Abstract
Objective To engage a group of people with relevant lived experience in the development of a text‐messaging intervention to reduce repetition of self‐harm.
Background Contact‐based interventions, such as follow‐up letters, postcards and telephone calls, have shown potential to reduce repetition of self‐harm in those who present at Accident and Emergency departments. Text messaging offers a low‐cost alternative that has not been tested. We set out to develop a text‐based intervention. The process of intervention development is rarely reported and little is known about the impact of service user involvement on intervention design.
Method We held a series of six participatory workshops and invited service users and clinicians to help us work out how to get the right message to the right person at the right time, and to simulate and test prototypes of an intervention.
Results Service users rejected both the idea of a generic, ‘one size fits all’ approach and that of ‘audience segmentation’, maintaining that text messages could be safe and effective only if individualized. This led us to abandon our original thinking and develop a way of supporting individuals to author their own self‐efficacy messages and store them in a personal message bank for withdrawal at times of crisis.
Conclusions This paper highlights both the challenge and the impact of involving consumers at the development stage. Working with those with lived experience requires openness, flexibility and a readiness to abandon or radically revise initial plans, and may have unexpected consequences for intervention design.
Keywords: intervention design, participatory methods, self‐harm, text messaging, user involvement
Introduction
Whilst it is by no means uncontested, 1 , 2 , 3 the value of consumer involvement in healthcare is widely accepted, 4 , 5 and is central to the UK Department of Health strategy for modernizing the English National Health Service (NHS) and improving the quality of care. 6 , 7 How the rhetoric of involvement translates into reality is a separate question. Much has been written about the practical benefits and challenges of involving service users in research, 8 , 9 , 10 , 11 , 12 service planning and development 13 , 14 , 15 and professional education. 16 , 17 Less attention has been given to the impact of consumer involvement in intervention design, 18 although it is reasonable to assume that the issues may be similar to those encountered in other areas. On the positive side, these include the empowerment of service users and improvement in the quality, relevance and acceptability of findings. 1 , 11 , 19 , 20 On the negative side, they include the danger of tokenism and fears about radicalism and representativeness, 2 , 14 , 19 , 21 together with the challenge of ensuring that participants receive appropriate skills training and support and concerns about resource implications. 8 , 10 , 22
Within healthcare, the science of intervention development is still in its infancy. 23 Few studies report the development process, giving the impression that interventions emerge ‘out of thin air’ and proceed straight to trial. Lack of clarity in this area was one of the factors that prompted the revision of the UK Medical Research Council’s guidance on development and evaluation of complex interventions. 24 , 25 The new guidance emphasizes the importance of good preparatory work, which may include new primary research such as conducting interviews with those targeted by the intervention, in order to develop a thorough understanding of the likely process of change and to ensure acceptability. Lovell and colleagues 26 highlighted the importance of patient‐centredness. They supplemented systematic reviews with a consensus process involving 32 key stakeholders in order to identify the core components required in a guided self‐help intervention for depression. Likewise, Hardeman et al. 23 incorporated focus groups and individual consultations with members of the target population in the development of an intervention to promote physical activity among individuals at risk of Type 2 diabetes, and Waller et al. 27 described a participatory process used in the development of a support system for young people with diabetes. Other authors have discussed user engagement in relation to medical device development. 18 , 28 , 29
Involving potential recipients at the design stage may be particularly important when the intervention is intended to bring about behavioural, as opposed to biochemical, change. However, it is not without difficulties. In this paper we report on the challenge of working with a group of people with relevant lived experience to develop a text‐messaging intervention to reduce repetition of self‐harm.
Contact‐based interventions to reduce repetition of self‐harm
It is estimated that, in England and Wales, at least 142 000 visits to Accident and Emergency (A&E) departments each year result from self‐inflicted injury. 30 Non‐fatal self‐harm is one of the strongest predictors of suicide, and those who repeatedly present at A&E following self‐harm are at the highest risk. 31 Preventing repetition of self‐harm may therefore reduce long‐term suicide risk. The National Suicide Prevention Strategy for England identified the management of self‐harm in A&E departments and the provision of appropriate aftercare as key areas for action, 32 and a recent review of patient attitudes towards clinical services underlined the importance of aftercare arrangements. 33
The benefit of maintaining long‐term contact with those who present at A&E departments has been demonstrated 34 and a number of contact‐based interventions have been developed and tested, including crisis cards, 35 , 36 , 37 letters, 38 postcards 39 , 40 and telephone calls. 41 These are based on the hypothesis that maintaining contact with patients once they leave the clinical setting encourages them to feel that ‘somebody cares’. Motto and Bostrum speculate that this sense of connectedness, the so‐called ‘delusion of fusion’, exerts a strong suicide‐preventative effect. 34
Text messaging offers an alternative to letters and postcards that not only fits well with the ambition of UK health policy to harness the power of technologies and new media to improve patient outcomes, 42 , 43 but is also more in line with the communication preferences of vulnerable young people, who may be reluctant to engage with health professionals. 44 Texting has always been valued by young people, not only as a means of organizing their social lives but also as a medium for informal peer‐support. It has been shown to have particular appeal for socially anxious, disaffiliated and difficult‐to‐reach young people, for whom it offers a highly controllable and unthreatening means of self‐expression. 45 , 46 We speculated that the ‘always on’, instant medium of text messaging might offer an interactive lifeline to those at risk of self‐harm, and set out to explore its potential as a cost‐effective medium for delivery of a low‐intensity intervention to provide psychological support following an A&E presentation.
