Abstract
Background Interest and investment in e‐health continue to grow world‐wide, but there remains relatively little engagement with the public on this subject, despite calls for more public involvement in health‐care planning.
Design This study used two modified citizen juries to explore barriers and facilitators to e‐health implementation and the priorities for future e‐health research from the perspective of health service users and lay representatives. Citizen juries bring together a group of people to deliberate over a specific issue. They are given information and invited to ‘cross‐examine’ witnesses during the process.
Results Jurors were very keen for lay views to be included in e‐health development and embraced the citizen jury approach. They agreed unanimously that e‐health should be developed and thought it was in many ways inevitable. Although there was much enthusiasm for a health‐care system which offered e‐health as an option, there was as much concern about what it might mean for patients if implemented inappropriately. E‐health was preferred as an enhancement rather than substitute for, existing services. Lack of universal access was seen as a potential barrier to implementation but problems such as lack of computer literacy were seen as a temporary issue. Participants emphasized that e‐health research needed to demonstrate both clinical and economic benefits.
Conclusion There was broad support from the citizen juries for the development of e‐health, although participants stressed that e‐health should enhance, rather than substitute, face‐to‐face services. One‐day citizen juries proved a practical method of public engagement on this subject.
Keywords: citizen juries, e‐health, lay participation
Introduction
Rapid developments in technology are enabling many new applications of information and communications technology within the health‐care arena. 1 Defined as e‐health, this covers a broad spectrum of activities, which have been categorized into four domains: management systems; communication systems; decision support; and information systems. 2 Some of these, such as electronic patient record systems or prescription management systems, are located within health‐care organizations. 3 Others, such as websites or condition‐specific communities of interest, provide the public with unprecedented access to health information. Such information can shape their expectations and behaviour, with the potential to enhance healthy lifestyle and disease prevention choices. 4 Decision support may assist reconfiguration of the workforce while enhanced communications may enable more integrated services and support clinical management of acute and lifelong illness. 5 Advances in remote monitoring can facilitate the management of lifelong conditions such as heart failure. 6 Such e‐health applications are particularly important in rural and remote communities, and can facilitate the dissemination of information to remote practitioners as well as to the public. 7
E‐health offers many opportunities for individual patients, the wider public and clinicians. Public consultation on the development of e‐health is important because it can fundamentally change the way in which healthcare is provided, 8 and change the relationship that individuals have with health services and service providers. 9 , 10 Thus, it is essential that members of the public are consulted about future developments to ensure that quality and equity 4 and public as well as professional perspectives are available to inform e‐health service developments. There is currently a plethora of literature about patient satisfaction with e‐health, 11 although methodological deficiencies limit the utility of much of this literature, 12 and some consultation with clinicians. 13 , 14 , 15 However, engagement with the public about the development of e‐health has received much less attention. 12 , 16
This gap in the literature, with regard to public perspectives on e‐health, is important because of the growing interest in developing and evaluating the use of e‐health technologies. There have been concerns about the potential for a ‘digital divide’, in which those in areas of socioeconomic deprivation have poorer access to the new technologies associated with e‐health such as the Internet and digital television. This may, in turn, lead to the adoption of new e‐health services increasing rather than decreasing health inequalities. However, there is a paucity of work that investigates public views of such issues. 12 Also, there is evidence that rurality is associated with different patterns of health and health behaviours and that the challenges of health service delivery vary according to remoteness. 17 It is therefore important that public perspectives across different contexts, urban, rural and remote settings are explored to identify commonalities and also issues unique to certain contexts.
While a major driver for e‐health is the need to increase access to and efficiency of services in remote and rural areas, there are opportunities to use e‐health technologies in urban areas as well. Recently, a multi‐institutional group based in Scotland called HAVEN, (e‐Health: Addressing eValuation, implEmentation and integratioN; a collaboration involving partners from the Universities of Glasgow, Aberdeen and Dundee, the Centre for Rural Health, the Scottish Centre for Telehealth and the Scottish School of Primary Care) has carried out scoping work to explore the extent and type of e‐health research and development across the country and has sought the views of both health‐care professionals and the public with respect to the development of e‐health technologies. 18 , 19 As part of this, we conducted two citizen juries, one in a rural and the other in an urban setting, with health service users, lay patient representatives and carers. The findings from these juries are reported in this paper. Citizen juries are becoming increasingly popular as a method of eliciting public opinion. 12 Internationally, they have deliberated on a range of issues including health. 20 This article reports the findings of two modified citizen juries exploring public perspectives on e‐health.
