and carers in both intervention and control hospitals; and further qualitative interviews with patients to examine issues raised in earlier phases of the study.
Recruitment
For the ‘phase 1’ interviews, nurses approached patients with STEMI who were admitted to hospital at two of the intervention sites. Consent was gained for a researcher to approach both the patient and their carer for interview. We used purposive sampling to select interviewees experiencing the range of referral routes within NIAP sites (i.e. via the emergency department, direct to catheter lab, hospital bypass). Based on these interviews we developed a questionnaire for patients and a questionnaire for carers. For the ‘phase 2’ survey, nurses recorded the admission of all patients with STEMI at the four intervention and four control sites. To comply with ethics committee requirements, nurses asked patients to consent to being sent a questionnaire and to provide details of a carer where possible. Patients who were critically ill, unable to consent due to cognitive impairment, or unable to understand English were excluded. A questionnaire, and up to two reminders, were then sent to patients and carers at around 1 week after admission. Recruitment took place between February and November 2007. For the ‘phase 3’ interviews, we followed up an issue which arose from phase 1 by selecting survey respondents who felt that they had been ‘fixed’ by their treatment or not, 12 and also followed up an issue which arose from phase 2 by selecting survey respondents who reported their discharge and aftercare as unsatisfactory.
Interview schedules and questionnaire
The phase 1 interviews followed a critical incident technique to identify key aspects of care. 13 Interviewees were asked to describe the positive and negative aspects of their experience from onset of symptoms to discharge home. The development of the phase 2 questionnaire was informed by the research brief and findings from the phase 1 interviews. The patient questionnaire consisted of 27 satisfaction items using a five point scale ‘excellent’‘very good’‘good’‘fair’‘poor’ and the extra option of ‘not sure’ because some patients may have been unaware of events for parts of their care. Items addressed communication with staff, speed and efficiency of care, management of pain and comfort, convenience of family visiting the hospital, discharge, post‐discharge care, the different places of care, and care overall. Other questions addressed demographical information, experience of transfer between hospitals and permission for an interview at a later time. There were four open‐ended questions about good and poor aspects of care. The carer questionnaire was similar, with a focus on convenience of visiting the patient. Phase 3 interviews focused on care after discharge from hospital.
Analysis
Survey data was analysed using SPSS version 12.0 and STATA version 8. We dichotomized satisfaction items into ‘excellent’ vs. ‘very good to poor’, because patients who tick ‘excellent’ tend to find no fault with a service. 14 We undertook multilevel logistic regression accounting for clustering by site using the XTLOGIT function in STATA. We adjusted for age and sex to determine whether the proportion of patients reporting ‘excellent’ differed in intervention and control sites. It was important to adjust for age because older people tend to report higher levels of satisfaction. 15 Because of the large number of statistical tests undertaken, the significance level was taken as P < 0.01 rather than the usual P < 0.05. Free text comments at the end of the questionnaire were read by one of the authors (FS) and key themes were identified. 16 These indicated the strength of feeling that respondents had about certain aspects of their care and elucidated answers within the structured part of the questionnaire.
The interviews were transcribed verbatim. We used the first stages of ‘framework analysis’ 17 by reading transcripts to identify themes and coding all transcripts systematically according to the thematic framework. The way in which different aspects of having primary angioplasty contributed to a sense of ‘feeling fixed’ has been published elsewhere. 12 Here, we report only the aspects of the qualitative findings which elaborate on the quantitative survey results.
Presentation of results
Three types of results are presented below. First, the survey data is used to identify differences between intervention and control sites. Second, the proportion of survey respondents reporting ‘excellent’ care is compared for the range of satisfaction items to identify poorly perceived aspects of care. Finally, findings from the interviews, and free text comments from the survey, are used to elaborate on issues raised in the survey data. We have combined these results within a set of themes addressing key aspects of care.
Results
Sample characteristics
Survey
For the survey, 1165 STEMI patients were identified across all eight sites, of whom 144 did not meet inclusion criteria (see Fig. 1). Of the 1021 eligible patients, 682 (67%) were recruited into the study. There was no difference in recruitment rates between intervention and control sites: 66% (432/659) vs. 69% (250/362), P = 0.255. Reasons for non‐recruitment included patient refusal, patients being missed, or patients being discharged or transferred before nurses could approach them for consent. Patients who were recruited were younger than non‐recruited patients (mean age 62 vs. 67, P = 0.001) and a higher proportion of males was recruited than females (60% vs. 51%, P = 0.006).