Text messaging in healthcare delivery: ‘push’ and ‘pull’ models
There is growing interest in the use of short message services (SMS), or text messaging, in healthcare delivery. 47 , 48 , 49 So far, it is the ‘push’ capability of SMS that has attracted the most interest. 48 ‘Push’ messaging is initiated by the service provider and is one‐way only, delivering specific messages to selected individuals at predetermined times. This has proved ideal for sending appointment and medication reminders, 50 , 51 , 52 communicating test results 53 and delivering condition‐specific health education. 54 Encouraging results have also been reported for some behaviour change interventions that rely on this model. 55 For example, Franklin et al. 56 , 57 developed a text‐messaging system for young people with diabetes (‘Sweet Talk’) that delivered scheduled messages tailored to individuals’ clinical profiles and self‐management goals, together with more generic advice. The authors comment that, for this classically hard‐to‐engage patient group, text messaging offers an ideal means of delivering support proactively, ‘where information is ‘pushed’ to the user rather than being actively sought.’ 27
‘Pull’ messaging, by contrast, is initiated by the user and may take the form of a request for information, advice or support, thus opening up the possibility of two‐way communication between patients and professionals. Atun and Sittampalam 48 report that attempts have been made to encourage young people to use SMS in this way to access counsellors and other health professionals on a range of issues, such as bulimia, exam anxiety, diabetes, smoking cessation, and relationship problems. Bauer et al. 58 developed and piloted a text‐message based intervention for use in the aftercare of bulimia patients, but found their semi‐automatic two‐way system of personalized messages to be labour intensive and only moderately acceptable to the users. Other studies have reported more promising results. 59 , 60
Methods
Early stakeholder involvement was seen to be crucial to the success of the project. Our belief was that inviting potential recipients of the intervention to play a central role in its development would be the best way to ensure that it was usable, acceptable and likely to achieve health benefit. As the intervention had to be clinically viable and affordable, it was also important to involve clinicians.
We therefore held a series of six participatory workshops, to which we invited mental health service users with histories of self‐harm, carers and clinicians working with self‐harm. The lay member of our project team used her extensive networks to recruit those with relevant lived experience, who were paid by the hour for attendance at the workshops. Clinicians were recruited from our local liaison psychiatry team.
The first workshop lasted a full day and was designed to introduce people to the project and enable the various stakeholders to understand and feel comfortable with one another. Some time was spent exploring the meaning and functions of self‐harm and attitudes towards prevention. We also discussed the acceptability and relative merits of text messaging, as compared with other communication media such as letters, postcards and phone calls, as a medium for post‐A&E follow‐up. We then turned our attention to the style and content of messages, the challenge being to work out how to get the right message to the right person at the right time in order to reduce the urge to self‐harm.
Right message
At the outset, our plan was to develop either a single generic message similar to that in Carter et al.’s postcards study, 39 or a set of messages, possibly targeted at different sub‐groups of self‐harmers, in accordance with the notion of audience segmentation that underpins both commercial and social marketing. 61 , 62 , 63 We therefore saw the principle task in Workshop 1 as being to generate a catalogue of potential messages that could be market tested, possibly with different sub‐groups of the target population, and rated for likely effectiveness.
To this end, each workshop participant was given a pad of sticky notes and asked to write down any ‘message’ that came into their head, however ridiculous it might seem, that they felt might help to reduce or quell an urge to self‐harm. Each message was written on a separate sticky note. Participants then worked in pairs (one service user or carer with one researcher or clinician) to identify categories and sort the notes accordingly. Duplicate messages were removed and themes were split, merged or renamed until the whole group was agreed on a small number of categories into which all the messages fitted.
Right person
This exercise was repeated in relation to the question ‘who self‐harms?’ Participants were asked to identify characteristics of individuals who self‐harm, again recording each one on a separate sticky note. These too were analysed thematically and sorted, with a view to understanding the ‘market’ and identifying discrete segments, i.e. sub‐groups, possibly distinguished by demographics, behaviours, motivations or patterns of service use, for which different types of message might be most appropriate.