Methods
We conducted a rural and an urban citizen jury, with twelve purposively recruited lay representatives in each. These ‘jurors’ were recruited from local disease‐specific Managed Clinical Networks (MCNs) and organizations such as Age Concern, Chest Heart and Stroke Scotland (CHSS) and NHS public participation networks. A Managed Clinical Network is a network of health staff (including doctors, pharmacists, nurses, health visitors, physiotherapists and occupational therapists) and organizations from primary, secondary and regional health care working together to make sure that high quality clinically effective services are fairly distributed. A number of these organizations have patient representation from which we recruited some of our jurors.
The staff within the organizations approached members based on particular demographic characteristics such as age, gender and ethnic and social background. We were keen to recruit ‘jurors’ with a range of demographic characteristics and with some experience of being on committees. We thought that ‘jurors’ with committee experience would be more comfortable and more able to represent their views in the more limited timescale of our planned, 1‐day citizen juries. Potential ‘jurors’ were approached to balance broadly the characteristics of those already recruited. For example, if the sample was predominantly older women, staff was asked to approach younger men.
We ran modified citizen juries of only 1‐day duration in contrast to the format of a typical citizen jury, which runs for between 2 and 5 days depending on the issues being debated. We chose 1 day for two main reasons. First, we thought that it would be more difficult to recruit ‘jurors’ for a 4‐day event, particularly for the remote and rural citizen jury, as in our experience, it can be more difficult to engage members of the public who live remotely from centres of population. Secondly, we judged that it would be adequate to discuss views on e‐health within a 1‐day structure. We wanted to confirm that this approach was feasible and could serve as a pragmatic and economical means of eliciting public views on this subject. This could then provide a valuable model for any future planned public engagement initiatives in this area. The process is described below and outlined in Fig. 1.
Figure 1.
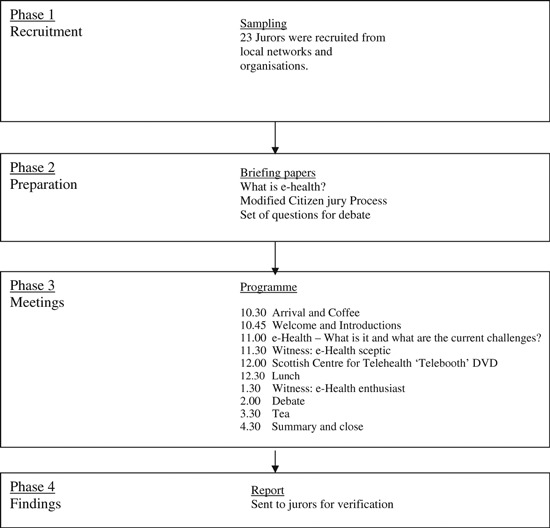
The process of the HAVEN citizen juries.
The citizen jury
Prior to the jury, participants were sent introductory material about the HAVEN study, 19 a description of e‐health and the citizen jury process. Participants also received a programme for the day, the aims of the jury and a set of questions to be debated. These questions addressed key issues under investigation by the HAVEN group and paralleled those discussed with policymakers and health professional key informants. 21
The questions were:
-
1
Do they think e‐health should be developed and why?
-
2
What do they think are user’s priorities and why?
-
3
What do they see as the biggest barriers to the uptake and utilization of such services?
-
4
How could these be overcome/addressed?
The first half of the day was designed to increase their knowledge about e‐health and its current and potential development. This included watching a DVD which provided an overview of e‐health and hearing from two ‘witnesses’ who delivered key messages about e‐health from their perspective. We engaged two clinicians with opposing perspectives, to provide jurors with a spectrum of opinion: one an e‐health enthusiast, the second a sceptic. The jurors were then given the opportunity to cross examine these witnesses.