Figure 1.
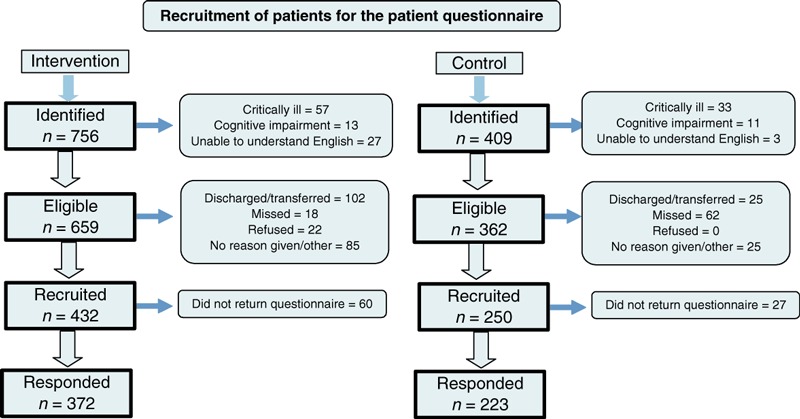
Flow diagram of patients recruited for the patient questionnaire.
The response rate to the survey was 87% (595/682) for patients and 86% (418/486) for carers. Questionnaires were completed on average 4 weeks after admission. There was no difference in response rates between intervention and control sites for patients (86% vs. 89%, P = 0.244). The response rate was similar for male and female patients (87% vs. 89%, P = 0.588) but respondents were older than non‐respondents (mean age 62 vs. 59, P = 0.033). Any statistically significant differences between patient respondents in intervention and control sites were related to the standard treatment offered within those sites (Table 1). That is, patients in intervention sites were more likely to have primary angioplasty and be transferred between hospitals.
Table 1.
Characteristics of respondents to patient and carer surveys
| Intervention % (n/N) | Control % (n/N) | All % (n/N) | P | |
|---|---|---|---|---|
| Patients | ||||
| Male | 76% (282/372) | 74% (165/223) | 75% (447/595) | 0.633* |
| Mean age (range, SD) | 63.1 (25–92, 12.04) | 61.34 (25–92, 12.02) | 62.4 (25–92, 12.05) | 0.098† |
| Primary angioplasty received | 92% (341/372) | 5% (12/223) | 59% (353/595) | <0.001* |
| Admission ‘in hours’ | 39% (116/297) | 38% (78/203) | 39% (194/500) | 0.886* |
| Transfer to second hospital | 28% (101/366) | 6% (13/215) | 20% (114/581) | <0.001* |
| Carers | ||||
| Male | 22% (59/263) | 19% (28/147) | 21% (87/410) | 0.421* |
| Mean age (range, SD) | 55 (16–85, 14.06) | 57 (22–90, 13.2) | 56 (16–90, 13.8) | 0.106† |
| Living with patient | 82% (216/262) | 86% (127/148) | 84% (343/410) | 0.376* |
*Chi‐square.
†Student t‐test.
Interviews
Prior to the survey, we undertook interviews with ten patients and six carers from intervention sites on average 2 weeks post‐admission. After the survey, we interviewed a further 11 patients at intervention sites and six patients at control sites who had responded to the survey.
Overall satisfaction
Satisfaction levels with different aspects of care are displayed in descending order for patients (Table 2) and carers (Table 3). Overall satisfaction with care was high in both intervention and control sites, for patients and carers. Although it appeared that overall satisfaction was higher at intervention than control sites for both patients (78% vs. 71%‘excellent’) and carers (63% vs. 55%‘excellent’), these were not statistically significantly different (P = 0.074 and P = 0.116 respectively). This was reflected in the open comments on the questionnaires and in the qualitative interviews. Both patients and carers praised the care, with almost one in ten patients adding additional comments to the questionnaire about how excellent their treatment had been. During interviews, patients referred to their treatment as ‘exceptional’ or ‘first class’ and expressed gratitude for the service they had received.
Table 2.