Right time
Finally, we turned to the question of timing. Participants with lived experience were invited to identify individual triggers (situations that precipitate self‐harm) and particular times of day at which the urge to self‐harm is strongest, and were asked to consider whether different situations might call for different types of message.
Subsequent workshops
Workshop 2 took the form of a focus group, to which additional participants with histories of self‐harm were invited for the purposes of validating and rating the messages generated in Workshop 1. Using a PowerPoint presentation, messages were presented in random order, one message per slide, for 15 sec each, with a break after each block of 10. Participants were given a score sheet and were asked to rate each message as it appeared on the screen using a 0–10 scale, where 10 represented ‘Would definitely reduce the urge to self‐harm’ and 0 represented ‘Would definitely not reduce urge’. Further discussion also took place on the characterization of key audience groups, based on the outputs from Workshop 1.
Workshop 3 began with a re‐test of a selection of messages from the previous session, followed by a free‐ranging discussion, during which the intervention began to take shape in an entirely unexpected way. This led us back to the literature to search for a theoretical basis for the emergent intervention and to enlist an IT consultant to develop the technology to support it. Workshops 4, 5 and 6 involved simulating, evaluating and refining the intervention.
Results
A total of eight mental health service users and one carer participated in the process at different times. Table 1 shows their characteristics. Three liaison psychiatry team members attended one or more workshops.
Table 1.
Characteristics of workshop participants
| Pseudonym | Sex | Age | In contact with MH services at the time* | Length of time self‐harming | No of workshops attended |
|---|---|---|---|---|---|
| Hannah | Female | 18–25 | Yes | >5 years | 5 |
| Charlotte | Female | 18–25 | Yes | >5 years | 2 |
| Andy | Male | 26–35 | No | >5 years | 3 |
| Jo | Female | 36–49 | Yes | >5 years | 2 |
| Rebecca | Female | 36–49 | No | >5 years | 6 |
| Dougie | Male | 36–49 | d/k | >5 years | 1 |
| Carol | Female | 50+ | No | >5 years | 4 |
| Alison | Female | 50+ | Yes | >5 years | 5 |
*All participants had been users of mental health services in the past.
From the outset, there was broad support for a text‐messaging intervention of some sort as an adjunct to clinical treatment. Texting was felt to have significant advantages over other media. It was perceived to be more private than letters or postcards and less intrusive than telephone calls. Moreover, there was a view that, for vulnerable or excluded individuals, the sending and receiving of texts could be a socially validating activity, giving the appearance of connectedness and participation in a social network. Reaching agreement on the content, targeting and timing of messages was more difficult.
Right message
Workshop 1 generated 122 possible messages, many of which were highly individual and context‐specific. One sticky note carried the message: ‘Do you like cheese?’ This phrase had immense sentimental meaning for its author, reminding her of her young son and the strength and intimacy of their bond. She maintained that, for her, it would be extremely powerful in combating thoughts of suicide or life‐threatening behaviour. Another, referring to the performance of two teams in the English football league, read: ‘Liverpool 0, Chelsea 2. Great result. Take care.’
Three broad categories of message emerged:
-
1
Those that affirmed or validated emotions (e.g. ‘It’s ok to feel angry’)
-
2
Those that prescribed actions, distractions or cognitive strategies (e.g. ‘Call Samaritans’; ‘Have a warm bath’; ‘Take it a minute at a time’)
-
3
Those that were interrogative or designed to initiate dialogue (e.g. ‘Do you want to talk?’)
There was an overall preference for those that validated emotions. Those that prescribed specific behaviours or demanded a cognitive response were less well received. Concerns were expressed about the resource implications of initiating dialogue, about the ethics of raising expectations of sustained personal contact and about those messages that required detailed knowledge of an individual’s lifestyle preferences.
By the end of the third workshop, the group was still unable to reach agreement on a set of messages that might ‘work’ in all circumstances to reduce the urge to self‐harm or enable people to feel cared for. Whilst each service user could identify several messages that might reduce their own risk of self‐harming, they were unwilling to give any assurances that these would be effective for another person in another situation. There was considerable concern that receiving the ‘wrong’ message (either a very bland, impersonal message or one tailored to someone else’s situation) might precipitate rather than reduce risk. One participant commented:
‘If I got a text that wasn’t mine when I was in a crisis it would make me self‐harm even more.’
During Workshop 3, the idea emerged of supporting individuals to author their own messages.
