Abstract
Background Health literacy is the ability to obtain, interpret and use health information. Low rates of health literacy in Australia have been suggested, but no validated measure exists.
Objective To explore health literacy competencies in a sample of community pharmacy consumers.
Design Structured interviews were undertaken by a team of researchers during August, 2009. The instrument was derived from available literature, measuring aspects of functional, interactive and critical health literacy regarding use of medicines.
Setting and participants Twelve community pharmacies in the Brisbane region, Australia.
Results Six hundred and forty‐seven consumers participated; 64% were women. A wide distribution of ages was evident. English was the first language of 89% of respondents. More than half of the sample (55%), predominantly aged 26–45 years, was tertiary educated. While 87% of respondents recognized a sample prescription, 20% could not readily match the prescription to a labelled medicine box. Eighty‐two percentage of respondents interpreted ‘three times a day’ appropriately, but interpretation of a standard ancillary label was highly variable. Advanced age, less formal education, non‐English‐speaking background and male gender were independently related to lower performance in some variables.
Discussion This health literacy measure applied comprehension and numeracy skills required of adults receiving prescription medications. While the majority of consumers adequately performed these tasks, some behaviours and responses were of sufficient concern to propose additional verbal and written information interventions by pharmacy staff.
Conclusions This research provides insight into issues that may affect consumers’ appropriate use of medicines and self‐efficacy. Initiatives to improve public health literacy are warranted.
Keywords: consumers, health literacy, instructions, labels, medicines, pharmacy
Introduction
Health literacy is defined as the ability of health consumers to obtain, understand, interpret and use information regarding their health. 1 The definition varies according to the context in which it is applied, although it is widely recognized that health literacy need not directly correspond to an individual’s level of education. 2 A health literate individual will be able to apply basic skills in reading, writing and numeracy to materials related to health and use the available information to inform appropriate health‐care activity, 3 , 4 thus demonstrating self‐efficacy and empowerment in his/her use of medicines and participation in health‐related decisions. 1 , 5 , 6 , 7 Indeed, numerous researchers have established that poor health literacy is a recognized problem and can compromise the quality use of medicines and health of consumers. 1 , 5 , 6 Moreover, the concept of health literacy has been recognized internationally in position papers relating to public health priorities 1 , 8 and has been described in Australia as a ‘key strategy that will underpin strengthened consumer engagement.’ 5 While patients are generally not involved in health decisions to their desired extent, not everyone is equally equipped, in terms of their health literacy, to be so involved. 5
There is a considerable body of international evidence supporting the prevalence of individual components of health literacy, such as reading ability, the consequences of poor health literacy and interventions to improve health literacy. 4 Consequences of poor health literacy include miscomprehension of instructions, inability to read labels, inadequate adherence to prescribed regimens and inability to assimilate and comprehend advice from health professionals. 3 These concepts are relevant to the health literacy of pharmacy consumers, who are at risk of under‐ or over‐treatment and medicine‐related events if unable to manage their treatment regimens. To optimize the medicine‐related advice provided in community pharmacy and enhance the safe and appropriate use of medicines, insight into the collective issues surrounding health literacy in pharmacy consumers is needed. Currently, there is no valid measure in Australia that encapsulates functional, communicative and critical components of health literacy.
Research conducted in the United States relating to pharmacy consumers has reported that almost 50% of the population has poor health literacy. 9 Specifically, patients with lower health literacy were less able to read and interpret commonly used warning labels, prompting the researchers to recommend the use of simplified labels and particular counselling techniques by pharmacists to enhance patients’ comprehension. 2 , 9 Some components of this study may be adaptable for use in Australian pharmacy practice.
According to the Australian Bureau of Statistics, approximately 59% of Australians aged 15–74 years have poor health literacy. 5 , 10 These findings were based on the 2006 Adult Literacy and Life Skills Survey, which examined, among other aspects, health maintenance and system navigation. 5 , 10 However, the findings were not based on practical exercises, did not gain insight into the specific areas of need and were based on overseas measures without validation for use in Australia. Other limitations relate to the complexity of the measurement and low response rates. 6 Recently, the Newest Vital Sign has been applied as a measure of functional health literacy in a brief survey of 2824 South Australians aged at least 15 years. 6 The key task, based on reading and interpretation of a nutrition panel from a food item, has potential to be converted to similar exercises relating to interpretation of instructions for use of medicines, although it gives limited insight into communicative and critical abilities.