Patient satisfaction with hospital treatment for a heart attack (% rating each aspect of care as ‘excellent’)
| Intervention % (n/N) | Control % (n/N) | Adjusted odds ratio (95% CI)* | P‐value | |
|---|---|---|---|---|
| (a) Efficiency with which you were treated | 83% (305/369) | 74% (162/219) | 1.72 (1.14, 2.59) | 0.009 |
| (b) Professional skill and ability of doctors and nurses | 81% (297/368) | 73% (161/221) | 1.50 (1.10, 2.24) | 0.052 |
| (c) Overall experience of being treated for a heart attack | 78% (287/367) | 71% (155/218) | 1.42 (097, 2.09) | 0.074 |
| (d) Time waited before having treatment | 80% (292/364) | 67% (148/219) | 2.17 (1.45, 3.22) | 0.001 |
| (e) Confidence in doctors and nurses treating you | 75% (278/369) | 69% (151/219) | 1.32 (0.86, 2.03) | 0.549 |
| (f) Confidence in the treatment received | 71% (263/370) | 61% (134/218) | 1.52 (1.06, 2.17) | 0.022 |
| (g) Explanations given about what was wrong with you | 56% (206/365) | 50% (109/220) | 1.18 (0.68, 2.03) | 0.549 |
| (h) Ease and convenience for friends and family to visit | 54% (196/363) | 51% (111/219) | 1.12 (0.80, 1.58) | 0.502 |
| (i) Explanations given of risks & benefits of treatment | 47% (170/361) | 44% (96/216) | 1.07 (0.70, 1.62) | 0.750 |
| (j) Time spent waiting to be discharged from hospital | 38% (115/306) | 46% (84/182) | 0.77 (0.51, 1.55) | 0.205 |
| (k) Involvement in decisions about treatment | 37% (133/357) | 32% 70/216) | 1.23 (0.75, 2.01) | 0.409 |
| (l) Information about medication & potential side‐effects | 34% (104/308) | 38% (69/183) | 0.81 (0.54, 1.23) | 0.322 |
| (m) Support and follow‐up provided once left hospital | 36% (108/300) | 32% (56/175) | 1.04 (0.62, 1.75) | 0.873 |
| (n) Information given about how to manage condition in future | 25% (78/311) | 30% (55/182) | 0.68 (0.47, 0.99) | 0.049 |
*Adjusted for patient age and sex.
Table 3.
Carer satisfaction with hospital treatment for a heart attack (% rating each aspect of care as ‘excellent’)
| Intervention % (n/N) | Control % (n/N) | Adjusted odds ratios (95% CI)* | P‐value | |
|---|---|---|---|---|
| (a) Professional skill and ability of doctors & nurses | 75% (198/265) | 66% (98/149) | 1.31 (0.63, 2.71) | 0.468 |
| (b) Confidence in doctors & nurses treating patient | 68% (181/265) | 65% (97/149) | 0.99 (0.49, 2.23) | 0.985 |
| (c) Overall impression of treatment & care in hospital | 63% (167/263) | 55% (81/147) | 1.50 (0.90, 2.49) | 0.116 |
| (d) Reassurance and support offered | 60% (158/265) | 55% (82/144) | 1.20 (0.70, 2.06) | 0.503 |
| (e) Confidence in the treatment received | 59% (157/265) | 53% (79/147) | 1.10 (0.55, 2.22) | 0.783 |
| (f) Information you were given about what was happening to patient | 49% (130/263) | 43% (64/149) | 1.23 (0.71, 2.14) | 0.462 |
| (g) Opportunity to ask doctors and nurses questions | 51% (135/266) | 37% (55/149) | 1.79 (1.06, 3.01) | 0.028 |
| (h) Convenience of hospital for you to visit patient | 28% (72/261) | 34% (50/145) | 0.72 (0.46, 1.12) | 0.149 |
| (i) Visiting times | 30% (77/258) | 31% (46/148) | 0.93 (0.54, 1.60) | 0.799 |
| (j) Facilities available to visitors | 28% (71/254) | 19% (28/144) | 1.61 (0.93, 2.78) | 0.089 |
*Adjusted for carer age and sex.
The way I was treated by the staff from the cleaner to the doctors was excellent and if private care is better then I would like to see it (patient 15, survey)
Speed and efficiency
Patients were very satisfied with the time they waited for treatment, and the efficiency with which they were treated, with significantly higher satisfaction levels at intervention than control sites for both aspects of care [see items (a) and (d), Table 2]. Again, these high levels of satisfaction were reflected in the open comments on the questionnaire and in the qualitative interviews. During the interviews at intervention sites, patients and carers expressed amazement at the short time period between contacting the emergency services to the completion of treatment. They perceived an efficiency and ‘smoothness’ in the care provided, and were impressed at the teamwork involved, often describing how the team were awaiting their arrival.