Right person
Characteristics of ‘self‐harmers’ listed by participants in Workshop 1 fell into a number of categories, all of which offered potential ways of classifying the target audience:
-
1
Diagnostic labels (e.g. personality disorders)
-
2
Demographics (e.g. young, female)
-
3
Background or vulnerability factors (e.g. sexually abused)
-
4
Types of self‐harm (e.g. cutting, overdosing)
-
5
Intended outcome of self‐harm (e.g. to die, to cope, to conform)
-
6
Service use (e.g. ‘first‐timer’, ‘regular visitor’)
-
7
Presentation style (e.g. ‘quiet and uncommunicative’, ‘agitated and angry’).
However, we were unable to identify any distinct segments that had face validity with service users, could be reliably identified in clinical practice and could be usefully matched to different message elements or styles. Moreover, from the outset there was considerable resistance, both from service users and from members of the research team, towards the stereotyping of audience sectors on which both commercial and social marketing models rely. A decision was therefore taken to abandon the notion of targeting particular messages at particular audience segments.
Right time
This exercise struck a chord with service users, who quickly generated a list of triggers and times at which the urge to self‐harm is strongest. These included:
-
1
People (e.g. ‘Being with my dad’)
-
2
Places (e.g. ‘Crowded places’)
-
3
Times of day (e.g. ‘Sunday afternoons’)
-
4
Service barriers (e.g. ‘Being told to wait till Monday morning to see someone’)
-
5
Bureaucracy and system failures (e.g. ‘Filling in forms’)
-
6
Physiological states (e.g. ‘Pre‐menstrual’)
-
7
Cognitive states (e.g. ‘Flashbacks’)
-
8
Emotional states (e.g. ‘No hope’)
Again, these were highly personal and underlined the need for messages to be individualized, not only in terms of content but also in terms of timing of delivery. The responses suggested that it would be difficult to generalize about the best times to deliver supportive messages and that the ideal solution would be to harness the ‘pull’ capability of text messaging to allow users to access support instantly, whenever they find themselves in a stressful or triggering situation.
Designing the intervention
By the close of Workshop 3, agreement had been reached among those with lived experience of self‐harm that a text‐based intervention could usefully supplement clinical treatment if messages could be accurately tailored to individual needs and delivered at times of greatest risk.
A further search of the literature by the research team, together with experimentation in the remaining three workshops, resulted in the development of an intervention that draws on elements of cognitive‐behavioural therapy (CBT) and involves the use of personal ‘coping statements’, delivered using SMS technology. Coping statements, sometimes known as ‘positive self‐statements’, are self‐authored statements that can be invoked in anxiety‐provoking situations in order to reduce tension, challenge cognitive distortions, promote self‐affirmation and thus encourage an individual to hold up under pressure. 64 , 65
Repeated simulations in the workshop setting resulted in a protocol that could be used to enable individuals to formulate a set of six to eight personal coping statements, and showed that a single structured telephone interview, conducted by a trained lay person, would be sufficient to achieve this end. Further tests indicated that the use of an automated system to store and deliver the messages would be acceptable to users. A software programme was then built that could store each individual’s statements electronically in a personal message bank and deliver one or more messages to his/her mobile phone on demand. This permits users to access individualized messages whenever they are most needed, at minimal cost. The intervention is known as txt4shs (Text for Self‐Harm Support).
An exploratory trial is currently in progress, in which we are testing a number of variations of the intervention in order to observe the effects of different components, make further refinements and gather evidence to inform the design of a full trial.
Discussion
Involving service users in the process of intervention design is challenging and may require researchers to abandon or radically revise firmly held ideas. At the outset, based on our initial review of the self‐harm literature, our plan had been to replicate the study by Carter et al 39 using a simple generic text message delivered at predetermined intervals. Early consultation with potential end‐users suggested that this was unlikely to engender a feeling of being ‘cared for’ and could even have a damaging effect on patterns of self‐harm or future service use. Another idea, derived from the marketing literature, of developing sets of messages targeted at different sub‐groups within the self‐harming population was also firmly rejected by members of that population. Their involvement in the design process changed the nature of the intervention dramatically.
Challenges of involving service users in intervention design
Although our ambition was to work with them as equals, workshop participants were not involved in every aspect of decision making. As other authors have commented, 10 , 11 the power balance may shift over the course of a project, depending on the time and skills demanded by particular tasks. Separate meetings of the project team took place alongside the participatory workshops and some tasks, such as searching the scientific literature, were undertaken by researchers alone.
Ram and colleagues 18 note that engaging users in product development is challenging ‘in terms of both accessing vulnerable users and resourcing the process, in the face of commercial pressures to get products into the market place’. Other authors have reported that adopting a participatory approach is likely to slow down the intervention development process and that users may become bored or disillusioned along the way. 27
One of the biggest challenges we faced in using a participatory approach with individuals who self‐harm was that, because of fluctuations in mental state and personal circumstances, it proved difficult to keep the same group of participants engaged throughout the process. A highly committed core group of three emerged, who were joined by different individuals on other occasions. This meant that we had to keep restating the aims of the project and re‐establishing consensus at each successive workshop.