The limited research in this area, along with the recognized role of pharmacists in encouraging responsible use of medicines, identified a need for exploration of health literacy relating to medicines obtained from pharmacies, which could inform the development and validation of measures for use in larger‐scale studies to quantify the prevalence of these issues.
Method
The objective of this study was to explore issues relating to health literacy in a sample of pharmacy consumers. It was expected that consumers accurately comprehend the majority of instructions relating to a given hypothetical medicine.
The research team comprised 16 Bachelor of Pharmacy students (all completing a final‐year research project) and three academic supervisors. The field research comprised in‐store interviews with medicine purchasers in community pharmacies using a structured instrument. Ethical approval was obtained from the Human Research Ethics Committee of School of Pharmacy, The University of Queensland.
To inform the development of the interview instrument, three of the researchers, under the guidance of a librarian and an academic supervisor, undertook a review of the published literature using EMBASE, Sociology, PubMed, PsycInfo and Web of Science. Search terms and themes included health literacy, patient/consumer comprehension of pharmacy, language (including the use of English as a second language), pharmacy counselling and communication issues. Literature to guide questionnaire design and interviewing was also sourced and reviewed.
The research team participated in questionnaire design, task sharing and follow‐up communication. The group meetings served to discuss and reach consensus on question face validity and comprehensibility and drew on the literature reviewed by the aforementioned subgroup. A researcher with expertise in psychometrics attended one of the group meetings to critique the structured interview instrument.
The interview instrument (Fig. 1) comprised 10 questions related to measurement of health literacy of pharmacy consumers, with age, gender, formal education and first language as predictors of health literacy. 5 , 6 The instrument was designed to be completed by brief interview with one researcher, and another noting the responses. The interview design allowed the researchers to clarify and document verbal responses that would otherwise be compromised in a self‐completed questionnaire. The respondent then self‐completed the demographic questions on the reverse, before filing the questionnaire to retain privacy. Standardized props, comprising hypothetical prescriptions, labelled medicine boxes and blister‐pack tablet strips (Fig. 2), were produced to support the questions.
Figure 1.
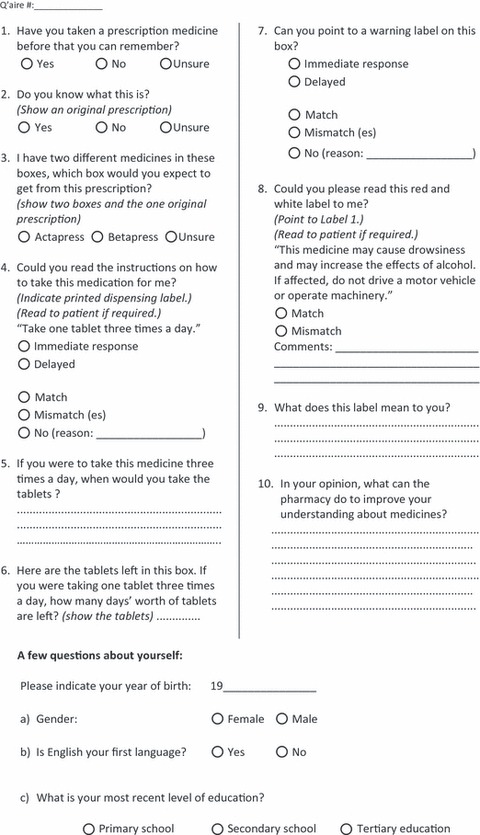
Questionnaire.
Figure 2.
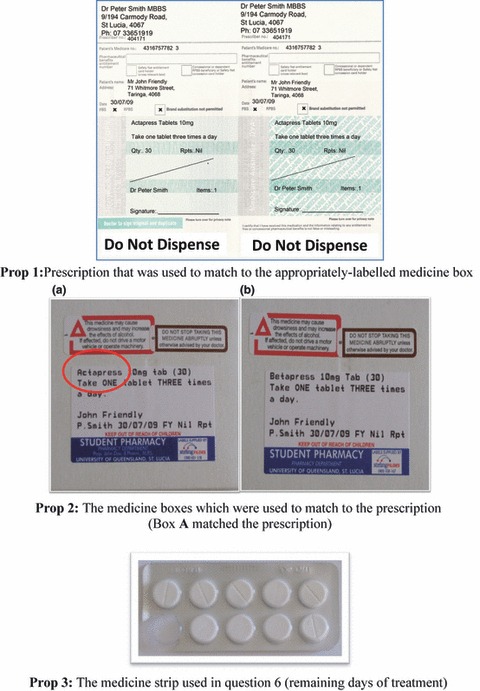
Props used in interviews.