During the afternoon, the jury debated the pre‐set questions in the presence of a moderator. The debate and questions were recorded and notes were taken by one of the researchers and one of the jurors. Jurors were asked to make specific decisions regarding the questions put to them and identify key points, which could be agreed upon before moving on to other questions. If there were dissenting views, jurors were encouraged to discuss and debate these. This process was recorded and key points agreed which reflected the outcomes of this process. The recordings and notes were then used to produce a comprehensive report, which was sent to jurors for verification as an accurate record. Jurors were given the opportunity to make changes to this report. In addition, jurors were also given an evaluation form to complete and were asked to rate various aspects of the day using a five‐point Likert scale. Lunch and refreshments were provided and expenses reimbursed.
Data analysis
The analysis of the debate was underpinned by a thematic approach. 22 This involved a four‐stage process: the development of the coding schedule; the coding of the data; description of the main themes; and developing explanations of the relationships between themes. The coding schedule was developed following extensive re‐reading of the transcripts, informed by a literature review and discussion amongst the research team. Using the coding schedule, two members of the study team coded the two transcripts independently. Comparison of coding highlighted that the researchers had consistently coded the same passages, but applied different codes to those passages, with differences in the interpretation of the meaning of the codes. During discussion between the two coders and other members of the team, it was apparent that this was because some of the codes overlapped. The codes were thus simplified, reapplied and the data grouped into categories. Consensus was reached at this point. During this process, the transcripts were examined for similarities and differences between the two juries.
Results
Sampling and recruitment
Of the twelve people invited to each jury, all attended the urban jury and ten attended the rural jury. There was an evenly balanced distribution of men and women in both groups, with most jurors between 50 and 70 years of age. The samples for both juries were skewed towards older participants. This was not intentional, but reflected the age demographic of the population approached. All ‘jurors’ were British, used English as their first language and had at least some experience of presenting their views in a committee environment. None of the jurors had any specific experience or knowledge of e‐health, but most of the jurors had experience of using a mobile phone and computer (Table 1). The key issues from the juries are presented in the following section.
Table 1.
Characteristics of jurors
| Characteristics of jurors | Rural N = 10 | Urban N = 12 |
|---|---|---|
| Gender | ||
| Male | 5 | 5 |
| Female | 5 | 7 |
| Age group | ||
| Under 50 | 0 | 2 |
| 50–59 | 7 | 4 |
| 60–69 | 2 | 4 |
| 70+ | 1 | 2 |
| Access to technology | ||
| Mobile phone | 9 | 11 |
| Home computer | 9 | 9 |
| Confidence using technology | ||
| Confident using mobile phone | 8 | 9 |
| Confident using computer | 8 | 8 |
Citizen jury as a method of public engagement in primary care research
Jurors’ perceptions of the method, that is the use of a modified citizens jury, were explored. Eighteen of the jurors completed the evaluation form and results were positive with all respondents rating their overall experience as either good (n = 4), very good (n = 12) or excellent (n = 6). A majority (n = 17) said they would take part in a citizen jury again; the remainder said they might. One juror remarked
‘I particularly liked the format of the days’ events and felt it helped to stimulate debate and discussion’. (Urban Juror)
The jurors said that this process gave them time to learn about the subject and time to think about the issues and implications for them. However, some of them noted that there was little need for a debate about e‐health because they had common views on the questions. The researchers also noted that there was a lack of contentious debate within the juries. Despite this, they discussed the questions in detail and their conversations were lively. When asked to verify the subsequent juror report, one of them remarked
‘You highlighted the salient points and mercifully cut out our ramblings’. (Urban Juror)
Correspondingly, the researchers identified that there were large sections of the transcripts, which neither of them coded due to perceived lack of relevance to e‐health.
Reasons why e‐health should be developed
Jurors agreed unanimously that e‐health should be developed and was in many ways inevitable. They agreed that in addition to overcoming the problems of distance in the delivery of healthcare; it may be a way of coping with increased demand on health services in the future and could help spread resources further. They felt that it should be developed to allow a better use of resources and services with increased access to specialists. Jurors suggested that e‐health could be the mechanism, which makes the centralization and specialization of services work more successfully.