Furthermore, the iterative nature of the participatory process meant that, although a preliminary programme for the whole workshop series was drawn up at the outset, plans had to be revised in response to the findings from each session. The whole process required flexibility, a constantly open mind and a willingness to embrace the unexpected. This way of working poses funding challenges, since funders typically expect very highly formulated proposals. Our findings suggest that involving service users at the initial design stage, in ways that are not just tokenistic, requires a high degree of latitude, which in turn may require funding bodies to tolerate uncertainty and to place a great deal of trust in research teams.
The development phase also took longer than anticipated and resulted in a far more complex intervention than we had originally envisaged, which had serious implications for the pilot trial design.
Benefits of involving service users in intervention design
On the positive side, user engagement has the potential to uncover unmet needs and preferences and to feed these into the design process at the earliest possible stage. This increases the likelihood of developing interventions that are ‘safe, usable, clinically effective and appropriate to cultural context.’ 18 It can also give users a real sense of ownership, which may lead to more successful implementation. 27
It is unlikely that the idea of enabling individuals to author their own self‐efficacy messages and to store them for future retrieval in times of distress would have occurred to us, had it not been for the workshops. Yet it accords perfectly with the self‐management agenda within healthcare generally 66 and with the principles of recovery within mental health care in particular. 67 , 68 , 69 , 70 The recovery model places emphasis on taking control of one’s own life, developing personal coping strategies and actively working to maintain wellness, rather than simply being the passive recipient of professional interventions. The Wellness Recovery Action Plan that mental health service users are encouraged to develop uses the same idea of planning during times of wellness and developing a toolkit of resources to draw on in times of crisis, when positive thoughts may be difficult to access. 71
The SMS‐assisted self‐management approach suggested by our service users takes account of the heterogeneity of the clinical population that is highlighted by Slee et al. 72 It overcomes one of the acknowledged limitations of the study by Carter et al., 39 namely that the messages might have benefited from being personalized (personal correspondence, GL Carter, 2009), and challenges the prevailing view within the self‐harm literature that contact is more important than content. Our service users were unable to identify a single generic message that would engender a feeling of social connectedness. Nor did they accept that such a feeling would necessarily reduce the urge to self‐harm. Even more significant was their readiness to countenance the use of an automated system to manage and deliver messages. Our findings suggest strongly that the benefits of personalized content outweigh those of human contact. The involvement of service users moved our intervention away from the purely contact‐based approaches, based on the ‘delusion of fusion’, 34 towards the cognitive restructuring model employed within CBT. 64
Finally, the service users’ insistence on the need to be able to access support immediately in response to escalating risk encouraged us to move beyond the use of text messaging to ‘push’ information and advice to a target population at pre‐scheduled times. In response to consumer demand, we were able to exploit the ‘pull’ capacity of the medium, whereby individual users are able to initiate requests for psychological support, and to develop a system that allows access to personal self‐efficacy messages and coping tools at the touch of a button, whenever they are most needed. This creates more opportunities to interrupt the process of self‐harm (Fig. 1), since messages can be accessed at different points and used for different purposes, either to reduce underlying risk or vulnerability (e.g. by boosting self‐esteem or resistance to chronic stressors) or to offer support in acutely stressful situations and help to forestall or fight the urge to self‐harm.
Figure 1.
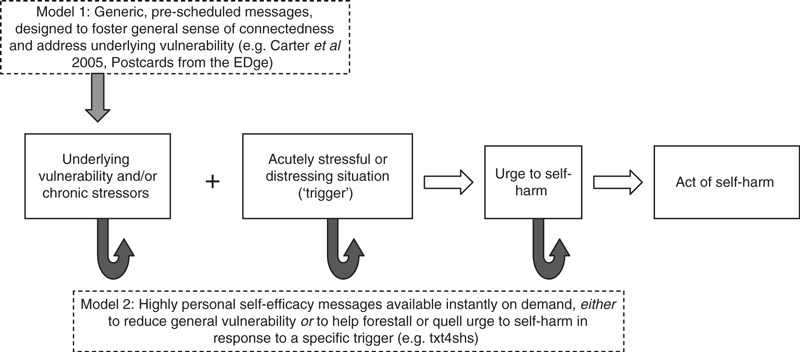
Contrasting models of contact‐based intervention to reduce repetition of self‐harm.
Despite both practical and intellectual challenges, we consider that much has been gained by involving potential users of the intervention in the development process. The effectiveness of the intervention has yet to be demonstrated.
Conflicts of interest
None.