The instrument explored key components of health literacy:
-
1
Functional health literacy, incorporating reading and numeracy skills, 9 measured in questions 3, 4, 6, 7 and 8. The focus on a single concept, in this case, hypothetical labelled medicines, is similar to the approach reported by Adams et al. 6 in their questions relating to a nutrition panel from a food item.
-
2
Interactive (or communicative) health literacy, assessing the ability to hold a conversation with a health professional about the meanings and options for actions, 11 investigated in questions 5 and 9.
-
3
Critical health literacy, assessing the ability to rationalize a situation and suggest courses of action, 11 investigated in question 10.
The questionnaire was pilot tested by 12 researchers who recruited approximately 10 lay health consumers each. The data obtained from the pilot study were reviewed and resulted in minor refinements to the interview instrument.
Twelve pharmacies were purposively selected in the south‐east Queensland region of Australia based on convenience of location to allocated pairs of researchers, and their distribution checked to cover a wide cross‐section of suburbs and potential clientele types. The respective managers of these pharmacies gave signed consent to host the data collection in their pharmacies. Pairs of researchers undertook data collection in each pharmacy for two or three consecutive days. Previous research has found that such sampling of pharmacies provides a range of socio‐demographic clientele characteristics. 12 , 13 A total sample size of 400 responses was anticipated to allow statistical analysis of the composite data and to provide feedback specific to each pharmacy.
Data collection took place during the week of 3rd–7th August, 2009, during regular business hours. Consumers interviewed were at least 16 years of age and conversant in English and included those for whom English was not their first language (Australian society is multicultural; English is accepted as the official language). Verbal consent was obtained from each customer before proceeding with the interview. The interviews took place in a quiet area of each pharmacy.
The data were entered into Excel® by each pair of students, then merged, screened and analysed by a supervisor, using SPSS Version 17. Data produced for each pharmacy allowed for a report to be written for that pharmacy. The collective data were analysed using descriptive statistics.
Results
A total of 647 customers from 12 pharmacies participated in the survey over the 5‐day period. The most common reason for non‐participation was customers reporting to be in a hurry.
Description of the sample
The majority of respondents were women (64.1%, n = 414). While ages (when classified in 10‐year brackets) were quite evenly represented, respondents aged 36–45 years were most common in this sample. There was no significant relationship (P > 0.1) between age, in 10‐year brackets, and gender.
The majority of respondents (89.3%, n = 578) reported English as their first language. Overall, 54.7% of respondents (n = 352) had attained tertiary qualification(s), while 37.9% (n = 244) had secondary‐level education and 7.5% (n = 48) had primary education. There was a significant inverse relationship between this variable and age (χ2 = 136.5, d.f. = 12, P < 0.001).
Health literacy measures
The majority of respondents (86.7%, n = 561) readily recognized the sample prescription (Fig. 2, Prop 1), and an even greater proportion (95.1%) recalled taking a prescription medicine. However, when matching the prescription with the correctly labelled box (Fig. 2, Prop 2), 17.6% of the participants (n = 114) were unsure and 2.2% (n = 14) mismatched the labelled box with the prescription. Influences of demographic variables on these concepts are explored later. Further, 7.6% of participants (n = 49) could not readily or accurately read the instructions on the box in the font normally used in community pharmacy.
For tablets to be taken three times daily, 82.4% of the respondents (n = 533) indicated a schedule of ‘breakfast, lunch, dinner’ dosing, as opposed to all three doses together or at irregular intervals. The follow‐on task, calculating the number of remaining days of treatment given a blister card containing nine remaining tablets, resulted in 93.4% of respondents (n = 604) correctly calculating 3 days as their answer.
Identifying and then reading, a warning label was correctly performed by the majority of consumers (96.3 and 91.3%, respectively, of 647 respondents). Failure to answer this question was mainly associated with respondents reportedly not having their spectacles with them. Interpretation of the warning label (Fig. 2, Prop 2, Label 1) was highly variable. Responses are categorized in Table 1.
Table 1.