This for me was the NHS working at its very best. From the 999 call to coming out of surgery took 3.5 h (patient 307, survey)
The speed/efficiency of (transfer hospital) sending me to the (intervention hospital) who, in turn, dealt with me with such speed that I was in the door, up the lift and straight into theatre – brilliant! (patient 242, survey)
Convenience of care
Carers in general had lower levels of satisfaction with convenience of visiting than for other aspects of care [see items (h) and (i), Table 3]. There was no difference between intervention and control sites in proportions rating convenience of visiting as ‘excellent’ for either patients [see item (h), Table 2] or carers [item (h), Table 3]. However, the distribution of satisfaction for this variable for carers was different than for other variables, with a large proportion of carers rating convenience of hospital for visiting as fair or poor. A higher proportion of carers rated convenience of visiting the hospital as ‘poor’ at intervention than control sites (12% (30/257) vs. 1% (2/143) ‘poor’, P = 0.001). During the qualitative interviews with carers from intervention sites, concerns were raised about the prohibitive cost of parking facilities and worries about travelling long distances, especially at night. However, carers also reported that they were willing to accept this inconvenience in the context of the life‐saving nature of primary angioplasty.
I think it’s a good thing he was brought there you know, I think if he had gone to his local hospital then he mightn’t, you know, I wouldn’t rate his chances to be honest (carer 5, phase 1 interview)
Discharge and aftercare
Satisfaction levels with hospital discharge procedures and aftercare were notably lower than for other aspects of care for both intervention and control sites [see items (j), (l), (m) and (n), Table 2]. Patient satisfaction with information about how to manage the condition in future was lower in intervention than control sites although this was not statistically significant at the 0.01 level (P = 0.049). This was explored further in ‘phase 3’ qualitative interviews where patients explained how they spent a long time waiting for hospital discharge, often involving several hours waiting for drugs from the pharmacy. They also felt there was a lack of consistency regarding follow‐up care and advice. Patients discussed how they found it difficult to absorb information about the drugs they were taking and future management of their condition during the hospital stay immediately following their heart attack. Some reported anxiety, when they suffered side‐effects from their medication because they did not know what was ‘normal’ and what might be a warning sign of something more serious, particularly if they felt that they had not received adequate follow‐up. When people had received aftercare they were happy with it, but some patients reported not receiving aftercare, or receiving it too late after discharge.
I felt I could have done with more [support]. There were lots of small things that worried me, the things that didn’t seem enough to ask my GP about really (patient 123, interview)
For the intervention sites, problems with aftercare may have been exacerbated by speedier discharge or transfer back to a feeder hospital before medication and rehabilitation procedures had been fully explained.
There was not enough time to inform me about medication etc. as the ambulance was waiting to take me back to (transfer hospital) (patient 321, survey)
Discussion
Patients and carers found care at primary angioplasty hospitals as acceptable as thrombolysis‐based care. There were a few differences between the two types of care, and differences mainly favoured primary angioplasty hospitals. A key exception was carer satisfaction with the convenience of travelling to visit the patient. This is a potential problem when services are centralized and indeed appeared to be a problem for primary angioplasty. However, qualitative interviews with carers identified that carers were willing to accommodate this inconvenience in the context of the life‐saving treatment of the patient.
Another potential concern was about information offered to patients about how to manage the problem in the future. Shorter lengths of stay associated with primary angioplasty may affect the ability of staff to inform patients about after care due to the shorter length of stay associated with primary angioplasty. 18 As well as identifying differences between patients and carers receiving two types of care, the survey also showed that patients and carers at both intervention and control sites were highly satisfied with many aspects of emergency treatment for STEMI, with the exception of hospital discharge and aftercare.