Sources of funding
The study was funded by the National Institute for Health Research, Research for Patient Benefit programme, grant no. PB‐PG‐0706‐10497. Peter Aitken’s time was funded by the NIHR Collaboration for Leadership in Applied Health Research and Care for the South West Peninsula (PenCLAHRC). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Acknowledgements
We wish to thank all the participants who took part in the workshops and Dr Fraser Reid, formerly of the University of Plymouth, for his contribution to the design of the study.
References
- 1. Boote J, Telford R, Cooper C. Consumer involvement in health research: a review and research agenda. Health Policy, 2002; 61: 213–236. [DOI] [PubMed] [Google Scholar]
- 2. Beresford P. User involvement, research and health inequalities: developing new directions. Health & Social Care in the Community, 2007; 15: 306–312. [DOI] [PubMed] [Google Scholar]
- 3. Cowden S, Singh G. The ‘User’: friend, foe or fetish? A critical exploration of user involvement in health and social care. Critical Social Policy, 2007; 27: 5–23. [Google Scholar]
- 4. Charles C, DeMaio S. Lay participation in health care decision making: a conceptual framework. Journal of Health Politics, Policy and Law, 1993; 18: 881–904. [DOI] [PubMed] [Google Scholar]
- 5. Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database of Systematic Reviews, 2006; 3: CD004563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Department of Health . Patient and Public Involvement in the NHS. London: Department of Health, 1999. [Google Scholar]
- 7. INVOLVE . Promoting public involvement in NHS, public health and social care research: Strategic Plan 2007 – 2011. 2007. (Accessed 28 August 2009, at http://www.invo.org.uk.)
- 8. Oliver S, Milne R, Bradburn J et al. Involving consumers in a needs‐led research programme: a pilot project. Health Expectation, 2001; 4: 18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hounsell J, Owens C. User researchers in control. Mental Health Today, 2005: 29–32. [PubMed] [Google Scholar]
- 10. Staniszewska S, Jones N, Newburn M, Marshall S. User involvement in the development of a research bid: barriers, enablers and impacts. Health Expectation, 2007; 10: 173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McKevitt C, Fudge N, Wolfe C. What is involvement in research and what does it achieve? Reflections on a pilot study of the personal costs of stroke. Health Expectation, 2009; 13: 86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smith E, Donovan S, Beresford P et al. Getting ready for user involvement in a systematic review. Health Expectation, 2009; 12: 197–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Crawford MJ, Rutter D, Manley C et al. Systematic review of involving patients in the planning and development of health care. BMJ, 2002; 325: 1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Crawford MJ, Aldridge T, Bhui K et al. User involvement in the planning and delivery of mental health services: a cross‐sectional survey of service users and providers. Acta Psychiatrica Scandinavica, 2003; 107: 410–414. [DOI] [PubMed] [Google Scholar]
- 15. Rutter D, Manley C, Weaver T, Crawford MJ, Fulop N. Patients or partners? Case studies of user involvement in the planning and delivery of adult mental health services in London. Social Science and Medicine, 2004; 58: 1973–1984. [DOI] [PubMed] [Google Scholar]
- 16. Morgan A, Jones D. Perceptions of service user and carer involvement in healthcare education and impact on students’ knowledge and practice: a literature review. Medical Teacher, 2009; 31: 82–95. [DOI] [PubMed] [Google Scholar]
- 17. Lathlean J, Burgess A, Coldham T et al. Experiences of service user and carer participation in health care education. Nurse Education Today, 2006; 26: 732–737. [DOI] [PubMed] [Google Scholar]
- 18. Ram MB, Grocott P, Weir H. Issues and challenges of involving users in medical device development. Health Expectation, 2007; 11: 63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Entwistle V, Renfrew M, Yearley S, Forrester J, Lamont T. Lay perspectives: advantages for health research. BMJ, 1998; 316: 463–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oliver S, Clarke‐Jones L, Rees R et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence‐based approach. Health Technology Assessment, 2004; 8: 1–2. [DOI] [PubMed] [Google Scholar]
- 21. Williamson C. ‘How do we find the right patients to consult?’ Quality in Primary Care, 2007; 15: 195–199. [Google Scholar]
- 22. Trivedi P, Wykes T. From passive subjects to equal partners: qualitative review of user involvement in research. British Journal of Psychiatry, 2002; 181: 468–472. [DOI] [PubMed] [Google Scholar]
- 23. Hardeman W, Sutton S, Griffin S et al. A causal modelling approach to the development of theory‐based behaviour change programmes for trial evaluation. Health Education Research, 2005; 20: 676–687. [DOI] [PubMed] [Google Scholar]
- 24. Developing and evaluating complex interventions: new guidance. 2008. (Accessed 21 Sept 2009, at http://www.mrc.ac.uk/complexinterventionsguidance.)