Interpretation of ancillary label 1
| Interpretation of ancillary label 1 | No. of responses | % of responses |
|---|---|---|
| ‘Don’t drive and/or operate machinery’ | 117 | 18.1 |
| ‘May cause drowsiness, so don’t drive/use machines if affected’ | 108 | 16.7 |
| ‘Don’t drink and/or drive/operate machinery’ | 104 | 16.1 |
| ‘Will feel drowsy; don’t drive and/or don’t drink’ | 58 | 9.0 |
| ‘May cause drowsiness/dizziness/sleepiness’ | 56 | 8.7 |
| ‘Don’t drink’ | 31 | 4.8 |
| Quoted the label | 26 | 4.0 |
| Explained the label correctly | 25 | 3.9 |
| ‘May cause drowsiness, and don’t drink if affected’ | 23 | 3.6 |
| Customer doesn’t drink or drive, so felt that the question is irrelevant/no response* | 21 | 3.3 |
| ‘If driving and/or drinking, don’t take the medicine’ | 17 | 2.6 |
| ‘Very serious medicine, stay at home and/or don’t drive’ | 14 | 2.2 |
| Other responses | 47 | 7.3 |
*Some customers felt that the ancillary label was too small to even notice it on the medicine box and/or would consult the doctor, who would explain it to them.
In terms of how pharmacy staff could improve consumers’ understanding of medicines, the most common responses related to counselling and other verbal services (22.9% of all responses), followed by written information (15.3%). Specific areas of need were explanation of instruction labels, medicines information sheets and generic substitutions, and textual and graphical enhancement of instruction and warning labels.
Demographic influences on health literacy
The four recorded demographic variables (age, gender, education and language) were analysed as potential influences on key indicators of health literacy: recognition of a prescription, identification of the prescription box, reading of instructions and identification of a warning label.
Age
There was no significant relationship between age and recognition of a prescription or reading of an instruction label. However, advancing age was significantly associated with matching of the prescription to the incorrectly labelled box (χ2 = 31.2, d.f. = 6, P < 0.001) (Fig. 3). A similar association was identified in relation to incorrect or delayed identification of a warning label on the box (χ2 = 18.1, d.f. = 6, P < 0.006).
Figure 3.
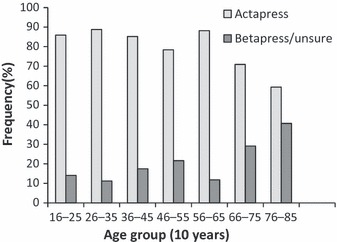
Identification of Correct Medication (Actapress) by Age (n = 631).
Gender
There was a weakly significant relationship between gender and ability to recognize a prescription; women (88.9%, n = 368) were more likely than men (82.8%, n = 192) to correctly answer this question (χ2 = 4.8, df = 1, P < 0.03). Additionally, 83.1% of women (n = 344) correctly identified the Actapress box to match the prescription, compared to 75.0% of men (n = 174) (χ2 = 6.1, d.f. = 1, P < 0.01). However, there were no significant relationships between gender and recognition of a warning label or correct reading of an instruction label.
Education
There was no significant relationship between level of formal education and recognition of a prescription or accurate reading of the instruction label. However, education did have a significant association with ability to match the medicine box to the prescription, where a higher percentage of customers with tertiary education (86.1%, n = 303) were able to match the correct labelled box with the prescription, compared to 60.4% of those who had only primary education (n = 29) (χ2 = 22.1, d.f. = 2, P < 0.001). Additionally, there was a significant relationship between the level of formal education and recognition of the warning label; a higher percentage of respondents with tertiary education (96.6%, n = 340) were able to immediately point to a warning label compared to 85.4% of those with primary education (n = 41) (χ2 = 11.4, d.f. = 2, P < 0.003).
First language
English as a first language was significantly related to correct responses to all four indicators of health literacy (Table 2).
Table 2.