Clinically, they thought that e‐health would give them a wider range of services, speedier diagnosis and treatment with easier access to clinical expertise and more effective monitoring. Practically, they perceived that there would be cost savings on patient travel with fewer journeys for short face‐to‐face consultations that may not be needed as consultations could take place close to home with a doctor located remotely. Jurors also suggested that e‐health could lead to an improved clinical assessment if two doctors were involved in the consultation, that is, if there were a doctor examining the patient locally and interacting with a remote specialist together with the patient.
Finally, they suggested that e‐health might encourage self‐care with patients becoming more active in their own treatment. It was suggested that accessing health information and having more choice about which doctors they could consult could lead to greater patient empowerment.
Caveats and concerns about e‐health
Although there was much enthusiasm for a health‐care system which offered e‐health as an option, there was as much concern about what it might mean for patients. For example, what would happen if that system was developed inappropriately? The jurors had a number of specific concerns.
First, they were of the opinion that e‐health should enhance rather than substitute traditional services. For example, they wanted the District Nurse to use e‐health to monitor some patients, and still see those who needed face‐to‐face visits. Using this example, they did not want e‐health to replace all the visits that the District Nurse carried out, but be used to enhance this service.
‘That’s the main message I think we’re trying to put across, complementary is a right good word isn’t it and enhancement; that e‐health should enhance and not replace current and future services.’ (Rural Juror)
Jurors were concerned that if e‐health became more routine, this would lead to a poorer quality service if they chose a face‐to‐face consultation. They believed face‐to‐face services should be maintained because e‐health would not always be appropriate, depending on the medical conditions or type of patient:
‘..statistically one in four people are going to get some sort of mental health difficulty in their lifetime, that is one area of health where I would think there would be a very, very mixed view as to whether this is appropriate..’ (Rural Juror)
It was also suggested that e‐health may not be appropriate for individual patients in their day‐to‐day care pathway; it may depend on the context: one juror reflected upon their personal experience of a recent mental health condition. It was put forward that different conditions will manifest in different ways and that during their recent mental health problem, the use of technology would have led to feelings of discomfort. However, now that this mental health problem has improved and they are at a different stage of the illness, their reaction to technology is different.
Furthermore, they felt that at least the first meeting with a new health professional should always be a face‐to‐face consultation. Indeed, face‐to‐face meetings were viewed as the gold standard for care giving, with the human touch regarded as crucial in some circumstances.
In addition to this, any new systems which are put in place need to be reliable, safe and secure. Jurors were concerned that if e‐health systems were developed throughout the health service, it would be important to ensure that there were adequate back‐up systems if they failed:
And I’ve been to meetings upon meetings and people shuffle their feet for the first 20 minutes and the guy says, ‘But this isn’t compatible with my laptop. It’s no longer – is there a doctor in the house? It’s – is there an IT person in the house? I mean, a patient at home hasn’t a backup. So the back up would need to be built in (Urban Juror).
Finally, there were general concerns about how services would be redesigned in the future. Jurors talked about the fear of being over‐monitored. They did not want health‐care staff to watch them ‘too closely’. Conversely, they believed that there was a danger of staff being over‐reliant on technology; assuming that people are well and not checking up on them if they have monitoring equipment in the home.
Perceived barriers to the uptake and utilization of e‐health services
One of the main barriers the jurors spoke about was lack of home access and that the systems, for whatever reason, would not be available to everyone. They identified poor infrastructure including lack of access to equipment and telecommunication signals, such as satellite or broadband as potential difficulties. This was particularly a concern for the rural citizen jury participants. Alongside this, both juries had concerns that any new system had to be compatible with what is already there.
Lack of confidence, physical and intellectual skills were identified as barriers to using this technology. Other challenges included set‐up costs to the health service and potential costs to the individual, slow progress of implementation, and a lack of education and training. The question of likely adherence to e‐health technologies was raised. For example, one participant raised the point that not all people who are currently prescribed the community alarm pendant wears it.
Furthermore, the jurors discussed attitudinal and cultural barriers. Some jurors were negative about attitudes of doctors to ‘active patients’:
‘Patients may ask more questions as a result of looking on the internet, but you can get doctors who think that you have no right to be asking questions’. (Urban Juror)
As patients become more empowered, there was a belief that doctors conversely would feel more disempowered and may therefore resist any role change.