A recent Department of Health policy review cites patient experience as the most important lever for service improvement in the NHS and there is a strong drive towards using outputs from patient and public involvement activity in influencing service planning and development. 19 , 20 However, relatively little research has been undertaken to date on patient views of primary angioplasty which could influence service delivery. Patient satisfaction with elective angioplasty in the United States has been found to be high, although the experience of elective angioplasty is likely to be different from that of primary angioplasty. 9 Recent studies of patient views of primary angioplasty in the UK both found that patients undergoing primary angioplasty were very positive about their experiences and also support our concerns about the information needs of these patients for their aftercare. 21 , 22 , 23 Radcliffe et al. found that experiences of aftercare were varied and some patients still had unanswered questions when interviewed, being particularly disappointed with their follow‐up in primary care. 23 Astin et al. reported some misconceptions around the perception of what had happened and the seriousness of the condition and advocate further patient education post‐discharge. 22
It is important to consider the information needs of primary angioplasty patients because patient satisfaction with medical treatment and information are associated with improved physical and mental health related quality of life in patients with angina pectoris. 24 In particular, advice on how to improve health is associated with improved physical health, 24 demonstrating the importance of adequate information and access to cardiac rehabilitation services.
Strengths and limitations
Recent UK Department of Health policy advocates finding new ways to measure patient experience. 25 The use of both qualitative and quantitative methods allowed us to achieve a more comprehensive understanding of patient and carer views than one method alone. The qualitative component allowed us to explore issues that were salient to participants, whilst the survey allowed us to identify differences between intervention and control sites. A recent editorial highlights the dangers of reporting ‘superficial assessments of service users’ opinions’, as overall positive experiences can mask important concerns with aspects of service provision. 26 In our phase one interviews, we indeed found that patients were initially reluctant to criticize the service due to their generally excellent experience and gratitude at receiving life‐saving treatment, although some negative aspects were very briefly mentioned. We then undertook a survey using a specific, wide ranging list of items and indeed identified some aspects of care that patients and carers were unhappy with, whilst being generally very satisfied with care. The second set of interviews then allowed us to probe further into these negative aspects.
Whilst our study supported that of other studies looking at the patient experience of primary angioplasty, we were able to attribute some of the findings to the new service itself, rather than solely the experience of having being treated for a heart attack as we included patients from a ‘control’ group who had received mainly thrombolysis. The survey was based on a large sample of patients from four intervention and four control sites with a high response rate (87%), suggesting little effect of any non‐response bias. However, although recruitment rates for the survey were reasonable (67%), nearly two‐fifths of patients who were not recruited were missed because they were transferred or discharged early. We may therefore have underrepresented the views of transfer patients who were repatriated back to their original hospital within the intervention group. Also, a large number of comparisons have been tested statistically and at least one may have occurred by chance. Further, this was an observational study, and sites were not randomized to be intervention or control. Therefore differences found between sites may be related to characteristics of the sites other than the main type of care offered. Finally, intervention sites were self‐selected and therefore keen to provide an innovative service. It is possible that patients at sites offering primary angioplasty in the future may have a less positive experience than those at these ‘early implementer’ sites.
Implications for practice
Hospitals can offer primary angioplasty without being concerned about adversely affecting patient or carer satisfaction. However, they will need to ease the added burden of travel for carers by informing them of travel reimbursement schemes and the availability of overnight accommodation. Additionally, the information needs of primary angioplasty patients need to be taken more seriously. In fact the last stages of care need attention regardless of the type of treatment offered in a hospital, particularly given the drive to reduce length of stay and expedite discharge for patients post‐STEMI. The discharge and aftercare of STEMI patients requires considerable attention to increase satisfaction levels to those with earlier parts of care.
Conclusions
Reorganization of care to offer a primary angioplasty service was acceptable to patients and their carers with the exception of convenience of visiting the hospital for carers, and information needs of patients about how to manage their condition in the future. Satisfaction levels were high regardless of the type of care received, with the exception of discharge and aftercare.
Conflicts of interest
No conflicts of interest have been declared.
Source of funding
This article presents independent research commissioned by the UK National Institute for Health Research Service Delivery and Organization Programme. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Acknowledgements
We would like to thank all of the patients and their carers who took part in interviews and completed questionnaires as well as the hospital staff who helped to recruit them. We would also like to thank Kathryn Paulucy for clerical assistance.
References
- 1. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet, 2003; 361: 13–20. [DOI] [PubMed] [Google Scholar]
- 2. Bravo Vergel Y, Palmer S, Asseburg C et al. Is primary angioplasty cost effective in the UK? Results of a comprehensive decision analysis. Heart, 2007; 93: 1238–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Myocardial Ischaemia National Audit Project . How the NHS manages heart attacks Seventh Public Report. London: Royal College of Physicians, 2008. [Google Scholar]
- 4. Department of Health . Our NHS, our Future: NHS Next Stage Review Interim Report. London: DH, 2007. [Google Scholar]
- 5. British Cardiovascular Society . National Infarct Angioplasty Project (NIAP). Available at: http://www.bcs.com/pages/news_full.asp?NewsID=2154 2005, accessed 31 July 2008.