Relationship between English as a first language and health literacy measures
| Health literacy indicator | Options | First language: English (%) | First language: other (%) | Statistical significance |
|---|---|---|---|---|
| Recognition of prescription | Yes | 89.3 | 64.7 | χ2 = 31.8 df = 1 P < 0.001 |
| No/Unsure | 10.7 | 35.3 | ||
| Correct matching of the Actapress box to the prescription | Actapress | 81.3 | 70.6 | χ2 = 4.4 df = 1 P < 0.036 |
| Betapress | 18.7 | 29.4 | ||
| Correct reading of instruction label | Immediately | 94.1 | 77.9 | χ2 = 22.7 df = 1 P < 0.001 |
| Delayed/did not read the label | 5.9 | 22.1 | ||
| Recognition of warning label | Immediately | 95.2 | 85.3 | χ2 = 10.7 df = 1 P < 0.001 |
| Delayed/did not point to a label | 4.8 | 14.7 |
Discussion
Current research on health literacy suggests that it is an under‐recognized problem in health care and that people with lower levels of health literacy lack the skills and knowledge to understand the appropriate way to use medicines, hence compromising their safe and effective use of medicines. 14
This study explored functional, interactive and critical health literacy, using questions that investigated comprehension and numeracy skills required of an adult consumer receiving a prescription medicine from a community pharmacy. The sample of 647 respondents exceeded the intended 400 respondents and facilitated statistical comparisons. Further multivariate and qualitative analyses will be reported elsewhere.
While the majority of participants were familiar with key aspects of prescriptions, the questions that required understanding of instruction and warning labels challenged some. Our data revealed that nearly one in five participants miscomprehended the dose spacing implied by ‘take ONE tablet THREE times a day,’ an error that could lead to sub‐therapeutic effects, overdose or other undesirable effects. Further, while nearly all participants were able to identify a warning label on a medicine box, only 4% correctly and fully explained the concepts within the label; others commonly truncated and interpreted the key message as ‘avoid alcohol’ or ‘do not drive’, losing the subtleties of the message. While the interpretations commonly erred on the side of conservatism and few could be considered dangerous, it was of some concern that a number of participants mentioned that they ignore labels where the print size is too small, which could have critical consequences depending on the medicine. Conversely, others stated that they would be cautious if they saw a warning label even it was unreadable. This latter reticence may be insufficient to avoid harm, but in some cases, the medicine might not be taken at all. In general though, ignorance or misunderstanding of this label, which advises of possible drowsiness and enhanced effects of alcohol and warns about driving or operating machinery if affected, has the potential to increase an individual’s risk of injury and/or excessive sedation (Table 1).
One indicator of functional literacy required participants to calculate the number of days’ worth of tablets remaining, given a card containing nine tablets; this was accomplished by 93% of the consumers. Our findings differ from those of Adams et al., 6 in which 21% of their sample were deemed highly likely to have ‘inadequate functional health literacy’ based on a series of six questions in a large‐scale household survey. While the questions in these studies cannot be directly compared, it could be that our approach of pharmacy clients in pharmacies overestimates the functional health literacy of consumers at large.
A higher proportion of female consumers (64%) participated in the study. This proportion reflects the gender difference in other studies of purchasing behaviour in pharmacies in the Brisbane region 12 , 13 and the greater prevalence of long‐term health conditions amongst women in Australia 15 that is expected to be mirrored in pharmacy visits. Responses from our female participants were marginally more accurate than those from men, where women were able to more confidently recognize a prescription and correctly match the prescription to a choice of two labelled boxes. Overall, however, our study found that the determinants of health literacy were similar among men and women, consistent with the findings by Adams et al. 6
Previous studies have found that poorer health literacy is more common as age (>65 years) increases. 6 , 10 The process of ageing is associated with decline in biological and physiological functioning, which can lead to multiple medical conditions and reduced mental processing skills, 10 with potentially more confusion as a result of managing more medicines. These issues, and additional factors such as lower levels of formal education in the older generation, which significantly correlated with advancing age in our study, could contribute to poor health literacy in older health consumers. 10 Further, an increasingly complex health system could be a reason why earlier learning experiences are not useful as consumers’ age. A counter‐argument, not supported by our data, is that greater exposure to prescription medicine use in the elderly may enhance their familiarity and vigilance with medicines. In our study, 71% of customers aged >65 years were able to correctly match the sample prescription to the labelled box, compared to 89% in the 26–35 years age group. The responses from the elderly population were also more delayed, and vision problems led to some difficulties in reading the instruction and identifying and reading warning labels. These findings are similar to those from previous studies. 10 , 16 A common reported reason for participants not attempting to read the warning label was not having spectacles on their person. Research has identified that ‘making excuses’ is a coping mechanism for patients who have trouble reading medical forms and instructions. 17 The association of greater formal education and health literacy is worthy of further exploration. While at face value, this finding is logical, it is interesting that there remain a number of tertiary‐educated respondents who did not manage the tasks; this could be related to the tasks requiring interpretation and application of given information.