Overcoming barriers
There was a general agreement that some barriers would inevitably be overcome by advancing technology. For example, lack of computer literacy was seen as a temporary issue; as demographics change, younger people would be more computer‐literate.
Some jurors thought that it was good enough for people to be able to access e‐health services at their family practice setting or other local centre; others thought that it should be available in the home. Positive publicity and dissemination of evidence was important with more money needed for education and training, especially for older people. Alongside this, jurors believed that support from professionals and family was crucial to people adopting and using e‐health.
Jurors were keen to have more public and patient engagement in the development of e‐health. They identified a role for themselves in helping to overcome these barriers and influence the development of e‐health. This was described as ‘long term institutionalized public consultation’.
Jurors envisaged a positive future with enhanced services combining e‐health and traditional services based on need, which was dependent on the context for the patient. They perceived that e‐health could release resources to maintain face‐to‐face services, where appropriate, and so strengthen the health service.
‘I came down here a cynic and thought no, what we really need is face to face, we need touch, we need humanity but I can see how this could support the face to face, the touch and the humanity which mustn’t be lost’. (Rural Juror)
Differences between urban and rural juries
Representatives in the rural jury talked more about access to health‐care services. They highlighted the difficulties with travelling to see specialists and the frustration when the consultation was seen by the jurors as a misuse of their time and resources. One of them said:
‘By filtering out some of this unnecessary transportations (sic) there can be more accessible transport to those who do need it’. (Rural Juror)
Although the urban jurors did talk about e‐health being useful to reduce travelling to services, their discussions were more limited than those in the rural jury.
In the rural jury, e‐health and home monitoring were seen as distinct entities, and some jurors raised significant concerns about the development of home monitoring. There was some difference of opinion in this between those who had real concerns that vulnerable people could be left even more vulnerable by the development of home monitoring and those who dismissed this as a possibility. They did all agree, however, that home monitoring was different from e‐health. Conversely, the urban jurors did not make a distinction between home monitoring and e‐health. They were positive about its development and believed that home monitoring was important for keeping people safe in the community.
E‐health research and vision for the future
Jurors thought that research should be done and had suggestions for taking it forward. First, to identify the objectives of e‐health. Secondly, to synthesize and disseminate existing evidence and identify good practice. Thirdly, to undertake pilots and trials where there is a direct comparison to get empirical data, which give evidence about what works and what does not – this would include economic benefits analysis. Finally, to identify opportunities for using e‐health for ethnic minority communities.
Jurors envisaged a positive future with enhanced and improved services combining e‐health and traditional services based on need, which was dependent on the context for the patient. They perceived that e‐health could release resources to maintain face‐to‐face services where appropriate and so strengthen the NHS.
Discussion
There was broad support from the two citizen juries for the development of e‐health, although they stressed that e‐health had to be an enhancement to rather than substitute for face‐to‐face services. The jurors reported that their main priority was rapid diagnosis, with subsequent appropriate and timely treatment. Lack of home access to technology was identified as the most significant barrier to the uptake of e‐health services. However, jurors suggested that advancing technology would resolve this issue. Their vision of the future was a positive model where e‐health and traditional face‐to‐face services were integrated, based on patient need and dependent on the context. They thought it was important to consider geography but also the nature of the illness and the particular stage in the patient’s care pathway. In that vision, they hoped that wider use of e‐health would potentially save resources, releasing them for improved face‐to‐face services. This would mean that patients who needed to be seen face‐to‐face would still meet with health professionals, whereas other patients would be able to access health services remotely.
There were minor differences in the views of the two juries. The rural jurors were perhaps understandably more aware of access issues, but were also more concerned about the development of the use of home monitoring. Although this may not seem a specifically rural issue, it may have been that this group was more suspicious of these developments being used to erode existing services.
Limitations and strengths of the study
This study has a number of limitations. First, the modified citizen jury was a less extensive approach than described by other studies in the literature. 23 However, in our view, the 1‐day approach is adequate for topics such as this.
Secondly, there was a lack of contentious debate in the juries, although an informed response was achieved. We wanted to choose jurors who had some knowledge of health systems. This, as well as the age profile, may have limited the diversity of our sample and the intensity of the debate. Even with the sample chosen, there were periods of discussion which were tangential to the key questions.