- 6. Black A. Reconfiguration of surgical, emergency, and trauma services in the United Kingdom. Centralisation of services is politically impossible. BMJ, 2004; 328: 178–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Trust P. Reconfiguration of surgical, emergency and trauma services: patient power may be the way forward. BMJ, 2004; 328: 522–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Senate of Surgery of Great Britain and Ireland . Reconfiguration of Surgical, Accident and Emergency and Trauma Services in the UK. Glasgow: RCSENG‐Professional Standards and Regulation, 2004. Available at: http://www.rcseng.ac.uk/publications/docs/reconfiguration.html, accessed 24 July 2008. [Google Scholar]
- 9. Gulanick M, Bliley A, Perino B et al. Patients’ responses to the angioplasty experience: a qualitative study. American Journal of Critical Care, 1997; 6: 25–32. [PubMed] [Google Scholar]
- 10. Creswell JW, Plano‐Clark V. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications, 2007. [Google Scholar]
- 11. O’Cathain A, Murphy E, Nicholl J. Integration and publications as indicators of ‘yield’ from mixed methods studies. Journal of Mixed Methods Research, 2007; 1: 147–163. [Google Scholar]
- 12. Sampson FC, O’Cathain A, Goodacre S. Feeling fixed and its contribution to patient satisfaction with primary angioplasty: a qualitative study. European Journal of Cardiovascular Nursing, 2009; 8: 85–90. [DOI] [PubMed] [Google Scholar]
- 13. Flanagan JC. The critical incident technique. Psychological Bulletin, 1954; 51: 327–358. [DOI] [PubMed] [Google Scholar]
- 14. Collins K, O’Cathain A. The continuum of patient satisfaction – from satisfied to very satisfied. Social Science & Medicine, 2003; 57: 2265–2470. [DOI] [PubMed] [Google Scholar]
- 15. Crow R, Gage H, Hampson S et al. The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature. Health Technology Assessment, 2002; 6: 45–51. [DOI] [PubMed] [Google Scholar]
- 16. O’Cathain A, Thomas KJ. ‘Any other comments?’ Open questions on questionnaires – a bane or a bonus to research? BMC Medical Research Methodology, 2004; 4: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ritchie J, Spencer L. Qualitative data analysis for applied policy research In: Bryman A, Burgess RG. (eds) Analysing Qualitative Data. London: Routledge, 1994: 173–194. [Google Scholar]
- 18. MINAP steering group . How the NHS Manages Heart Attacks. Sixth Public Report on the Myocardial Infarction National Audit Project (MINAP). London: Royal College of Physicians, 2007. [Google Scholar]
- 19. Darzi A. High Quality Care for all: NHS Next Stage Review Final Report. London: Department of Health, 2008. [Google Scholar]
- 20. Department of Health . Getting Over the Wall. How the NHS is Improving the Patient’s Experience. London: Department of Health, 2004. [Google Scholar]
- 21. Astin F, Closs SJ, McLenachan J et al. The information needs of patients treated with primary angioplasty for heart attack: an exploratory study. Patient Education and Counselling, 2008; 73: 325–332. [DOI] [PubMed] [Google Scholar]
- 22. Astin F, Closs SJ, McLenachan J, Hunter S, Priestley C. Primary angioplasty for heart attack: mismatch between expectations and reality? Journal of Advanced Nursing, 2009; 65: 72–83. [DOI] [PubMed] [Google Scholar]
- 23. Radcliffe EL, Harding G, Rothman MT, Feder GS. ‘It got right to the spot’. The patient experience of primary angioplasty: a qualitative study. European Journal of Cardiovascular Nursing. 2009. Online first. DOI:10.1016/j.ejcnurse.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 24. Guldvog B. Can patient satisfaction improve health among patients with angina pectoris? International Journal of Quality in Health Care, 1999; 11: 233–240. [DOI] [PubMed] [Google Scholar]
- 25. Darzi A. High Quality Care for all: Our Journey so far. London: Department of Health, 2009. [Google Scholar]
- 26. Entwistle VA. When service users’support obscures problems with care: the need for rigorous research into patients’ experiences. Health Expectations, 2009; 12: 117–119. [DOI] [PMC free article] [PubMed] [Google Scholar]