English was the first language for 89% of our respondents. Lack of English proficiency was associated with delayed and/or incorrect responses, lower likelihood of familiarity with the appearance of a prescription (65% vs. 89%) and greater difficulty in matching the prescription to the correctly labelled box, reading instructions and in recognizing a warning label. These data suggest that, however, difficult, pharmacists need to undertake medicine‐related counselling with non‐native‐English speakers to enhance their understanding of medicines information and appropriate usage. This, of course, assumes that the language deficiencies lie with the consumer, rather than the health professional; the latter is a topic of some concern and is being addressed in local initiatives. 18
Most participants readily offered suggestions to improve their understanding of medicines, predominantly relating to greater provision of verbal and written information, with a repeated message indicating the need for personalized counselling on indications for medicines, side effects and drug interactions, especially for initial therapy. These suggestions included larger font and simple wording on labels accompanied by clear explanations. In relation to generic substitution of medication, consumers expressed the need for tailored information. These suggestions may contribute toward improved adherence to a prescribed regimen. As such, it is recommended that pharmacists discuss relevant information and determine the consumers’ comprehension of this information.
Such communication is considered a core competency for pharmacists in Australia, 19 but data on the application of this competency are not readily available. Internationally, it is recognized that insufficient instructions are given to medicine consumers by general practitioners and pharmacists and that written information is a valuable reinforcement for verbally communicated instructions. 7
There were some limitations to this study:
-
1
The pharmacies were chosen to reflect a geographical spread through the Brisbane metropolitan and surrounding areas. However, as the study was limited to clients presenting to metropolitan pharmacies and did not extend to rural areas, where socio‐demographic differences may distinguish them from the metropolitan sample, we cannot affirm that the data represent a cross‐section of the population who use medicines.
-
2
Pilot testing was limited to around 120 respondents. While this identified a number of improvements, a second pilot testing stage was not possible because of the timeline of the study. In lieu of this, review and refinement of the questionnaire by the research team served to enhance the face validity of the questionnaire.
-
3
The study was limited to English‐speaking participants; that is, people who were conversant in English irrespective of whether English was or was not their first language. We cannot guarantee that the non‐native English speakers surveyed were representative of all ethnic groups in this region. Indeed, our interpretation of health literacy issues in non‐native English speakers may under‐represent the problems faced by this group. Further application of this survey, in different geographical regions and a broader cross‐section of the population, is warranted to quantify the prevalence of the identified issues.
-
4
It was beyond the scope of this study to recruit participants from all levels of health literacy; instead, this study is considered to explore a range of health literacy issues amongst pharmacy consumers who were willing to participate.
This study has elicited a number of important and unexpected findings amongst even highly educated and literate individuals. A contribution of this research to the field of health literacy is the inclusion of questions that facilitated explanatory responses; published health literacy instruments (e.g. the Newest Vital Sign 6 , REALM 3 , 20 ) have often focussed on knowledge rather than descriptive responses. There is potential to apply the instrument used in this study to other aspects of health behaviour, such as non‐prescription medicines and self‐care. However, the exploration of health literacy reported here may not relate to an individual’s ability to make beneficial health decisions; this is an area that warrants further research.
In conclusion, this study has provided insight into how community pharmacy consumers apply given information about medicines. Overall, the majority of participants comprehended the given information and displayed levels of health literacy that may result in safe and effective use of prescription medications. A key area of concern was consumers’ inability to readily locate a warning label on a sample medicine box, independently associated with advanced age, less formal education and non‐English‐speaking background. Further, incorrect matching of a sample prescription to a labelled box was associated with these three demographic variables, as well as male gender. These issues may result, respectively, in inappropriate use and mismanagement of medicines.
Observance of these needs for information in the pharmacy is considered paramount to improve the health literacy, and therefore, health outcomes, of consumers.
Funding sources
This study was conducted with financial support from the Pharmacists Board of Queensland. However, the views expressed do not necessarily represent the view of its members, Executive or staff of the Office of Health Practitioner Registration Boards.
Conflicts of interest
None.
Acknowledgements
The authors acknowledge the assistance of the pharmacists, pharmacy staff and consumers at the pharmacies who participated in the study, the final‐year Pharmacy students of The University of Queensland who assisted with questionnaire design and data collection, and academic input from Dr Remo Ostini.