- 25. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ, 2008; 337: 979–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lovell K, Bower P, Richards D et al. Developing guided self‐help for depression using the Medical Research Council complex interventions framework: a description of the modelling phase and results of an exploratory randomised controlled trial. BMC Psychiatry, 2008; 8: 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Waller A, Franklin V, Pagliari C, Greene S. Participatory design of a text message scheduling system to support young people with diabetes. Health Informatics Journal, 2006; 12: 304–318. [DOI] [PubMed] [Google Scholar]
- 28. Grocott P, Weir H, Ram MB. A model of user engagement in medical device development. International Journal of Health Care Quality Assurance, 2007; 20: 484–493. [DOI] [PubMed] [Google Scholar]
- 29. Shah SG, Robinson I. Benefits of and barriers to involving users in medical device technology development and evaluation. International Journal of Technology Assessment in Health Care, 2007; 23: 131–137. [DOI] [PubMed] [Google Scholar]
- 30. Hawton K, Harriss L, Hall S, Simkin S, Bale E, Bond A. Deliberate self‐harm in Oxford, 1990–2000: a time of change in patient characteristics. Psychological Medicine, 2003; 33: 987–995. [DOI] [PubMed] [Google Scholar]
- 31. Zahl D, Hawton K. Repetition of deliberate self‐harm and subsequent suicide risk: long‐term follow‐up study of 11,583 patients. British Journal of Psychiatry, 2004; 185: 70–75. [DOI] [PubMed] [Google Scholar]
- 32. Department of Health . National Suicide Prevention Strategy for England. London: Department of Health, 2002. [Google Scholar]
- 33. Taylor TL, Hawton K, Fortune S, Kapur N. Attitudes towards clinical services among people who self‐harm: systematic review. British Journal of Psychiatry, 2009; 194: 104–110. [DOI] [PubMed] [Google Scholar]
- 34. Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatric Services, 2001; 52: 828–833. [DOI] [PubMed] [Google Scholar]
- 35. Morgan HG, Jones EM, Owen JH. Secondary prevention of non‐fatal deliberate self‐harm: the green card study. British Journal of Psychiatry, 1993; 163: 111–112. [DOI] [PubMed] [Google Scholar]
- 36. Evans MO, Morgan HG, Hayward A, Gunnell DJ. Crisis telephone consultation for deliberate self‐harm patients: effects on repetition. British Journal of Psychiatry, 1999; 175: 23–27. [DOI] [PubMed] [Google Scholar]
- 37. Evans J, Evans M, Morgan HG, Hayward A, Gunnell D. Crisis card following self‐harm: 12‐month follow‐up of a randomised controlled trial. British Journal of Psychiatry, 2005; 187: 186–187. [DOI] [PubMed] [Google Scholar]
- 38. Bennewith O, Stocks N, Gunnell D, Peters TJ, Evans MO, Sharp DJ. General practice based intervention to prevent repeat episodes of deliberate self harm: cluster randomised controlled trial. BMJ, 2002; 324: 1254–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Carter G, Clover K, Whyte I, Dawson A, D’Este C. Postcards from the EDge project: randomised controlled trial of an intervention using postcards to reduce repetition of hospital treated deliberate self poisoning. BMJ, 2005; 331: 805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Carter G, Clover K, Whyte I, Dawson A, D’Este C. Postcards from the EDge: 24‐month outcomes of a randomised controlled trial for hospital‐treated self‐poisoning. British Journal of Psychiatry, 2007; 191: 548–553. [DOI] [PubMed] [Google Scholar]
- 41. Vaiva G, Ducrocq F, Meyer P et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. BMJ, 2006; 332: 1241–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Liddell A, Adshead S, Burgess E. Technology in the NHS: Transforming the Patient’s Experience of Care. London: The King’s Fund, 2008. [Google Scholar]
- 43. Department of Health . High Quality Care For All: NHS Next Stage Review Final Report. London: The Stationery Office, 2008. [Google Scholar]
- 44. Biddle L, Gunnell D, Sharp D, Donovan J. Factors influencing help seeking in mentally distressed young adults: a cross‐sectional survey. British Journal of General Practice, 2004; 54: 248–253. [PMC free article] [PubMed] [Google Scholar]
- 45. Reid D, Reid F. Textmates and text circles: insights into the social ecology of SMS text messaging In: Hamil L, Lasen A. (eds) Mobile World: Past, Present and Future. London: Springer‐Verlag, 2005: 105–118. [Google Scholar]
- 46. Reid D, Reid F. Text or talk? Social anxiety, loneliness and divergent preferences for cell phone use. Cyberpsychology & Behavior, 2007; 10: 424–435. [DOI] [PubMed] [Google Scholar]
- 47. Pal B. The doctor will text you now: is there a role for the mobile telephone in health care? BMJ, 2003; 326: 607. [Google Scholar]
- 48. Atun R, Sittampalam S. A review of the characteristics and benefits of SMS in delivering healthcare. Vodafone Policy Paper Series, No 4; 2006.