Thirdly, on reflection, the juror’s pre‐set questions could have been more contentious. Others have highlighted particular challenges associated with using broad, open‐ended questions. 24 , 25 If the debate had been facilitated in a more adversarial style, or if the jurors had been forced to make resource constrained choices, it may have generated more conflicting views, which jurors would then have had to work through and reconcile.
Finally, providing jurors with information in advance of, and in the early part of the meeting, could be seen as potentially introducing bias to the proceedings and facilitating the regurgitation of the experts’ views in the encounter, 26 although it is noteworthy that this approach is commonly used 1 and in our opinion, the information we provided to the jurors was unbiased and we were transparent about what was known and not known about e‐health.
Our experience was that jurors discussed barriers and opportunities for e‐health which had not been placed before them. While their response to the development of e‐health was very positive, they identified clear and relatively sophisticated caveats against its use, which suggested that they were responding to information and using it to think for themselves. For example, in addition to the more obvious limitations of using e‐health with some patient groups and some specific illnesses, the jurors highlighted that some individuals would have different needs at different stages along their care pathway. This particular insight did not emerge from any of the literature provided.
Importantly, the 1‐day model did seem a pragmatic method for public engagement on this subject. Wakeford identified a number of critical features to pay attention to when conducting citizen juries. These included the recruitment strategy, transparency and independence. 27 Jurors were recruited purposively to get a broad range of demographic characteristics and to include lay people with some experience of representing a view in a group setting. The recruited jurors were able to contribute to the discussion and listen critically to others’ views and in this way the recruitment strategy was successful. The engagement was transparent: information given to the jurors was presented and communicated in a clear and accessible manner; the review of literature reflected both the opportunities and the challenges in the implementation of e‐health; during the day, the jurors were given as much time as they wanted to cross‐examine the witnesses. As university researchers who acted as moderators, we were aware of the significance of our influence on the process and strove to ensure independence. For example, we explained the challenge of our role to the jurors and refrained from giving our opinions when asked during the debate and at other times during the day. Finally, the jurors were asked to verify whether or not a written report of the day’s events was a true representation of their experience.
In our view, these citizen juries gave us good value for money and significant outputs for our investment. Namely, in addition to confirming results from other studies looking at this topic, 12 , 21 our jurors identified issues not previously reported.
Conclusion
The modified citizen juries we conducted in the sphere of e‐health permitted expression of public perspectives, something which is often missing from the rhetoric on this subject. Our approach was relatively inexpensive, which means that it is a method that could be replicated by policymakers and others wishing to engage with the public in this area, not least as a way of building public confidence in e‐health. E‐health was viewed positively, although not as a panacea, and crucially, was seen to be a useful adjunct rather than a substitute for traditional health service delivery methods. The lay participant vision of the future was one in which e‐health and traditional services were integrated, based on patient need and local circumstances, underpinned by a robust evidence base that had shown both clinical and economic benefits.
Source of funding
Scottish Funding Council, Strategic Research Development Grant, Edinburgh, UK. Grant HR06004.
Conflict of interests
No conflict of interest has been declared.
Acknowledgements
We acknowledge our HAVEN collaborators: Professor Frank Sullivan, Professor Jeremy Wyatt, Dr Joe Liu and Dr Colin Cowan of the University of Dundee; Professor Dave Godden of the University of Aberdeen; Dr Alex McConnachie of the University of Glasgow; and Professor Gordon Peterkin, former Director of the Scottish Centre for Telehealth.
References
- 1. Scottish Executive . Delivering for Health. 2005.