References
- 1. The Joint Commission . “What did the doctor say?:” Improving health literacy to protect patient safety. Health Care at the Crossroads report 2007. Available at: http://www.jointcommission.org/nr/rdonlyres/d5248b2e‐e7e6‐4121‐8874‐99c7b4888301/0/improving_health_literacy.pdf. Accessed 18 December 2009.
- 2. Jeppesen KM, Coyle JD, Miser WF. Screening questions to predict limited health literacy: a cross‐sectional study of patients with diabetes mellitus. Annals of Family Medicine, 2009; 7: 24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mancuso JM. Assessment and measurement of health literacy: an integrative review of the literature. Nursing & Health Sciences, 2009; 11: 77–89. [DOI] [PubMed] [Google Scholar]
- 4. Coulter A, Ellins J. Effectiveness of strategies for informing, educating and involving patients. British Medical Journal, 2007; 35: 24–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nutbeam D. Building health literacy in Australia. Medical Journal of Australia, 2009; 191: 525. [DOI] [PubMed] [Google Scholar]
- 6. Adams RJ, Appleton SL, Hill CL, Dodd M, Findlay C, Wilson DH. Risks associated with low functional health literacy in an Australian population. Medical Journal of Australia, 2009; 191: 530–534. [DOI] [PubMed] [Google Scholar]
- 7. Raynor DK. Addressing medication literacy: a pharmacy practice priority. The International Journal of Pharmacy Practice, 2009; 17: 257–259. [PubMed] [Google Scholar]
- 8. UK Department of Health . Choosing health: making healthy choices easier. Annual report; 2005: Feb 24. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/Browsable/DH_4097491. Accessed 18 December 2009.
- 9. Wolf MS, Davis TC, Tilson HH, Bass PF, Parker RM. Misunderstanding of prescription drug warning labels among patients with low literacy. American Journal of Health-System Pharmacy, 2006; 63: 1048–1055. [DOI] [PubMed] [Google Scholar]
- 10. Australian Bureau of Statistics . Health literacy 2006. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4233.02006?OpenDocument. Accessed 18 December 2009.
- 11. Nutbeam D. The evolving concept of health literacy. Social Science & Medicine, 2008; 67: 2072–2078. [DOI] [PubMed] [Google Scholar]
- 12. Emmerton L. Purchasing behaviour for non‐prescription medicines. Australian Pharmacist, 2005; 24: 326–330. [Google Scholar]
- 13. Emmerton L. Behavioural aspects surrounding medicine purchases from pharmacies. Pharmacy Practice, 2008; 6: 158–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Davis TC, Michielutte R, Askov EN, Williams MV, Weiss BD. Practical assessment of adult literacy in health care. Health Education & Behavior, 1998; 25: 613–621. [DOI] [PubMed] [Google Scholar]
- 15. Australian Institute of Health and Welfare . Chapter 4: health of population groups In: Australia’s Health 2006. Canberra: Commonwealth of Australia, 2006. Available at: http://www.aihw.gov.au/publications/aus/ah06/ah06‐c08.pdf. Accessed 18 December 2009. [Google Scholar]
- 16. Schillinger D, Piette J, Grumbach K et al. Physician communication with diabetic patients who have low health literacy. Archives of Internal Medicine, 2003; 163: 83–90. [DOI] [PubMed] [Google Scholar]
- 17. Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient Education and Counseling, 1996; 27: 33–39. [DOI] [PubMed] [Google Scholar]
- 18. McKauge L, Emmerton L, Bond J et al. An initiative to improve the professional communication skills of first‐year pharmacy students In: The Student Experience, Proceedings of the 32nd HERDSA Annual Conference; 2009. July 6‐9; Darwin: 284‐95. Available at: http://www.herdsa.org.au/wp‐content/uploads/conference/2009/papers/HERDSA2009_McKauge_L.pdf. Accessed 18 December 2009. [Google Scholar]
- 19. Pharmaceutical Society of Australia . Competency standards for pharmacists in Australia 2003. Available at: http://www.psa.org.au/site.php?id=1123. Accessed 18 December 2009.
- 20. Chisolm DJ, Buchanan L. Measuring adolescent functional health literacy: a pilot validation of the test of functional health literacy in adults. Journal of Adolescent Health, 2007; 41: 312–314. [DOI] [PubMed] [Google Scholar]