- 49. Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemedicine Journal and e-Health, 2009; 15: 231–240. [DOI] [PubMed] [Google Scholar]
- 50. Koshy E, Car J, Majeed A. Effectiveness of mobile‐phone short message service (SMS) reminders for ophthalmology outpatient appointments: observational study. BMC Ophthalmology, 2008; 8: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Car J, Ng C, Atun R, Card A. SMS text message healthcare appointment reminders in England. The Journal of Ambulatory Care Management, 2008; 31: 216–219. [DOI] [PubMed] [Google Scholar]
- 52. Foley J, O’Neill M. Use of mobile telephone short message service (SMS) as a reminder: the effect on patient attendance. European Archives of Paediatric Dentistry, 2009; 10: 15–18. [DOI] [PubMed] [Google Scholar]
- 53. Menon‐Johansson AS, McNaught F, Mandalia S, Sullivan AK. Texting decreases the time to treatment for genital Chlamydia trachomatis infection. Sexually Transmitted Infections, 2006; 82: 49–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wangberg SC, Arsand E, Andersson N. Diabetes education via mobile text messaging. Journal of Telemedicine and Telecare, 2006; 12 (Suppl 1): 55–56. [DOI] [PubMed] [Google Scholar]
- 55. Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short‐message service. American Journal of Preventive Medicine, 2009; 36: 165–173. [DOI] [PubMed] [Google Scholar]
- 56. Franklin V, Waller A, Pagliari C, Greene S. “Sweet Talk”: text messaging support for intensive insulin therapy for young people with diabetes. Diabetes Technology & Therapeutics, 2003; 5: 991–996. [DOI] [PubMed] [Google Scholar]
- 57. Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text‐messaging system to support young people with diabetes. Diabetic Medicine, 2006; 23: 1332–1338. [DOI] [PubMed] [Google Scholar]
- 58. Bauer S, Percevic R, Okon E, Meermann R, Kordy H. Use of text messaging in the aftercare of patients with bulimia nervosa. European Eating Disorders Review, 2003; 11: 279–290. [Google Scholar]
- 59. Shapiro JR, Bauer S, Hamer RM, Kordy H, Ward D, Bulik CM. Use of text messaging for monitoring sugar‐sweetened beverages, physical activity and screen time in children: a pilot study. Journal of Nutrition Education and Behavior, 2008; 40: 385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kim HS. A randomized controlled trial of a nurse short‐message service by cellular phone for people with diabetes. International Journal of Nursing Studies, 2007; 44: 687–692. [DOI] [PubMed] [Google Scholar]
- 61. Weinstein A. Market Segmentation. Chicago: Probus, 1987. [Google Scholar]
- 62. Moss HB, Kirby SD, Donodeo F. Characterizing and reaching high‐risk drinkers using audience segmentation. Alcoholism, Clinical and Experimental Research, 2009; 33: 1336–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kolodinsky J, Reynolds T. Segmentation of overweight Americans and opportunities for social marketing. The International Journal of Behavioral Nutrition and Physical Activity, 2009; 6: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Glogower FD, Fremouw WJ, McCroskey JC. A component analysis of cognitive restructuring. Cognitive Therapy and Research, 1978; 2: 209–223. [Google Scholar]
- 65. Hayes SC, Hussian RA, Turner AE, Anderson NB, Grubb TD. The effect of coping statements on progress through a desensitization hierarchy. Journal of Behavior Therapy and Experimental Psychiatry, 1983; 14: 117–129. [DOI] [PubMed] [Google Scholar]
- 66. Department of Health . The Expert Patient: A New Approach to Chronic Disease Management for the 21st Century. London: Department of Health, 2001. [Google Scholar]
- 67. Department of Health . The Journey to Recovery: The Government’s Vision for Mental Health Care. London: Department of Health, 2001. [Google Scholar]
- 68. National Institute for Mental Health in England . Guiding Statement on Recovery. Leeds: National Institute for Mental Health in England, 2005. [Google Scholar]
- 69. Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal, 1993; 16: 11–23. [Google Scholar]
- 70. Slade M, Amering M, Oades L. Recovery: an international perspective. Epidemiologia e Psichiatria Sociale, 2008; 17: 128–137. [DOI] [PubMed] [Google Scholar]
- 71. Copeland ME. Wellness Recovery Action Plan. West Dummerston, VT: Peach Press, 1997. [Google Scholar]
- 72. Slee N, Arensman E, Garnefski N, Spinhoven P. Cognitive‐behavioural therapy for deliberate self‐harm. Crisis, 2007; 28: 175–182. [DOI] [PubMed] [Google Scholar]