- 2. Mair FS, May C, Finch T et al. Understanding the implementation and integration of e‐health services. Journal of Telemedicine and Telecare, 2007; 13: S36–S37. [Google Scholar]
- 3. Boonstra A, Boddy D, Fischbacher M. The limited acceptance of an electronic prescription system by general practitioners: reasons and practical implications. New Technology, Work and Employment, 2004; 19: 128. [Google Scholar]
- 4. Wyatt JC, Sullivan F. eHealth and the future: promise or peril? British Medical Journal, 2005; 331: 391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sullivan F, Wyatt JC. How decision support tools help define clinical problems. British Medical Journal, 2005; 331: 831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Garcia‐Lizana F, Sarria‐Santamera A. New technologies for chronic disease management and control: a systematic review. Journal of Telemedicine and Telecare, 2007; 13: 62–68. [DOI] [PubMed] [Google Scholar]
- 7. Richards H, King G, Reid M, Selvaraj S, McNicol I. Remote working: survey of attitudes to eHealth of doctors and nurses in rural general practices in the United Kingdom. Family Practice, 2004; 21: 1–6. [DOI] [PubMed] [Google Scholar]
- 8. Kashefi EMP, Mort M. Grounded citizens’ juries: a tool for health activism? Health Expectations, 2004; 7: 290–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hutton W. Why the NHS needs people power. BMJ, 2007; 334: 69–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bennett F, Roberts M. From Input to Influence, Participatory Approaches to Research on Poverty. New York: Joseph Rowntree Foundation, 2004. [Google Scholar]
- 11. Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. British Medical Journal, 2000; 320: 1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mort M, Finch T. Principles for telemedicine and telecare: the perspective of a citizens’ panel. Journal of Telemedicine and Telecare, 2005; 11 (Suppl 1): 66–68. [DOI] [PubMed] [Google Scholar]
- 13. King G, Richards H, Godden D. Adoption of telemedicine in Scottish remote and rural general practices: a qualitative study. Journal of Telemedicine and Telecare, 2007; 13: 382–386. [DOI] [PubMed] [Google Scholar]
- 14. Benson T. Why general practitioners use computers and hospital doctors do not. Part 1 incentives. BMJ, 2002; 325: 1086–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vierhout WPM, Knottnerus JA. A randomised controlled trial of joint consultations with general practitioners and cardiologists in primary care. British Journal of General Practice, 2003; 53: 108. [PMC free article] [PubMed] [Google Scholar]
- 16. Turner J, Thomas R, Gailiun M. Consumer response to virtual service organisations: the case of telemedicine. International Journal of Medical Marketing, 2001; 1: 309. [Google Scholar]
- 17. Shucksmith M, Roberts D, Scott D, Chapman P, Conway E. The Arkelton Centre for Rural Development Research, University of Aberdeen. Disadvantage in rural areas. 1996; Rural research report number 29.
- 18. Clark JS, Mair FS, O’Donnell C, Liu J. E‐health: implementation and evaluation research in Scotland – a scoping exercise. Journal of Telemedicine and Telecare, 2008; 14: 119. [DOI] [PubMed] [Google Scholar]
- 19. Mair FS. e‐Health: Addressing eValuation, implEmentation and integratioN (H.A.V.E.N) Final report. 2008.
- 20. The Jefferson Centre . About us, 2009, Available at: http://www.jefferson‐center.org/index.asp?Type=B_BASIC&SEC={549A0987‐DDA4‐43F7‐8281‐678FDDBDE3D8}, Accessed 15 June 2009.
- 21. Boddy D, King G, Clark JS, Heaney D, Mair F. The influence of context and process when implementing e‐health. BMC Medical Informatics and Decision Making, 2009; 9: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ritchie J, Spencer L. Qualitative data analysis for applied policy research In: Bryman A, Burgess R. (eds) Analysing Qualitative Data. London: Routledge, 1993: 173–194. [Google Scholar]
- 23. Pidgeon N, Rogers‐Hayden T. Opening up nanotechnology dialogue with the public: risk communication or ‘upstream engagement’. Health, Risk and Society, 2007; 9: 191–210. [Google Scholar]
- 24. Gooberman‐Hill R, Horwood J, Calnan M. Citizens’ juries in planning research priorities: process, engagement and outcome. Health Expectations, 2008; 11: 272–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lenagham J, New B, Mitchell E. Setting priorities: is there a role for citizens’ juries? [Miscellaneous]. BMJ, 1996; 312: 1591–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Coote A, Lenagham J. Citizens’ Juries: Theory into Practice. London, UK: Institute for Public Policy Research, 1997. [Google Scholar]
- 27. Wakeford T. Citizens Juries: a radical alternative for social for social research. Social Research Update, 2002; 37: 1–2. [Google Scholar]


